1. Introduction
Oral-health-related quality of life (OHRQoL) questionnaires are used to obtain patient-based outcomes that refer to the individual’s self-evaluation of the perception of a disease, and determine its perceived impact on quality of life [
1]. In this context, OHRQoL measures tend to focus on the functional, psychological, and social impacts of the oral conditions on the life of the patient [
2], and each of these instruments has its specific focus, purpose, and length [
3].
Nevertheless, in epidemiological surveys, and even in clinical settings, the use of the questionnaire may be restricted by its length and the burden placed on persons [
4]. Large scale population surveys are facing a persistent decrease in their response rates [
5,
6,
7,
8]. Various factors impact the decrease in response rates, including the effect of the instrument length [
9]. Subsequently, item non-responses, if they occur, affect the validity of the results, and the utility of the data [
10]. To address such situations, the application can be broadened by developing a short version of the questionnaire. This may lead to a reduction in the duration and financial costs of data collection. It can also lessen the risk of total and item non-responses [
4]. Nevertheless, other studies mentioned that there is small or insignificant difference in the response rate between the short and long versions of a questionnaire [
11,
12,
13]. Allen et al in 2020, [
14] recommended that the long and short questionnaire versions should be included among survey design options. For clinical settings, using the short forms might be essential for practitioners where health care interventions should be targeted toward what the patients feel is important [
15].
The Psychosocial Impact of Dental Aesthetics Questionnaire (PIDAQ) is a multidimensional instrument. It specifically aims to assess orthodontic aspects of OHRQoL [
16]. PIDAQ was developed to be used among individuals seeking orthodontic treatment [
17]. It consists of 23 items organized into four subscales: Dental Self-Confidence (six items); Social Impact (eight items); Psychological Impact (six items); and Aesthetic Concern (three items). PIDAQ version for adolescents aged 11 to 17 years old also showed good psychometric properties [
18].
This questionnaire has been adapted in other languages for use by Malaysian [
17,
19], Spanish [
20,
21], Swedish [
22], and Persian people [
23]. It has also been cross-culturally adapted into an Arabic version, i.e. PIDAQ(A) to be filled by 12–17-year-old Yemeni children [
24]. The PIDAQ(A) demonstrated good psychometric properties to be used for the Yemeni population with some modifications. The PIDAQ(A) consists of 24 items. These items are grouped into three subscales: Dental Self-Confidence (DSC) (6 items), Psychosocial Impact (PSI) (10 items), and Aesthetic Concern (AC) (8 items). The Cronbach’s α values for all subscales of the PIDAQ(A) were from 0.90 to 0.93 [
24].
In Yemen, there is a need to have further information on the effects of malocclusion on the OHRQoL of the population regardless of the severity of the malocclusion. This may make important and relevant information for planning future dental services, as well as a projection of manpower needed to provide the service, more accessible. Therefore, it will provide information on the actual priority for orthodontic treatment needs. The importance of the PIDAQ instrument has led to the need to generate a short version of the PIDAQ(A) to be used in large scale surveys, and even in clinical settings. Another benefit of a short version of the PIDAQ(A) is that its use will minimize item non-response.
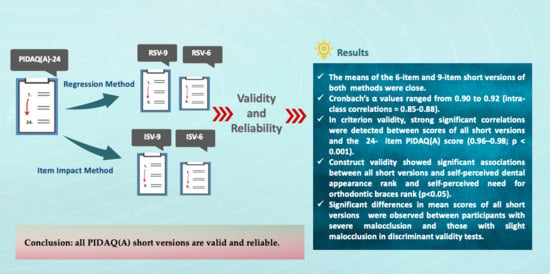
Therefore, the aim of this study was to derive the short versions of the PIDAQ(A) by using two item reduction methods. The objectives were to compare the content and psychometric properties of the short versions derived from the two methods, and to compare the short versions with the long version of the PIDAQ(A) [
24]. The null hypothesis was that it would not be possible to shorten the questionnaire into valid and reliable short versions. The alternative hypothesis was that it would be possible to shorten the questionnaire into valid and reliable short versions.
4. Discussion
The original PIDAQ instrument is a 23-item self-reporting questionnaire assessing the extent to which a person has experienced psychosocial problems due to malocclusion. The PIDAQA(A) was validated in the first part of our study [
24]. In this study, the PIDAQ(A) short versions have been derived, tested for the psychometric validation, and compared with the 24-item PIDAQ(A).
This study produced four short versions of the PIDAQ(A). They were referred as PIDAQ(A)-ISV-9, PIDAQ(A)-RSV-9, PIDAQ(A)-ISV-6, and PIDAQ(A)-RSV-6. The methods used to produce the short versions followed those in the previous studies [
4,
15], and the item impact method and the regression method were applied. Concurrently, each of the shortening techniques that were used produced nine-item and a six-item measures. As a result, two or three items per each subscale were considered as the minimum number of items. The item impact method involved reduction of the items from the PIDAQ(A)-24 to include items that showed the highest impact scores in each subscale, whereas in the forward regression method, the first three and two items from each subscale entering the model, and which produced the highest adjusted R
2, were selected. Two items per subscale were considered the minimum number of items [
4].
As recommended by Jokovic et al. [
4], the shortening of an instrument should take into account using more than one method to ascertain the effect of the approach on outcomes, because different methods can produce various short version measures, which may differ in items and properties. Therefore, this study had used two different methods to generate the short version.
Shortening a questionnaire is an effective way to increase the response rate [
10,
31]. Sahlqvist et al. [
10] reported in their study that shortening a relatively lengthy instrument significantly increased the responses. Findings of their study revealed that an increase in the response rate was due to the shortening of the original questionnaire. Also, using the short version will be a useful substitute to the long questionnaire when time and financial costs are limited.
To date, there is no literature support for shortening the PIDAQ instrument, but there are other OHRQoL measures which have been shortened, such as the short versions of the Child Perceptions Questionnaire (CPQ11–14) [
4,
32] and the Oral Health Impact Profile (OHIP) Questionnaire, which underwent item reductions [
33,
34,
35,
36].
The results of the study showed that the PIDAQ(A) short versions exhibited considerable sensitivity, where proportions of PIDAQ(A)-ISV-9, PIDAQ(A)-RSV-9, PIDAQ(A)-ISV-6, and PIDAQ(A)-RSV-6 (78.7%, 74.3%, 61.5%, and 61.0%, respectively) revealed that the short versions of questionnaires detected substantial variability in adolescents’ perceptions of the effect of malocclusion in their life. In comparing their values, PIDAQ(A)-ISV9 was the highest (78.7%). Therefore, it seems reasonable to assert that the selected items for the short versions concern the most frequent and annoying problems reported by adolescents. However, values of all short versions were smaller than the long questionnaire (85.5%).
The psychometric properties have been achieved in terms of reliability (internal consistency and reproducibility) and validity (criterion, convergent, and discriminant validities). The short versions were comparable with the long version of the PIDAQ(A) in terms of sensitive and discriminant validities. This assessment is based on the responses from 385 children who were the participants of the main study.
For internal consistency, the ISV-9 and RSV-9 versions have almost similar Cronbach’s α values, (0.92) and (0.91), respectively, whereas the ISV-6 and RSV-6 versions showed identical Cronbach’s α values (0.90). The ICC-score-evaluated reproducibility was generally good for the four short versions, with scores ranging from 0.90 to 0.92 for all short versions. These scores were slightly similar to those in the PIDAQ(A) long version, where all of its subscales values were between 0.89 and 0.96 [
24]. Nevertheless, RSV-9 version was better than others in the reproducibility test, and the RSV-9 version was the only version that showed no statistically significant differences between test and retest administrations. Assessment of criterion validity by comparing the correlation between all short versions and PIDAQ(A)-24 revealed that the correlation coefficient was highest for PIDAQ(A)-RSV9 (rho: 0.983). Whereas the correlation coefficient for the PIDAQ(A)-ISV9 was lesser (rho: 0.969). In addition, in criterion validity, the correlations between the short versions’ scores with the Child-OIDP score were shown to be statistically significant for all short versions (
p < 0.001). The correlation coefficient with the Child-OIDP performance scores for the four short versions were slightly similar, but the ISV-9 was the highest (0.656). For construct validity, an analysis of convergent validity, as well as discriminant validity, showed statistically significant differences in associations with other global scales in all short versions.
Consequently, the high correlations between the PIDAQ(A)-24 and the short versions suggest that they are measuring the same construct [
4]. All short versions were examined for cross-sectional validation, and all short forms showed good validity and reliability. Thus, the null hypotheses were rejected. In accordance with the results of the study, the short versions were almost identical. It may be worth pointing out that though the nine-item short versions presented interesting items, the results showed that the further shortening of the questionnaire to a six-item questionnaire was also valid, and as reliable as the nine-item version. In regard to the presence of differences between them, these differences were mostly negligible. However, the regression short versions were slightly stronger when compared to the impact short versions in reproducibility and criterion validity, that can be elucidated by the fact the items identified for the regression short versions were those that elucidate the most discrepancy in the total scores of the PIDAQ(A)-24 item.
The final consideration is if the regression method is better than the item impact method, or vice versa. Coste et al. [
37] took the view that the expert-based method is more expedient. The utility of the item impact method is in selecting the items which are considered more meaningful for the individuals who will be answering the questionnaire. These individuals may be considered to be experienced with the impact of the discussed circumstances on their quality of life [
4]. On the contrary, the short version, which was developed by statistical considerations represented by the regression method, performed reasonably well [
4]. Nonetheless, Locker and Allen [
15] considered that the approach of generating a short version measure is less important than its properties and content, this consideration was assisted by the findings of this study.
Eventually, PIDAQ(A) short versions can be used to distinguish Yemeni adolescents on the impact on their dental aesthetics when there is difficulty in using the PIDAQ(A) long version. The optional limitation of the study was that no short versions were administrated on their own. For further studies, we recommend measuring any changes in response rate when using both the long and short versions of the PIDAQ(A). Close attention should be paid to whether using the PIDAQ(A) short versions increases the response rate or not.