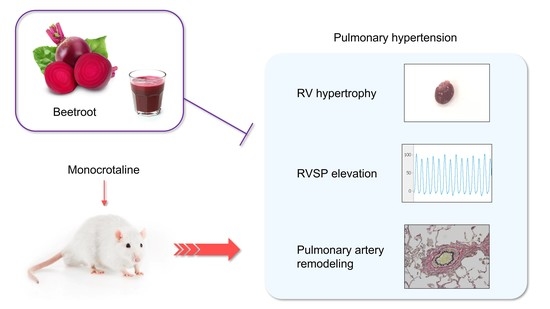
Ameliorative Effects of Beetroot Juice Supplementation on Monocrotaline-Induced Pulmonary Hypertension in Rats
Abstract
:1. Introduction
2. Materials and Methods
2.1. Animals
2.2. Experimental Design
2.3. Hemodynamic Measurement and Sample Collection
2.4. Histological Examination
2.5. Nitrite and Nitrate Measurement
2.6. TBARS Measurement
2.7. Statistics
3. Results
3.1. Morphological and Hemodynamic Parameters
3.2. Right Ventricle Hypertrophy
3.3. Right Ventricle Dysfunction
3.4. Pulmonary Vascular Remodeling
3.5. Nitrite and Nitrate Levels
3.6. Oxidative Stress
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mandras, S.A.; Mehta, H.S.; Vaidya, A. Pulmonary Hypertension: A Brief Guide for Clinicians. Mayo Clin. Proc. 2020, 95, 1978–1988. [Google Scholar] [CrossRef] [PubMed]
- Klinger, J.R.; Abman, S.H.; Gladwin, M.T. Nitric oxide deficiency and endothelial dysfunction in pulmonary arterial hypertension. Am. J. Respir. Crit. Care Med. 2013, 188, 639–646. [Google Scholar] [CrossRef] [PubMed]
- Abman, S.H. Inhaled nitric oxide for the treatment of pulmonary arterial hypertension. In Handbook of Experimental Pharmacology; Springer: Berlin/Heidelberg, Germany, 2013; Volume 218, pp. 257–276. [Google Scholar] [CrossRef]
- Triposkiadis, F.; Xanthopoulos, A.; Skoularigis, J.; Starling, R.C. Therapeutic augmentation of NO-sGC-cGMP signalling: Lessons learned from pulmonary arterial hypertension and heart failure. Heart Fail. Rev. 2022, 27, 1991–2003. [Google Scholar] [CrossRef]
- Kapil, V.; Khambata, R.S.; Jones, D.A.; Rathod, K.; Primus, C.; Massimo, G.; Fukuto, J.M.; Ahluwalia, A. The Noncanonical Pathway for In Vivo Nitric Oxide Generation: The Nitrate-Nitrite-Nitric Oxide Pathway. Pharmacol. Rev. 2020, 72, 692–766. [Google Scholar] [CrossRef] [PubMed]
- Carlström, M.; Lundberg, J.O.; Weitzberg, E. Mechanisms underlying blood pressure reduction by dietary inorganic nitrate. Acta Physiol. 2018, 224, e13080. [Google Scholar] [CrossRef] [PubMed]
- Guimaraes, D.A.; Batista, R.I.M.; Tanus-Santos, J.E. Nitrate and nitrite-based therapy to attenuate cardiovascular remodelling in arterial hypertension. Basic Clin. Pharmacol. Toxicol. 2021, 128, 9–17. [Google Scholar] [CrossRef]
- Zuckerbraun, B.S.; Shiva, S.; Ifedigbo, E.; Mathier, M.A.; Mollen, K.P.; Rao, J.; Bauer, P.M.; Choi, J.J.; Curtis, E.; Choi, A.M.; et al. Nitrite potently inhibits hypoxic and inflammatory pulmonary arterial hypertension and smooth muscle proliferation via xanthine oxidoreductase-dependent nitric oxide generation. Circulation 2010, 121, 98–109. [Google Scholar] [CrossRef] [PubMed]
- Pankey, E.A.; Badejo, A.M.; Casey, D.B.; Lasker, G.F.; Riehl, R.A.; Murthy, S.N.; Nossaman, B.D.; Kadowitz, P.J. Effect of chronic sodium nitrite therapy on monocrotaline-induced pulmonary hypertension. Nitric Oxide 2012, 27, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Kmecova, Z.; Malikova, E.; Krenek, P.; Klimas, J. Effects of nitrate therapy in monocrotaline-induced pulmonary hypertension in rats. J. Hypertens. 2017, 35, e278. [Google Scholar] [CrossRef]
- Tawa, M.; Furukawa, T.; Tongu, H.; Sugihara, M.; Taguwa, S.; Yamanaka, M.; Yano, Y.; Matsumori, H.; Kitada, R.; Sawano, T.; et al. Stimulation of nitric oxide-sensitive soluble guanylate cyclase in monocrotaline-induced pulmonary hypertensive rats. Life Sci. 2018, 203, 203–209. [Google Scholar] [CrossRef]
- Chen, L.; Zhu, Y.; Hu, Z.; Wu, S.; Jin, C. Beetroot as a functional food with huge health benefits: Antioxidant, antitumor, physical function, and chronic metabolomics activity. Food Sci. Nutr. 2021, 9, 6406–6420. [Google Scholar] [CrossRef]
- Mills, C.E.; Khatri, J.; Maskell, P.; Odongerel, C.; Webb, A.J. It is rocket science—Why dietary nitrate is hard to ‘beet’! Part II: Further mechanisms and therapeutic potential of the nitrate-nitrite-NO pathway. Br. J. Clin. Pharmacol. 2017, 83, 140–151. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Benjamim, C.J.R.; Porto, A.A.; Valenti, V.E.; Sobrinho, A.C.D.S.; Garner, D.M.; Gualano, B.; Bueno, C.R., Jr. Nitrate Derived From Beetroot Juice Lowers Blood Pressure in Patients With Arterial Hypertension: A Systematic Review and Meta-Analysis. Front. Nutr. 2022, 9, 823039. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, S.K.; Woessner, M.N.; Holmes, M.J.; Belbis, M.D.; Carlström, M.; Weitzberg, E.; Allen, J.D.; Hirai, D.M. Effects of inorganic nitrate supplementation on cardiovascular function and exercise tolerance in heart failure. J. Appl. Physiol. 2021, 130, 914–922. [Google Scholar] [CrossRef]
- Alsulayyim, A.S.; Alasmari, A.M.; Alghamdi, S.M.; Polkey, M.I.; Hopkinson, N.S. Impact of dietary nitrate supplementation on exercise capacity and cardiovascular parameters in chronic respiratory disease: A systematic review and meta-analysis. BMJ Open Respir. Res. 2021, 8, e000948. [Google Scholar] [CrossRef] [PubMed]
- Tawa, M.; Yano, Y.; Yamanaka, M.; Sawano, T.; Iesaki, K.; Murata, Y.; Tanaka, R.; Nakagawa, K.; Ohkita, M.; Matsumura, Y. Effects of Beet Juice Supplementation on Monocrotaline-Induced Pulmonary Hypertension in Rats. Am. J. Hypertens. 2019, 32, 216–222. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tawa, M.; Nagata, R.; Sumi, Y.; Nakagawa, K.; Sawano, T.; Ohkita, M.; Matsumura, Y. Preventive effects of nitrate-rich beetroot juice supplementation on monocrotaline-induced pulmonary hypertension in rats. PLoS ONE 2021, 16, e0249816. [Google Scholar] [CrossRef]
- Sun, X.; Ku, D.D. Selective right, but not left, coronary endothelial dysfunction precedes development of pulmonary hypertension and right heart hypertrophy in rats. Am. J. Physiol. Heart Circ. Physiol. 2006, 290, H758–H764. [Google Scholar] [CrossRef] [Green Version]
- Suzuki, R.; Maehara, R.; Kobuchi, S.; Tanaka, R.; Ohkita, M.; Matsumura, Y. Beneficial effects of γ-aminobutyric acid on right ventricular pressure and pulmonary vascular remodeling in experimental pulmonary hypertension. Life Sci. 2012, 91, 693–698. [Google Scholar] [CrossRef]
- Liu, F.; Haeger, C.M.; Dieffenbach, P.B.; Sicard, D.; Chrobak, I.; Coronata, A.M.; Suárez Velandia, M.M.; Vitali, S.; Colas, R.A.; Norris, P.C.; et al. Distal vessel stiffening is an early and pivotal mechanobiological regulator of vascular remodeling and pulmonary hypertension. JCI Insight 2016, 1, e86987. [Google Scholar] [CrossRef] [Green Version]
- Zimmer, A.; Teixeira, R.B.; Constantin, R.L.; Campos-Carraro, C.; Aparicio Cordero, E.A.; Ortiz, V.D.; Donatti, L.; Gonzalez, E.; Bahr, A.C.; Visioli, F.; et al. The progression of pulmonary arterial hypertension induced by monocrotaline is characterized by lung nitrosative and oxidative stress, and impaired pulmonary artery reactivity. Eur. J. Pharmacol. 2021, 891, 173699. [Google Scholar] [CrossRef] [PubMed]
- Wilson, D.W.; Segall, H.J.; Pan, L.C.; Lamé, M.W.; Estep, J.E.; Morin, D. Mechanisms and pathology of monocrotaline pulmonary toxicity. Crit. Rev. Toxicol. 1992, 22, 307–325. [Google Scholar] [CrossRef] [PubMed]
- Gillespie, M.N.; Goldblum, S.E.; Cohen, D.A.; McClain, C.J. Interleukin 1 bioactivity in the lungs of rats with monocrotaline-induced pulmonary hypertension. Proc. Soc. Exp. Biol. Med. 1988, 187, 26–32. [Google Scholar] [CrossRef] [PubMed]
- Kodama, K.; Adachi, H. Improvement of mortality by long-term E4010 treatment in monocrotaline-induced pulmonary hypertensive rats. J. Pharmacol. Exp. Ther. 1999, 290, 748–752. [Google Scholar] [PubMed]
- Yuyama, H.; Fujimori, A.; Sanagi, M.; Koakutsu, A.; Sudoh, K.; Sasamata, M.; Miyata, K. The orally active nonpeptide selective endothelin ETA receptor antagonist YM598 prevents and reverses the development of pulmonary hypertension in monocrotaline-treated rats. Eur. J. Pharmacol. 2004, 496, 129–139. [Google Scholar] [CrossRef]
- Cui, B.; Cheng, Y.S.; Dai, D.Z.; Li, N.; Zhang, T.T.; Dai, Y. CPU0213, a non-selective ETA/ETB receptor antagonist, improves pulmonary arteriolar remodeling of monocrotaline-induced pulmonary hypertension in rats. Clin. Exp. Pharmacol. Physiol. 2009, 36, 169–175. [Google Scholar] [CrossRef]
- Ogawa, A.; Sakao, S.; Tanabe, N.; Matsubara, H.; Tatsumi, K. Use of vasodilators for the treatment of pulmonary veno-occlusive disease and pulmonary capillary hemangiomatosis: A systematic review. Respir. Investig. 2019, 57, 183–190. [Google Scholar] [CrossRef]
- Wilson, D.W.; Segall, H.J.; Pan, L.C.; Dunston, S.K. Progressive inflammatory and structural changes in the pulmonary vasculature of monocrotaline-treated rats. Microvasc. Res. 1989, 38, 57–80. [Google Scholar] [CrossRef]
- Dos Santos Baião, D.; Vieira Teixeira da Silva, D.; Margaret Flosi Paschoalin, V. A Narrative Review on Dietary Strategies to Provide Nitric Oxide as a Non-Drug Cardiovascular Disease Therapy: Beetroot Formulations-A Smart Nutritional Intervention. Foods 2021, 10, 859. [Google Scholar] [CrossRef]
- de Jong, J.W.; Schoemaker, R.G.; de Jonge, R.; Bernocchi, P.; Keijzer, E.; Harrison, R.; Sharma, H.S.; Ceconi, C. Enhanced expression and activity of xanthine oxidoreductase in the failing heart. J. Mol. Cell Cardiol. 2000, 32, 2083–2089. [Google Scholar] [CrossRef]
- Farahmand, F.; Hill, M.F.; Singal, P.K. Antioxidant and oxidative stress changes in experimental cor pulmonale. Mol. Cell. Biochem. 2004, 260, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Redout, E.M.; Wagner, M.J.; Zuidwijk, M.J.; Boer, C.; Musters, R.J.; van Hardeveld, C.; Paulus, W.J.; Simonides, W.S. Right-ventricular failure is associated with increased mitochondrial complex II activity and production of reactive oxygen species. Cardiovasc. Res. 2007, 75, 770–781. [Google Scholar] [CrossRef] [PubMed]
- Steven, S.; Oelze, M.; Brandt, M.; Ullmann, E.; Kröller-Schön, S.; Heeren, T.; Tran, L.P.; Daub, S.; Dib, M.; Stalleicken, D.; et al. Pentaerythritol Tetranitrate In Vivo Treatment Improves Oxidative Stress and Vascular Dysfunction by Suppression of Endothelin-1 Signaling in Monocrotaline-Induced Pulmonary Hypertension. Oxid. Med. Cell. Longev. 2017, 2017, 4353462. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Donnell, V.B.; Freeman, B.A. Interactions between nitric oxide and lipid oxidation pathways: Implications for vascular disease. Circ. Res. 2001, 88, 12–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahmed, L.A.; Obaid, A.A.; Zaki, H.F.; Agha, A.M. Naringenin adds to the protective effect of L-arginine in monocrotaline-induced pulmonary hypertension in rats: Favorable modulation of oxidative stress, inflammation and nitric oxide. Eur. J. Pharm. Sci. 2014, 62, 161–170. [Google Scholar] [CrossRef]
- Lacerda, D.; Türck, P.; Campos-Carraro, C.; Hickmann, A.; Ortiz, V.; Bianchi, S.; Belló-Klein, A.; de Castro, A.L.; Bassani, V.L.; Araujo, A.S.D.R. Pterostilbene improves cardiac function in a rat model of right heart failure through modulation of calcium handling proteins and oxidative stress. Appl. Physiol. Nutr. Metab. 2020, 45, 987–995. [Google Scholar] [CrossRef]
- Farahmand, F.; Malik, A.; Sharma, A.; Bagchi, A.K.; Singal, P.K. Role of oxidative stress versus lipids in monocrotaline-induced pulmonary hypertension and right heart failure. Physiol. Rep. 2021, 9, e15090. [Google Scholar] [CrossRef]
- Parker, J.D.; Farrell, B.; Fenton, T.; Cohanim, M.; Parker, J.O. Counter-regulatory responses to continuous and intermittent therapy with nitroglycerin. Circulation 1991, 84, 2336–2345. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Irlbeck, M.; Muhling, O.; Iwai, T.; Zimmer, H.G. Different response of the rat left and right heart to norepinephrine. Cardiovasc. Res. 1996, 31, 157–162. [Google Scholar] [CrossRef]
- Tucker, A.; Bryant, S.E.; Frost, H.H.; Migally, N. Chemical sympathectomy and serotonin inhibition reduce monocrotaline-induced right ventricular hypertrophy in rats. Can. J. Physiol. Pharmacol. 1983, 61, 356–362. [Google Scholar] [CrossRef]
- Li, Z.C.; Zhang, F.Q.; Song, J.C.; Mei, Q.B.; Zhao, D.H. Therapeutic effects of DCDDP, a calcium channel blocker, on chronic pulmonary hypertension in rat. J. Appl. Physiol. 2002, 92, 997–1003. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vignozzi, L.; Morelli, A.; Cellai, I.; Filippi, S.; Comeglio, P.; Sarchielli, E.; Maneschi, E.; Vannelli, G.B.; Adorini, L.; Maggi, M. Cardiopulmonary protective effects of the selective FXR agonist obeticholic acid in the rat model of monocrotaline-induced pulmonary hypertension. J. Steroid Biochem. Mol. Biol. 2017, 165, 277–292. [Google Scholar] [CrossRef] [PubMed]
- Türck, P.; Salvador, I.S.; Campos-Carraro, C.; Ortiz, V.; Bahr, A.; Andrades, M.; Belló-Klein, A.; da Rosa Araujo, A.S. Blueberry extract improves redox balance and functional parameters in the right ventricle from rats with pulmonary arterial hypertension. Eur. J. Nutr. 2022, 61, 373–386. [Google Scholar] [CrossRef] [PubMed]
- Zamani, H.; de Joode, M.E.J.R.; Hossein, I.J.; Henckens, N.F.T.; Guggeis, M.A.; Berends, J.E.; de Kok, T.M.C.M.; van Breda, S.G.J. The benefits and risks of beetroot juice consumption: A systematic review. Crit. Rev. Food Sci. Nutr. 2021, 61, 788–804. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sharp, J.; Farha, S.; Park, M.M.; Comhair, S.A.; Lundgrin, E.L.; Tang, W.H.; Bongard, R.D.; Merker, M.P.; Erzurum, S.C. Coenzyme Q supplementation in pulmonary arterial hypertension. Redox Biol. 2014, 2, 884–891. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sharif Kashani, B.; Tahmaseb Pour, P.; Malekmohammad, M.; Behzadnia, N.; Sheybani-Afshar, F.; Fakhri, M.; Chaibakhsh, S.; Naghashzadeh, F.; Aidenlou, S. Oral l-citrulline malate in patients with idiopathic pulmonary arterial hypertension and Eisenmenger Syndrome: A clinical trial. J. Cardiol. 2014, 64, 231–235. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olsson, K.M.; Fuge, J.; Brod, T.; Kamp, J.C.; Schmitto, J.; Kempf, T.; Bauersachs, J.; Hoeper, M.M. Oral iron supplementation with ferric maltol in patients with pulmonary hypertension. Eur. Respir. J. 2020, 56, 2000616. [Google Scholar] [CrossRef]
- Chen, Y.; Lu, W.; Yang, K.; Duan, X.; Li, M.; Chen, X.; Zhang, J.; Kuang, M.; Liu, S.; Wu, X.; et al. Tetramethylpyrazine: A promising drug for the treatment of pulmonary hypertension. Br. J. Pharmacol. 2020, 177, 2743–2764. [Google Scholar] [CrossRef]
- Henrohn, D.; Björkstrand, K.; Lundberg, J.O.; Granstam, S.O.; Baron, T.; Ingimarsdóttir, I.J.; Hedenström, H.; Malinovschi, A.; Wernroth, M.L.; Jansson, M.; et al. Effects of Oral Supplementation with Nitrate-Rich Beetroot Juice in Patients with Pulmonary Arterial Hypertension-Results From BEET-PAH, an Exploratory Randomized, Double-Blind, Placebo-Controlled, Crossover Study. J. Card. Fail. 2018, 24, 640–653. [Google Scholar] [CrossRef]





| Parameters | Sham (n = 6) | MCT (n = 9) | BRJ-L (n = 6) | BRJ-H (n = 6) |
|---|---|---|---|---|
| BW (g) | 416 ± 10 ** | 348 ± 5 | 366 ± 9 | 337 ± 10 |
| HW/BW (g/kg) | 2.84 ± 0.14 ** | 3.57 ± 0.11 | 2.98 ± 0.11 ** | 3.70 ± 0.19 |
| (LV + S)W/BW (g/kg) | 1.94 ± 0.02 | 2.16 ± 0.04 | 2.01 ± 0.06 | 2.18 ± 0.10 |
| LW/BW (g/kg) | 3.32 ± 0.19 ** | 6.39 ± 0.17 | 6.10 ± 0.38 | 6.98 ± 0.33 |
| HR (bpm) | 405 ± 20 * | 324 ± 18 | 353 ± 22 | 325 ± 32 |
| MAP (mmHg) | 119 ± 7 | 112 ± 7 | 112 ± 5 | 105 ± 4 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tawa, M.; Nagano, J.; Kitama, J.; Abe, S.; Fujita, A.; Nakagawa, K.; Ohkita, M. Ameliorative Effects of Beetroot Juice Supplementation on Monocrotaline-Induced Pulmonary Hypertension in Rats. Future Pharmacol. 2022, 2, 547-557. https://doi.org/10.3390/futurepharmacol2040033
Tawa M, Nagano J, Kitama J, Abe S, Fujita A, Nakagawa K, Ohkita M. Ameliorative Effects of Beetroot Juice Supplementation on Monocrotaline-Induced Pulmonary Hypertension in Rats. Future Pharmacology. 2022; 2(4):547-557. https://doi.org/10.3390/futurepharmacol2040033
Chicago/Turabian StyleTawa, Masashi, Junya Nagano, Junpei Kitama, Shunto Abe, Ako Fujita, Keisuke Nakagawa, and Mamoru Ohkita. 2022. "Ameliorative Effects of Beetroot Juice Supplementation on Monocrotaline-Induced Pulmonary Hypertension in Rats" Future Pharmacology 2, no. 4: 547-557. https://doi.org/10.3390/futurepharmacol2040033