Bioactive Polyurethane–Poly(ethylene Glycol) Diacrylate Hydrogels for Applications in Tissue Engineering
Abstract
:1. Introduction
2. Results and Discussion
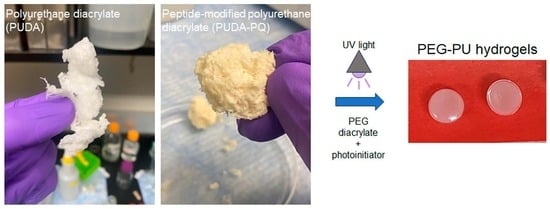
2.1. Preparation of Photocrosslinked PU Films and PEG–PU Hydrogels
2.2. Mechanical Testing
2.3. Hydrogel Swelling and Degradation
2.4. Cell Adhesion and Viability
3. Conclusions
4. Materials and Methods
4.1. Synthesis of Polyurethane Diacrylate
4.2. Synthesis of Peptide-Modified Polyurethane Diacrylate
4.3. Synthesis PEGDA and PEG–Peptide and –Protein Conjugates
4.4. Preparation of PU Films and PEG–PU Hydrogels
4.5. Mechanical Testing
4.6. Swelling and Degradation Studies
4.7. Cell Maintenance
4.8. Cell Adhesion and Viability Studies
4.9. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Peppas, N.A. Hydrogels in Medicine and Pharmacy; CRC Press: Boca Raton, FL, USA, 1986; Volume 1. [Google Scholar]
- Metters, A.; Hubbell, J. Network Formation and Degradation Behavior of Hydrogels Formed by Michael-Type Addition Reactions. Biomacromolecules 2005, 6, 290–301. [Google Scholar] [CrossRef]
- Tibbitt, M.W.; Anseth, K.S. Hydrogels as Extracellular Matrix Mimics for 3D Cell Culture. Biotechnol. Bioeng. 2009, 103, 655–663. [Google Scholar] [CrossRef]
- Unal, A.Z.; West, J.L. Synthetic ECM: Bioactive Synthetic Hydrogels for 3D Tissue Engineering. Bioconjugate Chem. 2020, 31, 2253–2271. [Google Scholar] [CrossRef]
- Catoira, M.C.; Fusaro, L.; Francesco, D.; Ramella, M.; Boccafoschi, F. Overview of Natural Hydrogels for Regenerative Medicine Applications. J. Mater. Sci. Mater. Med. 2019, 30, 115. [Google Scholar] [CrossRef]
- Shi, Z.; Gao, X.; Ullah, M.W.; Li, S.; Wang, Q.; Yang, G. Electroconductive Natural Polymer-Based Hydrogels. Biomaterials 2016, 111, 40–54. [Google Scholar] [CrossRef]
- Madduma-Bandarage, U.S.K.; Madihally, S.V. Synthetic Hydrogels: Synthesis, Novel Trends, and Applications. J. Appl. Polym. Sci. 2020, 138, 50376. [Google Scholar] [CrossRef]
- Liu, Y.; Song, S.; Liu, S.; Zhu, X.; Wang, P. Application of Nanomaterial in Hydrogels Related to Wound Healing. J. Nanomater. 2022, 2022, 4656037. [Google Scholar] [CrossRef]
- Fu, J.; Panhuis, M. Hydrogel Properties and Applications. J. Mater. Chem. B 2019, 7, 1523–1525. [Google Scholar] [CrossRef]
- Zainal, S.H.; Mohd, N.H.; Suhaili, N.; Anuar, F.H.; Lazim, A.M.; Othaman, R. Preparation of Cellulose-Based Hydrogel: A Review. J. Mater. Res. Technol. 2021, 10, 935–952. [Google Scholar] [CrossRef]
- Yazdi, M.K.; Vatanpour, V.; Taghizadeh, A.; Taghizadeh, M.; Ganjali, M.R.; Munir, M.T.; Habibzadeh, S.; Saeb, M.R.; Ghaedi, M. Hydrogel Membranes: A Review. Mater. Sci. Eng. C 2020, 114, 111023. [Google Scholar] [CrossRef]
- Caló, E.; Khutoryanskiy, V.V. Biomedical Applications of Hydrogels: A Review of Patents and Commercial Products. Eur. Polym. J. 2015, 65, 252–267. [Google Scholar] [CrossRef]
- Correa, S.; Grosskopf, A.K.; Lopez Hernandez, H.; Chan, D.; Yu, A.C.; Stapleton, L.M.; Appel, E.A. Translational Applications of Hydrogels. Chem. Rev. 2021, 121, 11385–11457. [Google Scholar] [CrossRef]
- Laurano, R.; Boffito, M.; Abrami, M.; Grassi, M.; Zoso, A.; Chiono, V.; Ciardelli, G. Dual Stimuli-Responsive Polyurethane-Based Hydrogels as Smart Drug Delivery Carriers for the Advanced Treatment of Chronic Skin Wounds. Bioact. Mater. 2021, 6, 3013–3024. [Google Scholar] [CrossRef] [PubMed]
- Pinelli, F.; Magagnin, L.; Rossi, F. Progress in Hydrogels for Sensing Applications: A Review. Mater. Today Chem. 2020, 17, 100317. [Google Scholar] [CrossRef]
- Tariq, A.; Arif, Z.U.; Khalid, M.Y.; Hossain, M.; Rasool, P.I.; Umer, R.; Ramakrishna, S. Recent Advances in the Additive Manufacturing of Stimuli-Responsive Soft Polymers. Adv. Eng. Mater. 2023, 25, 2301074. [Google Scholar] [CrossRef]
- Siwal, S.S.; Mishra, K.; Saini, A.K.; Alsanie, W.F.; Kovalcik, A.; Thakur, V.K. Additive Manufacturing of Bio-Based Hydrogel Composites: Recent Advances. J. Polym. Environ. 2022, 30, 4501–4516. [Google Scholar] [CrossRef]
- Rosa, E.; Gallo, E.; Sibillano, T.; Giannini, C.; Rizzuti, S.; Gianolio, E.; Scognamiglio, P.L.; Morelli, G.; Accardo, A.; Diaferia, C. Incorporation of PEG Diacrylates (PEGDA) Generates Hybrid Fmoc-FF Hydrogel Matrices. Gels 2022, 8, 831. [Google Scholar] [CrossRef]
- Naureen, B.; Haseeb, A.S.M.A.; Basirun, W.J.; Muhamad, F. Recent Advances in Tissue Engineering Scaffolds Based on Polyurethane and Modified Polyurethane. Mater. Sci. Eng. C 2021, 118, 111228. [Google Scholar] [CrossRef]
- Jun, H.-W.; Taite, L.J.; West, J.L. Nitric Oxide-Producing Polyurethanes. Biomacromolecules 2005, 6, 838–844. [Google Scholar] [CrossRef]
- Taite, L.J.; Yang, P.; Jun, H.W.; West, J.L. Nitric Oxide-Releasing Polyurethane-PEG Copolymer Containing the YIGSR Peptide Promotes Endothelialization with Decreased Platelet Adhesion. J. Biomed. Mater. Res. B Appl. Biomater. 2008, 84, 108–116. [Google Scholar] [CrossRef]
- Dumas, J.E.; Davis, T.; Holt, G.E.; Yoshii, T.; Perrien, D.S.; Nyman, J.S.; Boyce, T.; Guelcher, S.A. Synthesis, Characterization, and Remodeling of Weight-Bearing Allograft Bone/Polyurethane Composites in the Rabbit. Acta Biomater. 2010, 6, 2394–2406. [Google Scholar] [CrossRef]
- Dumas, J.E.; BrownBaer, P.B.; Prieto, E.M.; Guda, T.; Hale, R.G.; Wenke, J.C.; Guelcher, S.A. Injectable Reactive Biocomposites for Bone Healing in Critical-Size Rabbit Calvarial Defects. Biomed. Mater. 2012, 7, 024112. [Google Scholar] [CrossRef] [PubMed]
- Wienen, D.; Gries, T.; Cooper, S.L.; Heath, D.E. An Overview of Polyurethane Biomaterials and Their Use in Drug Delivery. J. Control Release 2023, 363, 376–388. [Google Scholar] [CrossRef] [PubMed]
- Wen, J.; Zhang, X.; Pan, M.; Yuan, J.; Jia, Z.; Zhu, L. A Robust, Tough and Multifunctional Polyurethane/Tannic Acid Hydrogel Fabricated by Physical-Chemical Dual Crosslinking. Polymers 2020, 12, 239. [Google Scholar] [CrossRef]
- Tang, Y.; Wang, H.; Liu, S.; Pu, L.; Hu, X.; Ding, J.; Xu, G.; Xu, W.; Xiang, S.; Yuan, Z. A Review of Protein Hydrogels: Protein Assembly Mechanisms, Properties, and Biological Applications. Colloids Surf. B Biointerfaces 2022, 220, 112973. [Google Scholar] [CrossRef]
- Divakaran, A.V.; Azad, L.B.; Surwase, S.S.; Torris, A.T.A.; Badiger, M.V. Mechanically Tunable Curcumin Incorporated Polyurethane Hydrogels as Potential Biomaterials. Chem. Mater. 2016, 28, 2120–2130. [Google Scholar] [CrossRef]
- Yoon, S.; Chen, B. Modulating the Properties of Poly(Glycerol Sebacate)-Based Polyurethane Hydrogels Using an Organoclay. ACS Biomater. Sci. Eng. 2022, 8, 786–800. [Google Scholar] [CrossRef]
- Wendels, S.; Averous, L. Biobased Polyurethanes for Biomedical Applications. Bioact. Mater. 2021, 6, 1083–1106. [Google Scholar] [CrossRef]
- Mandru, M.; Bercea, M.; Gradinaru, L.M.; Ciobanu, C.; Drobota, M.; Vlad, S.; Albulescu, R. Polyurethane/Poly (Vinyl Alcohol) Hydrogels: Preparation, Characterization and Drug Delivery. Eur. Polym. J. 2019, 118, 137–145. [Google Scholar] [CrossRef]
- Kamaci, M. Polyurethane-Based Hydrogels for Controlled Drug Delivery Applications. Eur. Polym. J. 2020, 123, 109444. [Google Scholar] [CrossRef]
- Noroozi, R.; Arif, Z.U.; Taghvaei, H.; Khalid, M.Y.; Sahbafar, H.; Hadi, A.; Sadeghianmaryan, A.; Chen, X. 3D and 4D Bioprinting Technologies: A Game Changer for the Biomedical Sector? Ann. Biomed. Eng. 2023, 51, 1683–1712. [Google Scholar] [CrossRef]
- Hakim Khalili, M.; Zhang, R.; Wilson, S.; Goel, S.; Impey, S.A.; Aria, A.I. Additive Manufacturing and Physicomechanical Characteristics of PEGDA Hydrogels: Recent Advances and Perspective for Tissue Engineering. Polymers 2023, 15, 2341. [Google Scholar] [CrossRef]
- Han, Y.; Lian, M.; Zhang, C.; Jia, B.; Wu, Q.; Sun, B.; Qiao, Z.; Sun, B.; Dai, K. Study on Bioactive PEGDA/ECM Hybrid Bi-Layered Hydrogel Scaffolds Fabricated by Electro-Writing for Cartilage Regeneration. Appl. Mater. Today 2022, 28, 101547. [Google Scholar] [CrossRef]
- Fu, J.; Wang, L.; Yu, H.; Haroon, M.; Haq, F.; Shi, W.; Wu, B.; Wang, L. Research Progress of UV-Curable Polyurethane Acrylate-Based Hardening Coatings. Prog. Org. Coat. 2019, 131, 82–99. [Google Scholar] [CrossRef]
- Yoon, J.; Cho, H.Y.; Shin, M.; Choi, H.K.; Lee, T.; Choi, J.W. Flexible Electrochemical Biosensors for Healthcare Monitoring. J. Mater. Chem. B 2020, 8, 7303–7318. [Google Scholar] [CrossRef]
- Warner, J.J.; Wang, P.; Mellor, W.M.; Hwang, H.H.; Park, J.H.; Pyo, S.-H.; Chen, S. 3D Printable Non-Isocyanate Polyurethanes with Tunable Material Properties. Polym. Chem. 2019, 10, 4665–4674. [Google Scholar] [CrossRef]
- Srivastava, A.; Agarwal, D.; Mistry, S.; Singh, J. UV Curable Polyurethane Acrylate Coatings for Metal Surfaces. Pigment. Resin. Technol. 2008, 37, 217–223. [Google Scholar] [CrossRef]
- Rao, L.; Zhou, H.; Li, T.; Li, C.; Duan, Y.Y. Polyethylene Glycol-Containing Polyurethane Hydrogel Coatings for Improving the Biocompatibility of Neural Electrodes. Acta Biomater. 2012, 8, 2233–2242. [Google Scholar] [CrossRef] [PubMed]
- Corneillie, S.; Lan, P.N.; Schacht, E.; Davies, M.; Shard, A.; Green, R.; Denyer, S.; Wassall, M.; Whitfield, H.; Choong, S. Polyethylene Glycol-Containing Polyurethanes for Biomedical Applications. Polym. Int. 1998, 46, 251–259. [Google Scholar] [CrossRef]
- Speidel, A.T.; Chivers, P.R.A.; Wood, C.S.; Roberts, D.A.; Correia, I.P.; Caravaca, A.S.; Chan, Y.K.V.; Hansel, C.S.; Heimgärtner, J.; Müller, E.; et al. Tailored Biocompatible Polyurethane-Poly(Ethylene Glycol) Hydrogels as a Versatile Nonfouling Biomaterial. Adv. Healthc. Mater. 2022, 11, 2201378. [Google Scholar] [CrossRef] [PubMed]
- Divakaran, A.V.; Torris AT, A.; Lele, A.K.; Badiger, M.V. Porous Poly(Ethylene Glycol)–Polyurethane Hydrogels as Potential Biomaterials. Polym. Int. 2015, 64, 397–404. [Google Scholar] [CrossRef]
- Breul, K.; Stengelin, E.; Urschbach, M.; Mondeshki, M.; Wüst, L.; Sirleaf, J.; Seitel, S.; Emt, T.; Pschierer, S.; Besenius, P.; et al. Cell Adhesion on UV-Crosslinked Polyurethane Gels with Adjustable Mechanical Strength and Thermoresponsiveness. Macromol. Rapid Commun. 2021, 42, 2100505. [Google Scholar] [CrossRef]
- Hahn, M.S.; Taite, L.J.; Moon, J.J.; Rowland, M.C.; Ruffino, K.A.; West, J.L. Photolithographic Patterning of Polyethylene Glycol Hydrogels. Biomaterials 2006, 27, 2519–2524. [Google Scholar] [CrossRef]
- Patel, D.; Vandromme, S.E.; Reid, M.E.; Taite, L.J. Synergistic Activity of Alphavbeta3 Integrins and the Elastin Binding Protein Enhance Cell-Matrix Interactions on Bioactive Hydrogel Surfaces. Biomacromolecules 2012, 13, 1420–1428. [Google Scholar] [CrossRef]
- Chapla, R.; Alhaj Abed, M.; West, J. Modulating Functionalized Poly(Ethylene Glycol) Diacrylate Hydrogel Mechanical Properties through Competitive Crosslinking Mechanics for Soft Tissue Applications. Polymers 2020, 12, 3000. [Google Scholar] [CrossRef]
- Taite, L.J.; Rowland, M.L.; Ruffino, K.A.; Smith, B.R.; Lawrence, M.B.; West, J.L. Bioactive Hydrogel Substrates: Probing Leukocyte Receptor-Ligand Interactions in Parallel Plate Flow Chamber Studies. Ann. Biomed. Eng. 2006, 34, 1705–1711. [Google Scholar] [CrossRef]
- Jun, H.; West, J. Development of a YIGSR-Peptide-Modified Polyurethaneurea to Enhance Endothelialization. J. Biomater. Sci. Polym. Ed. 2004, 15, 73–94. [Google Scholar] [CrossRef]
- Jun, H.W.; West, J.L. Modification of Polyurethaneurea with PEG and YIGSR Peptide to Enhance Endothelialization without Platelet Adhesion. J. Biomed. Mater. Res. B Appl. Biomater. 2005, 72, 131–139. [Google Scholar] [CrossRef]
- Jun, H.-W.; West, J.L. Endothelialization of Microporous YIGSR/PEG-Modified Polyurethaneurea. Tissue Eng. 2005, 11, 1133–1140. [Google Scholar] [CrossRef]
- Gill, B.J.; Gibbons, D.L.; Roudsari, L.C.; Saik, J.E.; Rizvi, Z.H.; Roybal, J.D.; Kurie, J.M.; West, J.L. A Synthetic Matrix with Independently Tunable Biochemistry and Mechanical Properties to Study Epithelial Morphogenesis and EMT in a Lung Adenocarcinoma Model. Cancer Res. 2012, 72, 6013–6023. [Google Scholar] [CrossRef]
- Katz, R.R.; West, J.L. Tunable PEG Hydrogels for Discerning Differential Tumor Cell Response to Biomechanical Cues. Adv. Biol. 2022, 6, 2200084. [Google Scholar] [CrossRef]
- Sawicki, L.A.; Kloxin, A.M. Design of Thiol–Ene Photoclick Hydrogels Using Facile Techniques for Cell Culture Applications. Biomater. Sci. 2014, 2, 1612–1626. [Google Scholar] [CrossRef]
- Schweller, R.M.; West, J.L. Encoding Hydrogel Mechanics via Network Cross-Linking Structure. ACS Biomater. Sci. Eng. 2015, 1, 335–344. [Google Scholar] [CrossRef]
- Leonard-Duke, J.; Bruce, A.C.; Peirce, S.M.; Taite, L.J. Variations in Mechanical Stiffness Alter Microvascular Sprouting and Stability in a PEG Hydrogel Model of Idiopathic Pulmonary Fibrosis. Microcirculation 2023, 30, e12817. [Google Scholar] [CrossRef]
- Huang, G.; Wang, L.; Wang, S.; Han, Y.; Wu, J.; Zhang, Q.; Xu, F.; Lu, T.J. Engineering Three-Dimensional Cell Mechanical Microenvironment with Hydrogels. Biofabrication 2012, 4, 042001. [Google Scholar] [CrossRef]
- Liu, J.; Zheng, H.; Poh, P.S.P.; Machens, H.-G.; Schilling, A.F. Hydrogels for Engineering of Perfusable Vascular Networks. Int. J. Mol. Sci. 2015, 16, 15997–16016. [Google Scholar] [CrossRef]
- Tejo-Otero, A.; Fenollosa-Artés, F.; Achaerandio, I.; Rey-Vinolas, S.; Buj-Corral, I.; Mateos-Timoneda, M.Á.; Engel, E. Soft-Tissue-Mimicking Using Hydrogels for the Development of Phantoms. Gels 2022, 8, 40. [Google Scholar] [CrossRef]
- Singh, S.; Kumar Paswan, K.; Kumar, A.; Gupta, V.; Sonker, M.; Ashhar Khan, M.; Kumar, A.; Shreyash, N. Recent Advancements in Polyurethane-Based Tissue Engineering. ACS Appl. Bio Mater. 2023, 6, 327–348. [Google Scholar] [CrossRef]
- Sarvazyan, A.; Tatarinov, A.; Sarvazyan, N. Ultrasonic Assessment of Tissue Hydration Status. Ultrasonics 2005, 43, 661–671. [Google Scholar] [CrossRef]
- Lozano, P.F.; Scholze, M.; Babian, C.; Scheidt, H.; Vielmuth, F.; Waschke, J.; Ondruschka, B.; Hammer, N. Water-Content Related Alterations in Macro and Micro Scale Tendon Biomechanics. Sci. Rep. 2019, 9, 7887. [Google Scholar] [CrossRef] [PubMed]
- Hubbell, J.A. Bioactive Biomaterials. Curr. Opin. Biotechnol. 1999, 10, 123–129. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Dargaville, B.L.; Hutmacher, D.W. Elucidating the Molecular Mechanisms for the Interaction of Water with Polyethylene Glycol-Based Hydrogels: Influence of Ionic Strength and Gel Network Structure. Polymers 2021, 13, 845. [Google Scholar] [CrossRef] [PubMed]
- Clevenger, A.J.; Jimenez-Vergara, A.C.; Tsai, E.H.; de Barros Righes, G.; Díaz-Lasprilla, A.M.; Ramírez-Caballero, G.E.; Munoz-Pinto, D.J. Growth Factor Binding Peptides in Poly (Ethylene Glycol) Diacrylate (PEGDA)-Based Hydrogels for an Improved Healing Response of Human Dermal Fibroblasts. Gels 2023, 9, 28. [Google Scholar] [CrossRef] [PubMed]
- Hsu, S.-H.; Chen, C.-W.; Hung, K.-C.; Tsai, Y.-C.; Li, S. Thermo-Responsive Polyurethane Hydrogels Based on Poly(ε-Caprolactone) Diol and Amphiphilic Polylactide-Poly(Ethylene Glycol) Block Copolymers. Polymers 2016, 8, 252. [Google Scholar] [CrossRef]
- Burdick, J.A.; Anseth, K.S. Photoencapsulation of Osteoblasts in Injectable RGD-Modified PEG Hydrogels for Bone Tissue Engineering. Biomaterials 2002, 23, 4315–4323. [Google Scholar] [CrossRef]
- Moon, J.J.; Hahn, M.S.; Kim, I.; Nsiah, B.A.; West, J.L. Micropatterning of Poly(Ethylene Glycol) Diacrylate Hydrogels with Biomolecules to Regulate and Guide Endothelial Morphogenesis. Tissue Eng. Part. A 2009, 15, 579–585. [Google Scholar] [CrossRef]
- Chapla, R.; Hammer, J.A.; West, J.L. Adding Dynamic Biomolecule Signaling to Hydrogel Systems via Tethered Photolabile Cell-Adhesive Proteins. ACS Biomater. Sci. Eng. 2022, 8, 208–217. [Google Scholar] [CrossRef]
- Ali, S.; Saik, J.E.; Gould, D.J.; Dickinson, M.E.; West, J.L. Immobilization of Cell-Adhesive Laminin Peptides in Degradable PEGDA Hydrogels Influences Endothelial Cell Tubulogenesis. Biores. Open Access 2013, 2, 241–249. [Google Scholar] [CrossRef]
- DeLong, S.A.; Gobin, A.S.; West, J.L. Covalent Immobilization of RGDS on Hydrogel Surfaces to Direct Cell Alignment and Migration. J. Control. Release 2005, 109, 139–148. [Google Scholar] [CrossRef]
- Gobin, A.S.; West, J.L. Cell Migration through Defined, Synthetic ECM Analogs. FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol. 2002, 16, 751–753. [Google Scholar] [CrossRef]
- Janmey, P.A.; Hinz, B.; McCulloch, C.A. Physics and Physiology of Cell Spreading in Two and Three Dimensions. Physiology 2021, 36, 382–391. [Google Scholar] [CrossRef] [PubMed]
- Li, K.; Li, Y.; Hu, J.; Zhang, Y.; Yang, Z.; Peng, S.; Wu, L.; Weng, Z. Waterborne Polyurethane Acrylates Preparation towards 3D Printing for Sewage Treatment. Materials 2022, 15, 3319. [Google Scholar] [CrossRef] [PubMed]
- Moon, J.J.; Saik, J.E.; Poché, R.A.; Leslie-Barbick, J.E.; Lee, S.H.; Smith, A.A.; Dickinson, M.E.; West, J.L. Biomimetic Hydrogels with Pro-Angiogenic Properties. Biomaterials 2010, 31, 3840–3847. [Google Scholar] [CrossRef] [PubMed]






Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yuan, Y.; Tyson, C.; Szyniec, A.; Agro, S.; Tavakol, T.N.; Harmon, A.; Lampkins, D.; Pearson, L.; Dumas, J.E.; Taite, L.J. Bioactive Polyurethane–Poly(ethylene Glycol) Diacrylate Hydrogels for Applications in Tissue Engineering. Gels 2024, 10, 108. https://doi.org/10.3390/gels10020108
Yuan Y, Tyson C, Szyniec A, Agro S, Tavakol TN, Harmon A, Lampkins D, Pearson L, Dumas JE, Taite LJ. Bioactive Polyurethane–Poly(ethylene Glycol) Diacrylate Hydrogels for Applications in Tissue Engineering. Gels. 2024; 10(2):108. https://doi.org/10.3390/gels10020108
Chicago/Turabian StyleYuan, Yixuan, Caleb Tyson, Annika Szyniec, Samuel Agro, Tara N. Tavakol, Alexander Harmon, DessaRae Lampkins, Lauran Pearson, Jerald E. Dumas, and Lakeshia J. Taite. 2024. "Bioactive Polyurethane–Poly(ethylene Glycol) Diacrylate Hydrogels for Applications in Tissue Engineering" Gels 10, no. 2: 108. https://doi.org/10.3390/gels10020108