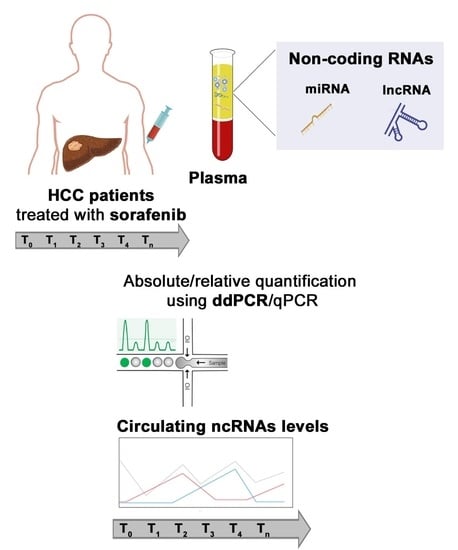
Longitudinal Circulating Levels of miR-23b-3p, miR-126-3p and lncRNA GAS5 in HCC Patients Treated with Sorafenib
Abstract
:1. Introduction
2. Materials and Methods
2.1. Liquid Biopsies Collection of Sorafenib Treated HCC Patients
2.2. Liquid Biopsies Collection of Untreated HCC Patients and Healthy Individuals
2.3. RNA Isolation from Plasma
2.4. Quantitative Real-Time PCR (qPCR)
2.5. Droplet Digital PCR Workflow
2.6. Statistical Analysis
3. Results
Amounts of GAS5, miR-126-3p and miR-23b-3p in the Plasma of Patients Treated with Sorafenib
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Hombach, S.; Kretz, M. Non-coding RNAs: Classification, biology and functioning. Adv. Exp. Med. Biol. 2016, 937, 3–17. [Google Scholar] [CrossRef] [PubMed]
- Tordonato, C.; Di Fiore, P.P.; Nicassio, F. The role of non-coding RNAs in the regulation of stem cells and progenitors in the normal mammary gland and in breast tumors. Front. Genet. 2015, 5. [Google Scholar] [CrossRef] [Green Version]
- Grossi, I.; Radeghieri, A.; PaoliniDI, L.; Porrini, V.; Pilotto, A.; Padovani, A.; Marengoni, A.; Barbon, A.; Bellucci, A.; Pizzi, M.; et al. MicroRNA-34a-5p expression in the plasma and in its extracellular vesicle fractions in subjects with Parkinson’s disease: An exploratory study. Int. J. Mol. Med. 2021, 47, 533–546. [Google Scholar] [CrossRef] [PubMed]
- Salvi, A.; Vezzoli, M.; Busatto, S.; Paolini, L.; Faranda, T.; Abeni, E.; Caracausi, M.; Antonaros, F.; Piovesan, A.; Locatelli, C.; et al. Analysis of a nanoparticle-enriched fraction of plasma reveals miRNA candidates for Down syndrome pathogenesis. Int. J. Mol. Med. 2019, 43, 2303–2318. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moshiri, F.; Salvi, A.; Gramantieri, L.; Sangiovanni, A.; Guerriero, P.; De Petro, G.; Bassi, C.; Lupini, L.; Sattari, A.; Cheung, D.; et al. Circulating miR-106b-3p, miR-101-3p and miR-1246 as diagnostic biomarkers of hepatocellular carcinoma. Oncotarget 2018, 9, 15350–15364. [Google Scholar] [CrossRef] [PubMed]
- Sohel, M.H. Extracellular/Circulating microRNAs: Release mechanisms, functions and challenges. Achiev. Life. Sci. 2016, 10, 542–568. [Google Scholar] [CrossRef] [Green Version]
- Silva, A.; Bullock, M.; Calin, G. The clinical relevance of long non-coding RNAs in cancer. Cancers 2015, 7, 2169–2182. [Google Scholar] [CrossRef]
- Hahne, J.C.; Valeri, N. Non-coding RNAs and resistance to anticancer drugs in gastrointestinal tumors. Front. Oncol. 2018, 8, 226–252. [Google Scholar] [CrossRef] [Green Version]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA. Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [Green Version]
- Kudo, M. Systemic therapy for hepatocellular carcinoma: Latest advances. Cancers 2018, 10, 412. [Google Scholar] [CrossRef] [Green Version]
- Kudo, M.; Finn, R.S.; Qin, S.; Han, K.H.; Ikeda, K.; Piscaglia, F.; Baron, A.; Park, J.W.; Han, G.; Jassem, J.; et al. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: A randomised phase 3 non-inferiority trial. Lancet 2018, 391, 1163–1173. [Google Scholar] [CrossRef] [Green Version]
- Finn, R.S.; Qin, S.; Ikeda, M.; Galle, P.R.; Ducreux, M.; Kim, T.-Y.; Kudo, M.; Breder, V.; Merle, P.; Kaseb, A.O.; et al. Atezolizumab plus Bevacizumab in unresectable hepatocellular carcinoma. N. Engl. J. Med. 2020, 382, 1894–1905. [Google Scholar] [CrossRef] [PubMed]
- Cervello, M.; Bachvarov, D.; Lampiasi, N.; Cusimano, A.; Azzolina, A.; McCubrey, J.A.; Montalto, G. Molecular mechanisms of sorafenib action in liver cancer cells. Cell. Cycle 2012, 11, 2843–2855. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abeni, E.; Salvi, A.; Marchina, E.; Traversa, M.; Arici, B.; De Petro, G. Sorafenib induces variations of the DNA methylome in HA22T/VGH human hepatocellular carcinoma-derived cells. Int. J. Oncol. 2017, 51, 128–144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kanthaje, S.; Makol, A.; Chakraborti, A. Sorafenib response in hepatocellular carcinoma: microRNAs as tuning forks. Hepatol. Res. 2018, 48, 5–14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Keating, G.M. Sorafenib: A review in hepatocellular carcinoma. Target. Oncol. 2017, 12, 243–253. [Google Scholar] [CrossRef] [PubMed]
- Gauthier, A.; Ho, M. Role of sorafenib in the treatment of advanced hepatocellular carcinoma: An update. Hepatol. Res. 2013, 43, 147–154. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ghidini, M.; Hahne, J.C.; Frizziero, M.; Tomasello, G.; Trevisani, F.; Lampis, A.; Passalacqua, R.; Valeri, N. MicroRNAs as mediators of resistance mechanisms to small-molecule tyrosine kinase inhibitors in solid tumours. Target. Oncol. 2018, 13, 423–436. [Google Scholar] [CrossRef] [PubMed]
- Galle, P.R.; Forner, A.; Llovet, J.M.; Mazzaferro, V.; Piscaglia, F.; Raoul, J.L.; Schirmacher, P.; Vilgrain, V. EASL clinical practice guidelines: Management of hepatocellular carcinoma. J. Hepatol. 2018, 69, 182–236. [Google Scholar] [CrossRef] [Green Version]
- Faranda, T.; Grossi, I.; Manganelli, M.; Marchina, E.; Baiocchi, G.; Portolani, N.; Crosatti, M.; De Petro, G.; Salvi, A. Differential expression profiling of long non-coding RNA GAS5 and miR-126-3p in human cancer cells in response to sorafenib. Sci. Rep. 2019, 9, 9118. [Google Scholar] [CrossRef] [Green Version]
- Grossi, I.; Salvi, A.; Baiocchi, G.; Portolani, N.; De Petro, G. Functional role of microRNA-23b-3p in cancer biology. MicroRNA 2018, 7, 156–166. [Google Scholar] [CrossRef]
- Salvi, A.; Sabelli, C.; Moncini, S.; Venturin, M.; Arici, B.; Riva, P.; Portolani, N.; Giulini, S.M.; De Petro, G.; Barlati, S. MicroRNA-23b mediates urokinase and c-met downmodulation and a decreased migration of human hepatocellular carcinoma cells. FEBS J. 2009, 276, 2966–2982. [Google Scholar] [CrossRef] [PubMed]
- Grossi, I.; Arici, B.; Portolani, N.; De Petro, G.; Salvi, A. Clinical and biological significance of miR-23b and miR-193a in human hepatocellular carcinoma. Oncotarget 2017, 8, 6955–6969. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, Y.; Zhao, J.; Zhang, W.; Gan, J.; Hu, C.; Huang, G.; Zhang, Y. IncRNA GAS5 enhances G1 cell cycle arrest via binding to YBX1 to regulate p21 expression in stomach cancer. Sci. Rep. 2015, 5. [Google Scholar] [CrossRef] [Green Version]
- Yu, Y.; Hann, S.S. Novel tumor suppressor lncRNA growth arrest-specific 5 (GAS5) in human cancer. Onco. Targets. Ther. 2019, 12, 8421–8436. [Google Scholar] [CrossRef] [Green Version]
- Isin, M.; Ozgur, E.; Cetin, G.; Erten, N.; Aktan, M.; Gezer, U.; Dalay, N. Investigation of circulating lncRNAs in B-cell neoplasms. Clin. Chim. Acta 2014, 431, 255–259. [Google Scholar] [CrossRef] [PubMed]
- Hu, M.H.; Ma, C.Y.; Wang, X.M.; Ye, C.D.; Zhang, G.X.; Chen, L.; Wang, J.G. MicroRNA-126 inhibits tumor proliferation and angiogenesis of hepatocellular carcinoma by down-regulating EGFL7 expression. Oncotarget 2016, 7, 66922–66934. [Google Scholar] [CrossRef] [Green Version]
- Du, C.; Lv, Z.; Cao, L.; Ding, C.; Gyabaah, O.-A.K.; Xie, H.; Zhou, L.; Wu, J.; Zheng, S. MiR-126-3p suppresses tumor metastasis and angiogenesis of hepatocellular carcinoma by targeting LRP6 and PIK3R2. J. Transl. Med. 2014, 12, 259. [Google Scholar] [CrossRef] [Green Version]
- Xiang, L.Y.; Ou, H.H.; Liu, X.C.; Chen, Z.J.; Li, X.H.; Huang, Y.; Yang, D.H. Loss of tumor suppressor miR-126 contributes to the development of hepatitis B virus-related hepatocellular carcinoma metastasis through the upregulation of ADAM9. Tumor. Biol. 2017, 39, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mensah, M.; Borzi, C.; Verri, C.; Suatoni, P.; Conte, D.; Pastorino, U.; Orazio, F.; Sozzi, G.; Boeri, M. MicroRNA based liquid biopsy: The experience of the plasma miRNA signature classifier (MSC) for lung cancer screening. J. Vis. Exp. 2017, 56326. [Google Scholar] [CrossRef]
- Fortunato, O.; Boeri, M.; Verri, C.; Conte, D.; Mensah, M.; Suatoni, P.; Pastorino, U.; Sozzi, G. Assessment of circulating micrornas in plasma of lung cancer patients. Molecules 2014, 19, 3038–3054. [Google Scholar] [CrossRef] [Green Version]
- Wang, H.; Peng, R.; Wang, J.; Qin, Z.; Xue, L. Circulating microRNAs as potential cancer biomarkers: The advantage and disadvantage. Clin. Epigenetics 2018, 10, 59. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Silvestris, N.; Ciliberto, G.; De Paoli, P.; Apolone, G.; Lavitrano, M.L.; Pierotti, M.A.; Stanta, G. Liquid dynamic medicine and N-of-1 clinical trials: A change of perspective in oncology research. J. Exp. Clin. Cancer Res. 2017, 36, 128. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chauhan, R.; Lahiri, N. Tissue- and Serum-Associated Biomarkers of Hepatocellular Carcinoma. Biomark. Cancer 2016, 8, 37–55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Malov, S.I.; Malov, I.V.; Dvornichenko, V.V.; Marche, P.N.; Decaens, T.; Macek-Jilkova, Z.; Yushchuk, N.D. Biomarkers in diagnosis and prediction of hepatocellular carcinoma recurrence (Review). Sovrem. Tehnol. Med. 2019, 11, 183. [Google Scholar] [CrossRef]
- Fayda, M.; Isin, M.; Tambas, M.; Guveli, M.; Meral, R.; Altun, M.; Sahin, D.; Ozkan, G.; Sanli, Y.; Isin, H.; et al. Do circulating long non-coding RNAs (lncRNAs) (LincRNA-p21, GAS 5, HOTAIR) predict the treatment response in patients with head and neck cancer treated with chemoradiotherapy? Tumor Biol. 2016, 37, 3969–3978. [Google Scholar] [CrossRef]
- Kresoja-Rakic, J.; Szpechcinski, A.; Kirschner, M.B.; Ronner, M.; Minatel, B.; Martinez, V.D.; Lam, W.L.; Weder, W.; Stahel, R.; Früh, M.; et al. MiR-625-3p and lncRNA GAS5 in liquid biopsies for predicting the outcome of malignant pleural mesothelioma patients treated with neo-adjuvant chemotherapy and surgery. Non-Coding RNA 2019, 5, 41. [Google Scholar] [CrossRef] [Green Version]
- Triozzi, P.L.; Achberger, S.; Aldrich, W.; Singh, A.D.; Grane, R.; Borden, E.C. The association of blood angioregulatory microRNA levels with circulating endothelial cells and angiogenic proteins in patients receiving dacarbazine and interferon. J. Transl. Med. 2012, 10, 241–248. [Google Scholar] [CrossRef] [Green Version]
- Hansen, T.F.; Carlsen, A.L.; Heegaard, N.H.H.; Sørensen, F.B.; Jakobsen, A. Changes in circulating microRNA-126 during treatment with chemotherapy and bevacizumab predicts treatment response in patients with metastatic colorectal cancer. Br. J. Cancer 2015, 112, 624–629. [Google Scholar] [CrossRef]
- Kou, C.H.; Zhou, T.; Han, X.L.; Zhuang, H.J.; Qian, H.X. Downregulation of mir-23b in plasma is associated with poor prognosis in patients with colorectal cancer. Oncol. Lett. 2016, 12, 4838–4844. [Google Scholar] [CrossRef] [Green Version]
- Zhuang, K.; Han, K.; Tang, H.; Yin, X.; Zhang, J.; Zhang, X.; Zhang, L. Up-regulation of plasma miR-23b is associated with poor prognosis of gastric cancer. Med. Sci. Monit. 2016, 22, 356–361. [Google Scholar] [CrossRef] [PubMed]




| KERRYPNX | Number of Patients | Low Copies/µL ≤ 305 | High Copies/µL > 305 | p-Value |
|---|---|---|---|---|
| Gender | 0.604 | |||
| Male | 21 | 11 | 10 | |
| Female | 4 | 3 | 1 | |
| Age # | 0.695 | |||
| ≤73 years | 13 | 6 | 7 | |
| >73 years | 12 | 7 | 5 | |
| Grading | 0.041 | |||
| G1–G2 | 14 | 5 | 10 | |
| G3 | 10 | 8 | 2 | |
| Hepatitis B infection | 0.593 | |||
| Yes | 4 | 3 | 1 | |
| No | 21 | 10 | 11 | |
| Hepatitis C infection | 0.695 | |||
| Yes | 12 | 7 | 5 | |
| No | 13 | 6 | 7 | |
| Cirrhosis | 0.238 | |||
| Yes | 12 | 8 | 4 | |
| No | 11 | 5 | 8 | |
| Recurrence after surgery | 1.000 | |||
| Yes | 17 | 9 | 8 | |
| No | 8 | 4 | 4 | |
| Tumor Size | 0.642 | |||
| >5 cm | 6 | 4 | 2 | |
| <5 cm | 14 | 7 | 7 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Manganelli, M.; Grossi, I.; Ferracin, M.; Guerriero, P.; Negrini, M.; Ghidini, M.; Senti, C.; Ratti, M.; Pizzo, C.; Passalacqua, R.; et al. Longitudinal Circulating Levels of miR-23b-3p, miR-126-3p and lncRNA GAS5 in HCC Patients Treated with Sorafenib. Biomedicines 2021, 9, 813. https://doi.org/10.3390/biomedicines9070813
Manganelli M, Grossi I, Ferracin M, Guerriero P, Negrini M, Ghidini M, Senti C, Ratti M, Pizzo C, Passalacqua R, et al. Longitudinal Circulating Levels of miR-23b-3p, miR-126-3p and lncRNA GAS5 in HCC Patients Treated with Sorafenib. Biomedicines. 2021; 9(7):813. https://doi.org/10.3390/biomedicines9070813
Chicago/Turabian StyleManganelli, Michele, Ilaria Grossi, Manuela Ferracin, Paola Guerriero, Massimo Negrini, Michele Ghidini, Chiara Senti, Margherita Ratti, Claudio Pizzo, Rodolfo Passalacqua, and et al. 2021. "Longitudinal Circulating Levels of miR-23b-3p, miR-126-3p and lncRNA GAS5 in HCC Patients Treated with Sorafenib" Biomedicines 9, no. 7: 813. https://doi.org/10.3390/biomedicines9070813