Mechanical Behavior of Repaired Monolithic Crowns: A 3D Finite Element Analysis
Abstract
:1. Introduction
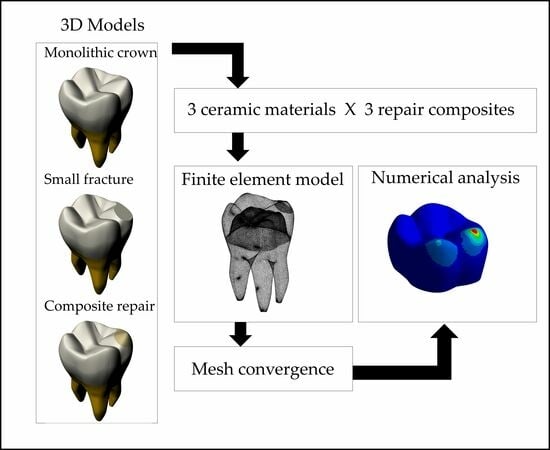
2. Materials and Methods
2.1. Finite Element Analysis (FEA)
2.2. In Vitro Shear Bond Strength Test
2.3. Statistical Analysis
2.4. Risk of Failure Measurement
3. Results
3.1. Maximum Tensile and Shear Stresses
3.2. In Vitro Shear Bond Strength Test
3.3. Risk of Failure
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Valenti, C.; Federici, M.I.; Masciotti, F.; Marinucci, L.; Xhimitiku, I.; Cianetti, S.; Pagano, S. Mechanical properties of 3D-printed prosthetic materials compared with milled and conventional processing: A systematic review and meta-analysis of in vitro studies. J. Prosthet. Dent. 2022, in press. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, K.; Harada, A.; Inagaki, R.; Kanno, T.; Niwano, Y.; Milleding, P.; Örtengren, U. Fracture resistance of monolithic zirconia molar crowns with reduced thickness. Acta Odontol. Scand. 2015, 73, 602–608. [Google Scholar] [CrossRef] [PubMed]
- de Lima, L.C.; Miranda, J.S.; de Carvalho, R.L.A.; de Pinho Barcellos, A.S.; Amaral, M.; Kimpara, E.T. Influence of Substrate, Cement and Aging on the Biaxial Flexural Strength of Lithium Disilicate. Braz. Dent. Sci. 2023, 26, e3923. [Google Scholar] [CrossRef]
- Blatz, M.B.; Vonderheide, M.; Conejo, J. The Effect of Resin Bonding on Long-Term Sucess of High-Strength Ceramics. J. Dent. Res. 2018, 97, 132–139. [Google Scholar] [CrossRef] [PubMed]
- Stawarczyk, B.; Keul, C.; Eichberger, M.; Figge, D.; Edelhoff, D.; Lümkemann, N. Three generations of zirconia: From veneered to monolithic. Part I. Quintessence Int. 2017, 48, 369–380. [Google Scholar] [CrossRef]
- Pjetursson, B.E.; Sailer, I.; Latyshev, A.; Rabel, K.; Kohal, R.J.; Karasan, D. A systematic review and meta-analysis evaluating the survival, the failure, and the complication rates of veneered and monolithic all-ceramic implant-supported single crowns. Clin. Oral. Implant. Res. 2021, 32 (Suppl. 21), 254–288. [Google Scholar] [CrossRef]
- Paolone, G.; Mandurino, M.; De Palma, F.; Mazzitelli, C.; Scotti, N.; Breschi, L.; Gherlone, E.; Cantatore, G.; Vichi, A. Color Stability of Polymer-Based Composite CAD/CAM Blocks: A Systematic Review. Polymers 2023, 15, 464. [Google Scholar] [CrossRef]
- Machry, R.V.; Dapieve, K.S.; Valcanaia, A.; Pereira, G.K.R.; Bottino, M.C.; Valandro, L.F. Thickness and internal adjustment of monolithic resin composite milled crowns: Effect on the load-bearing capacity under fatigue. J. Mech. Behav. Biomed. Mater. 2022, 134, 105407. [Google Scholar] [CrossRef]
- Heintze, S.D.; Rousson, V. Survival of zirconia- and metal-supported fixed dental prostheses: A systematic review. Int. J. Prosthodont. 2010, 23, 493–502. [Google Scholar]
- Greuling, A.; Wiemken, M.; Kahra, C.; Maier, H.J.; Eisenburger, M. Fracture Resistance of Repaired 5Y-PSZ Zirconia Crowns after Endodontic Access. Dent. J. 2023, 11, 76. [Google Scholar] [CrossRef]
- Estay, J.; Martín, J.; Viera, V.; Valdivieso, J.; Bersezio, C.; Vildosola, P.; Mjor, I.A.; Andrade, M.F.; Moraes, R.R.; Moncada, G.; et al. 12 Years of Repair of Amalgam and Composite Resins: A Clinical Study. Oper. Dent. 2018, 43, 12–21. [Google Scholar] [CrossRef] [PubMed]
- Carrabba, M.; Vichi, A.; Louca, C.; Ferrari, M. Comparison of traditional and simplified methods for repairing CAD/CAM feldspathic ceramics. J. Adv. Prosthodont. 2017, 9, 257–264. [Google Scholar] [CrossRef] [PubMed]
- Akgül, S.; Alp, C.K.; Bala, O. Repair potential of a bulk-fill resin composite: Effect of different surface-treatment protocols. Eur. J. Oral Sci. 2021, 129, e12814. [Google Scholar] [CrossRef] [PubMed]
- Altinci, P.; Mutluay, M.; Tezvergil-Mutluay, A. Repair bond strength of nanohybrid composite resins with a universal adhesive. Acta Biomater. Odontol. Scand. 2017, 4, 10–19. [Google Scholar] [CrossRef] [PubMed]
- Ugurlu, M.; Husain, N.A.; Özcan, M. Repair of Bulk-Fill and Nanohybrid Resin Composites: Effect of Surface Conditioning, Adhesive Promoters, and Long-Term Aging. Materials 2022, 15, 4688. [Google Scholar] [CrossRef] [PubMed]
- Van Ende, A.; de Munck, J.; Lise, D.P.; van Meerbeek, B. Bulk-fill composites: A review of the current literature. J. Adhes. Dent. 2017, 19, 95–109. [Google Scholar] [CrossRef] [PubMed]
- Erdemir, U.; Sancakli, H.S.; Sancakli, E.; Eren, M.M.; Ozel, S.; Yucel, T.; Yildiz, E. Shear bond strength of a new self-adhering flowable composite resin for lithium disilicate-reinforced CAD/CAM ceramic material. J. Adv. Prosthodont. 2014, 6, 434–443. [Google Scholar] [CrossRef]
- Tribst, J.P.M.; Dal Piva, A.M.D.O.; Borges, A.L.S.; Araújo, R.M.; da Silva, J.M.F.; Bottino, M.A.; Kleverlaan, C.J.; de Jager, N. Effect of different materials and undercut on the removal force and stress distribution in circumferential clasps during direct retainer action in removable partial dentures. Dent. Mater. 2020, 36, 179–186. [Google Scholar] [CrossRef]
- Özcan, C.; Lestriez, P.; Berry-Kromer, V.; Thiebaud, F.; Sockalingum, G.D.; Untereiner, V. Misinterpretation of ISO 4049 standard recommendations: Impact on Young’s modulus and conversion degree of dental composites. J. Mech. Behav. Biomed. Mater. 2020, 110, 103947. [Google Scholar] [CrossRef]
- Soares, P.M.; Cadore-rodrigues, A.C.; Borges, A.L.S.; Valandro, L.F.; Pereira, G.K.R.; Rippe, M.P. Load-bearing capacity under fatigue and FEA analysis of simplified ceramic restorations supported by Peek or zirconia polycrystals as foundation substrate for implant purposes. J. Mech. Behav. Biomed. Mater. 2021, 123, 104760. [Google Scholar] [CrossRef]
- Marovic, D.; Par, M.; Macan, M.; Klarić, N.; Plazonić, I.; Tarle, Z. Aging-Dependent Changes in Mechanical Properties of the New Generation of Bulk-Fill Composites. Materials 2022, 15, 902. [Google Scholar] [CrossRef] [PubMed]
- Tribst, J.P.M.; Dal Piva, A.M.O.; de Jager, N.; Bottino, M.A.; de Kok, P.; Kleverlaan, C.J. Full-Crown Versus Endocrown Approach: A 3D-Analysis of Both Restorations and the Effect of Ferrule and Restoration Material. J. Prosthodont. 2021, 30, 335–344. [Google Scholar] [CrossRef] [PubMed]
- Yamanel, K.; Caglar, A.; Gülsahi, K.; Ozden, U.A. Effects of different ceramic and composite materials on stress distribution in inlay and onlay cavities: 3-D finite element analysis. Dent. Mater. J. 2009, 28, 661–670. [Google Scholar] [CrossRef]
- Kelly, J.R. Dental ceramics: What is this stuff anyway? J. Am. Dent. Assoc. 2008, 139, 4S–7S. [Google Scholar] [CrossRef] [PubMed]
- Van Dijken, J.W.V.; Pallesen, U. Fracture frequency and longevity of fractured resin composite, polyacid-modified resin composite, and resin-modified glass ionomer cement class IV restorations: An up to 14 years of follow-up. Clin. Oral Investig. 2010, 14, 217–222. [Google Scholar] [CrossRef]
- Kosewski, P.; De Angelis, F.; Sorrentino, E.; Mielczarek, A.; Buonvivere, M.; D’Arcangelo, C. Effect of the Abutment Rigidity on the Wear Resistance of a Lithium Disilicate Glass Ceramic: An in Vitro Study. J. Funct. Biomater. 2023, 14, 395. [Google Scholar] [CrossRef]
- Preis, V.; Hahnel, S.; Behr, M.; Rosentritt, M. In vitro performance and fracture resistance of novel CAD/CAM ceramic molar crowns loaded on implants and human teeth. J. Adv. Prosthodont. 2018, 10, 300–307. [Google Scholar] [CrossRef]
- Saravia-Rojas, M.A.; Geng-Vivanco, R. Clinical protocol for intraoral repair of a chipped all-ceramic crown: A case report. Gen. Dent. 2023, 71, 54–57. [Google Scholar]
- de Kok, P.; Kleverlaan, C.J.; de Jager, N.; Kuijs, R.; Feilzer, A.J. Mechanical performance of implant-supported posterior crowns. J. Prosthet. Dent. 2015, 114, 59–66. [Google Scholar] [CrossRef]
- Ahmed, M.A.; Hamdy, A.M.; Fattah, G.A.; Elfadl, A.K.A. Effect of Prosthetic Design and Restorative Material on the Stress Distribution of Implant-Supported 3-Unit Fixed Partial Dentures: 3D-FEA. Braz. Dent. Sci. 2022, 25, e3523. [Google Scholar] [CrossRef]
- Nguyen, J.F.; Migonney, V.; Ruse, N.D.; Sadoun, M. Resin composite blocks via high-pressure high-temperature polymerization. Dent. Mater. 2012, 28, 529–534. [Google Scholar] [CrossRef] [PubMed]
- Arpa, C.; Ceballos, L.; Fuentes, M.V.; Perdigão, J. Repair bond strength and nano leakage of artificially aged CAD-CAM composite resin. J. Prosthet. Dent. 2019, 121, 523–530. [Google Scholar] [CrossRef] [PubMed]
- Ergucu, Z.; Turkun, L.S.; Aladag, A. Color stability of nanocomposites polished with one-step systems. Oper. Dent. 2008, 33, 413–420. [Google Scholar] [CrossRef] [PubMed]
- Chuang, S.F.; Liu, J.K.; Chao, C.C.; Liao, F.P.; Chen, Y.H.M. Effects of flowable composite lining and operator experience on microleakage and internal voids in class II composite restorations. J. Prosthet. Dent. 2001, 85, 177–183. [Google Scholar] [CrossRef]
- Sibai, N.; El Mourad, A.; Al Suhaibani, N.; Al Ahmadi, R.; Al Dosary, S. Shear Bond Strength of Self-Adhesive Flowable Resin Composite. Int. J. Dent. 2022, 2022, 6280624. [Google Scholar] [CrossRef]
- Ikeda, I.; Otsuki, M.; Sadr, A.; Nomura, T.; Kishikawa, R.; Tagami, J. Effect of filler content of flowable composites on resin-cavity interface. Dent. Mater. J. 2009, 28, 679–685. [Google Scholar] [CrossRef]
- Callea, C.; Ceddia, M.; Piattelli, A.; Specchiulli, A.; Trentadue, B. Finite Element Analysis (FEA) for a Different Type of Cono-in Dental Implant. Appl. Sci. 2023, 13, 5313. [Google Scholar] [CrossRef]
- Grande, M.F.B.; Lopes, G.D.R.S.; Teixeira, M.L.; Pelegrine, A.A.; de Matos, J.D.M.; Nishioka, R.S. Mechanical Behavior of Implant-Supported Full-Arch Prostheses in Different Locations in the Maxilla: 3D-FEA and Strain Gauge Analysis. Braz. Dent. Sci. 2023, 26, e3771. [Google Scholar] [CrossRef]
- De Matos, J.D.; De Carvalho Ramos, N.; Queiroz, D.A.; Sinhoreti, M.A.; Barbosa, A.B.; Bottino, M.A.; Borges, A.L.; Lopes, G.D. Biomechanical Behavior Evaluation of a Mandibular Full-Arch Implant-Supported Prosthesis on ZrO2 and TiO2 Monotype Dental Implants. Int. J. Odontostomatol. 2023, 17, 174–185. [Google Scholar] [CrossRef]
- Vadiraj, B.; Rao, P.K.; Kumar, K.K. Application of Biomaterials and Finite Element Analysis in Dentistry-A Review. Material Today Proc. 2022, 76, 564–568. [Google Scholar] [CrossRef]



| Materials | Young Modulus (GPa) | Poison Ratio |
|---|---|---|
| Lithium disilicate | 95 | 0.3 |
| Translucent zirconia | 200 | 0.3 |
| CAD-CAM resin composite | 11.61 | 0.3 |
| Nanohybrid repair composite | 11 | 0.3 |
| Bulk-fill repair composite | 8.4 | 0.3 |
| Flowable repair composite | 5.6 | 0.3 |
| Groups | Finite Element Analysis | In Vitro Test | Risk of Failure (%) | |
|---|---|---|---|---|
| Tensile Stress (MPa) | Shear Stress (MPa) | Shear Bond Strength (MPa) | ||
| TZ-NH | 3.09 | 8.97 | 7.99 (7.56) B | 112 |
| TZ-BULK | 3.13 | 9.00 | 6.69 (2.75) B | 135 |
| TZ-FLOW | 3.18 | 9.03 | 11.77 (5.44) AB | 77 |
| LD-NH | 2.90 | 8.81 | 8.66 (7.54) B | 102 |
| LD-BULK | 2.99 | 8.88 | 7.14 (4.13) B | 124 |
| LD-FLOW | 3.08 | 8.96 | 11.05 (3.16) AB | 81 |
| RC-NH | 1.77 | 7.03 | 17.96 (4.54) A | 39 |
| RC-BULK | 1.93 | 7.38 | 16.88 (8.15) A | 44 |
| RC-FLOW | 2.12 | 7.83 | 16.88 (5.26) A | 46 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Soares, P.M.; da Rosa, L.S.; Pereira, G.K.R.; Valandro, L.F.; Rippe, M.P.; Dal Piva, A.M.d.O.; Feilzer, A.J.; Kleverlaan, C.J.; Tribst, J.P.M. Mechanical Behavior of Repaired Monolithic Crowns: A 3D Finite Element Analysis. Dent. J. 2023, 11, 254. https://doi.org/10.3390/dj11110254
Soares PM, da Rosa LS, Pereira GKR, Valandro LF, Rippe MP, Dal Piva AMdO, Feilzer AJ, Kleverlaan CJ, Tribst JPM. Mechanical Behavior of Repaired Monolithic Crowns: A 3D Finite Element Analysis. Dentistry Journal. 2023; 11(11):254. https://doi.org/10.3390/dj11110254
Chicago/Turabian StyleSoares, Pablo Machado, Lucas Saldanha da Rosa, Gabriel Kalil Rocha Pereira, Luiz Felipe Valandro, Marilia Pivetta Rippe, Amanda Maria de Oliveira Dal Piva, Albert J. Feilzer, Cornelis J. Kleverlaan, and João Paulo Mendes Tribst. 2023. "Mechanical Behavior of Repaired Monolithic Crowns: A 3D Finite Element Analysis" Dentistry Journal 11, no. 11: 254. https://doi.org/10.3390/dj11110254