Impact of Scoring Balloon Angioplasty on Lesion Preparation for DCB Treatment of Coronary Lesions
Abstract
:1. Introduction
2. Methods
2.1. Study Population
2.2. Target Lesion Preparation and DCB Treatment
2.3. Angiographic Measurement and Study Endpoint
2.4. Patient Follow-Up
2.5. Statistical Analysis
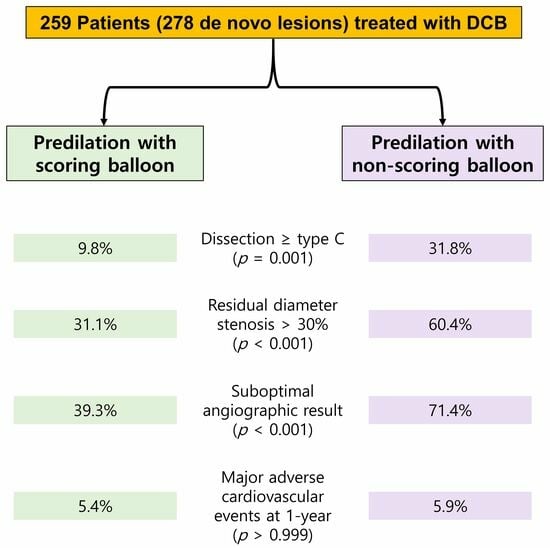
3. Results
3.1. Baseline Clinical and Procedure Characteristics
3.2. Angiographic Results and Study Endpoint
3.3. Clinical Outcomes
3.4. Independent Predictors Associated with Severe Dissection and Optimal Angiographic Result
4. Discussion
5. Study Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Her, A.Y.; Shin, E.S.; Bang, L.H.; Nuruddin, A.A.; Tang, Q.; Hsieh, I.C.; Hsu, J.C.; Kiam, O.T.; Qiu, C.; Qian, J.; et al. Drug-coated balloon treatment in coronary artery disease: Recommendations from an Asia-Pacific Consensus Group. Cardiol. J. 2021, 28, 136–149. [Google Scholar] [CrossRef] [PubMed]
- Jeger, R.V.; Eccleshall, S.; Wan Ahmad, W.A.; Ge, J.; Poerner, T.C.; Shin, E.S.; Alfonso, F.; Latib, A.; Ong, P.J.; Rissanen, T.T.; et al. Drug-coated balloons for coronary artery disease: Third report of the International DCB Consensus Group. JACC Cardiovasc. Interv. 2020, 13, 1391–1402. [Google Scholar] [CrossRef] [PubMed]
- Köln, P.J.; Scheller, B.; Liew, H.B.; Rissanen, T.T.; Ahmad, W.A.; Weser, R.; Hauschild, T.; Nuruddin, A.A.; Clever, Y.P.; Ho, H.H.; et al. Treatment of chronic total occlusions in native coronary arteries by drug-coated balloons without stenting—A feasibility and safety study. Int. J. Cardiol. 2016, 225, 262–267. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, T.; Hansen, S.; Meincke, F.; Frerker, C.; Kuck, K.H.; Bergmann, M.W. Safety and efficacy of lesion preparation with the AngioSculpt Scoring Balloon in left main interventions: The ALSTER Left Main registry. EuroIntervention 2016, 11, 1346–1354. [Google Scholar] [CrossRef] [PubMed]
- Kufner, S.; Joner, M.; Schneider, S.; Tölg, R.; Zrenner, B.; Repp, J.; Starkmann, A.; Xhepa, E.; Ibrahim, T.; Cassese, S.; et al. Neointimal modification with scoring balloon and efficacy of drug-coated balloon therapy in patients with restenosis in drug-eluting coronary stents: A randomized controlled trial. JACC Cardiovasc. Interv. 2017, 10, 1332–1340. [Google Scholar] [CrossRef] [PubMed]
- Bonaventura, K.; Schwefer, M.; Yusof, A.K.M.; Waliszewski, M.; Krackhardt, F.; Steen, P.; Ocaranza, R.; Zuhdi, A.S.; Bang, L.H.; Graf, K.; et al. Systematic scoring balloon lesion preparation for drug-coated balloon angioplasty in clinical routine: Results of the PASSWORD Observational Study. Adv. Ther. 2020, 37, 2210–2223. [Google Scholar] [CrossRef]
- Albertal, M.; Van Langenhove, G.; Regar, E.; Kay, I.P.; Foley, D.; Sianos, G.; Kozuma, K.; Beijsterveldt, T.; Carlier, S.G.; Belardi, J.A.; et al. Uncomplicated moderate coronary artery dissections after balloon angioplasty: Good outcome without stenting. Heart 2001, 86, 193–198. [Google Scholar] [CrossRef] [PubMed]
- Yahagi, K.; Kolodgie, F.D.; Otsuka, F.; Finn, A.V.; Davis, H.R.; Joner, M.; Virmani, R. Pathophysiology of native coronary, vein graft, and in-stent atherosclerosis. Nat. Rev. Cardiol. 2016, 13, 79–98. [Google Scholar] [CrossRef]
- Cutlip, D.E.; Windecker, S.; Mehran, R.; Boam, A.; Cohen, D.J.; van Es, G.A.; Steg, P.G.; Morel, M.A.; Mauri, L.; Vranckx, P.; et al. Clinical end points in coronary stent trials: A case for standardized definitions. Circulation 2007, 115, 2344–2351. [Google Scholar] [CrossRef]
- Her, A.Y.; Ann, S.H.; Singh, G.B.; Kim, Y.H.; Yoo, S.Y.; Garg, S.; Koo, B.K.; Shin, E.S. Comparison of paclitaxel-coated balloon treatment and plain old balloon angioplasty for de novo coronary lesions. Yonsei Med. J. 2016, 57, 337–341. [Google Scholar] [CrossRef] [PubMed]
- Ann, S.H.; Balbir Singh, G.; Lim, K.H.; Koo, B.K.; Shin, E.S. Anatomical and physiological changes after paclitaxel-coated balloon for atherosclerotic de novo coronary lesions: Serial IVUS-VH and FFR study. PLoS ONE 2016, 11, e0147057. [Google Scholar] [CrossRef] [PubMed]
- Her, A.Y.; Shin, E.S.; Lee, J.M.; Garg, S.; Doh, J.H.; Nam, C.W.; Koo, B.K. Paclitaxel-coated balloon treatment for functionally nonsignificant residual coronary lesions after balloon angioplasty. Int. J. Cardiovasc. Imaging 2018, 34, 1339–1347. [Google Scholar] [CrossRef] [PubMed]
- Her, A.Y.; Yuan, S.L.; Jun, E.J.; Bhak, Y.; Kim, M.H.; Garg, S.; Kim, Y.H.; Kun, L.; Hui, L.; Zhi, W.; et al. Drug-coated balloon treatment for nonsmall de-novo coronary artery disease: Angiographic and clinical outcomes. Coron. Artery Dis. 2021, 32, 534–540. [Google Scholar] [CrossRef] [PubMed]
- Hui, L.; Shin, E.S.; Jun, E.J.; Bhak, Y.; Garg, S.; Kim, T.H.; Sohn, C.B.; Choi, B.J.; Kun, L.; Yuan, S.L.; et al. Impact of dissection after drug-coated balloon treatment of de novo coronary lesions: Angiographic and clinical outcomes. Yonsei Med. J. 2020, 61, 1004–1012. [Google Scholar] [CrossRef] [PubMed]
- Ueno, K.; Morita, N.; Kojima, Y.; Takahashi, H.; Esaki, M.; Kondo, H.; Ando, Y.; Yamada, M.; Kosokabe, T. Serial quantitative angiographic study of target lumen enlargement after drug-coated balloon angioplasty for native coronary artery disease. Catheter. Cardiovasc. Interv. 2023, 101, 713–721. [Google Scholar] [CrossRef] [PubMed]
- de Ribamar Costa, J., Jr.; Mintz, G.S.; Carlier, S.G.; Mehran, R.; Teirstein, P.; Sano, K.; Liu, X.; Lui, J.; Na, Y.; Castellanos, C.; et al. Nonrandomized comparison of coronary stenting under intravascular ultrasound guidance of direct stenting without predilation versus conventional predilation with a semi-compliant balloon versus predilation with a new scoring balloon. Am. J. Cardiol. 2007, 100, 812–817. [Google Scholar] [CrossRef] [PubMed]
- Joner, M.; Byrne, R.A.; Lapointe, J.M.; Radke, P.W.; Bayer, G.; Steigerwald, K.; Wittchow, E. Comparative assessment of drug-eluting balloons in an advanced porcine model of coronary restenosis. Thromb. Haemost. 2011, 105, 864–872. [Google Scholar] [CrossRef] [PubMed]
- Radke, P.W.; Joner, M.; Joost, A.; Byrne, R.A.; Hartwig, S.; Bayer, G.; Steigerwald, K.; Wittchow, E. Vascular effects of paclitaxel following drug-eluting balloon angioplasty in a porcine coronary model: The importance of excipients. EuroIntervention 2011, 7, 730–737. [Google Scholar] [CrossRef] [PubMed]


| Scoring Balloon (N = 56 Patients) | Non-Scoring Balloon (N = 203 Patients) | p-Value | |
|---|---|---|---|
| Age, years | 60.8 ± 9.1 | 62.7 ± 11.3 | 0.202 |
| Men | 40 (71.4) | 138 (68.0) | 0.741 |
| Cardiovascular risk factors | |||
| Hypertension | 37 (66.1) | 143 (70.4) | 0.642 |
| Diabetes | 14 (25.0) | 72 (35.5) | 0.284 |
| Dyslipidemia | 47 (83.9) | 156 (76.8) | 0.461 |
| Current smoking | 13 (23.2) | 50 (26.5) | 0.352 |
| Previous PCI | 7 (12.5) | 44 (21.7) | 0.205 |
| Clinical manifestations | 0.573 | ||
| Stable angina | 21 (37.5) | 67 (33.0) | |
| Unstable angina | 22 (39.3) | 90 (44.3) | |
| Non-ST-segment elevation myocardial infarction | 11 (19.6) | 33 (16.3) | |
| ST-segment elevation myocardial infarction | 2 (3.6) | 13 (6.4) | |
| Treated vessel | N = 61 vessels | N = 217 vessels | <0.001 |
| Left main | 2 (3.3) | 1 (0.5) | |
| Left anterior descending | 33 (54.1) | 68 (31.3) | |
| Left circumflex | 12 (19.7) | 105 (48.4) | |
| Right coronary | 14 (23.0) | 43 (19.8) | |
| SYNTAX score | 9.8 ± 5.5 | 10.3 ± 7.0 | 0.504 |
| Total number of treated vessels | 1.0 ± 0.2 | 1.0 ± 0.1 | 0.234 |
| DCB treatment | |||
| DCB diameter, mm | 2.8 ± 0.4 | 2.5 ± 0.3 | <0.001 |
| DCB length, mm | 23.6 ± 5.0 | 22.0 ± 5.2 | 0.041 |
| Maximal inflation pressure, atm | 9.6 ± 2.1 | 9.2 ± 2.3 | 0.259 |
| Inflation time | 67.7 ± 21.0 | 52.4 ± 18.3 | <0.001 |
| DCB balloon-to-artery ratio | 1.0 ± 0.1 | 1.1 ± 0.2 | 0.337 |
| Dissection type after procedure | |||
| None | 17 (27.9) | 37 (17.1) | 0.088 |
| A | 19 (31.1) | 46 (21.2) | 0.147 |
| B | 19 (31.1) | 65 (30.0) | 0.983 |
| C | 6 (9.8) | 69 (31.8) | 0.001 |
| Scoring Balloon (N = 61 Vessels) | Non-Scoring Balloon (N = 217 Vessels) | p-Value | |
|---|---|---|---|
| Before procedure | |||
| Lesion length, mm | 14.61± 6.36 | 17.41 ± 5.58 | 0.001 |
| Reference vessel diameter, mm | 2.74 ± 0.49 | 2.46 ± 0.48 | <0.001 |
| Minimum lumen diameter, mm | 0.99 ± 0.35 | 0.71 ± 0.39 | <0.001 |
| Diameter stenosis, % | 61.33 ± 11.47 | 70.79 ± 13.70 | <0.001 |
| After procedure | |||
| Minimum lumen diameter, mm | 2.08 ± 0.42 | 1.64 ± 0.43 | <0.001 |
| Diameter stenosis, % | 26.29 ± 9.84 | 34.50 ± 11.93 | <0.001 |
| Lumen gain, mm | 1.10 ± 0.38 | 0.94 ± 0.42 | 0.009 |
| TIMI flow grade 3 | 61 (100) | 215 (99.1) | >0.999 |
| Residual stenosis ≤ 30% | 42 (68.9) | 86 (39.6) | <0.001 |
| Dissection < type C | 55 (90.2) | 148 (68.2) | 0.001 |
| Optimal angiographic result | 37 (60.7) | 62 (28.6) | <0.001 |
| Lumen gain according to dissection severity, mm | |||
| None | 1.31 ± 0.47 | 0.89 ± 0.42 | 0.002 |
| A | 0.96 ± 0.28 | 0.95 ± 0.43 | 0.969 |
| B | 1.05 ± 0.35 | 0.99 ± 0.42 | 0.601 |
| C | 1.10 ± 0.24 | 0.91 ± 0.43 | 0.273 |
| Scoring Balloon (N = 56) | Non-Scoring Balloon (N = 203) | |||
|---|---|---|---|---|
| Optimal Angiographic Result (N = 34) | Suboptimal Angiographic Result (N = 22) | Optimal Angiographic Result (N = 55) | Suboptimal Angiographic Result (N = 148) | |
| Major adverse cardiovascular events | 1 (1.8) | 2 (3.6) | 3 (1.5) | 9 (4.4) |
| Cardiac death | 0 | 0 | 0 | 2 (1.0) |
| Myocardial infarction | 0 | 0 | 0 | 0 |
| Target lesion thrombosis | 0 | 0 | 0 | 0 |
| Target vessel revascularization | 1 (1.8) | 2 (3.6) | 5 (1.5) | 8 (3.9) |
| Variable | Severe Dissection | Optimal Angiographic Result | ||
|---|---|---|---|---|
| Odds Ratio (95% CI) | p-Value | Odds Ratio (95% CI) | p-Value | |
| Age | 0.99 (0.96–1.02) | 0.359 | 1.00 (0.97–1.03) | 0.995 |
| Women | 1.62 (0.82–3.20) | 0.162 | 0.70 (0.35–1.35) | 0.291 |
| Hypertension | 0.65 (0.33–1.30) | 0.220 | 1.07 (0.55–2.13) | 0.845 |
| Diabetes | 1.25 (0.64–2.44) | 0.508 | 0.77 (0.39–1.50) | 0.454 |
| Dyslipidemia | 1.03 (0.52–2.04) | 0.936 | 1.00 (0.51–1.96) | 0.996 |
| Current smoking | 0.73 (0.32–1.58) | 0.433 | 1.14 (0.52–2.46) | 0.731 |
| Acute coronary syndrome | 0.96 (0.50–1.91) | 0.917 | 1.01 (0.53–1.96) | 0.968 |
| Left anterior descending artery | 0.59 (0.29–1.15) | 0.130 | 1.52 (0.82–2.81) | 0.181 |
| DCB balloon-to-artery ratio | 0.69 (0.12–3.87) | 0.679 | 5.46 (1.43–21.93) | 0.014 |
| DCB inflation time | 1.01 (0.99–1.03) | 0.380 | 1.00 (0.99–1.02) | 0.574 |
| Baseline diameter stenosis | 0.99 (0.97–1.02) | 0.566 | 0.99 (0.96–1.01) | 0.310 |
| Scoring balloon | 0.18 (0.05–0.49) | 0.002 | 3.08 (1.47–6.58) | 0.003 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shin, E.-S.; Ann, S.H.; Jang, M.H.; Kim, B.; Kim, T.-H.; Sohn, C.-B.; Choi, B.J. Impact of Scoring Balloon Angioplasty on Lesion Preparation for DCB Treatment of Coronary Lesions. J. Clin. Med. 2023, 12, 6254. https://doi.org/10.3390/jcm12196254
Shin E-S, Ann SH, Jang MH, Kim B, Kim T-H, Sohn C-B, Choi BJ. Impact of Scoring Balloon Angioplasty on Lesion Preparation for DCB Treatment of Coronary Lesions. Journal of Clinical Medicine. 2023; 12(19):6254. https://doi.org/10.3390/jcm12196254
Chicago/Turabian StyleShin, Eun-Seok, Soe Hee Ann, Mi Hee Jang, Bitna Kim, Tae-Hyun Kim, Chang-Bae Sohn, and Byung Joo Choi. 2023. "Impact of Scoring Balloon Angioplasty on Lesion Preparation for DCB Treatment of Coronary Lesions" Journal of Clinical Medicine 12, no. 19: 6254. https://doi.org/10.3390/jcm12196254