Diagnostic and Therapeutic Challenges in Patients with Primary or Secondary Brain Tumor
A topical collection in Cancers (ISSN 2072-6694). This collection belongs to the section "Cancer Causes, Screening and Diagnosis".
Viewed by 52318Editors
Interests: brain tumors; targeted therapy; quality of life; brain metastases
Special Issues, Collections and Topics in MDPI journals
Interests: high grade glioma; low grade glioma; brain metastasis; meningioma; hemangioblastoma; VHL; vestibular schwannoma; intramedullary tumors
Special Issues, Collections and Topics in MDPI journals
Topical Collection Information
Dear Colleagues,
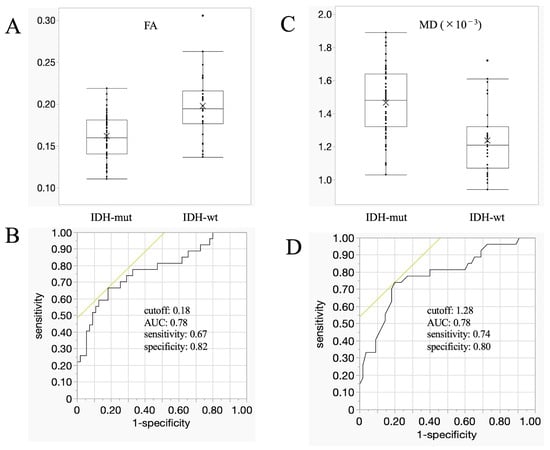
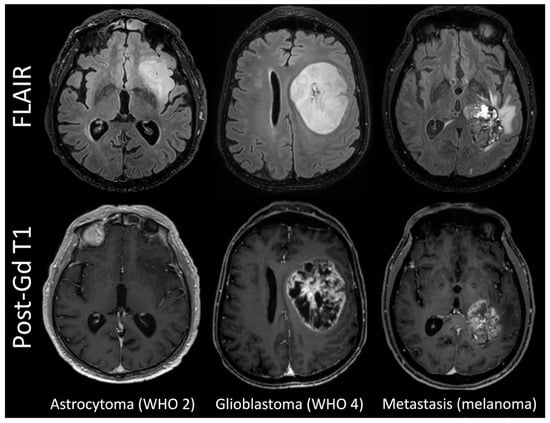
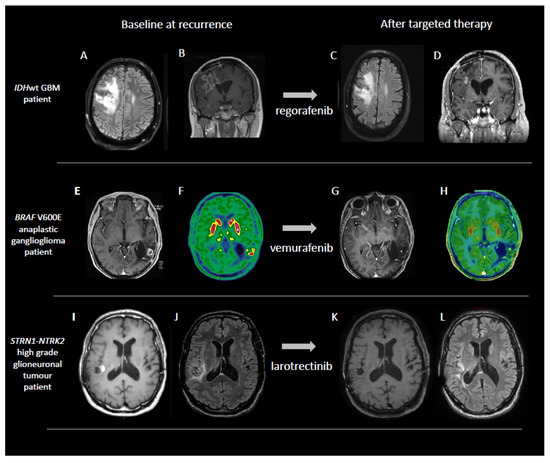
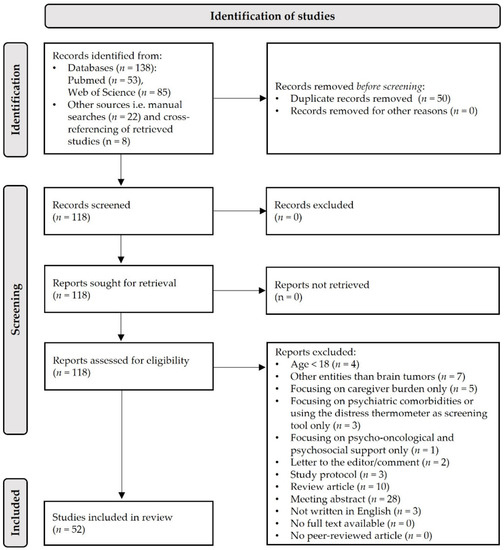
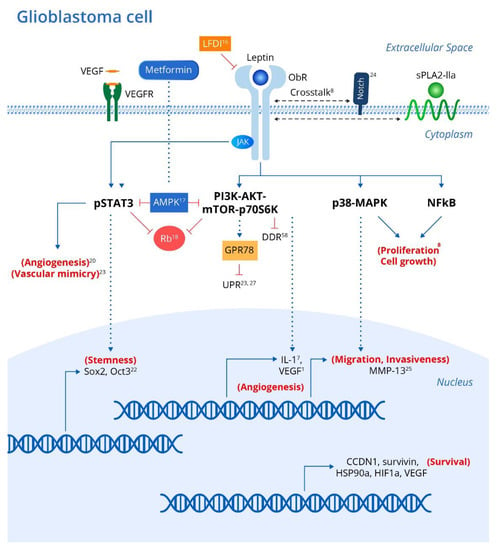
Primary and secondary brain tumors represent heterogeneous and aggressive diseases. Despite growing knowledge of the molecular changes responsible for tumor development, glioblastoma and other brain tumors such as low grade gliomas, meningioma, and brain metastases remain neoplasms with unmet medical needs. In recent years, new treatment approaches have been emerging, such as immunotherapy, targeted therapy. and their combination with radiotherapy, particularly in brain metastases from melanoma, lung, and renal cancers. Moreover, new molecular characteristics are emerging as predictors of therapy efficacy. Nonetheless, new approaches for neuroradiological assessment such as magnetic resonance imaging and positron emission tomography are integrated into diagnostic and follow up steps.
This Special Issue will cover all aspects of primary and secondary (brain metastases) brain tumors, including original research on advanced imaging, molecular characteristics, current and experimental treatment options, supportive care, neurocognitive functions, and quality of life. Expert opinions, systematic reviews, and meta-analyses are also welcome.
Dr. Giuseppe Lombardi
Prof. Dr. Alberto Feletti
Dr. Anna Luisa Di Stefano
Guest Editors
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Cancers is an international peer-reviewed open access semimonthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2900 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- primary brain tumors
- brain metastases
- glioblastoma
- meningioma
- imaging
- neuro-oncology