Pulmonary Hypertension: Insights on Pathophysiology, Diagnosis and Management
A special issue of Life (ISSN 2075-1729). This special issue belongs to the section "Physiology and Pathology".
Deadline for manuscript submissions: 31 July 2024 | Viewed by 4598
Special Issue Editor
2. Pulmonary Hypertension Unit, Royal Brompton Hospital, Guy’s and St Thomas’ Foundation Trust, Sydney Street, London, UK
Interests: pulmonary hypertension; adult congenital heart disease; heart failure; thrombosis
Special Issues, Collections and Topics in MDPI journals
Special Issue Information
Dear Colleagues,
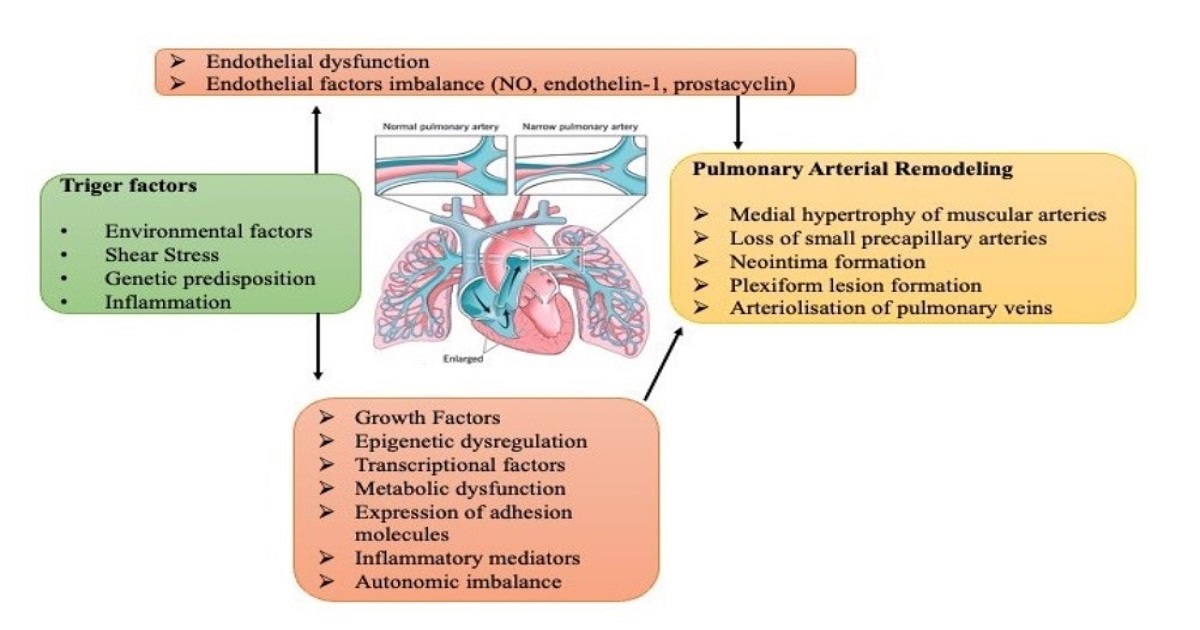
Pulmonary hypertension (PH) represents a rare and heterogeneous group of pulmonary vasculopathies defined by elevated mean pulmonary arterial pressure and pulmonary vascular resistance, which progressively lead to right heart failure and premature death if not diagnosed early and promptly treated. In the past 20 years there has been increased research interest in the fields of pathophysiology and targeted pulmonary arterial hypertension (PAH) therapy, while new diagnostic modalities and algorithms were employed to detect PH early. In addition, national and international registries have provided important information about the epidemiology of the disease, which changes steadily over time. Whereas younger female patients were diagnosed with idiopathic PAH in 1980, it is now frequently diagnosed in elderly patients with comorbidities, while a female predominance is not the rule among older patients. Furthermore, patients’ risk stratification according to clinical, neurohormonal, echocardiographic, and hemodynamic parameters plays an important role in decisions on therapeutic management. Finally, survival has substantially increased over time, but it is still poor in several PH subgroups.
In this Special Issue, we would like to invite original clinical as well as basic research and state-of-the-art reviews related to pathophysiology, diagnostics, and therapeutics in the whole spectrum of PH. We would be grateful to receive your submissions to move the field of PH forward.
Dr. Alexandra ArvanitakiGuest Editor
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the special issue website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Life is an international peer-reviewed open access monthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2600 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- pulmonary hypertension
- pulmonary arterial hypertension
- pathophysiology
- diagnosis
- risk stratification
- management
- pharmacotherapy






