Interactions between Obstructive Sleep Apnea Syndrome Severity, Obesity, Sex Difference and Attention-Deficit/Hyperactivity Disorder on Health-Related Quality of Life: A Non-Interventional Prospective Observational Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design, Setting, and Subject
2.2. Data Collection
2.3. Overnight PSG
2.4. Adult ASRS
2.5. Self-Reported HRQoL
2.6. Outcome Assessment
2.7. Statistical Analysis
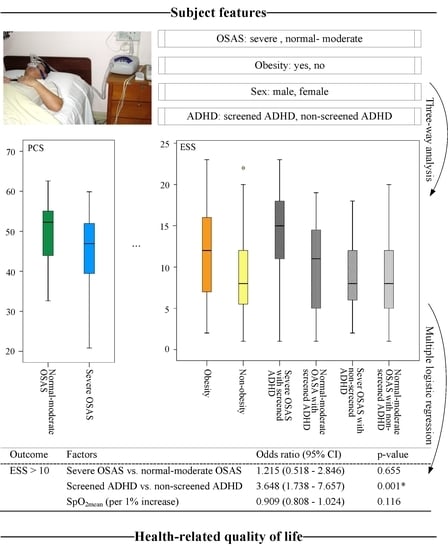
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Theofilou, P. Quality of Life: Definition and Measurement. Eur. J. Psychol. 2013, 9, 150–162. [Google Scholar] [CrossRef]
- Sosnowski, R.; Kulpa, M.; Ziętalewicz, U.; Wolski, J.K.; Nowakowski, R.; Bakuła, R.; Demkow, T. Basic issues concerning health-related quality of life. Cen Eur. J. Uro 2017, 70, 206–211. [Google Scholar] [CrossRef] [Green Version]
- Thorarinsdottir, E.H.; Bjornsdottir, E.; Benediktsdottir, B.; Janson, C.; Gislason, T.; Aspelund, T.; Kuna, S.T.; Pack, A.I.; Arnardottir, E.S. Definition of excessive daytime sleepiness in the general population: Feeling sleepy relates better to sleep-related symptoms and quality of life than the Epworth Sleepiness Scale score. Results from an epidemiological study. J. Sleep Res. 2019, 28, e12852. [Google Scholar] [CrossRef]
- Manzar, M.D.; BaHammam, A.S.; Hameed, U.A.; Spence, D.W.; Pandi-Perumal, S.R.; Moscovitch, A.; Streiner, D.L. Dimensionality of the Pittsburgh Sleep Quality Index: A systematic review. Health Qual. Life Outcomes 2018, 16, 89. [Google Scholar] [CrossRef] [PubMed]
- Calvin, A.D.; Albuquerque, F.N.; Lopez-Jimenez, F.; Somers, V.K. Obstructive sleep apnea, inflammation, and the metabolic syndrome. Metab. Syndr. Relat. Disord. 2009, 7, 271–278. [Google Scholar] [CrossRef] [Green Version]
- Phillips, C.L.; O’Driscoll, D.M. Hypertension and obstructive sleep apnea. Nat. Sci. Sleep 2013, 5, 43–52. [Google Scholar] [CrossRef] [Green Version]
- Coman, A.C.; Borzan, C.; Vesa, C.S.; Todea, D.A. Obstructive sleep apnea syndrome and the quality of life. Clujul. Med. 2016, 89, 390–395. [Google Scholar] [CrossRef] [Green Version]
- Moyer, C.A.; Sonnad, S.S.; Garetz, S.L.; Helman, J.I.; Chervin, R.D. Quality of life in obstructive sleep apnea: A systematic review of the literature. Sleep Med. 2001, 2, 477–491. [Google Scholar] [CrossRef]
- Park, J.G.; Ramar, K.; Olson, E.J. Updates on definition, consequences, and management of obstructive sleep apnea. Mayo Clin. Proc. 2011, 86, 549–555. [Google Scholar] [CrossRef] [Green Version]
- Arnardottir, E.S.; Maislin, G.; Jackson, N.; Schwab, R.J.; Benediktsdottir, B.; Teff, K.; Juliusson, S.; Pack, A.I.; Gislason, T. The role of obesity, different fat compartments and sleep apnea severity in circulating leptin levels: The Icelandic Sleep Apnea Cohort study. Int. J. Obes. 2013, 37, 835–842. [Google Scholar] [CrossRef] [Green Version]
- Gabbay, I.E.; Lavie, P. Age- and gender-related characteristics of obstructive sleep apnea. Sleep Breath. Schlaf. Atm. 2012, 16, 453–460. [Google Scholar] [CrossRef] [PubMed]
- Jehan, S.; Zizi, F.; Pandi-Perumal, S.R.; Wall, S.; Auguste, E.; Myers, A.K.; Jean-Louis, G.; McFarlane, S.I. Obstructive Sleep Apnea and Obesity: Implications for Public Health. Sleep Med. Disord. 2017, 1, 00019. [Google Scholar] [PubMed]
- Kastoer, C.; Benoist, L.B.L.; Dieltjens, M.; Torensma, B.; de Vries, L.H.; Vonk, P.E.; Ravesloot, M.J.L.; de Vries, N. Comparison of upper airway collapse patterns and its clinical significance: Drug-induced sleep endoscopy in patients without obstructive sleep apnea, positional and non-positional obstructive sleep apnea. Sleep Breath. Schlaf. Atm. 2018, 22, 939–948. [Google Scholar] [CrossRef]
- Kolotkin, R.L.; Meter, K.; Williams, G.R. Quality of life and obesity. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2001, 2, 219–229. [Google Scholar] [CrossRef] [PubMed]
- Mallampalli, M.P.; Carter, C.L. Exploring sex and gender differences in sleep health: A Society for Women’s Health Research Report. J. Womens Health 2014, 23, 553–562. [Google Scholar] [CrossRef] [Green Version]
- Krističević, T.; Štefan, L.; Sporiš, G. The Associations between Sleep Duration and Sleep Quality with Body-Mass Index in a Large Sample of Young Adults. Int. J. Environ. Res. Public Health 2018, 15, 758. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vgontzas, A.N.; Bixler, E.O.; Tan, T.L.; Kantner, D.; Martin, L.F.; Kales, A. Obesity without sleep apnea is associated with daytime sleepiness. Arch. Intern. Med. 1998, 158, 1333–1337. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Da Rocha, N.S.; Schuch, F.B.; Fleck, M.P. Gender differences in perception of quality of life in adults with and without chronic health conditions: The role of depressive symptoms. J. Health Psychol. 2014, 19, 721–729. [Google Scholar] [CrossRef]
- Salvi, V.; Migliarese, G.; Venturi, V.; Rossi, F.; Torriero, S.; Viganò, V.; Cerveri, G.; Mencacci, C. ADHD in adults: Clinical subtypes and associated characteristics. Riv. Di Psichiatr. 2019, 54, 84–89. [Google Scholar] [CrossRef]
- Agarwal, R.; Goldenberg, M.; Perry, R.; IsHak, W.W. The quality of life of adults with attention deficit hyperactivity disorder: A systematic review. Innov. Clin. Neurosci. 2012, 9, 10–21. [Google Scholar]
- Becker, A.; Roessner, V.; Breuer, D.; Döpfner, M.; Rothenberger, A. Relationship between quality of life and psychopathological profile: Data from an observational study in children with ADHD. Eur. Child Adolesc. Psychiatry 2011, 20, 267. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gau, S.S.; Kessler, R.C.; Tseng, W.L.; Wu, Y.Y.; Chiu, Y.N.; Yeh, C.B.; Hwu, H.G. Association between sleep problems and symptoms of attention-deficit/hyperactivity disorder in young adults. Sleep 2007, 30, 195–201. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Henriques, P.S.F. Sleep disorder investigation might be considered to be mandatory in attention deficit/hyperactivity disorder guideline. Arq. De Neuro-Psiquiatr. 2016, 74, 701–707. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oğuztürk, Ö.; Ekici, M.; Çimen, D.; Ekici, A.; Senturk, E. Attention deficit/hyperactivity disorder in adults with sleep apnea. J. Clin. Psychol. Med. Settings 2013, 20, 234–239. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hsieh, T.-H.; Lee, J.J.; Yu, E.W.-R.; Hu, H.-Y.; Lin, S.-Y.; Ho, C.-Y. Association between obesity and education level among the elderly in Taipei, Taiwan between 2013 and 2015: A cross-sectional study. Sci. Rep. 2020, 10, 20285. [Google Scholar] [CrossRef]
- Wu, M.-F.; Chen, Y.-H.; Chen, H.-C.; Huang, W.-C. Interactions among Obstructive Sleep Apnea Syndrome Severity, Sex, and Obesity on Circulatory Inflammatory Biomarkers in Patients with Suspected Obstructive Sleep Apnea Syndrome: A Retrospective, Cross-Sectional Study. Int. J. Environ. Res. Public Health 2020, 17, 4701. [Google Scholar] [CrossRef]
- Iber, C.; Ancoli-Israel, S.; Chesson, A.L.; Quan, S. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications. Westchest. IL Am. Acad. Sleep Med. 2007, 176, 2012. [Google Scholar]
- Shen, Y.; Zhang, Y.; Chan, B.S.M.; Meng, F.; Yang, T.; Luo, X.; Huang, C. Association of ADHD symptoms, depression and suicidal behaviors with anxiety in Chinese medical college students. BMC Psychiatry 2020, 20, 180. [Google Scholar] [CrossRef] [Green Version]
- Shi, M.; Liu, L.; Sun, X.; Wang, L. Associations between symptoms of attention-deficit/ hyperactivity disorder and life satisfaction in medical students: The mediating effect of resilience. BMC Med. Educ. 2018, 18, 164. [Google Scholar] [CrossRef]
- Matteson, K.A.; Raker, C.A.; Clark, M.A.; Frick, K.D. Abnormal uterine bleeding, health status, and usual source of medical care: Analyses using the Medical Expenditures Panel Survey. J. Womens Health 2013, 22, 959–965. [Google Scholar] [CrossRef] [Green Version]
- Mishra, G.D.; Hockey, R.; Dobson, A.J. A comparison of SF-36 summary measures of physical and mental health for women across the life course. Qual. Life Res. Int. J. Qual. Life Asp. Treat. Care Rehabil. 2014, 23, 1515–1521. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Kachuee, H.; Ameli, J.; Taheri, S.; Assari, S.; Riahipour, F.; Khedmat, H.; Saadat, A.R. Sleep Quality and Its Correlates in Renal Transplant Patients. Transplant. Proc. 2007, 39, 1095–1097. [Google Scholar] [CrossRef]
- Lapin, B.R.; Bena, J.F.; Walia, H.K.; Moul, D.E. The Epworth Sleepiness Scale: Validation of One-Dimensional Factor Structure in a Large Clinical Sample. J. Clin. Sleep Med. 2018, 14, 1293–1301. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hvolby, A. Associations of sleep disturbance with ADHD: Implications for treatment. Atten. Defic. Hyperact. Disord. 2015, 7, 1–18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Flemons, W.W.; Douglas, N.J.; Kuna, S.T.; Rodenstein, D.O.; Wheatley, J. Access to diagnosis and treatment of patients with suspected sleep apnea. Am. J. Respir. Crit. Care Med. 2004, 169, 668–672. [Google Scholar] [CrossRef] [PubMed]



| Variable | Mean ± SD/n (%) | |
|---|---|---|
| Demography | Number of male | 104 (78.8%) |
| Age (years) | 50.5 ± 13.4 | |
| BMI (kg/m2) | 27.8 ± 4.2 | |
| Number of obesity | 69 (52.3%) | |
| NC (cm) | 39.0 ± 3.8 | |
| WC (cm) | 96.0 ± 11.6 | |
| Polysomnography | AHI | 39.5 ± 28.5 |
| Number of severe OSAS | 70 (53.0%) | |
| SpO2nadir (%) | 79.2 ± 9.7 | |
| SpO2mean (%) | 93.1 ± 3.8 | |
| Sleep stage N1 (%) | 26.7 ± 19.1 | |
| Sleep stage N2 (%) | 52.4 ± 16.4 | |
| Sleep stage N3 (%) | 8.7 ± 9.5 | |
| Sleep stage REM (%) | 11.5 ± 6.5 | |
| TRT (min) | 367.1 ± 14.7 | |
| TST (min) | 317.1 ± 37.7 | |
| SE (%) | 86.3 ± 9.7 | |
| Questionnaire | Number of screened ADHD | 60 (45.5%) |
| PSQI | 9.2 ± 4.2 | |
| Number of PSQI > 5 | 104 (78.8%) | |
| PCS | 47.4 ± 9.0 | |
| Number of PCS < 50 | 73 (55.3%) | |
| MCS | 43.2 ± 12.0 | |
| Number of MCS < 50 | 89 (67.4%) | |
| ESS | 10.3 ± 5.3 | |
| Number of ESS > 10 | 62 (47.0%) |
| Three-Way Factor | PSQI | PCS | MCS | ESS |
|---|---|---|---|---|
| A, B, S | A, S | - | A | A, B |
| A, B, O | A | O | A | A, O |
| A, O, S | A, S | - | A | A∩O |
| B, O, S | - | O | - | - |
| Significant factor | A, S | O | A | B, A∩O |
| PSQI | PCS | MCS | ESS | |
|---|---|---|---|---|
| Age (year) | 0.231 | 0.1130 | 0.001 * | 0.544 |
| NC (cm) | 0.280 | 0.067 | 0.406 | 0.588 |
| WC (cm) | 0.114 | 0.034 * | 0.128 | 0.579 |
| SpO2nadir (%) | 0.198 | 0.616 | 0.941 | 0.065 |
| SpO2mean (%) | 0.916 | 0.288 | 0.833 | 0.047 * |
| Stage N1(%) | 0.009 * | 0.224 | 0.001 * | 0.814 |
| Stage N2 (%) | 0.127 | 0.482 | 0.002 * | 0.653 |
| Stage N3 (%) | 0.000 * | 0.568 | 0.067 | 0.839 |
| REM (%) | 0.472 | 0.031 * | 0.561 | 0.772 |
| SE (%) | 0.553 | 0.685 | 0.134 | 0.074 |
| Main Effect | |||
|---|---|---|---|
| Outcome | Factors | Odds Ratio (95% CI) | p-Value |
| PSQI > 5 | Screened ADHD vs. non-screened ADHD | 4.126 (1.490–11.423) | 0.006 * |
| Stage N1 (per 1% increase) | 0.985 (0.962–1.008) | 0.208 | |
| Stage N3 (per 1% increase) | 1.077 (1.000–1.160) | 0.049 * | |
| PSQI > 5 | Female vs. male | 0.674 (0.204–2.224) | 0.518 |
| Stage N1 (per 1% increase) | 0.982 (0.959–1.006) | 0.137 | |
| Stage N3 (per 1% increase) | 1.072 (0.998–1.152) | 0.056 | |
| PCS < 50 | Severe OSAS vs. normal-moderate OSAS | 1.948 (0.842–4.508) | 0.119 |
| WC (per 1cm increase) | 1.016 (0.979–1.054) | 0.411 | |
| REM (per 1% increase) | 0.949 (0.897–1.005) | 0.075 | |
| MCS < 50 | Screened ADHD vs. non-screened ADHD | 5.873 (2.262–15.251) | 0.000 * |
| Age (per 1 year increase) | 0.971 (0.940–1.003) | 0.078 | |
| Stage N1 (per 1% increase) | 0.974 (0.943–1.006) | 0.105 | |
| Stage N2 (per 1% increase) | 1.010 (0.974–1.047) | 0.589 | |
| ESS > 10 | Obesity vs. non-obesity | 1.662 (0.799–3.460) | 0.174 |
| SpO2mean (per 1% increase) | 0.922 (0.830–1.025) | 0.132 | |
| Simple main effect | |||
| Outcome | Factors | Odds ratio (95% CI) | p-value |
| ESS > 10 | Severe OSAS vs. normal-moderate OSAS | 1.215 (0.518–2.846) | 0.655 |
| Screened ADHD vs. non-screened ADHD | 3.648 (1.738–7.657) | 0.001 * | |
| SpO2mean (per 1% increase) | 0.909 (0.808–1.024) | 0.116 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, Y.-H.; Wu, M.-F.; Wen, C.-Y.; Chang, S.-P.; Lin, C.-Y.; Chen, Y.-C.; Lin, C.-C.; Chen, H.-C.; Huang, W.-C.; Chang, K.-M. Interactions between Obstructive Sleep Apnea Syndrome Severity, Obesity, Sex Difference and Attention-Deficit/Hyperactivity Disorder on Health-Related Quality of Life: A Non-Interventional Prospective Observational Study. Biomedicines 2022, 10, 1576. https://doi.org/10.3390/biomedicines10071576
Chen Y-H, Wu M-F, Wen C-Y, Chang S-P, Lin C-Y, Chen Y-C, Lin C-C, Chen H-C, Huang W-C, Chang K-M. Interactions between Obstructive Sleep Apnea Syndrome Severity, Obesity, Sex Difference and Attention-Deficit/Hyperactivity Disorder on Health-Related Quality of Life: A Non-Interventional Prospective Observational Study. Biomedicines. 2022; 10(7):1576. https://doi.org/10.3390/biomedicines10071576
Chicago/Turabian StyleChen, Yu-Hsuan, Ming-Feng Wu, Chih-Yu Wen, Shih-Pei Chang, Ching-Yi Lin, Yi-Chan Chen, Ching-Cheng Lin, Hui-Chen Chen, Wei-Chang Huang, and Kai-Ming Chang. 2022. "Interactions between Obstructive Sleep Apnea Syndrome Severity, Obesity, Sex Difference and Attention-Deficit/Hyperactivity Disorder on Health-Related Quality of Life: A Non-Interventional Prospective Observational Study" Biomedicines 10, no. 7: 1576. https://doi.org/10.3390/biomedicines10071576