Editorial Board Members’ Collection Series: Intensive Care and Anesthesiology
A special issue of Medicina (ISSN 1648-9144). This special issue belongs to the section "Intensive Care/ Anesthesiology".
Deadline for manuscript submissions: closed (31 March 2024) | Viewed by 2524
Special Issue Editors
Interests: oxygen transport; carbon dioxide metabolism; shock; microcirculation; acid-base metabolism
2. Department of Medicine, Surgery and Dentistry “Scuola Medica Salernitana”, University of Salerno, 84084 Fisciano, Italy
Interests: sepsis; trauma; heart and lung failure
Special Issues, Collections and Topics in MDPI journals
Special Issue Information
Dear Colleagues,
We are pleased to announce this Special Issue, titled “Editorial Board Members' Collection Series: Intensive Care and Anesthesiology”. This Special Issue will be a collection of papers from our Editorial Board Members and researchers invited by the Editorial Board Members. The aim is to provide a venue for networking and communication between Medicina and scholars in the field of gastrointestinal and hepatic diseases. All papers will be published fully open access after undergoing peer review.
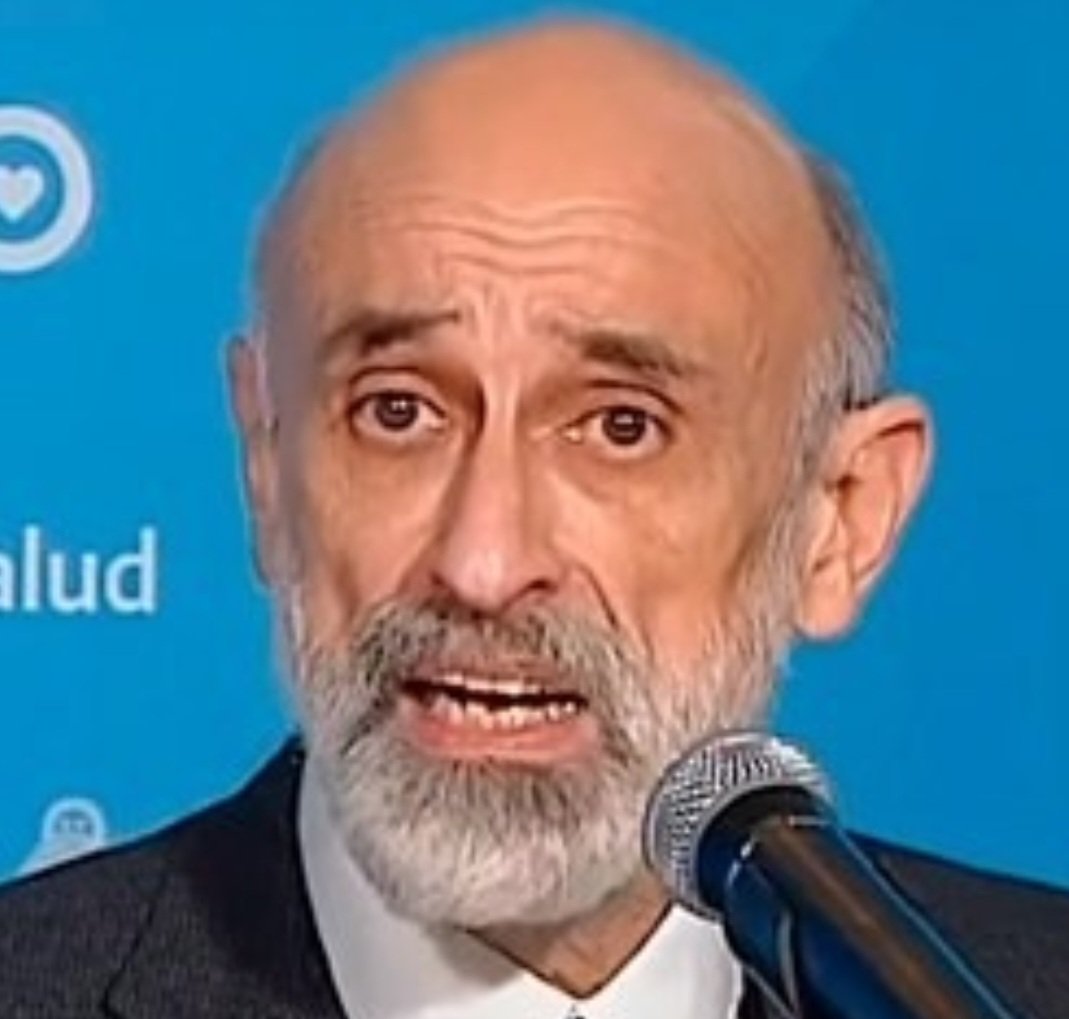
Prof. Dr. Arnaldo Dubin
Prof. Dr. Ornella Piazza
Dr. Edward A. Bittner
Guest Editors
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the special issue website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Medicina is an international peer-reviewed open access monthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 1800 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- critical care
- airway management
- post-anesthesia care
- anesthesia for general surgery
- burn injury
- microcirculation
- acid-base metabolism
- oxygen transport
- sepsis
- heart and lung failure
- trauma
- emergency medicine
- acute pain management
- intra-operative management