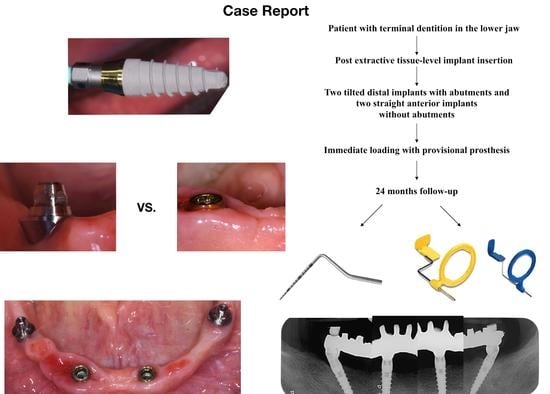
Full-Arch Rehabilitation Using Trans-Mucosal Tissue-Level Implants with and without Implant-Abutment Units: A Case Report
Abstract
:1. Introduction
2. Case Report
Surgery Appointment
3. Results
- -
- Probing depth (mm): Distal right (DR) implants showed 2 mm probing depth on the mesial side, 2 mm on the vestibular side, 3 mm on the distal side, and 3 mm on the lingual side. The anterior right (AR) implant showed 3 mm probing depth on the mesial side, 3 mm on the vestibular side, 2 mm on the distal side, and 3 mm on the lingual side. The anterior left (AL) implant showed 2 mm probing depth on the mesial side, 2 mm on the vestibular side, 3 mm on the distal side, and 3 mm on the lingual side. The distal left (DL) implant showed 2 mm probing depth on the mesial side, 2 mm on the vestibular side, 3 mm on the distal side, and 3 mm on the lingual side.
- -
- Bleeding on probing (BOP): DR, AR, and DL implants presented one side each with BOP. No BOP was detected on the AL implant.
- -
- No plaque was detected at any sites.
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pera, P.; Menini, M.; Pesce, P.; Bevilacqua, M.; Pera, F.; Tealdo, T. Immediate Versus Delayed Loading of Dental Implants Supporting Fixed Full-Arch Maxillary Prostheses: A 10-year Follow-up Report. Int. J. Prosthodont. 2019, 32, 27–31. [Google Scholar] [CrossRef]
- Menini, M.; Signori, A.; Tealdo, T.; Bevilacqua, M.; Pera, F.; Ravera, G.; Pera, P. Tilted implants in the immediate loading rehabilitation of the maxilla: A systematic review. J. Dent. Res. 2012, 91, 821–827. [Google Scholar] [CrossRef]
- Schropp, L.; Isidor, F.; Kostopoulos, L.; Wenzel, A. Patient experience of, and satisfaction with, delayed-immediate vs. delayed single-tooth implant placement. Clin. Oral. Implants Res. 2004, 15, 498–503. [Google Scholar] [CrossRef]
- Chrcanovic, B.R.; Albrektsson, T.; Wennerberg, A. Tilted versus axially placed dental implants: A meta-analysis. J. Dent. 2015, 43, 149–170. [Google Scholar] [CrossRef]
- Balshi, T.J.; Wolfinger, G.J.; Slauch, R.W.; Balshi, S.F. A retrospective analysis of 800 Brånemark System implants following the All-on-Four protocol. J. Prosthodont. 2014, 23, 83–88. [Google Scholar] [CrossRef]
- Wittneben, J.G.; Buser, D.; Salvi, G.E.; Bürgin, W.; Hicklin, S.; Brägger, U. Complication and failure rates with implant-supported fixed dental prostheses and single crowns: A 10-year retrospective study. Clin. Implant Dent. Relat. Res. 2014, 16, 356–364. [Google Scholar] [CrossRef]
- Natali, A.N.; Gasparetto, A.; Carniel, E.L.; Pavan, P.G.; Fabbro, S. Interaction phenomena between oral implants and bone tissue in single and multiple implant frames under occlusal loads and misfit conditions: A numerical approach. J. Biomed. Mater. Res. B Appl. Biomater. 2007, 83, 332–339. [Google Scholar] [CrossRef]
- Zervas, P.J.; Papazoglou, E.; Beck, F.M.; Carr, A.B. Distortion of three-unit implant frameworks during casting, soldering, and simulated porcelain firings. J. Prosthodont. 1999, 8, 171–179. [Google Scholar] [CrossRef]
- Manzella, C.; Burello, V.; Bignardi, C.; Carossa, S.; Schierano, G. A method to improve passive fit of frameworks on implant-supported prostheses: An in vivo study. Int. J. Prosthodont. 2013, 26, 577–579. [Google Scholar] [CrossRef] [Green Version]
- Göthberg, C.; André, U.; Gröndahl, K.; Thomsen, P.; Slotte, C. Bone Response and Soft Tissue Changes Around Implants With/Without Abutments Supporting Fixed Partial Dentures: Results From a 3-Year, Prospective, Randomized, Controlled Study. Clin. Implant Dent. Relat. Res. 2016, 18, 309–322. [Google Scholar] [CrossRef]
- Canullo, L.; Tallarico, M.; Gracis, S.; Vela, X.; Rodriguez, X.; Covani, U. Clinical Considerations on Strategies That Avoid Multiple Connections and Disconnections of Implant Abutments. Int. J. Periodontics Restor. Dent. 2020, 40, 9–17. [Google Scholar] [CrossRef]
- Göthberg, C.; André, U.; Gröndahl, K.; Ljungquist, B.; Thomsen, P.; Slotte, C. Immediately loaded implants with or without abutments supporting fixed partial dentures: 1-year results from a prospective, randomized, clinical trial. Clin. Implant Dent. Relat. Res. 2014, 16, 487–500. [Google Scholar] [CrossRef]
- Göthberg, C.; Gröndahl, K.; Omar, O.; Thomsen, P.; Slotte, C. Bone and soft tissue outcomes, risk factors, and complications of implant-supported prostheses: 5-Years RCT with different abutment types and loading protocols. Clin. Implant Dent. Relat. Res. 2018, 20, 313–321. [Google Scholar] [CrossRef]
- Canullo, L.; Penarrocha-Oltra, D.; Soldini, C.; Mazzocco, F.; Penarrocha, M.; Covani, U. Microbiological assessment of the implant-abutment interface in different connections: Cross-sectional study after 5 years of functional loading. Clin. Oral Implants Res. 2015, 26, 426–434. [Google Scholar] [CrossRef]
- Quirynen, M.; Naert, I.; van Steenberghe, D. Fixture design and overload influence marginal bone loss and fixture success in the Brånemark system. Clin. Oral Implants Res. 1992, 3, 104–111. [Google Scholar] [CrossRef]
- Tallarico, M.; Canullo, L.; Caneva, M.; Ozcam, M. Microbial colonization of the implant-abutment interface and its possible influence on the development of peri-implantitis: A systematic review with meta-analysis. J. Prosthodont. Res. 2017, 61, 233–241. [Google Scholar] [CrossRef] [Green Version]
- Menini, M.; Pesce, P.; Bagnasco, F.; Carossa, M.; Mussano, F.; Pera, F. Evaluation of internal and external hexagon connections in immediately loaded full-arch rehabilitations: A within-person randomised split-mouth controlled trial. Int. J. Oral Implantol. 2019, 12, 169–179. [Google Scholar]
- Pozzan, M.C.; Grande, F.; Mochi Zamperoli, E.; Tesini, F.; Carossa, M.; Catapano, S. Assessment of Preload Loss after Cyclic Loading in the OT Bridge System in an “All-on-Four” Rehabilitation Model in the Absence of One and Two Prosthesis Screws. Materials 2022, 15, 1582. [Google Scholar] [CrossRef]
- Corvino, E.; Pesce, P.; Mura, R.; Marcano, E.; Canullo, L. Influence of Modified Titanium Abutment Surface on Peri-implant Soft Tissue Behavior: A Systematic Review of In Vitro Studies. Int. J. Oral Maxillofac. Implant. 2020, 35, 503–519. [Google Scholar] [CrossRef]
- Pesce, P.; Menini, M.; Tommasato, G.; Patini, R.; Canullo, L. Influence of modified titanium abutment surface on peri-implant soft tissue behaviour: A systematic review of histological findings. Int. J. Oral Implantol. 2019, 12, 419–429. [Google Scholar]
- Ceruso, F.M.; Barnaba, P.; Mazzoleni, S.; Ottria, L.; Gargari, M.; Zuccon, A.; Bruno, G.; DI Fiore, A. Implant-abutment connections on single crowns: A systematic review. Oral Implantol. 2017, 10, 349–353. [Google Scholar] [CrossRef]
- Agustín-Panadero, R.; Martínez-Martínez, N.; Fernandez-Estevan, L.; Faus-López, J.; Solá-Ruíz, M.F. Influence of Transmucosal Area Morphology on Peri-Implant Bone Loss in Tissue-Level Implants. Int. J. Oral Maxillofac Implant. 2019, 34, 947–952. [Google Scholar] [CrossRef]
- Canullo, L.; Tallarico, M.; Pradies, G.; Marinotti, F.; Loi, I.; Cocchetto, R. Soft and hard tissue response to an implant with a convergent collar in the esthetic area: Preliminary report at 18 months. Int. J. Esthet. Dent. 2017, 12, 306–323. [Google Scholar]
- Canullo, L.; Menini, M.; Covani, U.; Pesce, P. Clinical outcomes of using a prosthetic protocol to rehabilitate tissue-level implants with a convergent collar in the esthetic zone: A 3-year prospective study. J. Prosthet. Dent. 2020, 123, 246–251. [Google Scholar] [CrossRef]
- Tealdo, T.; Menini, M.; Bevilacqua, M.; Pera, F.; Pesce, P.; Signori, A.; Pera, P. Immediate versus delayed loading of dental implants in edentulous patients’ maxillae: A 6-year prospective study. Int. J. Prosthodont. 2014, 27, 207–214. [Google Scholar] [CrossRef] [Green Version]
- Butera, A.; Pascadopoli, M.; Pellegrini, M.; Gallo, S.; Zampetti, P.; Scribante, A. Oral Microbiota in Patients with Peri-Implant Disease: A Narrative Review. Appl. Sci. 2022, 12, 3250. [Google Scholar] [CrossRef]
- Butera, A.; Pascadopoli, M.; Pellegrini, M.; Gallo, S.; Zampetti, P.; Cuggia, G.; Scribante, A. Domiciliary Use of Chlorhexidine vs. Postbiotic Gels in Patients with Peri-Implant Mucositis: A Split-Mouth Randomized Clinical Trial. Appl. Sci. 2022, 12, 2800. [Google Scholar] [CrossRef]
- Butera, A.; Gallo, S.; Pascadopoli, M.; Luraghi, G.; Scribante, A. Ozonized Water Administration in Peri-Implant Mucositis Sites: A Randomized Clinical Trial. Appl. Sci. 2021, 11, 7812. [Google Scholar] [CrossRef]
- Costa Castillo, M.; Laguna Martos, M.; Marco Pitarch, R.; García Selva, M.; del Cid Rodríguez, S.; Fons-Badal, C.; Agustín Panadero, R. Analysis of Peri-Implant Bone Loss with a Convergent Transmucosal Morphology: Retrospective Clinical Study. Int. J. Environ. Res. Public Health 2022, 19, 3443. [Google Scholar] [CrossRef]
- Canullo, L.; Menini, M.; Bagnasco, F.; Di Tullio, N.; Pesce, P. Tissue-level versus bone-level single implants in the anterior area rehabilitated with feather-edge crowns on conical implant abutments: An up to 5-year retrospective study. J. Prosthet. Dent. 2021, S0022-3913(21)00082, 2. [Google Scholar] [CrossRef]
- Häkkinen, L.; Uitto, V.J.; Larjava, H. Cell biology of gingival wound healing. Periodontology 2000 2000, 24, 127–152. [Google Scholar] [PubMed]
- Rompen, E.; Raepsaet, N.; Domken, O.; Touati, B.; Van Dooren, E. Soft tissue stability at the facial aspect of gingivally converging abutments in the esthetic zone: A pilot clinical study. J. Prosthet Dent. 2007, 97, 119–125. [Google Scholar] [CrossRef]
- Suárez-López Del Amo, F.; Lin, G.H.; Monje, A.; Galindo-Moreno, P.; Wang, H.L. Influence of Soft Tissue Thickness on Peri-Implant Marginal Bone Loss: A Systematic Review and Meta-Analysis. J. Periodontol. 2016, 87, 690–699. [Google Scholar] [CrossRef] [PubMed]
- Welander, M.; Abrahamsson, I.; Berglundh, T. The mucosal barrier at implant abutments of different materials. Clin. Oral Implants Res. 2008, 19, 635–641. [Google Scholar] [CrossRef] [PubMed]
- Lazzara, R.J.; Porter, S.S. Platform switching: A new concept in implant dentistry for controlling postrestorative crestal bone levels. Int. J. Periodontics Restor. Dent. 2006, 26, 9–17. [Google Scholar]
- Cannizzaro, G.; Felice, P.; Gherlone, E.; Barausse, C.; Ferri, V.; Leone, M.; Trullenque-Eriksson, A.; Esposito, M. Immediate loading of two (fixed-on-2) vs four (fixed-on-4) implants placed with a flapless technique supporting mandibular cross-arch fixed prostheses: 3-year results from a pilot randomised controlled trial. Eur. J. Oral Implantol. 2017, 10, 133–145. [Google Scholar]
- Esposito, M.; Felice, P.; Barausse, C.; Pistilli, R.; Grandi, G.; Simion, M. Immediately loaded machined versus rough surface dental implants in edentulous jaws: One-year postloading results of a pilot randomised controlled trial. Eur. J. Oral Implantol. 2015, 8, 387–396. [Google Scholar]












Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carossa, M.; Alovisi, M.; Crupi, A.; Ambrogio, G.; Pera, F. Full-Arch Rehabilitation Using Trans-Mucosal Tissue-Level Implants with and without Implant-Abutment Units: A Case Report. Dent. J. 2022, 10, 116. https://doi.org/10.3390/dj10070116
Carossa M, Alovisi M, Crupi A, Ambrogio G, Pera F. Full-Arch Rehabilitation Using Trans-Mucosal Tissue-Level Implants with and without Implant-Abutment Units: A Case Report. Dentistry Journal. 2022; 10(7):116. https://doi.org/10.3390/dj10070116
Chicago/Turabian StyleCarossa, Massimo, Mario Alovisi, Armando Crupi, Giulia Ambrogio, and Francesco Pera. 2022. "Full-Arch Rehabilitation Using Trans-Mucosal Tissue-Level Implants with and without Implant-Abutment Units: A Case Report" Dentistry Journal 10, no. 7: 116. https://doi.org/10.3390/dj10070116