Nutritional Strategies to Assist in Alleviating Psychiatric and Neurological Disorders through the Gut-Brain Axis
A special issue of Nutrients (ISSN 2072-6643). This special issue belongs to the section "Prebiotics and Probiotics".
Deadline for manuscript submissions: closed (16 June 2023) | Viewed by 25592
Special Issue Editor
Interests: prebiotics and probiotics; gut microbiota; nutrition; immunology; metabolic diseases; gut–brain axis; gastrointestinal diseases; endocrine disease
Special Issues, Collections and Topics in MDPI journals
Special Issue Information
Dear Colleagues,
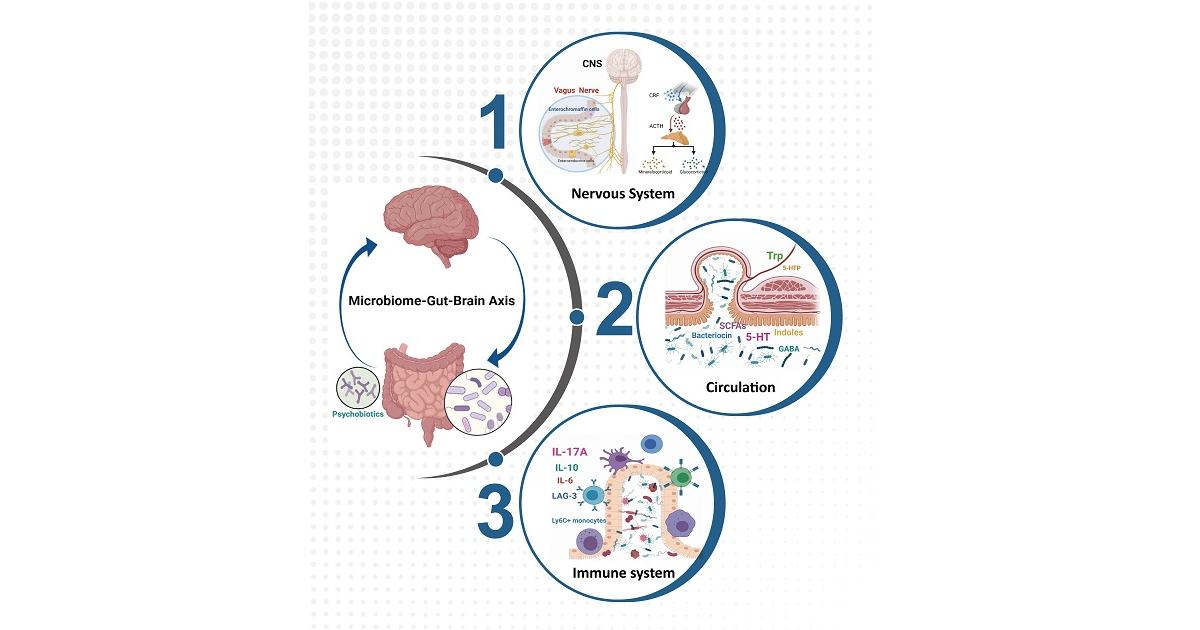
Gut microbiota are emerging as an area of scientific interest and a possible new target for different psychiatric and neurological disorders. Modification in gut microbiota composition appears to influence mood, cognition, learning, and memory by modulating endocrine, immune, and neuronal pathways. A better understanding of the involvement of the gut–brain axis in brain diseases may provide new therapeutic strategies.
The aim of this Special Issue is to understand how a nutritional strategy—including prebiotics, probiotics, postbiotics, and natural compounds that regulate the intestinal environment, such as gut microbiota, gut barrier function, gut immunity, etc.— can affect the nervous system and alleviate different diseases (i.e., mood disorders, autism, neurological and neurodegenerative diseases, chronic pain, addiction, and other social-stress-induced diseases). It will also explore the identification of specific pathways, molecules, or mechanisms to develop future therapies. We invite all interested researchers to submit review articles or original papers related to this topic.
Prof. Dr. Gang Wang
Guest Editor
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the special issue website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Nutrients is an international peer-reviewed open access semimonthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2900 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- psychiatric and neurological disorders
- postbiotics
- probiotics
- prebiotics
- natural compounds
- gut microbiota
- gut–brain axis






