Healthy or Not Healthy? A Mixed-Methods Approach to Evaluate Front-of-Pack Nutrition Labels as a Tool to Guide Consumers
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Ethical Considerations
2.3. Recruitment
2.3.1. Interview Participants: Qualitative Study
2.3.2. Survey Respondents: Quantitative Study
2.4. Procedure
2.4.1. Interviews: Qualitative Study
2.4.2. Surveys: Quantitative Study
2.5. Data Analysis
2.5.1. Interview Data: Qualitative Study
2.5.2. Survey Data: Quantitative Study
2.5.3. Integration of Data Sets
2.6. Trustworthiness, Validity and Reliability
3. Results
3.1. Study Sample Characteristics
3.1.1. Qualitative Study (Interview Participants)
3.1.2. Quantitative Study (Survey Respondents)
3.2. Qualitative Themes from the Interviews
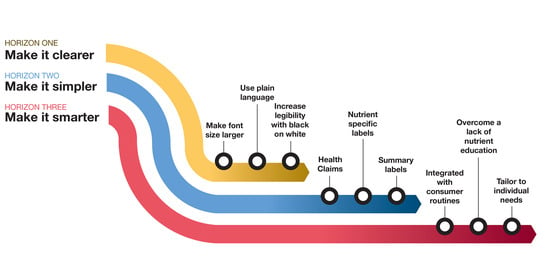
3.2.1. Make it Clearer (Theme 1)
3.2.2. Make it Simpler (Theme 2)
“Whatever you do, you have to be consistent because consumers can’t see ‘live well, eat well’ for one company’s product [a local manufacturer’s logo], but then there are GDAs on all the multinationals’ products.”[PR21]
3.2.3. Make it Smarter (Theme 3)
“It is an enormous task to try and put a statement [on a package], a blanket statement that would fit 53 million people. But then I thought to myself—with algorithms and big data, it’s maybe not so far off anymore… Information interpreted for me, to help me to make better decisions.”[CN1]
“If your target is the poorly educated poor people, then technology is not the solution, because they can’t afford data… and the older generation, who didn’t grow up with that technology, get excluded.”[PR23]
3.2.4. Challenges to Effective Static (On-Pack) Food Labels
3.3. Quantitative Findings from the Consumer Survey
3.3.1. Selection and Creation of FOP Labels
3.3.2. Reliability of Survey Results
3.3.3. Performance of FOP Labels
3.4. Integration
- Synopsis of the label improvement suggestions made by participants in the qualitative phase of the study;
- A single illustrative quote for the theme (additional quotes are available in the Supplementary Materials);
- Application of qualitative insights to the consumer survey;
- A synopsis of the survey findings (exclusive to Horizon 2); and
- Positive and negative implications for each horizon through the integration of qualitative and quantitative data.
4. Discussion
4.1. Short Term: Make It Clearer
4.2. Medium Term: Make It Simpler
4.3. Long Term: Make It Smarter
4.4. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Noncommunicable Diseases: Country Profiles 2018; World Health Organization: Geneva, Switzerland, 2018.
- Burger, R.; Christian, C. Access to Health Care in Post-Apartheid South Africa: Availability, Affordability, Acceptability. Health Econ. Policy Law 2020, 15, 43–55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gordon, T.; Booysen, F.; Mbonigaba, J. Socio-Economic Inequalities in the Multiple Dimensions of Access to Healthcare: The Case of South Africa. BMC Public Health 2020, 20, 289. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. World Health Statistics 2018: Monitoring Health for the SDGs; World Health Organization: Geneva, Switzerland, 2018.
- Lane, M.M.; Davis, J.A.; Beattie, S.; Gómez-Donoso, C.; Loughman, A.; O’Neil, A.; Jacka, F.; Berk, M.; Page, R.; Marx, W.; et al. Ultraprocessed Food and Chronic Noncommunicable Diseases: A Systematic Review and Meta-Analysis of 43 Observational Studies. Obes. Rev. 2021, 22, e13146. [Google Scholar] [CrossRef] [PubMed]
- Popkin, B.M.; Adair, L.S.; Ng, S.W. Global Nutrition Transition and the Pandemic of Obesity in Developing Countries. Nutr. Rev. 2012, 70, 3–21. [Google Scholar] [CrossRef] [Green Version]
- Fanzo, J.; Drewnowski, A.; Blumberg, J.; Miller, G.; Kraemer, K. Nutrients, Foods, Diets, People: Promoting Healthy Eating. Curr. Dev. Nutr. 2020, 4, nzaa069. [Google Scholar] [CrossRef] [Green Version]
- Moodie, R.; Stuckler, D.; Monteiro, C.; Sheron, N.; Neal, B.; Thamarangsi, T.; Lincoln, P.; Casswell, S. Profits and Pandemics: Prevention of Harmful Effects of Tobacco, Alcohol, and Ultra-Processed Food and Drink Industries. Lancet 2013, 381, 670–679. [Google Scholar] [CrossRef]
- Kliemann, N.; Kraemer, M.V.S.; Id, T.S.; Rodrigues, V.M.; Fernandes, A.C.; Id, G.L.B.; Uggioni, P.L.; Proença, R.P.C. Serving Size and Nutrition Labelling: Implications for Nutrition Information and Nutrition Claims on Packaged Foods. Nutrients 2018, 10, 891. [Google Scholar] [CrossRef] [Green Version]
- Koen, N.; Blaauw, R.; Wentzel-Viljoen, E. Food and Nutrition Labelling: The Past, Present and the Way Forward. South Afr. J. Clin. Nutr. 2016, 29, 13–21. [Google Scholar] [CrossRef] [Green Version]
- Crockett, R.A.; King, S.E.; Marteau, T.M.; Prevost, A.T.; Bignardi, G.; Roberts, N.W.; Stubbs, B.; Hollands, G.J.; Jebb, S.A. Nutritional Labelling for Healthier Food or Non-Alcoholic Drink Purchasing and Consumption. Cochrane Database Syst. Rev. 2018, 2018, CD009315. [Google Scholar] [CrossRef] [Green Version]
- Bhattacharya, S.; Saleem, S.M.; Bera, O.P. Prevention of Childhood Obesity through Appropriate Food Labeling. Clin. Nutr. ESPEN 2022, 47, 418–421. [Google Scholar] [CrossRef]
- Jacobs, S.A.; De Beer, H.; Larney, M. Adult Consumers’ Understanding and Use of Information on Food Labels: A Study among Consumers Living in the Potchefstroom and Klerksdorp Regions, South Africa. Public Health Nutr. 2011, 14, 510–522. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van der Colff, N.; Van der Merwe, D.; Bosman, M.; Erasmus, A.; Ellis, S. Consumers’ Prepurchase Satisfaction with the Attributes and Information of Food Labels. Int. J. Consum. Stud. 2016, 40, 220–228. [Google Scholar] [CrossRef]
- Koen, N.; Wentzel-Viljoen, E.; Nel, D.; Blaauw, R. Consumer Knowledge and Use of Food and Nutrition Labelling in South Africa: A Cross-Sectional Descriptive Study. Int. J. Consum. Stud. 2018, 42, 335–346. [Google Scholar] [CrossRef]
- Bosman, M.J.C.; van der Merwe, D.; Ellis, S.M.; Jerling, J.C.; Badham, J. South African Adult Metropolitan Consumers’ Opinions and Use of Health Information on Food Labels. Br. Food J. 2014, 116, 30–43. [Google Scholar] [CrossRef]
- Todd, M.; Guetterman, T.; Sigge, G.; Joubert, E. Multi-Stakeholder Perspectives on Food Labeling and Health Claims: Qualitative Insights from South Africa. Appetite 2021, 167, 105606. [Google Scholar] [CrossRef]
- World Economic Forum. These Countries Have the Most Official Languages. Available online: https://www.weforum.org/agenda/2017/08/these-countries-have-the-most-official-languages/ (accessed on 10 February 2022).
- Ataguba, J.E.; Akazili, J.; McIntyre, D. Socioeconomic-Related Health Inequality in South Africa: Evidence from General Household Surveys. Int. J. Equity Health 2011, 10, 48. [Google Scholar] [CrossRef] [Green Version]
- Storcksdieck, S.; Marandola, G.; Ciriolo, E.; van Bavel, R.; Wollgast, J. Front-of-Pack Nutrition Labelling Schemes: A Comprehensive Review; Publications Office of the European Union: Luxembourg, 2020. [Google Scholar]
- Temple, N.J. Front-of-Package Food Labels: A Narrative Review. Appetite 2020, 144, 104485. [Google Scholar] [CrossRef]
- Swedish National Food Agency. The Keyhole. Available online: https://www.livsmedelsverket.se/en/food-and-content/labelling/nyckelhalet (accessed on 6 February 2022).
- Choices International Foundation. Choices Programme. Available online: https://www.choicesprogramme.org/ (accessed on 6 February 2022).
- Australian Government Department of Health. Front-of-Pack Labelling Updates. Available online: https://foodregulation.gov.au/internet/fr/publishing.nsf/Content/front-of-pack-labelling-1 (accessed on 25 January 2022).
- Julia, C.; Blanchet, O.; Méjean, C.; Péneau, S.; Ducrot, P.; Allès, B.; Fezeu, L.K.; Touvier, M.; Kesse-Guyot, E.; Singler, E.; et al. Impact of the Front-of-Pack 5-Colour Nutrition Label (5-CNL) on the Nutritional Quality of Purchases: An Experimental Study. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 101. [Google Scholar] [CrossRef]
- Carreño, I. Chile’s Black STOP Sign for Foods High in Fat, Salt or Sugar. Eur. J. Risk Regul. 2015, 6, 622–628. [Google Scholar] [CrossRef]
- Croker, H.; Packer, J.; Russell, S.J.; Stansfield, C.; Viner, R.M. Front of Pack Nutritional Labellin Schemes: A Systematic Review and Meta-Analysis of Recent Evidence Relating to Objectively Measured Consumption and Purchasing. J. Hum. Nutr. Diet. 2020, 33, 518–537. [Google Scholar] [CrossRef]
- Vanderlee, L.; Franco-Arellano, B.; Ahmed, M.; Oh, A.; Lou, W.; L’Abbé, M.R. The Efficacy of ‘High in’ Warning Labels, Health Star and Traffic Light Front-of-Package Labelling: An Online Randomised Control Trial. Public Health Nutr. 2020, 24, 62–74. [Google Scholar] [CrossRef] [PubMed]
- Franco-Arellano, B.; Vanderlee, L.; Ahmed, M.; Oh, A.; Abbé, M.L. Influence of Front-of-Pack Labelling and Regulated Nutrition Claims on Consumers ’ Perceptions of Product Healthfulness and Purchase Intentions: A Randomized Controlled Trial. Appetite 2020, 149, 104629. [Google Scholar] [CrossRef]
- Van der Bend, D.L.M.; Jansen, L.; Van der Velde, G.; Blok, V. The Influence of a Front-of-Pack Nutrition Label on Product Reformulation: A Ten-Year Evaluation of the Dutch Choices Programme. Food Chem. X 2020, 6, 100086. [Google Scholar] [CrossRef] [PubMed]
- Ronquest-Ross, L.C.; Vink, N.; Sigge, G.O. Food Consumption Changes in South Africa since 1994. S. Afr. J. Sci. 2015, 111, 1–12. [Google Scholar] [CrossRef]
- Storcksdieck genannt Bonsmann, S.; Robinson, M.; Wollgast, J.; Caldeira, S. The Ineligibility of Food Products from across the EU for Marketing to Children According to Two EU-Level Nutrient Profile Models. PLoS ONE 2019, 14, e0213512. [Google Scholar] [CrossRef]
- Monteiro, C.A.; Cannon, G.; Moubarac, J.C.; Levy, R.B.; Louzada, M.L.C.; Jaime, P.C. The UN Decade of Nutrition, the NOVA Food Classification and the Trouble with Ultra-Processing. Public Health Nutr. 2018, 21, 5–17. [Google Scholar] [CrossRef] [Green Version]
- O’Cathain, A.; Murphy, E.; Nicholl, J. Three Techniques for Integrating Data in Mixed Methods Studies. BMJ 2010, 341, 1147–1150. [Google Scholar] [CrossRef]
- Creswell, J.W.; Plano Clark, V.L. Designing and Conducting Mixed Methods Research, 3rd ed.; Kindle Edition; SAGE Publications: Los Angeles, CA, USA, 2017. [Google Scholar]
- Creswell, J.; Creswell, J. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches; SAGE Publications: Thousand Oaks, CA, USA, 2017. [Google Scholar]
- Doyle, L.; Brady, A.M.; Byrne, G. An Overview of Mixed Methods Research. J. Res. Nurs. 2009, 14, 175–185. [Google Scholar] [CrossRef]
- Patten, M.L.; Newhart, M. Mixed Methods Designs. In Understanding Research Methods; Taylor & Francis Group: Abingdon, UK, 2018; pp. 177–179. [Google Scholar] [CrossRef]
- Reyes, M.; Garmendia, M.L.; Olivares, S.; Aqueveque, C.; Zacarías, I.; Corvalán, C. Development of the Chilean Front-of-Package Food Warning Label. BMC Public Health 2019, 19, 906. [Google Scholar] [CrossRef] [Green Version]
- Creswell, J.W.; Poth, C.N. Qualitative Inquiry and Research Design: Choosing Among Five Approaches; SAGE Publications: Thousand Oaks, CA, USA, 2016. [Google Scholar]
- Feilzer, M.Y. Doing Mixed Methods Research Pragmatically: Implications for the Rediscovery of Pragmatism as a Research Paradigm. J. Mix. Methods Res. 2010, 4, 6–16. [Google Scholar] [CrossRef]
- Noy, C. Sampling Knowledge: The Hermeneutics of Snowball Sampling in Qualitative Research. Int. J. Soc. Res. Methodol. 2008, 11, 327–344. [Google Scholar] [CrossRef]
- Guest, G.; Bunce, A.; Johnson, L. How Many Interviews Are Enough? An Experiment with Data Saturation and Variability. Field Methods 2006, 18, 59–82. [Google Scholar] [CrossRef]
- Zuo, Y.; Zhang, K.; Xu, S.; Law, R.; Qiu, Q.; Zhang, M. What Kind of Food Can Win Gen Z’s Favor? A Mixed Methods Study from China. Food Qual. Prefer. 2022, 98, 104522. [Google Scholar] [CrossRef]
- Kendall, H.; Brennan, M.; Seal, C.; Ladha, C.; Kuznesof, S. Behind the Kitchen Door: A Novel Mixed Method Approach for Exploring the Food Provisioning Practices of the Older Consumer. Food Qual. Prefer. 2016, 53, 105–116. [Google Scholar] [CrossRef] [Green Version]
- Gould, S.J. Health Consciousness and Health Behavior: The Application of a New Health Consciousness Scale. Am. J. Prev. Med. 1990, 6, 228–237. [Google Scholar] [CrossRef]
- World Health Organization. WHO Guidelines on Physical Activity and Sedentary Behaviour; World Health Organization: Geneva, Switzerland, 2020.
- Braun, V.; Clarke, V. Using Thematic Analysis in Psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- Guetterman, T.C.; Fetters, M.D.; Creswell, J.W. Integrating Quantitative and Qualitative Results in Health Science Mixed Methods Research through Joint Displays. Ann. Fam. Med. 2015, 13, 554–561. [Google Scholar] [CrossRef]
- Lincoln, Y.; Guba, E.G. Naturalistic Inquiry; Sage: Newbury Park, CA, USA, 1985. [Google Scholar]
- Birt, L.; Scott, S.; Cavers, D.; Campbell, C.; Walter, F. Member Checking: A Tool to Enhance Trustworthiness or Merely a Nod to Validation? Qual. Health Res. 2016, 26, 1802–1811. [Google Scholar] [CrossRef] [Green Version]
- Koch, T. Establishing Rigour in Qualitative Research: The Decision Trail. J. Adv. Nurs. 1994, 19, 976–986. [Google Scholar] [CrossRef]
- Mohamad, M.M.; Sulaiman, N.L.; Sern, L.C.; Salleh, K.M. Measuring the Validity and Reliability of Research Instruments. Procedia Soc. Behav. Sci. 2015, 204, 164–171. [Google Scholar] [CrossRef] [Green Version]
- Ursachi, G.; Horodnic, I.A.; Zait, A. How Reliable Are Measurement Scales? External Factors with Indirect Influence on Reliability Estimators. Procedia Econ. Financ. 2015, 20, 679–686. [Google Scholar] [CrossRef] [Green Version]
- Deliza, R.; de Alcantara, M.; Pereira, R.; Ares, G. How Do Different Warning Signs Compare with the Guideline Daily Amount and Traffic-Light System? Food Qual. Prefer. 2020, 80, 103821. [Google Scholar] [CrossRef]
- Department of Health Republic of South Africa. Regulations Relating to the Labelling and Advertsing of Foods: Amendment; Government Notice R. 429 of 29 May 2014; Promulgated under Foodstuffs, Cosmetics and Disinfectants Act, 54 of 1972; Department of Health, Republic of South Africa: Pretoria, South Africa, 2014.
- Baleta, A.; Mitchell, F. Country in Focus: Diabetes and Obesity in South Africa. Lancet Diabetes Endocrinol. 2014, 2, 678–688. [Google Scholar] [CrossRef]
- Coley, S. Enduring Ideas: The Three Horizons of Growth. In McKinsey Quarterly; McKinsey & Company: New York, NY, USA, 2009. [Google Scholar]
- Department of Health Republic of South Africa. Regulations Relating to the Labelling and Advertising of Foodstuffs (R146/2010); No. 32975, 1 March 2010; Department of Health, Republic of South Africa: Pretoria, South Africa, 2010.
- Sharma, L.L.; Teret, S.P.; Brownell, K.D. The Food Industry and Self-Regulation: Standards to Promote Success and to Avoid Public Health Failures. Am. J. Public Health 2010, 100, 240–246. [Google Scholar] [CrossRef]
- Simone, M. Can Food Companies Be Trusted to Self-Regulate? An Analysis of Corporate Lobbying and Deception to Undermine Children’s Health. Loyola Los Angel. Law Rev. 2006, 39, 169–237. [Google Scholar]
- Ronit, K.; Jensen, J.D. Obesity and Industry Self-Regulation of Food and Beverage Marketing: A Literature Review. Eur. J. Clin. Nutr. 2014, 68, 753–759. [Google Scholar] [CrossRef]
- Fooks, G.J.; Godziewski, C. The World Health Organization, Corporate Power, and the Prevention and Management of Conflicts of Interest in Nutrition Policy Comment on “Towards Preventing and Managing Conflict of Interest in Nutrition Policy? An Analysis of Submissions to a Consultati”. Int. J. Health Policy Manag. 2020, 11, 228–232. [Google Scholar] [CrossRef]
- Mialon, M.; Ho, M.; Carriedo, A.; Ruskin, G.; Crosbie, E. Beyond Nutrition and Physical Activity: Food Industry Shaping of the Very Principles of Scientific Integrity. Global. Health 2021, 17, 37. [Google Scholar] [CrossRef]
- Lauber, K.; Rutter, H.; Gilmore, A.B. Big Food and the World Health Organization: A Qualitative Study of Industry Attempts to Influence Global-Level Non-Communicable Disease Policy. BMJ Glob. Health 2021, 6, e005216. [Google Scholar] [CrossRef]
- Hoe, C.; Weiger, C.; Minosa, M.K.R.; Alonso, F.; Koon, A.D.; Cohen, J.E. Strategies to Expand Corporate Autonomy by the Tobacco, Alcohol and Sugar-Sweetened Beverage Industry: A Scoping Review of Reviews. Global. Health 2022, 18, 17. [Google Scholar] [CrossRef]
- Maphumulo, W.T.; Bhengu, B.R. Challenges of Quality Improvement in the Healthcare of South Africa Post-Apartheid: A Critical Review. Clin. Gov. Gen. Dent. Pract. 2019, 42, 233–240. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marimwe, C.; Dowse, R. Health Literacy Test for Limited Literacy Populations (HELT-LL): Validation in South Africa. Cogent Med. 2019, 6, 1650417. [Google Scholar] [CrossRef]
- Department of Health Republic of South Africa. Foodstuffs, Cosmetics and Disinfectants; Act, No. 54 of 1972; Regulations Relating To Health Messages on Container Labels of Alcoholic Beverages; R.764; Department of Health Republic of South Africa: Pretoria, South Africa, 2007; pp. 4–5.
- TobaccoTactics. South Africa—Country Profile. Available online: https://tobaccotactics.org/wiki/south-africa-country-profile/ (accessed on 7 February 2022).
- Starling, S. UK Food Industry Backs GDA Labelling. Available online: https://www.newhope.com/regulatory/uk-food-industry-backs-gda-labelling (accessed on 28 January 2022).
- European Commission. Commission Regulation (EU) No 1018/2013 of 23 October 2013 Amending Regulation (EU) No 432/2012 Establishing a List of Permitted Health Claims Made on Foods Other than Those Referring to the Reduction of Disease Risk and to Children’s Development and Health. Off. J. Eur. Union 2013, 56, 43–45. [Google Scholar]
- Boztuğ, Y.; Juhl, H.J.; Elshiewy, O.; Jensen, M.B. Consumer Response to Monochrome Guideline Daily Amount Nutrition Labels. Food Policy 2015, 53, 1–8. [Google Scholar] [CrossRef]
- Draper, A.K.; Adamson, A.J.; Clegg, S.; Malam, S.; Rigg, M.; Duncan, S. Front-of-Pack Nutrition Labelling: Are Multiple Formats a Problem for Consumers? Eur. J. Public Health 2013, 23, 517–521. [Google Scholar] [CrossRef]
- Grunert, K.G.; Wills, J.M. A Review of European Research on Consumer Response to Nutrition Information on Food Labels. J. Public Health 2007, 15, 385–399. [Google Scholar] [CrossRef] [Green Version]
- Schor, D.; Maniscalco, S.; Tuttle, M.M.; Alligood, S.; Kapsak, W.R. Nutrition Facts You Can’t Miss: The Evolution of Front-of-Pack Labeling. Nutr. Today 2010, 45, 22–32. [Google Scholar] [CrossRef]
- Söderlund, F.; Eyles, H.; Mhurchu, C.N. Stars versus Warnings: Comparison of the Australasian Health Star Rating Nutrition Labelling System with Chilean Warning Labels. Aust. N. Z. J. Public Health 2020, 44, 28–33. [Google Scholar] [CrossRef] [Green Version]
- Muller, L.; Ruffieux, B. What Makes a Front-of-Pack Nutritional Labelling System Effective: The Impact of Key Design Components on Food Purchases. Nutrients 2020, 12, 2870. [Google Scholar] [CrossRef]
- Van Herpen, E.; Hieke, S.; Van Trijp, H.C.M. Inferring Product Healthfulness from Nutrition Labelling. The Influence of Reference Points. Appetite 2014, 72, 138–149. [Google Scholar] [CrossRef]
- Clarke, N.; Pechey, E.; Mantzari, E.; Blackwell, A.K.M.; De-loyde, K.; Morris, R.W.; Munafò, M.R.; Marteau, T.M.; Hollands, G.J. Impact of Health Warning Labels on Snack Selection: An Online Experimental Study. Appetite 2020, 154, 104744. [Google Scholar] [CrossRef] [PubMed]
- Hunter-Adams, J.; Battersby, J.; Oni, T. Food Insecurity in Relation to Obesity in Peri-Urban Cape Town, South Africa: Implications for Diet-Related Non-Communicable Disease. Appetite 2019, 137, 244–249. [Google Scholar] [CrossRef] [PubMed]
- Davis, J.; Magadzire, N.; Hemerijckx, L.M.; Maes, T.; Durno, D.; Kenyana, N.; Lwasa, S.; Van Rompaey, A.; Verburg, P.H.; May, J. Precision Approaches to Food Insecurity: A Spatial Analysis of Urban Hunger and Its Contextual Correlates in an African City. World Dev. 2022, 149, 105694. [Google Scholar] [CrossRef]
- Dubois, P.; Albuquerque, P.; Allais, O.; Bonnet, C.; Bertail, P.; Combris, P.; Lahlou, S.; Rigal, N.; Ruffieux, B.; Chandon, P. Effects of Front-of-Pack Labels on the Nutritional Quality of Supermarket Food Purchases: Evidence from a Large-Scale Randomized Controlled Trial. J. Acad. Mark. Sci. 2021, 49, 119–138. [Google Scholar] [CrossRef] [Green Version]
- Ikonen, I.; Sotgiu, F.; Aydinli, A.; Verlegh, P.W.J. Consumer Effects of Front-of-Package Nutrition Labeling: An Interdisciplinary Meta-Analysis. J. Acad. Mark. Sci. 2020, 48, 360–383. [Google Scholar] [CrossRef] [Green Version]
- An, R.; Shi, Y.; Shen, J.; Bullard, T.; Liu, G.; Yang, Q.; Chen, N.; Cao, L. Effect of Front-of-Package Nutrition Labeling on Food Purchases: A Systematic Review. Public Health 2021, 191, 59–67. [Google Scholar] [CrossRef]
- Ordovas, J.M.; Ferguson, L.R.; Tai, E.S.; Mathers, J.C. Personalised Nutrition and Health. BMJ 2018, 361, bmj.k2173. [Google Scholar] [CrossRef] [Green Version]
- Celis-Morales, C.; Lara, J.; Mathers, J.C. Personalising Nutritional Guidance for More Effective Behaviour Change. Proc. Nutr. Soc. 2015, 74, 130–138. [Google Scholar] [CrossRef] [Green Version]
- Hartwell, H.; Appleton, K.M.; Bray, J.; Price, S.; Mavridis, I.; Giboreau, A.; Perez-Cueto, F.J.A.; Ronge, M. Shaping Smarter Consumer Food Choices: The FoodSMART Project. Nutr. Bull. 2019, 44, 138–144. [Google Scholar] [CrossRef] [Green Version]
- Adams, S.H.; Anthony, J.C.; Carvajal, R.; Chae, L.; Khoo, C.S.; Latulippe, M.E.; Matusheski, N.V.; Mcclung, H.L.; Rozga, M.; Schmid, C.H.; et al. Guiding Principles for the Implementation of Personalized Nutrition Approaches That Benefit Health and Function. Adv. Nutr. 2020, 11, 25–34. [Google Scholar] [CrossRef]
- Gibney, M.; Walsh, M.; Goosens, J. Personalized Nutrition: Paving the Way to Better Population Health. In Good Nutrition: Perspectives for the 21st Century; Karger Publishers: Basel, Switzerland, 2016; pp. 235–248. [Google Scholar]
- Haghi, M.; Thurow, K.; Stoll, R. Wearable Devices in Medical Internet of Things: Scientific Research and Commercially Available Devices. Healthc. Inform. Res. 2017, 23, 4–15. [Google Scholar] [CrossRef] [PubMed]
- Balaji, M.S.; Roy, S.K. Value Co-Creation with Internet of Things Technology in the Retail Industry. J. Mark. Manag. 2017, 33, 7–31. [Google Scholar] [CrossRef]
- Statista Smartphone Users in South Africa 2014–2023. Available online: https://www.statista.com/statistics/488376/forecast-of-smartphone-users-in-south-africa/ (accessed on 7 February 2022).
- Fausset, C.B.; Harley, L.; Farmer, S.; Fain, B. Older Adults’ Perceptions and Use of Technology: A Novel Approach. In Proceedings of the Universal Access in Human-Computer Interaction. User and Context Diversity. UAHCI 2013. Lecture Notes in Computer Science, Las Vegas, NV, USA, 21–26 July 2013; Springer: Berlin/Heidelberg, Germany, 2013; Volume 8010. [Google Scholar]
- Mitzner, T.L.; Boron, J.B.; Fausset, C.B.; Adams, A.E.; Charness, N.; Czaja, S.J.; Dijkstra, K.; Fisk, A.D.; Rogers, W.A.; Sharit, J.; et al. Older Adults Talk Technology: Technology Usage and Attitudes. Comput. Hum. Behav. 2010, 26, 1710–1721. [Google Scholar] [CrossRef] [Green Version]
- Heinz, M.; Martin, P.; Margrett, J.A.; Yearns, M.; Franke, W.; Yang, H.-I.; Wong, J.; Chang, C.K. Perceptions of Technology among Older Adults. J. Gerontol. Nurs. 2013, 39, 42–51. [Google Scholar] [CrossRef] [Green Version]
- Forbes 7 Predictions for How the Internet Will Change over the next 15 Years. Available online: https://www.forbes.com/sites/jaysondemers/2016/04/18/7-predictions-for-how-the-internet-will-change-over-the-next-15-years/?sh=49ef953622e0 (accessed on 5 February 2022).
- Marra, F. Food Products and Digital Tools: The Unexpected Interconnections. Front. Nutr. 2022, 9, 847038. [Google Scholar] [CrossRef] [PubMed]
- Dunford, E.K.; Neal, B. FoodSwitch and Use of Crowdsourcing to Inform Nutrient Databases. J. Food Compos. Anal. 2017, 64, 13–17. [Google Scholar] [CrossRef]
- Ares, G.; Antúnez, L.; Alcaire, F.; Vidal, L.; Bove, I. Listening to the Voices of Adolescents for the Design of Strategies to Promote Healthy Eating: An Exploratory Study in a Latin American Country. Public Health Nutr. 2021, 24, 5953–5962. [Google Scholar] [CrossRef]
- Diop, M. Africa Can Enjoy Leapfrog Development. Available online: https://www.worldbank.org/en/news/opinion/2017/10/11/africa-can-enjoy-leapfrog-development (accessed on 18 January 2022).
- Volpentesta, A.P.; Felicetti, A.M.; Ammirato, S. Intelligent Food Information Provision to Consumers in an Internet of Food Era. IFIP Adv. Inf. Commun. Technol. 2017, 506, 725–736. [Google Scholar] [CrossRef] [Green Version]
- Bove, L.A. Increasing Patient Engagement through the Use of Wearable Technology. J. Nurse Pract. 2019, 15, 535–539. [Google Scholar] [CrossRef] [Green Version]
- Mazzù, M.F.; Romani, S.; Baccelloni, A.; Lavini, L. Introducing the Front-of-Pack Acceptance Model: The Role of Usefulness and Ease of Use in European Consumers’ Acceptance of Front-of-Pack Labels. Int. J. Food Sci. Nutr. 2021, 73, 378–395. [Google Scholar] [CrossRef]





| Demographic Attribute | Category | Total (n) | ercentage (%) |
|---|---|---|---|
| Gender | Female | 915 | 72.6 |
| Male | 346 | 27.4 | |
| Age | 18–24 years old | 149 | 11.8 |
| 25–34 years old | 493 | 39.1 | |
| 35–49 years old | 441 | 35.0 | |
| 50+ years old | 178 | 14.1 | |
| Race | Black | 730 | 57.9 |
| Colored | 156 | 12.4 | |
| White | 274 | 21.7 | |
| Indian/Asian | 93 | 7.4 | |
| Prefer not to answer | 6 | 0.5 | |
| Other | 2 | 0.2 | |
| Household Income (monthly) | Less than ZAR 5000 | 365 | 28.9 |
| ZAR 5000–ZAR 9999 | 239 | 19.0 | |
| ZAR 10,000–ZAR 19,999 | 232 | 18.4 | |
| ZAR 20,000–ZAR 29,999 | 155 | 12.3 | |
| ZAR 30,000–ZAR 69,999 | 203 | 16.1 | |
| ZAR 70,000+ | 67 | 5.3 | |
| Education | Less than Grade 12 | 94 | 7.5 |
| Grade 12 | 394 | 31.2 | |
| Trade or vocational training | 247 | 19.6 | |
| Diploma | 253 | 20.1 | |
| Degree or Postgraduate Degree | 273 | 21.6 | |
| Children (<18 years) in Household | 0 | 356 | 28.2 |
| 1 | 340 | 27.0 | |
| 2 | 359 | 28.5 | |
| 3 | 147 | 11.7 | |
| 4+ | 59 | 4.7 | |
| Household size (Total) | 1 | 74 | 5.9 |
| 2 | 206 | 16.3 | |
| 3 | 248 | 19.7 | |
| 4 | 286 | 22.7 | |
| 5 | 213 | 16.9 | |
| 6 | 116 | 9.2 | |
| 7+ | 118 | 9.4 | |
| Province of residence | Gauteng | 615 | 48.8 |
| Western Cape | 225 | 17.8 | |
| KwaZulu-Natal | 188 | 14.9 | |
| Rest of South Africa | 233 | 18.5 | |
| Industry of employment | Arts, Entertainment, Recreation | 44 | 3.5 |
| Unemployed | 263 | 20.9 | |
| Education | 102 | 8.1 | |
| Food | 58 | 4.6 | |
| Financial Services | 73 | 5.8 | |
| Government, Public Administration | 92 | 7.3 | |
| Healthcare | 65 | 5.2 | |
| Media, Advertising, Public Relations | 68 | 5.4 | |
| Mining, Construction | 60 | 4.8 | |
| Scientific or Technical Services | 22 | 1.7 | |
| Student | 94 | 7.5 | |
| Telecommunications | 42 | 3.3 | |
| Other | 278 | 22.0 | |
| Relationship status | Single | 440 | 34.9 |
| In a relationship | 359 | 28.5 | |
| Married | 387 | 30.7 | |
| Divorced | 56 | 4.4 | |
| Other | 19 | 1.5 | |
| Smoking status | Non-smoker | 800 | 63.4 |
| Smoker | 229 | 18.2 | |
| Occasional smoker | 122 | 9.7 | |
| Ex-smoker | 110 | 8.7 | |
| Physical activity level | Inactive | 297 | 23.6 |
| Less than 150–300 min moderate-intensity exercise OR 75–150 min high-intensity exercise in a week | 511 | 40.5 | |
| About 150–300 min moderate-intensity exercise OR 75–150 min high-intensity exercise in a week | 327 | 25.9 | |
| More than 150–300 min moderate-intensity exercise OR 75–150 min high-intensity exercise in a week | 126 | 10.0 | |
| Shopping responsibility | Shared responsibility | 430 | 34.1 |
| Sole responsibility | 831 | 65.9 | |
| Cereal purchased | Occasional/Sometimes | 171 | 13.6 |
| Yes | 1090 | 86.4 | |
| How well do you understand food labels? | Not at all | 45 | 3.6 |
| A little | 110 | 8.7 | |
| Fifty-fifty | 268 | 21.3 | |
| Fairly well | 391 | 31.0 | |
| Very well | 447 | 35.4 | |
| Do food labels inform your food choices? | Not at all | 91 | 7.2 |
| A little | 126 | 10.0 | |
| Fifty-fifty | 297 | 23.6 | |
| Fairly well | 362 | 28.7 | |
| Very well | 385 | 30.5 | |
| Most searched nutrients on food labels (all that apply) | Sugar | 897 | 71.1 |
| Energy | 849 | 67.3 | |
| Fat | 787 | 62.4 | |
| Carbohydrates | 752 | 59.6 | |
| Protein | 734 | 58.2 | |
| Sodium | 510 | 40.4 | |
| Do not use label at all | 113 | 9.0 | |
| Main factor influencing food choices | Health | 521 | 41.3 |
| Price | 367 | 29.1 | |
| Taste | 218 | 17.3 | |
| Brand | 126 | 10.0 | |
| Appearance | 23 | 1.8 | |
| Other | 6 | 0.5 | |
| Main source of health information | Food labels | 389 | 30.8 |
| Doctor or dietician | 263 | 20.9 | |
| Social Media | 214 | 17.0 | |
| Books and Magazines | 165 | 13.1 | |
| Friends and Family | 129 | 10.2 | |
| Television or radio | 57 | 4.5 | |
| Other | 44 | 3.5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Todd, M.; Guetterman, T.; Volschenk, J.; Kidd, M.; Joubert, E. Healthy or Not Healthy? A Mixed-Methods Approach to Evaluate Front-of-Pack Nutrition Labels as a Tool to Guide Consumers. Nutrients 2022, 14, 2801. https://doi.org/10.3390/nu14142801
Todd M, Guetterman T, Volschenk J, Kidd M, Joubert E. Healthy or Not Healthy? A Mixed-Methods Approach to Evaluate Front-of-Pack Nutrition Labels as a Tool to Guide Consumers. Nutrients. 2022; 14(14):2801. https://doi.org/10.3390/nu14142801
Chicago/Turabian StyleTodd, Melvi, Timothy Guetterman, Jako Volschenk, Martin Kidd, and Elizabeth Joubert. 2022. "Healthy or Not Healthy? A Mixed-Methods Approach to Evaluate Front-of-Pack Nutrition Labels as a Tool to Guide Consumers" Nutrients 14, no. 14: 2801. https://doi.org/10.3390/nu14142801