Neurodevelopmental Disorders: From Pathophysiology to Treatment
Share This Topical Collection
Editors
 Dr. Nader Perroud
Dr. Nader Perroud
 Dr. Nader Perroud
Dr. Nader Perroud
E-Mail
Website
Collection Editor
1. Department of Psychiatry, Faculty of Medicine, University of Geneva, Geneva, Switzerland
2. TRE Unit, Division of Psychiatric Specialties, Department of Psychiatry, University Hospital of Geneva, Geneva, Switzerland
Interests: ADHD; personality disorders from diagnosis to treatment
Special Issues, Collections and Topics in MDPI journals
 Dr. Markus Mathaus Kosel
Dr. Markus Mathaus Kosel
 Dr. Markus Mathaus Kosel
Dr. Markus Mathaus Kosel
E-Mail
Website
Collection Editor
Hôpitaux universitaires de Genève, Geneva, Switzerland
Interests: clinically oriented research in treatment-resistant depression; autism spectrum disorder and intellectual disability; main topics include diagnosis, treatment, genetics and neuroimaging
Special Issues, Collections and Topics in MDPI journals
 Dr. Gaelle E. Doucet
Dr. Gaelle E. Doucet
 Dr. Gaelle E. Doucet
Dr. Gaelle E. Doucet
E-Mail
Website
Collection Editor
Institute for Human Neuroscience, Boys Town National Research Hospital, Omaha, NE 68010, USA
Interests: human cognition; resting-state fMRI; aging; schizophrenia; epilepsy; functional connectivity
Topical Collection Information
Dear Colleagues,
DSM-5, introduced in 2013, allowed a renewed appreciation of the longitudinal, whole-life perspective of neurodevelopmental disorders in psychiatry including autism spectrum disorder (ASD) and other communication, speech and language disorders, attention-deficit/hyperactivity disorder (ADHD), intellectual disability (ID) as well as other specific learning disorders.
However, our understanding of the basic aspects of the pathophysiology of these disorders and efficient therapies is still incomplete. The adult population suffering from these disorders is also widely underresearched and thus rarely benefit from adequate treatments.
In this Topical Collection of Biomedicines, we aim to present to the journal readers the actual state of the art in the understanding of the pathophysiology of neurodevelopmental disorders and their treatments, from birth to the end of life.
Dr. Nader Perroud
Dr. Markus Mathaus Kosel
Dr. Gaelle E. Doucet
Collection Editors
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Biomedicines is an international peer-reviewed open access monthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript.
The Article Processing Charge (APC) for publication in this open access journal is 2600 CHF (Swiss Francs).
Submitted papers should be well formatted and use good English. Authors may use MDPI's
English editing service prior to publication or during author revisions.
Keywords
- intellectual disability
- autism spectrum disorder
- attention-deficit/hyperactivity disorder
- drug treatment
- neuroimaging
Published Papers (4 papers)
Open AccessReview
Relationship between Non-Invasive Brain Stimulation and Autonomic Nervous System
by
Giovanni Messina, Antonietta Monda, Antonietta Messina, Girolamo Di Maio, Vincenzo Monda, Pierpaolo Limone, Anna Dipace, Marcellino Monda, Rita Polito and Fiorenzo Moscatelli
Biomedicines 2024, 12(5), 972; https://doi.org/10.3390/biomedicines12050972 (registering DOI) - 28 Apr 2024
Viewed by 184
Abstract
Non-invasive brain stimulation (NIBS) approaches have seen a rise in utilization in both clinical and basic neuroscience in recent years. Here, we concentrate on the two methods that have received the greatest research: transcranial direct current stimulation (tDCS) and repetitive transcranial magnetic stimulation
[...] Read more.
Non-invasive brain stimulation (NIBS) approaches have seen a rise in utilization in both clinical and basic neuroscience in recent years. Here, we concentrate on the two methods that have received the greatest research: transcranial direct current stimulation (tDCS) and repetitive transcranial magnetic stimulation (rTMS). Both approaches have yielded pertinent data regarding the cortical excitability in subjects in good health as well as pertinent advancements in the management of various clinical disorders. NIBS is a helpful method for comprehending the cortical control of the ANS. Previous research has shown that there are notable changes in muscular sympathetic nerve activity when the motor cortex is modulated. Furthermore, in NIBS investigations, the ANS has been employed more frequently as an outcome measure to comprehend the overall impacts of these methods, including their safety profile. Though there is ample proof that brain stimulation has autonomic effects on animals, new research on the connection between NIBS and the ANS has produced contradictory findings. In order to better understand NIBS processes and ANS function, it is crucial to take into account the reciprocal relationship that exists between central modulation and ANS function.
Full article
Open AccessArticle
Preliminary Findings of Elevated Inflammatory Plasma Cytokines in Children with Autism Who Have Co-Morbid Gastrointestinal Symptoms
by
Paul Ashwood
Cited by 3 | Viewed by 1647
Abstract
Autism spectrum disorder (AU) is present in approximately 2% of the population and is often associated with co-morbidities that can impact quality of life. One of the most common co-morbidities in autism is the presence of gastrointestinal (GI) symptoms consisting of irregular bowel
[...] Read more.
Autism spectrum disorder (AU) is present in approximately 2% of the population and is often associated with co-morbidities that can impact quality of life. One of the most common co-morbidities in autism is the presence of gastrointestinal (GI) symptoms consisting of irregular bowel habits such as constipation, diarrhea, or alternating bowel habit. Evidence of immune infiltration and immune activation has been shown in the ileum and colon of children with AU with GI symptoms. Moreover, immune dysfunction is a contributing factor in many GI diseases, and we hypothesize that it would be more apparent in children with AU that exhibit GI symptoms than those who do not present with GI symptoms. The aim of this preliminary study was to determine whether there are altered cytokine levels in plasma in children with AU with GI symptoms compared with children with AU without GI symptoms, typically developing (TD) children with GI symptoms and TD children without GI symptoms, from the same population-based cohort. Plasma cytokine levels were assessed by multiplex assays. No differences in plasma cytokines were observed in TD controls with or without GI symptoms; however, many innate (IL-1α, TNFα, GM-CSF, IFNα) and adaptive cytokines (IL-4, IL-13, IL-12p70) were increased in AU children with GI symptoms compared with children with AU with no GI symptoms. The mucosal relevant cytokine IL-15 was increased in AU with GI symptoms compared with all groups. In contrast, the regulatory cytokine IL-10, was reduced in AU with GI symptoms and may suggest an imbalance in pro-inflammatory/regulatory signals. These data suggest that children with AU and GI symptoms have an imbalance in their immune response that is evident in their circulating plasma cytokine levels. A finding that could point to potential therapeutic and/or monitoring strategies for GI issues in AU.
Full article
Open AccessReview
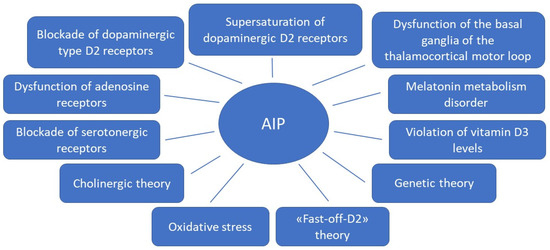
Pathophysiological Mechanisms of Antipsychotic-Induced Parkinsonism
by
Elena E. Vaiman, Natalia A. Shnayder, Aiperi K. Khasanova, Anna I. Strelnik, Arseny J. Gayduk, Mustafa Al-Zamil, Margarita R. Sapronova, Natalia G. Zhukova, Daria A. Smirnova and Regina F. Nasyrova
Cited by 8 | Viewed by 2728
Abstract
Among neurological adverse reactions in patients with schizophrenia treated with antipsychotics (APs), drug-induced parkinsonism (DIP) is the most common motility disorder caused by drugs affecting dopamine receptors. One of the causes of DIP is the disruption of neurotransmitter interactions that regulate the signaling
[...] Read more.
Among neurological adverse reactions in patients with schizophrenia treated with antipsychotics (APs), drug-induced parkinsonism (DIP) is the most common motility disorder caused by drugs affecting dopamine receptors. One of the causes of DIP is the disruption of neurotransmitter interactions that regulate the signaling pathways of the dopaminergic, cholinergic, GABAergic, adenosinergic, endocannabinoid, and other neurotransmitter systems. Presently, the development mechanisms remain poorly understood despite the presence of the considered theories of DIP pathogenesis.
Full article
►▼
Show Figures
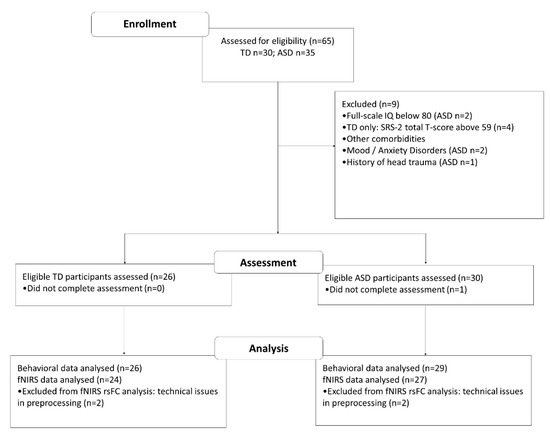
Open AccessArticle
Abnormal Prefrontal Functional Connectivity Is Associated with Inflexible Information Processing in Patients with Autism Spectrum Disorder (ASD): An fNIRS Study
by
Melody M. Y. Chan, Ming-Chung Chan, Oscar Long-Hin Lai, Karthikeyan Krishnamurthy and Yvonne M. Y. Han
Cited by 6 | Viewed by 2524
Abstract
Individuals with autism spectrum disorder (ASD) are characterized by impairments in flexibly acquiring and maintaining new information, as well as in applying learned information for problem solving. However, the neural mechanism underpinning such impairments remains unclear. This study investigated the flexibility in the
[...] Read more.
Individuals with autism spectrum disorder (ASD) are characterized by impairments in flexibly acquiring and maintaining new information, as well as in applying learned information for problem solving. However, the neural mechanism underpinning such impairments remains unclear. This study investigated the flexibility in the acquisition and application of visual information in ASD (aged 14–21) when they performed the Wisconsin Card Sorting Test (WCST). Behavioral data including response accuracy and latency, and prefrontal hemodynamic data measured by functional near-infrared spectroscopy (fNIRS), were collected when individuals performed WCST. Canonical general linear model and functional connectivity analyses were performed to examine the prefrontal activation and synchronization patterns, respectively. Results showed that although ASD individuals (
n = 29) achieved comparable accuracy rates when compared with age- and intelligence quotient (IQ)-matched typically developing (TD;
n = 26) individuals (F
1,53 = 3.15,
p = 0.082), ASD individuals needed significantly more time to acquire and apply WCST card sorting rules (F
1,53 = 17.92,
p < 0.001). Moreover, ASD individuals showed significantly lower prefrontal functional connectivity than TD individuals during WCST (F
1,42 = 9.99,
p = 0.003). The hypoconnectivity in ASD individuals was highly significant in the right lateral PFC in the acquisition condition (
p = 0.005) and in the bilateral lateral PFC in the application condition (ps = 0.006). Furthermore, slower WCST reaction time was correlated with lower bilateral lateral PFC functional connectivity only in the application condition (ps = 0.003) but not the acquisition condition. Impairment in information acquisition and application is evident in ASD individuals and is mediated by processing speed, which is associated with lower functional connectivity in the bilateral lateral PFC when these individuals apply learned rules to solve novel problems.
Full article
►▼
Show Figures