Depression Disorders in Mexican Adolescents: A Predictive Model
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sample
2.2. Instrument
2.3. Procedure
2.4. Statistical Analysis
3. Results
3.1. Pearson’s Correlation
3.2. Logistic Regression
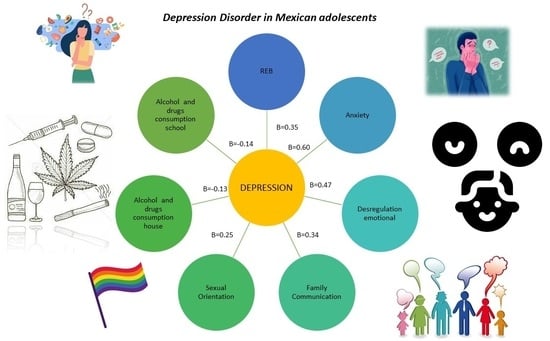
3.3. Structural Model
4. Discussion
5. Conclusions
6. Strengths and Limitations of the Study
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Organización Mundial de la Salud (OMS). Depresión. Available online: https://www.who.int/es/news-room/fact-sheets/detail/depression (accessed on 31 March 2023).
- Marcheco Teruel, B. El rol de los genes en la depresión: Una mirada al presente y futuro en el campo de las investigaciones genéticas. Rev. Cuban. Genét. Comun. 2015, 9, 5–7. [Google Scholar]
- Retamal, C.P. Depresión; Editorial Universitaria: Santiago, Chile, 1999; pp. 43–48. [Google Scholar]
- Vásquez Machado, A. Depresión. Diferencias de género. Multimed 2013, 17, 193–217. [Google Scholar]
- Lazarevick, I.; Mora-Carrasco, F. Depresión y género: Factores psicosociales de riesgo. Segunda Época 2008, 4, 7–16. [Google Scholar]
- Vásquez Machado, A. Relación entre violencia y depresión en mujeres. Rev. Chil. Neuro-Psiquiat 2007, 70, 88–95. [Google Scholar] [CrossRef] [Green Version]
- Rodriguez Espínola, S. Relación entre nivel socioeconómico, apoyo social percibido, género y depresión en niños. Interdisciplinaria 2010, 27, 261–275. [Google Scholar]
- Summerland, A.; Marston, L.; Huntley, J.; Livingston, G.; Lewis, G.; Steptoe, A.; Fancourt, D. Relaciones sociales y depresión durante el confinamiento por la COVID-19: Análisis longitudinal del estudio social de la COVID-19. Med. Psic. 2022, 32, 3381–3390. [Google Scholar] [CrossRef]
- Ferrel Ortega, R.F.; Celis Barros, A.; Hernández Cantero, O. Depresión y factores socio demográficos asociados en estudiantes universitarios de ciencias de la salud de una universidad pública (Colombia). Psicol. Desde El Caribe 2011, 27, 40–60. [Google Scholar]
- Álvarez, Z.M.; Ramírez Jacobo, B.; Silva Rodríguez, A.; Coffin Cabrera, N.; Jiménez Rentería, M.L. La relación entre depresión y conflictos familiares en adolescentes. Rev. Int. Psicol. Ter. Psicol. 2009, 9, 205–216. [Google Scholar]
- Gonzales Lugo, S.; Pineda Domínguez, A.; Gaxiola Romero, J.C. Depresión adolescente: Factores de riesgo y apoyo social como factor protector. Univ. Psychol. 2018, 17, 1–16. [Google Scholar] [CrossRef]
- Zysberg, L.; Rubanov, A. Inteligencia emocional y patrones de alimentación emocional: ¿una nueva perspectiva sobre los antecedentes de los trastornos alimentarios? J. Nutr. Educ. Behav. 2010, 42, 345–348. [Google Scholar] [CrossRef]
- Mills, P.; Newman, E.F.; Cossar, J.; Murray, G. Emotional Maltreatment and Disordered Eating in Adolescents: Testing the Mediating Role of Emotion Regulation. Child Abus. Negl. 2015, 39, 156–166. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Silk, J.S.; Shaw, D.S.; Skuban, E.M.; Oland, A.A.; Kovacs, M. Estrategias de regulación de emociones en hijos de madres con depresión infantil. J. Child Psychol. Psychiatry 2006, 47, 69–78. [Google Scholar] [CrossRef] [PubMed]
- Garber, J.; Braafladt, N.; Zeman, J. The regulation of sad affect: An information processing perspective. In The Development of Emotion Regulation and Dysregulation; Garber, J., Dodge, K., Eds.; Cambridge University Press: New York, NY, USA, 1991; pp. 208–240. [Google Scholar]
- Bariola, E.; Hughes, E.K.; Gullone, E. Relaciones entre padres e hijos Uso de estrategias de regulación emocional: Un informe breve. J. Child Fam. Stud. 2012, 21, 443–448. [Google Scholar] [CrossRef]
- Cassano, M.; Perry-Parrish, C.; Zeman, J. Influencia del género en la socialización de los padres de la regulación de la tristeza de los niños. Des. Soc. 2007, 16, 210–231. [Google Scholar]
- Hansson, E.; Daukantaité, D.; Johnsson, P. Disordered eating and emotion dysregulation among adolescents and their parents. BMC Psychol. 2017, 5, 12. [Google Scholar] [CrossRef] [Green Version]
- Campos, M.S.; Martínez-Larrea, J.A. Trastornos afectivos: Análisis de su comorbilidad en los trastornos psiquiátricos más frecuentes. An. Sist. Sanit. 2002, 25, 117–136. [Google Scholar]
- Boden, J.M.; Foulds, J.A. Major depression and alcohol use disorder in adolescence: Does comorbidity lead to poorer outcomes of depression? J. Affect. Disord. 2016, 206, 287–293. [Google Scholar] [CrossRef]
- Boden, J.; Fergusson, D.M.M. Alcohol and depression. Addiction 2011, 106, 906–914. [Google Scholar] [CrossRef]
- Fergusson, D.M.; Horwood, L.J.; Lynskey, M.T. Childhood sexual abuse and psychiatric disorder in young adulthood: II. Psychiatric outcomes of childhood sexual abuse. J. Am. Acad. Child. Adolesc. Psychiatry 1996, 35, 1365–1374. [Google Scholar] [CrossRef]
- Pedrelli, P.; Shapero, B.; Archibald, A.; Dale, C. Alcohol use and depression during adolescence and young adulthood: A summary and interpretation of mixed findings. Curr. Addict. Rep. 2016, 1, 91–97. [Google Scholar] [CrossRef] [Green Version]
- González Sánchez, J.D.; García Aurrecoechea, V.R.; y Córdova Alcaráz, A. Uso de sustancias entre adolescentes y su asociación con síntomas de depresión y percepción de sus relaciones familiares. Dir. Investig. Y Enseñanza Subdirección Investig. 2004, 3, 1–28. [Google Scholar]
- Unikel Santoncini, C.; Díaz de León-Vázquez, C.; González-Forteza, C.; Wagner Echeagaray, F.; Rivera Márquez, J.A. Conducta alimentaria de riesgo, síntomas depresivos y correlatos psicosociales en estudiantes universitarios de primer ingreso. Acta Univ. 2015, 25, 35–95. [Google Scholar] [CrossRef]
- American Psychological Association (APA). Sexual Orientation and Gender Diversity. Available online: https://www.apa.org/topics/lgbtq (accessed on 5 February 2023).
- Genise, G.; Humeniuk, A.R.; Ungaretti, J.; Etchezahar, E.D.; de Giuli, S. Relación entre la orientación sexual y personalidad en una muestra de adolescentes argentinos. Rev. Psicol. Clín. Niñ. Adolesc. 2019, 6, 49–53. [Google Scholar] [CrossRef]
- Hatzenbuehler, M.L.; Keyes, K.M.; McLaughlin, K.A.; Hasin, D.S. The Impact of Institutional Discrimination on Psychiatric Disorders in Lesbian, Gay, and Bisexual Populations: A Prospective Study. Am. J. Public Health 2010, 100, 452–459. [Google Scholar] [CrossRef]
- Marshal, M.P.; Dietz, L.J.; Friedman, M.S.; Stall, R.; Smith, H.A.; McGinley, J.; Thoma, B.C.; Murray, P.J.; D’Augelli, A.R.; Brent, D.A. Suicidality and depression disparities between sexual minority and heterosexual youth: A meta-analytic review. J. Adolesc. Health 2011, 49, 115–123. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bjureberg, J.; Sahlin, H.; Hedman-Lagerlöf, E.; Gratz, K.L.; Tull, M.T.; Jokinen, J.; Hellner, C.; Ljótsson, B. Extending research on Emotion Regulation Individual Therapy for Adolescents (ERITA) with nonsuicidal self-injury disorder: Open pilot trial and mediation analysis of a novel online version. BMC Psychiatry 2018, 18, 1–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Klonsky, E.D. The function of self-injury in young adults who cut themselves: Clarifying the evidence for affect-regulation. Psychiatry Res. 2009, 166, 260–268. [Google Scholar] [CrossRef] [Green Version]
- Bruce, M.L.; Ten Have, T.R.; Reynolds, C.F.; Katz, I.I.; Schulberg, H.C.; Mulsant, B.H.; Brown, G.K.; McAvay, G.J.; Pearson, J.L.; Alexopoulos, G.S. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients: A randomized controlled trial. JAMA 2004, 291, 1081–1091. [Google Scholar] [CrossRef] [Green Version]
- Alansari, B.M. Relationship between depression and anxiety among undergraduates students in eighteen arab countries: A cross-cultural study. Soc. Behav. Pers. 2005, 33, 503–512. [Google Scholar] [CrossRef]
- Gómez-Peresmitré, G.; Platas-Acevedo, R.S.; León-Hernández, R.; Pineda-García, G.; Guzmán-Saldaña, R. Psychometric Assessment of an Online Self-Test Measuring Risky Eating Behavior, Depression, Social Anxiety, and Self-Injury in Mexican Adolescents. Int. J. Environ. Res. Public Health 2023, 20, 399. [Google Scholar] [CrossRef]
- Potthat, M. Confirmatory factor analysis of ordered categorical variables with large models. Br. J. Math. Stat. Psychol. 1993, 46, 273–286. [Google Scholar] [CrossRef]
- Ortega, M.; María, R.; Pendás, T.; Leonel, C.; Ortega, M.; Mercedes; Abreu, P.; María, A.Y.C.A. El coeficiente de correlación de los rangos de Spearman caracterización. Rev. Hab. Cien. Med. 2009, 8, 2. [Google Scholar]
- Kline, R.B. Principles and Practice of Structural Equation Modeling, 4th ed.; The Guilford Press: New York, NY, USA, 2018. [Google Scholar]
- Hoyle, R. Manual de Modelado de Ecuaciones Estructurales, 2nd ed.; The Guilford Press: New York, NY, USA, 2014. [Google Scholar]
- Ibrahim, A.; Kelly, S.J. A Systematic review of studies of depression prevalence in university students. J. Psychiatr Rev. 2012, 47, 391–400. [Google Scholar] [CrossRef] [PubMed]
- Organización Mundial de la Salud (OMS). Trastornos Mentales. Available online: https://www.who.int/es/news-room/fact-sheets/detail/mental-disorders (accessed on 20 May 2023).
- Contreras Olive, Y.; Miranda Gómez, O.; Torres Lio-Coo, V. Ansiedad y depresión en pacientes adictos a sustancias psicoactivas. Rev. Cub. Med. Mil. 2020, 49, 71–85. [Google Scholar]
- Restrepo, J.E.; Amador Sánchez, O.; Calderon Vallejo, C.; Castañeda Quirama, T.; Diez Cardona, P. Depresión y su relación con el consumo de sustancias psicoactivas, el estrés académico y la ideación suicida en estudiantes universitarios colombianos. Health Adict. 2018, 18, 227–239. [Google Scholar] [CrossRef] [Green Version]
- Consejo Nacional Para el Desarrollo y la Inclusión de las Personas con Discapacidad. Día Mundial de la Lucha Contra la Depresión. Available online: https://www.gob.mx/conadis/articulos/13-de-enero-dia-mundial-de-la-lucha-contra-la-depresion#:~:text=El%2013%20de%20enero%20se,mayores%20los%20grupos%20m%C3%A1s%20afectados (accessed on 12 February 2023).
- Sánchez Hervás, E. Depresión, ansiedad y consumo de drogas. Anál. Modif. Conducta. 1995, 21, 735–743. [Google Scholar]
- Bjorklund, D.F.; Hernández Blasi, C. Child and Development an Integrated Approach, 1st ed.; Cengage Learn: Boston, MA, USA, 2011. [Google Scholar]
- Escobar Palomeque, A.M.; Peñaloza Brito, M.P. Relación del Ambiente Familiar, Consumo de Sustancias y Calidad de Vida, con Ansiedad y Depresión, en Adolescentes de 12 a 17 Años, que Asisten a Centros de Acogida y Adicciones, en Quito Cotacachi, Pusuqui, y Guayaquil, Periodo Noviembre 2017 a Julio 2018. Tesis de Licenciatura en Pediatría; Pontificia Universidad Católica Ecuador: Quito, Ecuador, 2018. [Google Scholar]
- Ruíz Cárdenas, C.T.; Jiménez Flores, J.; García Méndez, M.; Flores Herrera, L.M.; Trejo Márquez, H.D. Factores del ambiente familiar predictores de depresión en adolescentes escolares: Análisis por sexo. Rev. Digit. Int. Psicol. Y Cienc. Soc. 2020, 6, 104–122. [Google Scholar]
- Caldera Zamora, I.A.; del Campo Rayas, P.M.; Caldera Montes, J.F.; Reynoso Gonzales, O.U.; Zamora Betancourt, M.R. Predictores de conductas alimentarias de riesgo en estudiantes de bachillerato. RevMexTrastalim 2019, 10, 22–31. [Google Scholar]
- Matera Bryteck, A. Mood and emotional symptoms in eating disorder patients. Arch. Psychiatry Psychother. 2008, 2, 65–71. [Google Scholar]
- Toro, J.; Vilardel, E. Anorexia Nerviosa, 1st ed.; Martinez Roca, S.A.: Barcelona, España, 2000; pp. 88–91. [Google Scholar]
- Gander, M.; Sevecke, K.; Buchheim, A. Eating disorders in adolescence: Attachment issues from a developmental perspective. Front. Psychol. 2015, 6, 1136. [Google Scholar] [CrossRef] [Green Version]
- Holm-Denoma, J.M.; Hankin, B.L.; Young, J.F. Developmental trends of eating disorder symptoms and comorbid internalizing symptoms in children and adolescents. Eat. Behav. 2014, 15, 275–279. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schaumberg, K.; Zerwas, S.; Goodman, E.; Yilmaz, Z.; Bulik, C.M.; Micali, N. Anxiety disorders symptoms at age 10 predict eating disorder symptoms and diagnoses in adolescence. J. Child. Psychol. Psychiatry 2018, 60, 686–696. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morgan-Lowes, K.L.; Clarke, P.J.F.; Hoiles, K.J.; Shu, C.Y.; Watson, H.J.; Dunlop, P.D.; Egan, S.J. The relationships between perfectionism, anxiety and depression across time in pediatric eating disorders. Eat. Behav. 2019, 34, 101305. [Google Scholar] [CrossRef]
- Gómez-Peresmitré, G.; Pineda-García, G.; Platas Acevedo, S.; Velasco Ariza, V. Ansiedad como predictor del riesgo de anorexia y bulimia: Comparación entre universitarios de Baja California y Ciudad de México. Rev. Mex Tras. Aliment. 2017, 8, 49–55. [Google Scholar]
- Nuño Gutiérrez, B.L.; Celis de la Rosa, A.; Unikel Santoncini, C. Prevalencia y factores asociados a las conductas alimentarias de riesgo en adolescentes escolares de Guadalajara según sexo. Rev. Investig. Clin. 2009, 6, 286–293. [Google Scholar]
- de la Vega, M.I.; Gómez -Peresmitré, G. Intervención cognitivo-conductual en conductas alimentarias de riesgo. Rev. Psicol. y Sal. 2012, 22, 225–234. [Google Scholar]
- Gratz, K.L.; Roemer, L. Multidimensional Assessment of Emotion Regulation and Dysregulation: Development, Factor Structure, and Initial Validation of the Difficulties in Emotion Regulation Scale. J. Psychopathol. Behav. Assess 2004, 26, 41–54. [Google Scholar] [CrossRef]
- Campbell-Sills, L.; Barlow, D.H. Incorporating Emotion Regulation into Conceptualizations and Treatments of Anxiety and Mood Disorders. In Handbook of Emotion Regulation; Gross, J.J., Ed.; Guilford Press: New York, NY, USA, 2007; pp. 542–559. [Google Scholar]
- Inzlicht, M.; Bartholow, B.D.; Hirsh, J.B. Emotional foundations of cognitive control. Trends Cogn. Sci. 2015, 19, 126–132. [Google Scholar] [CrossRef] [Green Version]
- Medina Pradas, C.; Navarro, J.B.; López, S.R.; Grau, A.; Obiols, J.E. Dyadic view of expressed emotion, stress, and eating disorder psychopathology. Appetite 2011, 57, 743–748. [Google Scholar] [CrossRef]
- Merry, S.N.; Hetrick, S.E.; Cox, G.R.; Brudevold-Iversen, T.; Bir, J.J.; McDowell, H. Psychological and educational interventions for preventing depression in children and adolescents. Cochrane Database Syst. Rev. 2011, 7, CD003380. [Google Scholar]
- Schuch, F.B.; Vancampfort, D.; Firth, J.; Rosenbaum, S.; Ward, P.B.; Reichert, T.; Stubbs, B. Physical activity and incident depression: A meta-analysis of prospective cohort studies. Am. J. Psychiatry 2018, 175, 631–648. [Google Scholar] [CrossRef] [PubMed]

| Male (n = 181) | Female (n = 376) | |
|---|---|---|
| Living with | ||
| Nuclear family | 135 (74.6%) | 294 (79.1%) |
| Single parent (Mother or father) | 45 (24.9%) | 80 (21.3%) |
| Siblings | 1 (0.6%) | 1 (0.3%) |
| Partner | - | 1 (0.3%) |
| Father’s occupation | ||
| No parent | 36 (19.9%) | 41 (10.9%) |
| Informal economic activity | 23 (12.7%) | 62 (16.5%) |
| Formal economic activity | 121 (66.9%) | 253 (67.3%) |
| Unknown | 1 (0.6%) | 8 (2.1%) |
| Unemployed | - | 12 (3.2%) |
| Father’s education | ||
| No parent | 36 (19.9%) | 41 (10.9%) |
| Basic education | 38 (21%) | 108 (28.7%) |
| Middle education | 59 (32.6%) | 119 (31.6%) |
| Higher education | 48 (26.5%) | 106 (28.2%) |
| No education | - | 2 (0.5%) |
| Mother’s occupation | ||
| No parent | 8 (4.4%) | 5 (1.3%) |
| Informal economic activity | 24 (13.3%) | 47 (12.5%) |
| Formal economic activity | 83 (45.9%) | 182 (48.4%) |
| Unpaid job | 66 (36.5%) | 142 (37.8%) |
| Sexual orientation | ||
| Heterosexual | 136 (75.1%) | 248 (66%) |
| Bisexual | 17 (9.4%) | 99 (26.3%) |
| Homosexual | 16 (8.8%) | 7 (1.9%) |
| Other | 12 (6.6%) | 22 (5.9%) |
| Domestic violence | ||
| Yes | 28 (15.5%) | 123 (32.7%) |
| No | 153 (84.5%) | 253 (67.3%) |
| Use of alcohol and drugs school | ||
| Consumption | 67 (37%) | 177 (47.1%) |
| Nonconsumption | 114 (63%) | 199 (52.9%) |
| Use of alcohol and drugs house | ||
| Consumption | 44 (24.3%) | 143 (38%) |
| Nonconsumption | 137 (75.7%) | 233 (62%) |
| Variables | Pearson Correlation |
|---|---|
| REB | 0.40 ** |
| Anxiety | 0.60 ** |
| Emotional dysregulation | 0.47 ** |
| Sexual orientation | 0.33 ** |
| Violence in the family | −0.26 ** |
| Drugs and alcohol at school | −0.20 ** |
| Drugs and alcohol at home | −0.28 ** |
| Model | R | R Square | R Square Adjusted | Standard Error of the Estimate | Statistics of Changes | ||||
|---|---|---|---|---|---|---|---|---|---|
| Change of Square of R | Change of F | df1 | df2 | Next Change in F | |||||
| 1 | 0.725a | 0.525 | 0.518 | 6.256 | 0.525 | 74.720 | 8 | 541 | 0.000 |
| B | Standard Error | Wald | gl | Sig. | Exp (B) | 95% CI EXP (B) | ||
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| REB | 0.695 | 0.252 | 7.596 | 1 | 0.006 | 2.003 | 1.222 | 3.282 |
| Anxiety | 1.176 | 0.265 | 19.631 | 1 | 0.000 | 3.240 | 1.926 | 5.451 |
| Emotional dysregulation | 1.066 | 0.259 | 16.996 | 1 | 0.000 | 2.903 | 1.749 | 4.819 |
| Sexual orientation | 1.297 | 0.358 | 13.092 | 1 | 0.000 | 3.657 | 1.812 | 7.383 |
| Family violence | −0.810 | 0.341 | 5.651 | 1 | 0.017 | 0.445 | 0.228 | 0.867 |
| Alcohol and drugs at school | −0.728 | 0.267 | 7.445 | 1 | 0.006 | 0.483 | 0.286 | 0.815 |
| Alcohol and drugs at home | −1.189 | 0.355 | 11.242 | 1 | 0.001 | 0.304 | 0.152 | 0.610 |
| Constant | −0.328 | 1.211 | 0.074 | 1 | 0.786 | 0.720 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gómez-Peresmitré, G.; Platas-Acevedo, R.S. Depression Disorders in Mexican Adolescents: A Predictive Model. Children 2023, 10, 1264. https://doi.org/10.3390/children10071264
Gómez-Peresmitré G, Platas-Acevedo RS. Depression Disorders in Mexican Adolescents: A Predictive Model. Children. 2023; 10(7):1264. https://doi.org/10.3390/children10071264
Chicago/Turabian StyleGómez-Peresmitré, Gilda, and Romana Silvia Platas-Acevedo. 2023. "Depression Disorders in Mexican Adolescents: A Predictive Model" Children 10, no. 7: 1264. https://doi.org/10.3390/children10071264