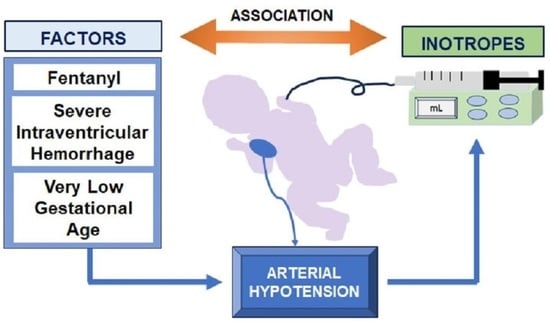
Strong Association between Inotrope Administration and Intraventricular Hemorrhage, Gestational Age, and the Use of Fentanyl in Very Low Gestational Age Infants: A Retrospective Study
Abstract
:1. Introduction
2. Patients and Methods
Statistical Analysis
3. Results
3.1. Maternal, Prenatal, and Neonatal Characteristics of the Treated and Control Groups
3.2. Demographic, Prenatal, and Neonatal Data in the Early Treatment and Late-Treated Subgroups
3.3. Multiple Regression Analyses
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dasgupta, S.J.; Gill, A.B. Hypotension in the Very Low Birthweight Infant: The Old, the New, and the Uncertain. Arch. Dis. Child. Fetal Neonatal Ed. 2003, 88, F450–F454. [Google Scholar] [CrossRef]
- Song, Y.H.; Lee, J.A.; Choi, B.M.; Lim, J.W. Risk Factors and Prognosis in Very Low Birth Weight Infants Treated for Hypotension during the First Postnatal Week from the Korean Neonatal Network. PLoS ONE 2021, 16, e0258328. [Google Scholar] [CrossRef]
- Kim, T.-H.; Moon, C.-J.; Sung, I.K.; Youn, Y.A. Hypotension within 1 Week of Life Associated with Poor Short- and Long-Term Outcomes in Very Low Birth Weight Infants. Cardiol. Young 2018, 28, 1037–1041. [Google Scholar] [CrossRef]
- Durrmeyer, X.; Marchand-Martin, L.; Porcher, R.; Gascoin, G.; Roze, J.-C.; Storme, L.; Favrais, G.; Ancel, P.-Y.; Cambonie, G.; Hemodynamic EPIPAGE 2 Study Group. Abstention or Intervention for Isolated Hypotension in the First 3 Days of Life in Extremely Preterm Infants: Association with Short-Term Outcomes in the EPIPAGE 2 Cohort Study. Arch. Dis. Child. Fetal Neonatal Ed. 2017, 102, 490–496. [Google Scholar] [CrossRef] [PubMed]
- Samuels, N.; van de Graaf, R.A.; de Jonge, R.C.J.; Reiss, I.K.M.; Vermeulen, M.J. Risk Factors for Necrotizing Enterocolitis in Neonates: A Systematic Review of Prognostic Studies. BMC Pediatr. 2017, 17, 105. [Google Scholar] [CrossRef]
- Faust, K.; Härtel, C.; Preuß, M.; Rabe, H.; Roll, C.; Emeis, M.; Wieg, C.; Szabo, M.; Herting, E.; Göpel, W.; et al. Short-Term Outcome of Very-Low-Birthweight Infants with Arterial Hypotension in the First 24 h of Life. Arch. Dis. Child. Fetal Neonatal Ed. 2015, 100, F388–F392. [Google Scholar] [CrossRef]
- Batton, B.; Zhu, X.; Fanaroff, J.; Kirchner, H.L.; Berlin, S.; Wilson-Costello, D.; Walsh, M. Blood Pressure, Anti-Hypotensive Therapy, and Neurodevelopment in Extremely Preterm Infants. J. Pediatr. 2009, 154, 351–357. [Google Scholar] [CrossRef] [PubMed]
- Batton, B.J.; Li, L.; Newman, N.S.; Das, A.; Watterberg, K.L.; Yoder, B.A.; Faix, R.G.; Laughon, M.M.; Van Meurs, K.P.; Carlo, W.A.; et al. Feasibility Study of Early Blood Pressure Management in Extremely Preterm Infants. J. Pediatr. 2012, 161, 65–69. [Google Scholar] [CrossRef]
- Gurram Venkata, S.K.R.; Srivastava, A.; Murthy, P.; Scott, J.N.; Zein, H.; Leijser, L.; Ghosh, A.; Momin, S.; Thomas, S.; Mohammad, K. Hemodynamic Quality Improvement Bundle to Reduce the Use of Inotropes in Extreme Preterm Neonates. Paediatr. Drugs 2022, 24, 259–267. [Google Scholar] [CrossRef] [PubMed]
- Miller, L.E.; Laughon, M.M.; Clark, R.H.; Zimmerman, K.O.; Hornik, C.P.; Aleem, S.; Brian Smith, P.; Greenberg, R.G. Vasoactive Medications in Extremely Low Gestational Age Neonates during the First Postnatal Week. J. Perinatol. 2021, 41, 2330–2336. [Google Scholar] [CrossRef]
- Sarafidis, K.; Verykouki, E.; Nikopoulos, S.; Apostolidou-Kiouti, F.; Diakonidis, T.; Agakidou, E.; Kontou, A.; Haidich, A.-B. Systematic Review and Meta-Analysis of Cardiovascular Medications in Neonatal Hypotension. Biomed. Hub 2022, 7, 70–79. [Google Scholar] [CrossRef] [PubMed]
- Lasky, T.; Greenspan, J.; Ernst, F.R.; Gonzalez, L. Dopamine and Dobutamine Use in Preterm or Low Birth Weight Neonates in the Premier 2008 Database. Clin. Ther. 2011, 33, 2082–2088. [Google Scholar] [CrossRef] [PubMed]
- Burns, M.L.; Stensvold, H.J.; Risnes, K.; Guthe, H.J.; Astrup, H.; Nordhov, S.M.; Selberg, T.R.; Rønnestad, A.; Lang, A.M.; Norwegian Neonatal Network. Inotropic Therapy in Newborns, A Population-Based National Registry Study. Pediatr. Crit. Care Med. 2016, 17, 948–956. [Google Scholar] [CrossRef] [PubMed]
- Giesinger, R.E.; McNamara, P.J. Hemodynamic Instability in the Critically Ill Neonate: An Approach to Cardiovascular Support Based on Disease Pathophysiology. Semin. Perinatol. 2016, 40, 174–188. [Google Scholar] [CrossRef] [PubMed]
- Papile, L.A.; Burstein, J.; Burstein, R.; Koffler, H. Incidence and Evolution of Subependymal and Intraventricular Hemorrhage: A Study of Infants with Birth Weights Less than 1500 Gm. J. Pediatr. 1978, 92, 529–534. [Google Scholar] [CrossRef]
- Miall-Allen, V.M.; de Vries, L.S.; Whitelaw, A.G. Mean Arterial Blood Pressure and Neonatal Cerebral Lesions. Arch. Dis. Child. 1987, 62, 1068–1069. [Google Scholar] [CrossRef] [PubMed]
- Bada, H.S.; Korones, S.B.; Perry, E.H.; Arheart, K.L.; Ray, J.D.; Pourcyrous, M.; Magill, H.L.; Runyan, W.; Somes, G.W.; Clark, F.C. Mean Arterial Blood Pressure Changes in Premature Infants and Those at Risk for Intraventricular Hemorrhage. J. Pediatr. 1990, 117, 607–614. [Google Scholar] [CrossRef]
- Watkins, A.M.; West, C.R.; Cooke, R.W. Blood Pressure and Cerebral Haemorrhage and Ischaemia in Very Low Birthweight Infants. Early Hum. Dev. 1989, 19, 103–110. [Google Scholar] [CrossRef]
- Fanaroff, J.M.; Wilson-Costello, D.E.; Newman, N.S.; Montpetite, M.M.; Fanaroff, A.A. Treated Hypotension Is Associated with Neonatal Morbidity and Hearing Loss in Extremely Low Birth Weight Infants. Pediatrics 2006, 117, 1131–1135. [Google Scholar] [CrossRef]
- Batton, B.; Li, L.; Newman, N.S.; Das, A.; Watterberg, K.L.; Yoder, B.A.; Faix, R.G.; Laughon, M.M.; Stoll, B.J.; Van Meurs, K.P.; et al. Use of Antihypotensive Therapies in Extremely Preterm Infants. Pediatrics 2013, 131, e1865–e1873. [Google Scholar] [CrossRef] [PubMed]
- Vesoulis, Z.A.; Flower, A.A.; Zanelli, S.; Rambhia, A.; Abubakar, M.; Whitehead, H.V.; Fairchild, K.D.; Mathur, A.M. Blood Pressure Extremes and Severe IVH in Preterm Infants. Pediatr. Res. 2020, 87, 69–73. [Google Scholar] [CrossRef]
- Pellicer, A.; Bravo, M.d.C.; Madero, R.; Salas, S.; Quero, J.; Cabañas, F. Early Systemic Hypotension and Vasopressor Support in Low Birth Weight Infants: Impact on Neurodevelopment. Pediatrics 2009, 123, 1369–1376. [Google Scholar] [CrossRef]
- Logan, J.W.; O’Shea, T.M.; Allred, E.N.; Laughon, M.M.; Bose, C.L.; Dammann, O.; Batton, D.G.; Engelke, S.C.; Leviton, A.; ELGAN Study Investigators Early Postnatal. Hypotension and Developmental Delay at 24 Months of Age among Extremely Low Gestational Age Newborns. Arch. Dis. Child. Fetal Neonatal Ed. 2011, 96, F321–F328. [Google Scholar] [CrossRef]
- Alderliesten, T.; Lemmers, P.M.A.; van Haastert, I.C.; de Vries, L.S.; Bonestroo, H.J.C.; Baerts, W.; van Bel, F. Hypotension in Preterm Neonates: Low Blood Pressure Alone Does Not Affect Neurodevelopmental Outcome. J. Pediatr. 2014, 164, 986–991. [Google Scholar] [CrossRef] [PubMed]
- Dempsey, E.M.; Barrington, K.J.; Marlow, N.; O’Donnell, C.P.F.; Miletin, J.; Naulaers, G.; Cheung, P.-Y.; Corcoran, J.D.; El-Khuffash, A.F.; Boylan, G.B.; et al. Hypotension in Preterm Infants (HIP) Randomised Trial. Arch. Dis. Child. Fetal Neonatal Ed. 2021, 106, 398–403. [Google Scholar] [CrossRef] [PubMed]
- Tofthagen, C. Threats to Validity in Retrospective Studies. J. Adv. Pract. Oncol. 2012, 3, 181. [Google Scholar]
- Zubrow, A.B.; Hulman, S.; Kushner, H.; Falkner, B. Determinants of Blood Pressure in Infants Admitted to Neonatal Intensive Care Units: A Prospective Multicenter Study. Philadelphia Neonatal Blood Pressure Study Group. J. Perinatol. 1995, 15, 470–479. [Google Scholar]
- Hegyi, T.; Carbone, M.T.; Anwar, M.; Ostfeld, B.; Hiatt, M.; Koons, A.; Pinto-Martin, J.; Paneth, N. Blood Pressure Ranges in Premature Infants. I. The First Hours of Life. J. Pediatr. 1994, 124, 627–633. [Google Scholar] [CrossRef] [PubMed]
- Laughon, M.; Bose, C.; Allred, E.; O’Shea, T.M.; Van Marter, L.J.; Bednarek, F.; Leviton, A.; ELGAN Study Investigators. Factors Associated with Treatment for Hypotension in Extremely Low Gestational Age Newborns during the First Postnatal Week. Pediatrics 2007, 119, 273–280. [Google Scholar] [CrossRef] [PubMed]
- Abdul Aziz, A.N.; Thomas, S.; Murthy, P.; Rabi, Y.; Soraisham, A.; Stritzke, A.; Kamaluddeen, M.; Al-Awad, E.; Mohammad, K. Early Inotropes Use Is Associated with Higher Risk of Death and/or Severe Brain Injury in Extremely Premature Infants. J. Matern. Neonatal Med. 2020, 33, 2751–2758. [Google Scholar] [CrossRef] [PubMed]
- Yanowitz, T.D.; Baker, R.W.; Roberts, J.M.; Brozanski, B.S. Low Blood Pressure among Very-Low-Birth-Weight Infants with Fetal Vessel Inflammation. J. Perinatol. 2004, 24, 299–304. [Google Scholar] [CrossRef] [PubMed]
- Pejovic, B.; Peco-Antic, A.; Marinkovic-Eric, J. Blood Pressure in Non-Critically Ill Preterm and Full-Term Neonates. Pediatr. Nephrol. 2007, 22, 249–257. [Google Scholar] [CrossRef] [PubMed]
- Kent, A.L.; Chaudhari, T. Determinants of Neonatal Blood Pressure. Curr. Hypertens. Rep. 2013, 15, 426–432. [Google Scholar] [CrossRef] [PubMed]
- Smal, J.C.; Uiterwaal, C.S.P.M.; Bruinse, H.W.; Steendijk, P.; van Bel, F. Inverse Relationship between Birth Weight and Blood Pressure in Growth-Retarded but Not in Appropriate for Gestational Age Infants during the First Week of Life. Neonatology 2009, 96, 86–92. [Google Scholar] [CrossRef] [PubMed]
- Ziesenitz, V.C.; Vaughns, J.D.; Koch, G.; Mikus, G.; van den Anker, J.N. Pharmacokinetics of Fentanyl and Its Derivatives in Children: A Comprehensive Review. Clin. Pharmacokinet. 2018, 57, 125–149. [Google Scholar] [CrossRef] [PubMed]
- Lampe, R.; Rieger-Fackeldey, E.; Sidorenko, I.; Turova, V.; Botkin, N.; Eckardt, L.; Alves-Pinto, A.; Kovtanyuk, A.; Schündeln, M.; Felderhoff-Müser, U. Assessing Key Clinical Parameters before and after Intraventricular Hemorrhage in Very Preterm Infants. Eur. J. Pediatr. 2020, 179, 929–937. [Google Scholar] [CrossRef]
- Welzing, L.; Oberthuer, A.; Junghaenel, S.; Harnischmacher, U.; Stützer, H.; Roth, B. Remifentanil/Midazolam versus Fentanyl/Midazolam for Analgesia and Sedation of Mechanically Ventilated Neonates and Young Infants: A Randomized Controlled Trial. Intensiv. Care Med. 2012, 38, 1017–1024. [Google Scholar] [CrossRef]
- Ancora, G.; Lago, P.; Garetti, E.; Pirelli, A.; Merazzi, D.; Mastrocola, M.; Pierantoni, L.; Faldella, G. Efficacy and Safety of Continuous Infusion of Fentanyl for Pain Control in Preterm Newborns on Mechanical Ventilation. J. Pediatr. 2013, 163, 645–651. [Google Scholar] [CrossRef]
- Madathil, S.; Thomas, D.; Chandra, P.; Agarwal, R.; Sankar, M.J.; Thukral, A.; Deorari, A. “NOPAIN-ROP” Trial: Intravenous Fentanyl and Intravenous Ketamine for Pain Relief during Laser Photocoagulation for Retinopathy of Prematurity (ROP) in Preterm Infants: A Randomised Trial. BMJ Open 2021, 11, e046235. [Google Scholar] [CrossRef] [PubMed]
- Bäcke, P.; Bruschettini, M.; Sibrecht, G.; Thernström Blomqvist, Y.; Olsson, E. Pharmacological Interventions for Pain and Sedation Management in Newborn Infants Undergoing Therapeutic Hypothermia. Cochrane Database Syst. Rev. 2022, 11, CD015023. [Google Scholar] [CrossRef]
- Bellù, R.; Romantsik, O.; Nava, C.; de Waal, K.A.; Zanini, R.; Bruschettini, M. Opioids for Newborn Infants Receiving Mechanical Ventilation. Cochrane Database Syst. Rev. 2021, 3, CD013732. [Google Scholar] [CrossRef]
- Engstrom, K.; Brown, C.S.; Mattson, A.E.; Lyons, N.; Rech, M.A. Pharmacotherapy Optimization for Rapid Sequence Intubation in the Emergency Department. Am. J. Emerg. Med. 2023, 70, 19–29. [Google Scholar] [CrossRef] [PubMed]
- Sudo, Y.; Seki-Nagasawa, J.; Kajikawa, D.; Kuratsuji, G.; Haga, M.; Shokraneh, F.; Yamaji, N.; Ota, E.; Namba, F. Effect of Fentanyl for Preterm Infants on Mechanical Ventilation: A Systematic Review and Meta-Analysis. Neonatology 2023, 120, 287–294. [Google Scholar] [CrossRef] [PubMed]
- Kinoshita, M.; Olsson, E.; Borys, F.; Bruschettini, M. Opioids for Procedural Pain in Neonates. Cochrane Database Syst. Rev. 2023, 4, CD015056. [Google Scholar] [CrossRef] [PubMed]
- Ojha, S.; Abramson, J.; Dorling, J. Sedation and Analgesia from Prolonged Pain and Stress during Mechanical Ventilation in Preterm Infants: Is Dexmedetomidine an Alternative to Current Practice? BMJ Paediatr. Open 2022, 6, e001460. [Google Scholar] [CrossRef] [PubMed]



| Inotrope | Number (%) of Treated Neonates |
|---|---|
| Dopamine | 73 (88) |
| Dobutamine | 37 (44.6) |
| Epinephrine | 13 (15.7) |
| Norepinephrine | 11 (13.3) |
| Milrinone | 5 (6.0) |
| Characteristics | Groups of Neonates | p-Value | |
|---|---|---|---|
| Control | Treated | ||
| N | 139 | 83 | |
| Maternal data | |||
| Hypertension $ | 25 (18.0) | 12 (14.5) | 0.751 £ |
| Chorioamnionitis $ | 17 (12.2) | 17 (20.5) | 0.123 £ |
| Prenatal steroids $ | 123 (88.5) | 74 (89.2) | 1.0 £ |
| Mg administration $ | 60 (46.5) | 40 (51.9) | 0.541 £ |
| Anesthesia for labor/CS $ | 117 (84.2) | 60 (72.3) | 0.176 £ |
| Caesarean section $ | 122 (87.8) | 65 (78.3) | 0.093 £ |
| Inborn $ | 133 (95.7) | 77 (92.8) | 0.534 £ |
| Delayed cord clamping $ | 70 (50.4) | 30 (36.7) | 0.055 £ |
| PPROM $ | 36 (25.9) | 26 (31.3) | 0.473 £ |
| Neonatal data | |||
| Gestational age (wks) * | 30 (28; 31) | 26 (24; 29) | <0.001 # |
| Birth weight (g) * | 1270 (1110; 1540) | 810 (632; 1085) | <0.001 # |
| 1 min Apgar score * | 7 (6; 8) | 5 (4; 7) | <0.001 # |
| 5 min Apgar score * | 9 (8; 9) | 8 (7; 8) | <0.001 # |
| Base deficit on NICU admission * | −5.4 (−7.3; −3.6) | −7 (−9.6; −4.8) | <0.001 # |
| pH on admission * | 7.32 (7.27; 7.38) | 7.30 (7.24; 7.37) | 0.101 # |
| Male sex $ | 55 (39.6) | 43 (51.8) | 0.102 £ |
| SGA $ | 10 (7.2) | 10 (12.0) | 0.327 £ |
| IUGR $ | 23 (16.5) | 17 (20.5) | 0.557 £ |
| Intubation at birth $ | 26 (18.7) | 52 (62.7) | <0.001 £ |
| Surfactant at birth $ | 14 (10.1) | 27 (32.5) | <0.001 £ |
| Symptomatic PDA $ | 13 (9.4) | 35 (42.2) | <0.001 £ |
| Severe IVH $ | 3 (2.2) | 33 (39.8) | <0.001 £ |
| Pulmonary hemorrhage $ | 8 (5.8) | 21 (25.3) | <0.001 £ |
| Air-leak syndromes $ | 5 (3.6) | 9 (10.8) | 0.044 £ |
| Sepsis (confirmed early or late) $ | 50 (36) | 49 (59) | 0.001 £ |
| Septic shock $ | 6 (4.3) | 28 (33.7) | <0.001 £ |
| Fentanyl monotherapy $ | 11 (7.9) | 21 (25.3) | 0.002 £ |
| Sedative monotherapy $ | 0 (0) | 10 (12) | <0.001 £ |
| Fentanyl and sedatives $ | 2 (1.4) | 22 (26.5) | <0.001 £ |
| NEC stage II, III $ | 8 (5.8) | 10 (12.0) | 0.159 £ |
| Surgical NEC $ | 2 (1.4) | 6 (7.2) | 0.055 £ |
| BPD any grade $ | 52 (37.4) | 27 (32.5) | 0.555 £ |
| RDS $ | 73 (52.5) | 62 (74.7) | 0.001 £ |
| Overall mechanical ventilation $ | 125 (89.9) | 82 (98.8) | 0.011 £ |
| Invasive ventilation $ | 46 (33.1) | 80 (96.4) | <0.001 £ |
| Non-invasive ventilation $ | 116 (83.5) | 42 (50.6) | <0.001 £ |
| Survival $ | 130 (96.3) | 34 (42.0) | <0.001 £ |
| Days in NICU for all population * | 50 (41; 69.7) | 17 (6.3; 80.5) | <0.001 # |
| Days in NICU for survivors * | 52 (42; 70) | 95 (63; 134) | <0.001 # |
| Days in NICU for non-survivors * | 5.0 (1.5; 12.5) | 7.5 (2.5; 15) | 0.432 # |
| Characteristics | Subgroups of Treated Neonates | p | |
|---|---|---|---|
| Early-Treated | Late -Treated | ||
| N | 56 | 27 | |
| Maternal data | |||
| Hypertension $ | 5 (10) | 7 (28) | 0.091 £ |
| Chorioamnionitis $ | 14 (26.9) | 3 (11.1) | 0.150 £ |
| Prenatal steroids $ | 49 (87.5) | 25 (92.6) | 0.711 £ |
| Mg $ | 25 (48.1) | 15 (60.0) | 0.461 £ |
| Anesthesia for labor/CS $ | 37 (66.2) | 23 (85.2) | 0.140 £ |
| Caesarean section $ | 43 (76.8) | 22 (81.5) | 0.779 £ |
| Inborn $ | 53 (94.6) | 24 (88.9) | 0.385 £ |
| Delayed cord clamping $ | 16 (28.6) | 14 (51.9) | 0.068 £ |
| PPROM $ | 20 (35.7) | 6 (22.2) | 0.323 £ |
| Neonatal data | |||
| Gestational age (wks) * | 26 (24; 29) | 27 (24; 27) | 0.018 # |
| Birth weight (g) * | 725 (602; 1220) | 865 (746; 1220) | 0.194 # |
| 1 min Apgar score * | 5 (3; 7) | 7 (4; 7) | 0.092 # |
| 5 min Apgar score * | 8 (7; 8) | 8 (8; 9) | 0.001 # |
| Base deficit on NICU admission * | −7.9 (−12.6; −6.0) | −5 (−6.6; −3.2) | <0.001 # |
| pH on admission * | 7.29 (7.23; 7.35) | 7.33 (7.30; 7.41) | 0.008 # |
| Male sex $ | 31 (55.4) | 12 (44.4) | 0.064 £ |
| SGA $ | 4 (7.1) | 6 (22.2) | 0.071 £ |
| IUGR $ | 7 (12.5) | 10 (37.0) | 0.021 £ |
| Intubation at birth $ | 39 (69.6) | 13 (48.1) | 0.098 £ |
| Surfactant at birth $ | 19 (33.9) | 8 (29.6) | 0.805 £ |
| Symptomatic PDA $ | 23 (41.1) | 12/27 (44.4) | 0.957 £ |
| Severe IVH $ | 28 (50.0) | 5 (18.5) | 0.008 £ |
| Pulmonary hemorrhage $ | 16 (28.6) | 5 (18.5) | 0.423 £ |
| Air-leak syndromes $ | 9 (16.1) | 0 (0) | 0.028 £ |
| Sepsis (confirmed early or late) $ | 28 (50.0) | 21 (77.8) | 0.030 £ |
| Septic shock $ | 13 (23.2) | 15 (55.6) | 0.008 £ |
| Fentanyl monotherapy $ | 13 (23.2) | 7 (25.9) | 1.0 £ |
| Sedative monotherapy $ | 6 (10.7) | 4 (15.4) | 0.718 £ |
| Fentanyl and sedatives $ | 17 (30.4) | 5 (18.5) | 0.423 £ |
| NEC stage II–III $ | 4 (7.2) | 6 (22.2) | 0.071 £ |
| Surgical NEC $ | 3 (5.4) | 3 (11.1) | 0.385 £ |
| BPD any stage $ | 13 (23.2) | 14 (51.9) | 0.018 £ |
| RDS $ | 40 (71.4) | 22 (81.5) | 0.423 £ |
| Overall mechanical ventilation $ | 55 (98.2) | 27 (100) | 0.999 £ |
| Invasive ventilation $ | 54 (96.4) | 26 (96.3) | 0.999 £ |
| Non-invasive ventilation $ | 21 (37.5) | 21 (13.3) | 0.001 £ |
| Survival $ | 17 (30.9) | 17 (65.4) | 0.004 £ |
| Days in NICU for all population * | 11 (4; 50) | 63 (23.5; 98.5) | <0.001 # |
| Days in NICU for survivors * | 88 (62; 133) | 65 (63; 138) | 0.823 # |
| Days in NICU for non-survivors * | 7 (1.7; 12.5) | 16.5 (6.75; 28.5) | 0.014 # |
| Significant Independent Factors | Odds Ratio | Confidence Intervals | p-Value | |
|---|---|---|---|---|
| Lower | Upper | |||
| GA | 0.74 | 0.63 | 0.86 | <0.001 |
| Fentanyl | 4.66 | 2.05 | 10.88 | <0.001 |
| SIVH | 6.67 | 1.94 | 31.19 | 0.01 |
| Septic shock | 4.95 | 1.76 | 15.45 | <0.001 |
| Discriminating ability | ||||
| AUC | 0.88 | 0.84 | 0.93 | |
| Threshold | 0.34 | |||
| Specificity | 0.86 | |||
| Sensitivity | 0.82 | |||
| Significant Independent Factors | Odds Ratio | Confidence Intervals | p-Value | |
|---|---|---|---|---|
| Lower | Upper | |||
| GA | 0.769 | 0.648 | 0.908 | 0.002 |
| Base deficit | 0.900 | 0.806 | 0.989 | 0.042 |
| Fentanyl ± sedatives | 4.089 | 1.809 | 9.329 | 0.001 |
| SIVH | 5.544 | 2.032 | 16.157 | 0.001 |
| Discriminating ability | ||||
| AUC | 0.877 | 0.824 | 0.932 | |
| Threshold | 0.272 | |||
| Specificity | 0.861 | |||
| Sensitivity | 0.804 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stathopoulou, T.; Agakidou, E.; Paschaloudis, C.; Kontou, A.; Chatzioannidis, I.; Sarafidis, K. Strong Association between Inotrope Administration and Intraventricular Hemorrhage, Gestational Age, and the Use of Fentanyl in Very Low Gestational Age Infants: A Retrospective Study. Children 2023, 10, 1667. https://doi.org/10.3390/children10101667
Stathopoulou T, Agakidou E, Paschaloudis C, Kontou A, Chatzioannidis I, Sarafidis K. Strong Association between Inotrope Administration and Intraventricular Hemorrhage, Gestational Age, and the Use of Fentanyl in Very Low Gestational Age Infants: A Retrospective Study. Children. 2023; 10(10):1667. https://doi.org/10.3390/children10101667
Chicago/Turabian StyleStathopoulou, Theodora, Eleni Agakidou, Christos Paschaloudis, Angeliki Kontou, Ilias Chatzioannidis, and Kosmas Sarafidis. 2023. "Strong Association between Inotrope Administration and Intraventricular Hemorrhage, Gestational Age, and the Use of Fentanyl in Very Low Gestational Age Infants: A Retrospective Study" Children 10, no. 10: 1667. https://doi.org/10.3390/children10101667