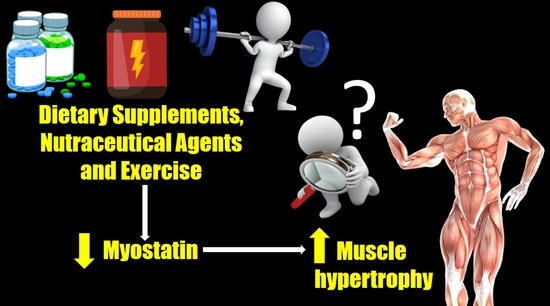
The Effects of Dietary Supplements, Nutraceutical Agents, and Physical Exercise on Myostatin Levels: Hope or Hype?
Abstract
:1. Introduction
2. Mechanisms
3. Laboratory Levels
General Considerations
4. Functional Foods and Supplements
4.1. Proteins, Amino Acids, and Derivatives
4.1.1. Egg
4.1.2. Milk
4.1.3. Whey Protein
4.1.4. Amino Acids
4.1.5. HMB
4.1.6. Creatine
4.2. Non-Protein Supplements
4.2.1. Brown Seaweed
4.2.2. Spirulina
4.2.3. Cocoa
4.2.4. Epicatechins
4.2.5. Vitamin D
4.3. General Considerations
5. Physical Exercise
5.1. Resistance Training
5.2. Concurrent Training
5.3. Clinical Populations
5.4. General Considerations
6. Pharmacological Agents
6.1. Specific Myostatin-Blocking Drugs
6.2. Testosterone
6.3. Growth Hormone
6.4. General Considerations
7. Take-Home Messages
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Suh, J.; Lee, Y.-S. Myostatin Inhibitors: Panacea or Predicament for Musculoskeletal Disorders? J. Bone Metab. 2020, 27, 151–165. [Google Scholar] [CrossRef] [PubMed]
- Joulia-Ekaza, D.; Cabello, G. Myostatin regulation of muscle development: Molecular basis, natural mutations, physiopathological aspects. Exp. Cell Res. 2006, 312, 3458. [Google Scholar] [CrossRef]
- Benny Klimek, M.E.; Aydogdu, T.; Link, M.J.; Pons, M.; Koniaris, L.G.; Zimmers, T.A. Acute inhibition of myostatin-family proteins preserves skeletal muscle in mouse models of cancer cachexia. Biochem. Biophys. Res. Commun. 2010, 391, 1548–1554. [Google Scholar] [CrossRef] [PubMed]
- Gallot, Y.S.; Durieux, A.-C.; Castells, J.; Desgeorges, M.M.; Vernus, B.; Plantureux, L.; Rémond, D.; Jahnke, V.E.; Lefai, E.; Dardevet, D.; et al. Myostatin Gene Inactivation Prevents Skeletal Muscle Wasting in Cancer. Cancer Res. 2014, 74, 7344–7356. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McPherron, A.C.; Lawler, A.M.; Lee, S.J. Regulation of skeletal muscle mass in mice by a new TGF-beta superfamily member. Nature 1997, 387, 83–90. [Google Scholar] [CrossRef] [PubMed]
- Matsakas, A.; Diel, P. The Growth Factor Myostatin, a Key Regulator in Skeletal Muscle Growth and Homeostasis. Int. J. Sport. Med. 2005, 26, 83–89. [Google Scholar] [CrossRef] [PubMed]
- Rodgers, B.D.; Garikipati, D.K. Clinical, Agricultural, and Evolutionary Biology of Myostatin: A Comparative Review. Endocr. Rev. 2008, 29, 513–534. [Google Scholar] [CrossRef]
- Leung, D.G.; Carrino, J.A.; Wagner, K.R.; Jacobs, M.A. Whole-body magnetic resonance imaging evaluation of facioscapulohumeral muscular dystrophy. Muscle Nerve 2015, 52, 512–520. [Google Scholar] [CrossRef] [Green Version]
- Palsgaard, J.; Brøns, C.; Friedrichsen, M.; Domínguez, H.; Jensen, M.; Storgaard, H.; Spohr, C.; Torp-Pedersen, C.; Borup, R.; De Meyts, P.; et al. Gene Expression in Skeletal Muscle Biopsies from People with Type 2 Diabetes and Relatives: Differential Regulation of Insulin Signaling Pathways. PLoS ONE 2009, 4, e6575. [Google Scholar] [CrossRef] [Green Version]
- Eilers, W.; Chambers, D.; Cleasby, M.; Foster, K. Local myostatin inhibition improves skeletal muscle glucose uptake in insulin-resistant high-fat diet-fed mice. Am. J. Physiol. Metab. 2020, 319, E163–E174. [Google Scholar] [CrossRef]
- Dong, J.; Dong, Y.; Chen, F.; Mitch, W.; Zhang, L. Inhibition of myostatin in mice improves insulin sensitivity via irisin-mediated cross talk between muscle and adipose tissues. Int. J. Obes. 2015, 40, 434–442. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Santos, H.O.; Earnest, C.P.; Tinsley, G.M.; Izidoro, L.F.M.; Macedo, R.C.O. Small dense low-density lipoprotein-cholesterol (sdLDL-C): Analysis, effects on cardiovascular endpoints and dietary strategies. Prog. Cardiovasc. Dis. 2020, 63, 503–509. [Google Scholar] [CrossRef] [PubMed]
- James, P.A.; Oparil, S.; Carter, B.L.; Cushman, W.C.; Dennison-Himmelfarb, C.; Handler, J.; Lackland, D.T.; LeFevre, M.L.; MacKenzie, T.D.; Ogedegbe, O.; et al. 2014 evidence-based guideline for the management of high blood pressure in adults: Report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014, 311, 507–520. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sarwar, N.; Gao, P.; Seshasai, S.R.; Gobin, R.; Kaptoge, S.; Di Angelantonio, E.; Ingelsson, E.; Lawlor, D.A.; Selvin, E.; Stampfer, M.; et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: A collaborative meta-analysis of 102 prospective studies. Lancet 2010, 375, 2215–2222. [Google Scholar] [PubMed] [Green Version]
- Rizzuti, A.; Stocker, G.; Santos, H.O. Exploring the Role of Testosterone Replacement Therapy in Benign Prostatic Hyperplasia and Prostate Cancer: A Review of Safety. Uro 2022, 2, 30–39. [Google Scholar] [CrossRef]
- Santos, H.O.; Cadegiani, F.A.; Forbes, S.C. Nonpharmacological Interventions for the Management of Testosterone and Sperm Parameters: A Scoping Review. Clin. Ther. 2022, 44, 1129–1149. [Google Scholar] [CrossRef] [PubMed]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E., Jr.; Collins, K.J.; Dennison Himmelfarb, C.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018, 71, 1269–1324. [Google Scholar]
- Pippitt, K.; Li, M.; Gurgle, H. Diabetes Mellitus: Screening and Diagnosis. Am. Fam. Physician 2016, 93, 103–109. [Google Scholar] [PubMed]
- A Study to Investigate the Safety and Efficacy of RO7204239 in Combination with Risdiplam (RO7034067) in Ambulatory Children with Spinal Muscular Atrophy. Available online: https://clinicaltrials.gov/ct2/show/NCT05115110 (accessed on 15 November 2022).
- Efficacy and Safety of Apitegromab in Patients with Later-Onset Spinal Muscular Atrophy Treated with Nusinersen or Risdiplam (SAPPHIRE). Available online: https://clinicaltrials.gov/ct2/show/NCT05156320 (accessed on 15 November 2022).
- A Study to Evaluate the Efficacy and Safety of Taldefgrobep Alfa in Participants with Spinal Muscular Atrophy (RESILIENT). Available online: https://clinicaltrials.gov/ct2/show/NCT05337553 (accessed on 15 November 2022).
- Paoli, A.; Pacelli, Q.F.; Neri, M.; Toniolo, L.; Cancellara, P.; Canato, M.; Moro, T.; Quadrelli, M.; Morra, A.; Faggian, D.; et al. Protein Supplementation Increases Postexercise Plasma Myostatin Concentration After 8 Weeks of Resistance Training in Young Physically Active Subjects. J. Med. Food 2015, 18, 137–143. [Google Scholar] [CrossRef] [Green Version]
- Amasene, M.; Cadenas-Sanchez, C.; Echeverria, I.; Sanz, B.; Alonso, C.; Tobalina, I.; Irazusta, J.; Labayen, I.; Besga, A. Effects of Resistance Training Intervention along with Leucine-Enriched Whey Protein Supplementation on Sarcopenia and Frailty in Post-Hospitalized Older Adults: Preliminary Findings of a Randomized Controlled Trial. J. Clin. Med. 2021, 11, 97. [Google Scholar] [CrossRef]
- Pourabbas, M.; Bagheri, R.; Moghadam, B.H.; Willoughby, D.; Candow, D.; Elliott, B.; Forbes, S.; Ashtary-Larky, D.; Eskandari, M.; Wong, A.; et al. Strategic Ingestion of High-Protein Dairy Milk during a Resistance Training Program Increases Lean Mass, Strength, and Power in Trained Young Males. Nutrients 2021, 13, 948. [Google Scholar] [CrossRef] [PubMed]
- Argiles, J.M.; Orpí, M.; Busquets, S.; López-Soriano, F.J. Myostatin: More than just a regulator of muscle mass. Drug Discov. Today 2012, 17, 702–709. [Google Scholar] [CrossRef] [PubMed]
- McCroskery, S.; Thomas, M.; Maxwell, L.; Sharma, M.; Kambadur, R. Myostatin negatively regulates satellite cell activation and self-renewal. J. Cell Biol. 2003, 162, 1135–1147. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goodman, C.A.; Hornberger, T.A. New roles for Smad signaling and phosphatidic acid in the regulation of skeletal muscle mass. F1000Prime Rep. 2014, 6, 20. [Google Scholar] [CrossRef]
- Allen, D.L.; Unterman, T.G. Regulation of myostatin expression and myoblast differentiation by FoxO and SMAD transcription factors. Am. J. Physiol. Physiol. 2007, 292, C188–C199. [Google Scholar] [CrossRef]
- McFarlane, C.; Plummer, E.; Thomas, M.; Hennebry, A.; Ashby, M.; Ling, N.; Smith, H.; Sharma, M.; Kambadur, R. Myostatin induces cachexia by activating the ubiquitin proteolytic system through an NF-κB-independent, FoxO1-dependent mechanism. J. Cell. Physiol. 2006, 209, 501–514. [Google Scholar] [CrossRef]
- Szulc, P.; Schoppet, M.; Goettsch, C.; Rauner, M.; Dschietzig, T.B.; Chapurlat, R.; Hofbauer, L.C. Endocrine and Clinical Correlates of Myostatin Serum Concentration in Men—The STRAMBO Study. J. Clin. Endocrinol. Metab. 2012, 97, 3700–3708. [Google Scholar] [CrossRef]
- Choi, S.; Lee, M.; Kang, D.-H.; Ko, G.; Lim, H.-S.; Yu, B.; Park, M.; Kim, J.; Kim, C.-H.; Hwang, S.; et al. Myostatin/Appendicular Skeletal Muscle Mass (ASM) Ratio, Not Myostatin, Is Associated with Low Handgrip Strength in Community-Dwelling Older Women. Int. J. Environ. Res. Public Healh 2021, 18, 7344. [Google Scholar] [CrossRef]
- Lakshman, K.M.; Bhasin, S.; Corcoran, C.; Collins-Racie, L.A.; Tchistiakova, L.; Forlow, S.B.; Ledger, K.S.; Burczynski, M.E.; Dorner, A.J.; LaVallie, E.R. Measurement of myostatin concentrations in human serum: Circulating concentrations in young and older men and effects of testosterone administration. Mol. Cell. Endocrinol. 2009, 302, 26–32. [Google Scholar] [CrossRef]
- Bojar, I.; Mlak, R.; Homa-Mlak, I.; Prendecka, M.; Owoc, A.; Małecka-Massalska, T. Association between myostatin serum concentration and body fat level in peri- and postmenopausal women. Arch. Med. Sci. 2021, 18, 365–375. [Google Scholar] [CrossRef]
- Miyamoto, Y.; Hanna, D.L.; Zhang, W.; Baba, H.; Lenz, H.J. Molecular Pathways: Cachexia Signaling-A Targeted Approach to Cancer Treatment. Clin. Cancer Res. 2016, 22, 3999–4004. [Google Scholar] [CrossRef] [PubMed]
- Huang, P.-Y.; Tsai, J.-P.; Chen, Y.-C.; Lee, M.-C.; Hsu, B.-G. The Correlation of Serum Myostatin Levels with Gait Speed in Kidney Transplantation Recipients. Int. J. Environ. Res. Public Health 2022, 19, 465. [Google Scholar] [CrossRef] [PubMed]
- Furihata, T.; Kinugawa, S.; Fukushima, A.; Takada, S.; Homma, T.; Masaki, Y.; Abe, T.; Yokota, T.; Oba, K.; Okita, K.; et al. Serum myostatin levels are independently associated with skeletal muscle wasting in patients with heart failure. Int. J. Cardiol. 2016, 220, 483–487. [Google Scholar] [CrossRef] [Green Version]
- Han, D.-S.; Chu-Su, Y.; Chiang, C.-K.; Tseng, F.-Y.; Tseng, P.-H.; Chen, C.-L.; Wu, K.-D.; Yang, W.-S. Serum Myostatin Is Reduced in Individuals with Metabolic Syndrome. PLoS ONE 2014, 9, e108230. [Google Scholar] [CrossRef] [PubMed]
- de Sordi, C.M.; Dos Reis-Neto, E.T.; Keppeke, G.D.; Shinjo, S.K.; Sato, E.I. Serum Myostatin and Follistatin Levels in Patients With Dermatomyositis and Polymyositis. JCR J. Clin. Rheumatol. 2022, 28, 33–37. [Google Scholar] [CrossRef]
- Koyun, D.; Nergizoglu, G.; Kir, K.M. Evaluation of the relationship between muscle mass and serum myostatin levels in chronic hemodialysis patients. Saudi J. Kidney Dis. Transplant. 2018, 29, 809–815. [Google Scholar] [CrossRef]
- Delanaye, P.; Bataille, S.; Quinonez, K.; Buckinx, F.; Warling, X.; Krzesinski, J.M.; Pottel, H.; Burtey, S.; Bruyère, O.; Cavalier, E. Myostatin and Insulin-Like Growth Factor 1 Are Biomarkers of Muscle Strength, Muscle Mass, and Mortality in Patients on Hemodialysis. J. Ren. Nutr. 2019, 29, 511–520. [Google Scholar] [CrossRef]
- Han, D.-S.; Chen, Y.-M.; Lin, S.-Y.; Chang, H.-H.; Huang, T.-M.; Chi, Y.-C.; Yang, W.-S. Serum myostatin levels and grip strength in normal subjects and patients on maintenance haemodialysis. Clin. Endocrinol. 2011, 75, 857–863. [Google Scholar] [CrossRef]
- Yamada, S.; Tsuruya, K.; Yoshida, H.; Tokumoto, M.; Ueki, K.; Ooboshi, H.; Kitazono, T. Factors Associated with the Serum Myostatin Level in Patients Undergoing Peritoneal Dialysis: Potential Effects of Skeletal Muscle Mass and Vitamin D Receptor Activator Use. Calcif. Tissue Res. 2016, 99, 13–22. [Google Scholar] [CrossRef]
- Nishikawa, H.; Enomoto, H.; Ishii, A.; Iwata, Y.; Miyamoto, Y.; Ishii, N.; Yuri, Y.; Hasegawa, K.; Nakano, C.; Nishimura, T.; et al. Elevated serum myostatin level is associated with worse survival in patients with liver cirrhosis. J. Cachex- Sarcopenia Muscle 2017, 8, 915–925. [Google Scholar] [CrossRef]
- Alexopoulos, T.; Vasilieva, L.; Kontogianni, M.D.; Tenta, R.; Georgiou, A.; Stroumpouli, E.; Mani, I.; Alexopoulou, A. Myostatin in combination with creatine phosphokinase or albumin may differentiate patients with cirrhosis and sarcopenia. Am. J. Physiol. Liver Physiol. 2021, 321, G543–G551. [Google Scholar] [CrossRef] [PubMed]
- Skladany, L.; Koller, T.; Molcan, P.; Vnencakova, J.; Zilincan, M.; Jancekova, D.; Kukla, M. Prognostic usefulness of serum myostatin in advanced chronic liver disease: Its relation to gender and correlation with inflammatory status. J. Physiol. Pharmacol. Off. J. Pol. Physiol. Soc. 2019, 70, 357–368. [Google Scholar] [CrossRef]
- Shamseddeen, H.; Madathanapalli, A.; Are, V.S.; Shah, V.H.; Sanyal, A.J.; Tang, Q.; Liang, T.; Gelow, K.; Zimmers, T.A.; Chalasani, N.; et al. Changes in Serum Myostatin Levels in Alcoholic Hepatitis Correlate with Improvement in MELD. Am. J. Dig. Dis. 2020, 66, 3062–3073. [Google Scholar] [CrossRef] [PubMed]
- Efthymiadou, A.; Vasilakis, I.-A.; Giannakopoulos, A.; Chrysis, D. Myostatin serum levels in children with type 1 diabetes mellitus. Hormones 2021, 20, 777–782. [Google Scholar] [CrossRef]
- Burch, P.M.; Pogoryelova, O.; Palandra, J.; Goldstein, R.; Bennett, D.; Fitz, L.; Guglieri, M.; Bettolo, C.M.; Straub, V.; Evangelista, T.; et al. Reduced serum myostatin concentrations associated with genetic muscle disease progression. J. Neurol. 2017, 264, 541–553. [Google Scholar] [CrossRef]
- Ju, C.-R.; Chen, R.-C. Serum myostatin levels and skeletal muscle wasting in chronic obstructive pulmonary disease. Respir. Med. 2012, 106, 102–108. [Google Scholar] [CrossRef] [Green Version]
- Blomstrand, E.; Eliasson, J.; Karlsson, H.; Köhnke, R. Branched-Chain Amino Acids Activate Key Enzymes in Protein Synthesis after Physical Exercise. J. Nutr. 2006, 136 (Suppl. 1), 269S–273S. [Google Scholar] [CrossRef] [Green Version]
- Li, R.; Ferreira, M.P.; Cooke, M.B.; La Bounty, P.; Campbell, B.; Greenwood, M.; Willoughby, D.S.; Kreider, R.B. Co-ingestion of carbohydrate with branched-chain amino acids or l-leucine does not preferentially increase serum IGF-1 and expression of myogenic-related genes in response to a single bout of resistance exercise. Amino Acids 2015, 47, 1203–1213. [Google Scholar] [CrossRef] [Green Version]
- Bagheri, R.; Moghadam, B.H.; Jo, E.; Tinsley, G.M.; Stratton, M.T.; Ashtary-Larky, D.; Eskandari, M.; Wong, A. Comparison of whole egg v. egg white ingestion during 12 weeks of resistance training on skeletal muscle regulatory markers in resistance-trained men. Br. J. Nutr. 2020, 124, 1035–1043. [Google Scholar] [CrossRef] [PubMed]
- Bagheri, R.; Forbes, S.C.; Candow, D.G.; Wong, A. Effects of branched-chain amino acid supplementation and resistance training in postmenopausal women. Exp. Gerontol. 2020, 144, 111185. [Google Scholar] [CrossRef]
- Saremi, A.; Gharakhanloo, R.; Sharghi, S.; Gharaati, M.; Larijani, B.; Omidfar, K. Effects of oral creatine and resistance training on serum myostatin and GASP-1. Mol. Cell. Endocrinol. 2010, 317, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Deldicque, L.; Atherton, P.; Patel, R.; Theisen, D.; Nielens, H.; Rennie, M.J.; Francaux, M. Effects of resistance exercise with and without creatine supplementation on gene expression and cell signaling in human skeletal muscle. J. Appl. Physiol. 2008, 104, 371–378. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsien, C.; Davuluri, G.; Singh, D.; Allawy, A.; Have, G.A.T.; Thapaliya, S.; Schulze, J.M.; Barnes, D.; McCullough, A.J.; Engelen, M.P.; et al. Metabolic and molecular responses to leucine-enriched branched chain amino acid supplementation in the skeletal muscle of alcoholic cirrhosis. Hepatology 2015, 61, 2018–2029. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olveira, G.; Olveira, C.; Doña, E.; Palenque, F.J.; Porras, N.; Dorado, A.; Godoy, A.M.; Rubio-Martínez, E.; Rojo-Martínez, G.; Martín-Valero, R. Oral supplement enriched in HMB combined with pulmonary rehabilitation improves body composition and health related quality of life in patients with bronchiectasis (Prospective, Randomised Study). Clin. Nutr. 2015, 35, 1015–1022. [Google Scholar] [CrossRef]
- Dirks, M.L.; Wall, B.T.; Nilwik, R.; Weerts, D.H.; Verdijk, L.B.; van Loon, L.J. Skeletal Muscle Disuse Atrophy Is Not Attenuated by Dietary Protein Supplementation in Healthy Older Men. J. Nutr. 2014, 144, 1196–1203. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Constantin, D.; Menon, M.K.; Houchen-Wolloff, L.; Morgan, M.D.; Singh, S.J.; Greenhaff, P.; Steiner, M. Skeletal muscle molecular responses to resistance training and dietary supplementation in COPD. Thorax 2013, 68, 625–633. [Google Scholar] [CrossRef] [Green Version]
- Teixeira, F.J.; Santos, H.O.; Howell, S.L.; Pimentel, G.D. Whey protein in cancer therapy: A narrative review. Pharmacol. Res. 2019, 144, 245–256. [Google Scholar] [CrossRef]
- Retamales, A.; Zuloaga, R.; Valenzuela, C.; Gallardo-Escarate, C.; Molina, A.; Valdés, J. Insulin-like growth factor-1 suppresses the Myostatin signaling pathway during myogenic differentiation. Biochem. Biophys. Res. Commun. 2015, 464, 596–602. [Google Scholar] [CrossRef]
- Santos, H.O.; Gomes, G.K.; Schoenfeld, B.J.; de Oliveira, E.P. The Effect of Whole Egg Intake on Muscle Mass: Are the Yolk and Its Nutrients Important? Int. J. Sport Nutr. Exerc. Metab. 2021, 31, 514–521. [Google Scholar] [CrossRef]
- Santos, H.O. Update of the Impact of Consumption of Whole Chicken Eggs on the Lipid Profile: To What Extent are They Impacting? Arq. Bras. Cardiol. 2018, 110, 585–587. [Google Scholar] [CrossRef]
- Wette, S.G.; Birch, N.P.; Soop, M.; Zügel, M.; Murphy, R.M.; Lamb, G.D.; Smith, H.K. Expression of titin-linked putative mechanosensing proteins in skeletal muscle after power resistance exercise in resistance-trained men. J. Appl. Physiol. 2021, 130, 545–561. [Google Scholar] [CrossRef]
- Hoffman, J.R.; Falvo, M.J. Protein-Which is Best? J. Sport. Sci. Med. 2004, 3, 118–130. [Google Scholar]
- Gorissen, S.H.M.; Crombag, J.J.R.; Senden, J.M.G.; Waterval, W.A.H.; Bierau, J.; Verdijk, L.B.; van Loon, L.J.C. Protein content and amino acid composition of commercially available plant-based protein isolates. Amino Acids 2018, 50, 1685–1695. [Google Scholar] [CrossRef] [Green Version]
- Hulmi, J.J.; Kovanen, V.; Lisko, I.; Selänne, H.; Mero, A.A. The effects of whey protein on myostatin and cell cycle-related gene expression responses to a single heavy resistance exercise bout in trained older men. Eur. J. Appl. Physiol. 2007, 102, 205–213. [Google Scholar] [CrossRef]
- Hulmi, J.J.; Kovanen, V.; Selänne, H.; Kraemer, W.J.; Häkkinen, K.; Mero, A.A. Acute and long-term effects of resistance exercise with or without protein ingestion on muscle hypertrophy and gene expression. Amino Acids 2008, 37, 297–308. [Google Scholar] [CrossRef] [PubMed]
- Dalbo, V.J.; Roberts, M.D.; Hassell, S.; Kerksick, C.M. Effects of pre-exercise feeding on serum hormone concentrations and biomarkers of myostatin and ubiquitin proteasome pathway activity. Eur. J. Nutr. 2012, 52, 477–487. [Google Scholar] [CrossRef] [PubMed]
- de Sire, A.; Baricich, A.; Renò, F.; Cisari, C.; Fusco, N.; Invernizzi, M. Myostatin as a potential biomarker to monitor sarcopenia in hip fracture patients undergoing a multidisciplinary rehabilitation and nutritional treatment: A preliminary study. Aging Clin. Exp. Res. 2020, 32, 959–962. [Google Scholar] [CrossRef] [PubMed]
- Wilson, G.J.; Wilson, J.M.; Manninen, A.H. Effects of beta-hydroxy-beta-methylbutyrate (HMB) on exercise performance and body composition across varying levels of age, sex, and training experience: A review. Nutr. Metab. 2008, 5, 1. [Google Scholar] [CrossRef] [Green Version]
- Delpino, F.M.; Figueiredo, L.M.; Forbes, S.C.; Candow, D.G.; Santos, H.O. Influence of age, sex, and type of exercise on the efficacy of creatine supplementation on lean body mass: A systematic review and meta-analysis of randomized clinical trials. Nutrition 2022, 103–104, 111791. [Google Scholar] [CrossRef]
- dos Santos, E.E.P.; de Araújo, R.C.; Candow, D.G.; Forbes, S.C.; Guijo, J.A.; de Almeida Santana, C.C.; do Prado, W.L.; Botero, J.P. Efficacy of Creatine Supplementation Combined with Resistance Training on Muscle Strength and Muscle Mass in Older Females: A Systematic Review and Meta-Analysis. Nutrients 2021, 13, 3757. [Google Scholar] [CrossRef]
- Chen, L.; Liu, R.; He, X.; Pei, S.; Li, D. Effects of brown seaweed polyphenols, a class of phlorotannins, on metabolic disorders via regulation of fat function. Food Funct. 2021, 12, 2378–2388. [Google Scholar] [CrossRef] [PubMed]
- Willoughby, D.S. Effects of an Alleged Myostatin-Binding Supplement and Heavy Resistance Training on Serum Myostatin, Muscle Strength and Mass, and Body Composition. Int. J. Sport Nutr. Exerc. Metab. 2004, 14, 461–472. [Google Scholar] [CrossRef] [PubMed]
- Karkos, P.D.; Leong, S.C.; Karkos, C.D.; Sivaji, N.; Assimakopoulos, D.A. Spirulina in clinical practice: Evidence-based human applications. Evid. Based Complement. Alternat. Med. 2011, 2011, 531053. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gutiérrez-Salmeán, G.; Fabila-Castillo, L.; Chamorro-Cevallos, G. Nutritional and toxicological aspects of Spirulina (Arthrospira). Nutr. Hosp. 2015, 32, 34–40. [Google Scholar]
- Santos, H.O.; Price, J.C.; Bueno, A.A. Beyond Fish Oil Supplementation: The Effects of Alternative Plant Sources of Omega-3 Polyunsaturated Fatty Acids upon Lipid Indexes and Cardiometabolic Biomarkers—An Overview. Nutrients 2020, 12, 3159. [Google Scholar] [CrossRef]
- Bagheri, R.; Negaresh, R.; Motevalli, M.S.; Wong, A.; Ashtary-Larky, D.; Kargarfard, M.; Rashidlamir, A. Spirulina supplementation during gradual weight loss in competitive wrestlers. Br. J. Nutr. 2021, 127, 248–256. [Google Scholar] [CrossRef]
- Santos, H.O.; Macedo, R.C. Cocoa-induced (Theobroma cacao) effects on cardiovascular system: HDL modulation pathways. Clin. Nutr. ESPEN 2018, 27, 10–15. [Google Scholar] [CrossRef]
- ngel García-Merino, J.; Moreno-Pérez, D.; de Lucas, B.; Montalvo-Lominchar, M.G.; Muñoz, E.; Sánchez, L.; Naclerio, F.; Herrera-Rocha, K.M.; Moreno-Jiménez, M.R.; Rocha-Guzmán, N.E.; et al. Chronic flavanol-rich cocoa powder supplementation reduces body fat mass in endurance athletes by modifying the follistatin/myostatin ratio and leptin levels. Food Funct. 2020, 11, 3441–3450. [Google Scholar] [CrossRef]
- Zbinden-Foncea, H.; Castro-Sepulveda, M.; Fuentes, J.; Speisky, H. Effect of epicatechin on skeletal muscle. Curr. Med. Chem. 2021, 29, 1110–1123. [Google Scholar] [CrossRef]
- Mafi, F.; Biglari, S.; Afousi, A.G.; Gaeini, A.A. Improvement in Skeletal Muscle Strength and Plasma Levels of Follistatin and Myostatin Induced by an 8-Week Resistance Training and Epicatechin Supplementation in Sarcopenic Older Adults. J. Aging Phys. Act. 2019, 27, 384–391. [Google Scholar] [CrossRef]
- Halfon, M.; Phan, O.; Teta, D. Vitamin D: A Review on Its Effects on Muscle Strength, the Risk of Fall, and Frailty. BioMed Res. Int. 2015, 2015, 953241. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Santos, H.O.; Howell, S.; Nichols, K.; Teixeira, F. Reviewing the Evidence on Vitamin D Supplementation in the Management of Testosterone Status and Its Effects on Male Reproductive System (Testis and Prostate): Mechanistically Dazzling but Clinically Disappointing. Clin. Ther. 2020, 42, e101–e114. [Google Scholar] [CrossRef] [PubMed]
- Beaudart, C.; Buckinx, F.; Rabenda, V.; Gillain, S.; Cavalier, E.; Slomian, J.; Petermans, J.; Reginster, J.-Y.; Bruyère, O. The Effects of Vitamin D on Skeletal Muscle Strength, Muscle Mass, and Muscle Power: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Clin. Endocrinol. Metab. 2014, 99, 4336–4345. [Google Scholar] [CrossRef]
- Gonnelli, S.; Pitinca, M.D.T.; Camarri, S.; Lucani, B.; Franci, B.; Nuti, R.; Caffarelli, C. Pharmacokinetic profile and effect on bone markers and muscle strength of two daily dosage regimens of calcifediol in osteopenic/osteoporotic postmenopausal women. Aging Clin. Exp. Res. 2021, 33, 2539–2547. [Google Scholar] [CrossRef]
- Kim, J.-S.; Cross, J.M.; Bamman, M.M. Impact of resistance loading on myostatin expression and cell cycle regulation in young and older men and women. Am. J. Physiol. Metab. 2005, 288, E1110–E1119. [Google Scholar] [CrossRef]
- Hulmi, J.J.; Ahtiainen, J.P.; Kaasalainen, T.; Pöllänen, E.; Häkkinen, K.; Alen, M.; Selänne, H.; Kovanen, V.; Mero, A.A. Postexercise myostatin and activin IIb mRNA levels: Effects of strength training. Med. Sci. Sport. Exerc. 2007, 39, 289–297. [Google Scholar] [CrossRef]
- Roth, S.; Martel, G.F.; Ferrell, R.E.; Metter, E.J.; Hurley, B.F.; Rogers, M.A. Myostatin Gene Expression is Reduced in Humans with Heavy-Resistance Strength Training: A Brief Communication. Exp. Biol. Med. 2003, 228, 706–709. [Google Scholar] [CrossRef]
- Kim, J.-S.; Petrella, J.K.; Cross, J.M.; Bamman, M.M. Load-mediated downregulation of myostatin mRNA is not sufficient to promote myofiber hypertrophy in humans: A cluster analysis. J. Appl. Physiol. 2007, 103, 1488–1495. [Google Scholar] [CrossRef] [Green Version]
- Jespersen, J.G.; Nedergaard, A.; Andersen, L.L.; Schjerling, P. Myostatin expression during human muscle hypertrophy and subsequent atrophy: Increased myostatin with detraining. Scand. J. Med. Sci. Sport 2011, 21, 215–223. [Google Scholar] [CrossRef]
- Bagheri, R.; Moghadam, B.H.; Church, D.D.; Tinsley, G.; Eskandari, M.; Moghadam, B.H.; Motevalli, M.S.; Baker, J.S.; Robergs, R.A.; Wong, A. The effects of concurrent training order on body composition and serum concentrations of follistatin, myostatin and GDF11 in sarcopenic elderly men. Exp. Gerontol. 2020, 133, 110869. [Google Scholar] [CrossRef]
- Jones, S.W.; Hill, R.J.; Krasney, P.A.; O’Conner, B.; Peirce, N.; Greenhaff, P. Disuse atrophy and exercise rehabilitation in humans profoundly affects the expression of genes associated with the regulation of skeletal muscle mass. FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol. 2004, 18, 1025–1027. [Google Scholar] [CrossRef] [PubMed]
- Diel, P.; Schiffer, T.; Geisler, S.; Hertrampf, T.; Mosler, S.; Schulz, S.; Wintgens, K.F.; Adler, M. Analysis of the effects of androgens and training on myostatin propeptide and follistatin concentrations in blood and skeletal muscle using highly sensitive Immuno PCR. Mol. Cell. Endocrinol. 2010, 330, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Lewis, M.I.; Fournier, M.; Storer, T.W.; Bhasin, S.; Porszasz, J.; Ren, S.-G.; Da, X.; Casaburi, R. Skeletal muscle adaptations to testosterone and resistance training in men with COPD. J. Appl. Physiol. 2007, 103, 1299–1310. [Google Scholar] [CrossRef] [PubMed]
- Schoenfeld, B.J.; Contreras, B.; Krieger, J.; Grgic, J.; Delcastillo, K.; Belliard, R.; Alto, A. Resistance Training Volume Enhances Muscle Hypertrophy but Not Strength in Trained Men. Med. Sci. Sport. Exerc. 2019, 51, 94–103. [Google Scholar] [CrossRef] [PubMed]
- Krzysztofik, M.; Wilk, M.; Wojdała, G.; Gołaś, A. Maximizing Muscle Hypertrophy: A Systematic Review of Advanced Resistance Training Techniques and Methods. Int. J. Environ. Res. Public Health 2019, 16, 4897. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, Z.; Chen, X.; Chen, D. Myostatin: A novel insight into its role in metabolism, signal pathways, and expression regulation. Cell. Signal. 2011, 23, 1441–1446. [Google Scholar] [CrossRef]
- Whittemore, L.-A.; Song, K.; Li, X.; Aghajanian, J.; Davies, M.; Girgenrath, S.; Hill, J.J.; Jalenak, M.; Kelley, P.; Knight, A.; et al. Inhibition of myostatin in adult mice increases skeletal muscle mass and strength. Biochem. Biophys. Res. Commun. 2002, 300, 965–971. [Google Scholar] [CrossRef]
- Jayasena, C.N.; Anderson, R.A.; Llahana, S.; Barth, J.H.; MacKenzie, F.; Wilkes, S.; Smith, N.; Sooriakumaran, P.; Minhas, S.; Wu, F.C.W.; et al. Society for Endocrinology guidelines for testosterone replacement therapy in male hypogonadism. Clin. Endocrinol. 2021, 96, 200–219. [Google Scholar] [CrossRef]
- Santos, H.O.; Haluch, C.E.F. Downregulation of Androgen Receptors upon Anabolic-Androgenic Steroids: A Cause or a Flawed Hypothesis of the Muscle-Building Plateau? Muscles 2022, 1, 92–101. [Google Scholar] [CrossRef]
- Ghanim, H.; Dhindsa, S.; Batra, M.; Green, K.; Abuaysheh, S.; Kuhadiya, N.D.; Makdissi, A.; Chaudhuri, A.; Dandona, P. Effect of Testosterone on FGF2, MRF4, and Myostatin in Hypogonadotropic Hypogonadism: Relevance to Muscle Growth. J. Clin. Endocrinol. Metab. 2019, 104, 2094–2102. [Google Scholar] [CrossRef]
- Kvorning, T.; Andersen, M.; Brixen, K.; Schjerling, P.; Suetta, C.; Madsen, K. Suppression of testosterone does not blunt mRNA expression of myoD, myogenin, IGF, myostatin or androgen receptor post strength training in humans. J. Physiol. 2007, 578, 579–593. [Google Scholar] [CrossRef]
- Tritos, N.A.; Klibanski, A. Effects of Growth Hormone on Bone. Prog. Mol. Biol. Transl. Sci. 2016, 138, 193–211. [Google Scholar] [PubMed]
- Velloso, C.P. Regulation of muscle mass by growth hormone and IGF-I. Br. J. Pharmacol. 2008, 154, 557–568. [Google Scholar] [CrossRef] [PubMed]
- Xie, M.; Zhong, Y.; Xue, Q.; Wu, M.; Deng, X.; Santos, H.O.; Tan, S.C.; Kord-Varkaneh, H.; Jiao, P. Impact of dehydroepianrosterone (DHEA) supplementation on serum levels of insulin-like growth factor 1 (IGF-1): A dose-response meta-analysis of randomized controlled trials. Exp. Gerontol. 2020, 136, 110949. [Google Scholar] [CrossRef] [PubMed]
- Paul, R.G.; McMahon, C.D.; Elston, M.S.; Conaglen, J.V. GH replacement titrated to serum IGF-1 does not reduce concentrations of myostatin in blood or skeletal muscle. Growth Horm. IGF Res. 2019, 44, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Thomas, S.G.; Asa, S.; Gonzalez-Cadavid, N.; Bhasin, S.; Ezzat, S. Myostatin Is a Skeletal Muscle Target of Growth Hormone Anabolic Action. J. Clin. Endocrinol. Metab. 2003, 88, 5490–5496. [Google Scholar] [CrossRef] [Green Version]
- Cesari, M.; Bernabei, R.; Vellas, B.; Fielding, R.; Rooks, D.; Azzolino, D.; Mariani, J.; Oliva, A.; Bhasin, S.; Rolland, Y. Challenges in the Development of Drugs for Sarcopenia and Frailty-Report from the International Conference on Frailty and Sarcopenia Research (icfsr) Task Force. J. Frailty Aging 2022, 11, 135–142. [Google Scholar] [CrossRef]
- Hevia-Larraín, V.; Gualano, B.; Longobardi, I.; Gil, S.; Fernandes, A.L.; Costa, L.A.R.; Pereira, R.M.R.; Artioli, G.G.; Phillips, S.M.; Roschel, H. High-Protein Plant-Based Diet Versus a Protein-Matched Omnivorous Diet to Support Resistance Training Adaptations: A Comparison Between Habitual Vegans and Omnivores. Sport. Med. 2021, 51, 1317–1330. [Google Scholar] [CrossRef]
- Teixeira, F.J.; Matias, C.N.; Faleiro, J.; Giro, R.; Pires, J.; Figueiredo, H.; Carvalhinho, R.; Monteiro, C.P.; Reis, J.F.; Valamatos, M.J.; et al. A Novel Plant-Based Protein Has Similar Effects Compared to Whey Protein on Body Composition, Strength, Power, and Aerobic Performance in Professional and Semi-Professional Futsal Players. Front. Nutr. 2022, 9, 934438. [Google Scholar] [CrossRef]
- Phillips, S.M.; van Loon, L.J. Dietary protein for athletes: From requirements to optimum adaptation. J. Sport. Sci. 2011, 29 (Suppl. 1), S29–S38. [Google Scholar] [CrossRef]
- Genario, R.; Cipolla-Neto, J.; Bueno, A.A.; Santos, H.O. Melatonin supplementation in the management of obesity and obesity-associated disorders: A review of physiological mechanisms and clinical applications. Pharmacol. Res. 2020, 163, 105254. [Google Scholar] [CrossRef] [PubMed]
- Leproult, R.; Van Cauter, E. Effect of 1 week of sleep restriction on testosterone levels in young healthy men. JAMA 2011, 305, 2173–2174. [Google Scholar] [CrossRef] [PubMed]
| Population | Serum Myostatin Levels | Reference |
|---|---|---|
| Young and older male (n = 1121) | 30.5 ± 9.5 ng/mL for 20 to 30 yr (n = 76) | [30] |
| 26.7 ± 10.6 ng/mL for >30 to 40 yr (n = 69) | ||
| 28.3 ± 10.1 ng/mL for >40 to 50 yr (n = 88) | ||
| 32.7 ± 10.1 ng/mL for >50 to 60 yr (n = 91) | ||
| 30.6 ± 11.9 ng/mL for >60 to 70 yr (n = 314) | ||
| 28.4 ± 12.3 ng/mL for >70 to 80 yr (n = 345) | ||
| 28.9 ± 10.4 ng/mL for >80 yr (n = 121) | ||
| Older individuals (n = 1053) | 3.7 ± 1.2 ng/mL for men | [31] |
| 3.2 ± 1.1 ng/mL for women | ||
| Caucasian women (in perimenopause or postmenopause) (n = 300) | 6.58 ± 3.59 ng/mL | [33] |
| Menstruating women (n = 33), Naturally menopausal (n = 24), and Surgically menopausal women (n = 37) | 7.0 ± 2.7 ng/dL for menstruating women | [32] |
| 6.7 ± 2.8 ng/mL for naturally menopausal | ||
| 6.7 ± 2.7 surgically menopausal women | ||
| Kidney transplantation recipients (n = 84) | 6.99 (5.82–8.32) ng/mL | [35] |
| Heart failure (n = 41) | 18.7 ± 7.4 ng/mL | [36] |
| Metabolic syndrome (n = 204) | 7.39 ± 3.46 ng/mL | [37] |
| Type 2 diabetes (n = 246) | 7.82 ± 3.85 ng/mL | [37] |
| Dermatomyositis and polymyositis (n = 50) | 16.9 ± 12.1 ng/mL | [38] |
| Hemodialysis (n = 140) | 40.18 ± 8.36 ng/mL | [39] |
| Hemodialysis (n = 204) | 2573 (1662; 3703) pg/mL | [40] |
| Hemodialysis (n = 60) | 25.7 ± 12.8 μg/mL | [41] |
| Peritoneal dialysis (n = 69) | 7.59 ± 3.37 ng/mL | [42] |
| Liver cirrhosis (108 men and 90 women) | 3419.6 pg/mL (578.4–12897.7 pg/mL) for men | [43] |
| 2662.4 pg/mL (710.4–8782.0 pg/mL) for women | ||
| Liver cirrhosis (n = 115) | 1.14 (0.57–2.19) ng/mL | [44] |
| Advanced chronic liver disease (198 men and 90 women) | 1959.4 pg/mL (1082.8, 3914.8) for men and 1790.1 pg/mL (914.1, 3158.7) for women | [45] |
| Alcoholic hepatitis (n = 131) | 1.58 ng/mL (IQR 0.73, 3.17) for men | [46] |
| 0.84 ng/mL (IQR 0.56, 1.76) for women | ||
| Heavy drinkers (n = 124) | 3.06 ng/mL (IQR 2.25, 4.08) for men | [46] |
| 2.01 ng/mL (IQR 1.66, 3.07) for women | ||
| Children with T1DM (n = 87) | 23.60 ± 7.70 ng/mL | [47] |
| Healthy children (n = 75) | 16.74 ± 6.95 ng/mL | [47] |
| Duchenne muscular dystrophy (n = 74) | 1.1 ± 0.8 ng/mL | [48] |
| Chronic obstructive pulmonary disease (n = 70) | 11.85 ± 4.01 ng/mL | [49] |
| Reference | Participants | Duration | Dietary Intervention | Myostatin Levels |
|---|---|---|---|---|
| Proteins, amino acids, and derivatives | ||||
| Hulmi et al. (2008) [67] | 18 trained middle-aged to older men | Acute and chronic (21 week) | 15 g of whey protein both before and after exercise | ↓myostatin mRNA levels at 48 h assessment postexercise for placebo |
| Hulmi et al. (2009) [68] | 31 untrained young men | Acute and chronic (21 week) | 15 g of whey protein both before and after exercise | ↓31% myostatin mRNA expression only in the placebo group at 1 h post-exercise |
| Dalbo et al. (2013) [69] | 10 untrained college-aged men (crossover) | Acute | Whey protein isolate (25 g), maltodextrin (25 g), or placebo 30 min prior to RT | ↓myostatin mRNA expression reduced in all conditions (−29.4% for placebo, −24.7% for protein, and −3.4% for carbohydrate) 6 h after RT |
| Amasene et al. (2022) [23] | 41 hospitalized older individuals | 12 week | Whey protein (20 g) + leucine (3 g) | ↔ |
| Dirks et al. (2014) [58] | 23 older individuals on immobilization of one knee | 5 d | Whey protein (20.7 g protein) | ↔ |
| Constantin et al. (2013) [59] | 59 patients with COPD and 21 healthy controls | 8 week | Whey protein concentrate + glucose polymer carbohydrate (19 g protein, 49 g carbohydrates) | ↔ |
| Pourabbas et al. (2021) [24] | 30 resistance-trained young men | 6 week | High-protein milk (30 g of protein, 6 g from whey and 24 g from casein) | ↓serum myostatin levels compared to placebo |
| Wette et al. (2021) [64] | 7 men on RT (crossover) | Acute | Postexercise meal milk protein (600 mL chocolate milk and 85 g muesli bar, 102 g carbohydrate, 34 g protein, and 22 g fat) | ↔ |
| Li et al. (2015) [51] | 41 young men | Acute | Peri-exercise supplementation of carbohydrates (1.5 g/kg), carbohydrates + BCAA (120 mg/kg BCAA), or carbohydrates + leucine (120 mg/kg) | myostatin mRNA expression over 360 min postexercise was higher for those who supplemented with carbohydrates (1.00 ± 0.09) and carbohydrates + BCAA (1.05 ± 0.08) than carbohydrates + leucine (0.92 ± 0.07) or placebo (0.90 ± 0.05) |
| Bagheri et al. (2021b) [53] | 20 postmenopausal women on RT | 8 week | BCAA (9 g/d) | ↔ |
| Tsien et al. (2015) [56] | 6 men with cirrhosis and 8 healthy controls | Acute | BCAA (7.5 g of leucine, 3.75 g of isoleucine, and 3.75 g of valine) | ↔ |
| Olveira et al. (2016) [57] | 28 patients with bronchiectasis | 12 week | HMB-enriched protein supplementation (18 g protein, 1.5 g HMB) | ↔ |
| Saremi et al. (2010) [54] | 24 men | 8 week | Creatine (0.3 g/kg/d BW at week 1 and 0.05 g/kg BW/d for the rest) | ↓plasma myostatin levels in creatine and placebo groups |
| Deldicque et al. (2008) [55] | 9 young men on RT | Acute (measures after 5 d of creatine loading) | Creatine (21 g/d; 7 g 3 x/d) | ↔ |
| Sire et al. (2019) [70] | 20 patients submitted to hip replacement | 8 week | Amino acids (4 g 2 x/d) | ↓serum myostatin levels for amino acid (from 1.2 ± 0.2 to 0.9 ± 0.3 ng/mL) and placebo (from 1.3 ± 0.3 to 1.1 ± 0.4 ng/mL) groups |
| Paoli et al. (2015) [22] | 18 active young men without experience with RT | 8 week | High-protein diet (1.8 g protein/kg BW/d) vs. normal-protein diet (0.85 g protein/kg BW/d) | ↑plasma myostatin levels after RT session (pretraining and posttraining levels: from 3.66 ± 1.42 to 12.0 ± 2.5 ng/mL) in the high-protein group |
| Bagheri et al. (2020) [52] | 30 young men | 12 week | Whole eggs (3 units) vs. egg whites (6 units) | ↔ |
| Non-protein supplements | ||||
| Willoughby (2004) [75] | 22 untrained health men | 12 week | Cystoseira canariensis (1200 mg/d) | ↔ |
| García-Merino et al. (2020) [81] | 44 training endurance athletes (men) | 10 week | Cocoa (5 g cocoa powder, 425 mg flavonoids) | ↔ |
| Mafi et al. (2018) [83] | 62 older individuals | 8 week | Epicatechin (1 mg/kg BW/d | ↓49% in plasma myostatin levels in the RT plus epicatechin group than in the RT group |
| Gonnelli et al. (2021) [87] | 50 postmenopausal women | 180 d | Calcifediol (20 or 30 μg/d) | ↔ |
| Bagheri et al. (2021a) [79] | 40 male wrestlers | 12 d | Spirulina (3 g/d) | ↓serum myostatin levels by 0.1 ng/mL |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Santos, H.O.; Cerqueira, H.S.; Tinsley, G.M. The Effects of Dietary Supplements, Nutraceutical Agents, and Physical Exercise on Myostatin Levels: Hope or Hype? Metabolites 2022, 12, 1146. https://doi.org/10.3390/metabo12111146
Santos HO, Cerqueira HS, Tinsley GM. The Effects of Dietary Supplements, Nutraceutical Agents, and Physical Exercise on Myostatin Levels: Hope or Hype? Metabolites. 2022; 12(11):1146. https://doi.org/10.3390/metabo12111146
Chicago/Turabian StyleSantos, Heitor O., Henrique S. Cerqueira, and Grant M. Tinsley. 2022. "The Effects of Dietary Supplements, Nutraceutical Agents, and Physical Exercise on Myostatin Levels: Hope or Hype?" Metabolites 12, no. 11: 1146. https://doi.org/10.3390/metabo12111146