Advances in Cancer Imaging
A topical collection in Diagnostics (ISSN 2075-4418). This collection belongs to the section "Medical Imaging and Theranostics".
Viewed by 10014Editor
Interests: multimodal-3D analysis/AI
Topical Collection Information
Cancer imaging is playing an essential role in research discovery and in the detection and determination of the stage and decisions around treatment and evaluation of treatment in the clinical area.
In the last decade, in addition to traditional cancer imaging modalities such as CT and MRI, new imaging technologies have been and are being developed, and those provide further information for high-quality diagnosis and treatment.
Multimodal imaging and computational power with artificial intelligence (AI) have been showing the additional dimension of information around cancer.
The aim of this Special Issue is to help us to better understand current and future cancer imaging technologies and guide how these technologies can improve research, diagnosis, and treatment in cancer.
Specifically, this Special Issue will focus on the roles of multimodality imaging and AI in cancer imaging.
Original research articles and review articles aiming to shed light on important advances in modalities in cancer imaging, including radiological and pathology imaging, are invited.
Dr. Yukako Yagi
Collection Editor
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Diagnostics is an international peer-reviewed open access semimonthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2600 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- Computed tomography (CT) and magnetic resonance imaging (MRI)
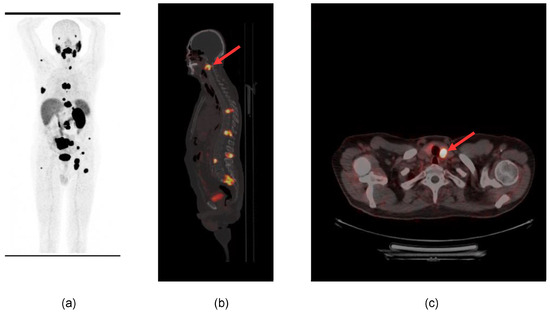
- Molecular and nuclear imaging (PET and SPECT)
- Endoscopy
- 3D Imaging
- Digital Pathology
- Spatial transcriptomics
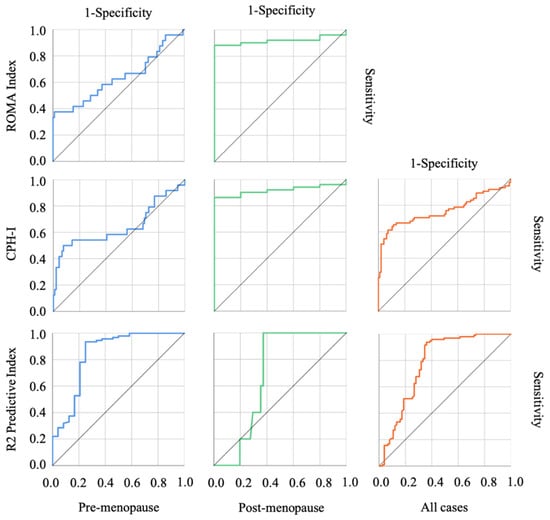
- Artificial Intelligenve (AI)
- Machine learning
- Multimodal imaging