Efficacy of Pulmonary Rehabilitation in Post-COVID-19: A Systematic Review and Meta-Analysis
Abstract
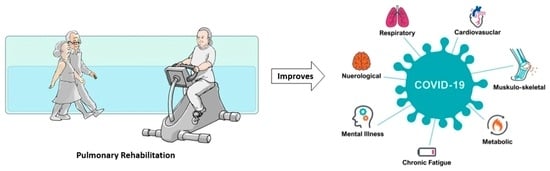
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility Criteria
2.3. Inclusion Procedure
2.4. Risk of Bias Assessment
2.5. Data Analysis
3. Results
3.1. Characteristics of the Included Studies
3.2. Intervention
3.3. Outcomes
3.4. Risk of Bias
3.5. Efficacy of Pulmonary Rehabilitation in COVID-19
3.6. Subgroup Analysis
3.7. Heterogeneity Analysis
3.8. Publication Bias
4. Discussion
4.1. Strengths and Limitations
4.2. Clinical Messages
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
Pubmed Search String
References
- Klaser, K.; Thompson, E.J.; Nguyen, L.H.; Sudre, C.H.; Antonelli, M.; Murray, B.; Canas, L.S.; Molteni, E.; Graham, M.S.; Kerfoot, E.; et al. Anxiety and depression symptoms after COVID-19 infection: Results from the COVID Symptom Study app. J. Neurol. Neurosurg. Psychiatry 2021, 92, 1254–1258. [Google Scholar] [CrossRef]
- Fiore, E.; Corbellini, C.; Acucella, L.; Gargano, S.; Sánchez Romero, E.A.; Cotella, D.; Villafañe, J.H. Dolor musculoesquelético en supervivientes del COVID-19 tras la hospitalización: Una breve revision (Musculoskeletal pain related to COVID-19 survivors after hospitalization: A short review). Retos 2022, 44, 789–795. [Google Scholar] [CrossRef]
- El-Maradny, Y.A.; Rubio-Casillas, A.; Uversky, V.N.; Redwan, E.M. Intrinsic factors behind long-COVID: I. Prevalence of the extracellular vesicles. J. Cell. Biochem. 2023, 124, 656–673. [Google Scholar] [CrossRef]
- Jimeno-Almazán, A.; Pallarés, J.G.; Buendía-Romero, Á.; Martínez-Cava, A.; Franco-López, F.; Martínez, B.J.S.-A.; Bernal-Morel, E.; Courel-Ibáñez, J. Post-COVID-19 Syndrome and the Potential Benefits of Exercise. Int. J. Environ. Res. Public Health 2021, 18, 5329. [Google Scholar] [CrossRef] [PubMed]
- Fernández-de-Las-Peñas, C.; Palacios-Ceña, D.; Gómez-Mayordomo, V.; Palacios-Ceña, M.; Rodríguez-Jiménez, J.; de-la-Llave-Rincón, A.I.; Velasco-Arribas, M.; Fuensalida-Novo, S.; Ambite-Quesada, S.; Guijarro, C.; et al. Fatigue and Dyspnoea as Main Persistent Post-COVID-19 Symptoms in Previously Hospitalized Patients: Related Functional Limitations and Disability. Respiration 2022, 101, 132–141. [Google Scholar] [CrossRef] [PubMed]
- Scurati, R.; Papini, N.; Giussani, P.; Alberti, G.; Tringali, C. The Challenge of Long COVID-19 Management: From Disease Molecular Hallmarks to the Proposal of Exercise as Therapy. Int. J. Mol. Sci. 2022, 23, 12311. [Google Scholar] [CrossRef]
- Cheng, S.W.M.; McKeough, Z.J.; McNamara, R.J.; Alison, J.A. Pulmonary Rehabilitation Using Minimal Equipment for People with Chronic Obstructive Pulmonary Disease: A Systematic Review and Meta-Analysis. Phys. Ther. 2023, 103, pzad013. [Google Scholar] [CrossRef]
- Sanchez-Ramirez, D.C.; Normand, K.; Zhaoyun, Y.; Torres-Castro, R. Long-Term Impact of COVID-19: A Systematic Review of the Literature and Meta-Analysis. Biomedicines 2021, 9, 900. [Google Scholar] [CrossRef]
- Corbellini, C.; Villafane, J.; Gugliotta, E.; Tavella, S.; Zampese, S.; Pessina, P.; Monti, R.; Carnuccio, C.; Romero, E.A.S.; Meroni, R. Late Breaking Abstract—Pulmonary Rehabilitation in Post—COVID Subjects with Moderate Lung Restriction, A Case Series. Eur. Respir. J. 2021, 58 (Suppl. 65), PA2003. [Google Scholar]
- Sánchez Romero, E.A.; Alonso Pérez, J.L.; Vinuesa Suárez, I.; Corbellini, C.; Villafañe, J.H. Spanish experience on the efficacy of airways clearance techniques in SARS-CoV-2 (COVID-19) at intensive care unit: An editorial and case report. SAGE Open Med. Case Rep. 2022, 10, 2050313X221112507. [Google Scholar] [CrossRef]
- Nicolás Cuenca-Zaldivar, J.; Acevedo, Á.M.; Fernández-Carnero, J.; Sánchez-Romero, E.A.; Villafañe, J.H.; Barragán Carballar, C. Effects of a Multicomponent Exercise Program on Improving Frailty in Post-COVID-19 Older Adults after Intensive Care Units:A Single-Group Retrospective Cohort Study. Biology 2022, 11, 1084. [Google Scholar] [CrossRef] [PubMed]
- Martínez Rolando, L.; Villafañe, J.H.; Cercadillo García, S.; Sanz Argüello, A.; Villanueva Rosa, M.; Sánchez Romero, E.A. Multicomponent Exercise Program to Improve the Immediate Sequelae of COVID-19: A Prospective Study with a Brief Report of 2-Year Follow-Up. Int. J. Environ. Res. Public Health 2022, 19, 12396. [Google Scholar] [CrossRef]
- Sánchez Romero, E.A.; Fernández Carnero, J.; Alonso Pérez, J.L.; Martínez Rolando, L.; Villafañe, J.H. Addressing post-COVID-19musculoskeletal symptoms through telemedicine: A study protocol. F1000Research 2022, 11, 898. [Google Scholar] [CrossRef]
- Ahmed, I.; Mustafaoglu, R.; Yeldan, I.; Yasaci, Z.; Erhan, B. Effect of Pulmonary Rehabilitation Approaches on Dyspnea, Exercise Capacity, Fatigue, Lung Functions, and Quality of Life in Patients with COVID-19: A Systematic Review and Meta-analysis. Arch. Phys. Med. Rehabil. 2022, 103, 2051–2062. [Google Scholar] [CrossRef]
- Reinert, G.; Müller, D.; Wagner, P.; Martínez-Pozas, O.; Cuenca-Záldivar, J.N.; Fernández-Carnero, J.; Sánchez Romero, E.A.; Corbellini, C. Pulmonary Rehabilitation in SARS-CoV-2: A Systematic Review and Meta-Analysis of Post-Acute Patients. Diagnostics 2022, 12, 3032. [Google Scholar] [CrossRef] [PubMed]
- Al-Mhanna, S.B.; Mohamed, M.; Noor, N.M.; Afolabi, H.A.; Irekeola, A.A.; Bello, K.E.; Aldhahi, M.I.; Ghazali, W.S.W. Effectiveness of Pulmonary Rehabilitation among COVID-19 Patients: A Systematic Review and Meta-Analysis. Healthcare 2022, 10, 2130. [Google Scholar] [CrossRef]
- Fugazzaro, S.; Contri, A.; Esseroukh, O.; Kaleci, S.; Croci, S.; Massari, M.; Facciolongo, N.C.; Besutti, G.; Iori, M.; Salvarani, C.; et al. Rehabilitation Interventions for Post-Acute COVID-19 Syndrome: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 5185. [Google Scholar] [CrossRef]
- Da Silva Vieira, A.G.; Pinto, A.C.P.N.; Garcia, B.M.S.P.; Eid, R.A.C.; Mól, C.G.; Nawa, R.K. Telerehabilitation improves physical function and reduces dyspnoea in people with COVID-19 and post-COVID-19 conditions: A systematic review. J. Physiother. 2022, 68, 90–98. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E.; et al. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017, 358, j4008. [Google Scholar] [CrossRef] [Green Version]
- Spruit, M.A. Pulmonary rehabilitation. Eur. Respir. Rev. 2014, 23, 55–63. [Google Scholar] [CrossRef]
- Barton, C.J.; Webster, K.E.; Menz, H.B. Evaluation of the scope and quality of systematic reviews on nonpharmacological conservative treatment for patellofemoral pain syndrome. J. Orthop. Sports Phys. Ther. 2008, 38, 529–541. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sterne, J.A.C.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Viechtbauer, W. Conducting meta-analyses in R with the metafor package. J. Stat. Softw. 2010, 36, 1–48. [Google Scholar] [CrossRef] [Green Version]
- Balduzzi, S.; Rücker, G.; Schwarzer, G. How to perform a meta-analysis with R: A practical tutorial. Evid Based Ment Health 2019, 22, 153–160. [Google Scholar] [CrossRef] [Green Version]
- Luo, D.; Wan, X.; Liu, J.; Tong, T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat. Methods Med Res. 2018, 27, 1785–1805. [Google Scholar] [CrossRef] [Green Version]
- Shi, J.; Luo, D.; Weng, H.; Zeng, X.; Lin, L.; Chu, H.; Tong, T. Optimally estimating the sample standard deviation from the five-number summary. Res. Synth. Methods 2020, 11, 641–654. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane handbook for systematic reviews of interventions. In Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons: Chichester, UK, 2019; pp. 1–694. [Google Scholar]
- Rosenthal, R. Meta-analytic procedures for social research. In Meta-Analytic Procedures for Social Research; SAGE Publications, Inc.: Thousand Oaks, CA, USA, 1991. [Google Scholar] [CrossRef]
- Berlim, M.T.; McGirr, A.; Dos Santos, N.R.; Tremblay, S.; Martins, R. Efficacy of theta burst stimulation (TBS) for major depression: An exploratory meta-analysis of randomized and sham-controlled trials. J. Psychiatr. Res. 2017, 90, 102–109. [Google Scholar] [CrossRef]
- Kallapiran, K.; Koo, S.; Kirubakaran, R.; Hancock, K. Review: Effectiveness of mindfulness in improving mental health symptoms of children and adolescents: A meta-analysis. Child Adolesc. Ment. Health 2015, 20, 182–194. [Google Scholar] [CrossRef]
- McGirr, A.; Berlim, M.T.; Bond, D.J.; Neufeld, N.H.; Chan, P.Y.; Yatham, L.N.; Lam, R.W. A systematic review and meta-analysis of randomized controlled trials of adjunctive ketamine in electroconvulsive therapy: Efficacy and tolerability. J. Psychiatr. Res. 2015, 62, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Yagiz, G.; Akaras, E.; Kubis, H.-P.; Owen, J.A. The Effects of Resistance Training on Architecture and Volume of the Upper Extremity Muscles: A Systematic Review of Randomised Controlled Trials and Meta-Analyses. Appl. Sci. 2022, 12, 1593. [Google Scholar] [CrossRef]
- Papadopoulos, V.P.; Apergis, N.; Filippou, D.K. Nocturia in CPAP-Treated Obstructive Sleep Apnea Patients: A Systematic Review and Meta-Analysis. SN Compr. Clin. Med. 2020, 2, 2799–2807. [Google Scholar] [CrossRef]
- Jimeno-Almazán, A.; Buendía-Romero, Á.; Martínez-Cava, A.; Franco-López, F.; Sánchez-Alcaraz, B.J.; Courel-Ibáñez, J.; Pallarés, J.G. Effects of a concurrent training, respiratory muscle exercise, and self-management recommendations on recovery from post-COVID-19 conditions: The RECOVE trial. J. Appl. Physiol. 2023, 134, 95–104. [Google Scholar] [CrossRef]
- Baujat, B.; Mahé, C.; Pignon, J.P.; Hill, C. A graphical method for exploring heterogeneity in meta-analyses: Application to a meta-analysis of 65 trials. Stat. Med. 2002, 21, 2641–2652. [Google Scholar] [CrossRef]
- Shi, L.; Lin, L.; Omboni, S. The trim-and-fill method for publication bias: Practical guidelines and recommendations based on a large database of meta-analyses. Medicine 2019, 98, e15987. [Google Scholar] [CrossRef] [PubMed]
- Abodonya, A.M.; Abdelbasset, W.K.; Awad, E.A.; Elalfy, I.E.; Salem, H.A.; Elsayed, S.H. Inspiratory muscle training for recovered COVID-19 patients after weaning from mechanical ventilation: A pilot control clinical study. Medicine 2021, 100, E25339. [Google Scholar] [CrossRef]
- Bargahi, M.; Soltani, S.; Rastgoo, N.; Aryanejad, F.; Nemati, R.; Ghaebi, M.; Bajelan, A.; Esmaielzade, S. Effect of Balloon-Blowing on Dyspnea and Oxygenation in Noncritical Adult Covid19 Patients: A Pilot Study. medRxiv 2021, preprint. [Google Scholar] [CrossRef]
- Fereydounnia, S.; Shadmehr, A.; Tahmasbi, M.A.; Salehi, M.R.S. The Comparison of the Effectiveness of Respiratory Physiotherapy Plus Myofascial Release Therapy Versus Respiratory Physiotherapy Alone on Cardiorespiratory Parameters in Patients With COVID-19. Int. J. Ther. Massage Bodywork Res. Educ. Pr. 2022, 15, 4–14. [Google Scholar] [CrossRef]
- Gonzalez-Gerez, J.J.; Saavedra-Hernandez, M.; Anarte-Lazo, E.; Bernal-Utrera, C.; Perez-Ale, M.; Rodriguez-Blanco, C. Short-Term Effects of a Respiratory Telerehabilitation Program in Confined COVID-19 Patients in the Acute Phase: A Pilot Study. Int. J. Environ. Res. Public Health 2021, 18, 7511. [Google Scholar] [CrossRef]
- Hayden, M.C.; Limbach, M.; Schuler, M.; Merkl, S.; Schwarzl, G.; Jakab, K.; Nowak, D.; Schultz, K. Effectiveness of a Three-Week Inpatient Pulmonary Rehabilitation Program for Patients after COVID-19: A Prospective Observational Study. Int. J. Environ. Res. Public Health 2021, 18, 9001. [Google Scholar] [CrossRef]
- Hockele, L.F.; Sachet Affonso, J.V.; Rossi, D.; Eibel, B. Pulmonary and Functional Rehabilitation Improves Functional Capacity, Pulmonary Function and Respiratory Muscle Strength in Post COVID-19 Patients: Pilot Clinical Trial. Int. J. Environ. Res. Public Health 2022, 19, 14899. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Xia, W.; Zhan, C.; Liu, S.; Yin, Z.; Wang, J.; Chong, Y.; Zheng, C.; Fang, X.; Cheng, W.; et al. A telerehabilitation programme in post-discharge COVID-19 patients (TERECO): A randomised controlled trial. Thorax 2022, 77, 697–706. [Google Scholar] [CrossRef] [PubMed]
- Liu, K.; Zhang, W.; Yang, Y.; Zhang, J.; Li, Y.; Chen, Y. Respiratory rehabilitation in elderly patients with COVID-19: A randomized controlled study. Complement. Ther. Clin. Pract. 2020, 39, 101166. [Google Scholar] [CrossRef]
- Llurda-Almuzara, L.; Rodríguez-Sanz, J.; López-De-Celis, C.; Aiguadé-Aiguadé, R.; Arán-Jové, R.; Labata-Lezaun, N.; Fernández-De-Las-Peñas, C.; Bosch, J.; Pérez-Bellmunt, A. Effects of Adding an Online Exercise Program on Physical Function in Individuals Hospitalized by COVID-19: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2022, 19, 16619. [Google Scholar] [CrossRef]
- Lobanov, A.A.; Grishechkina, I.A.; Andronov, S.V.; Barashkov, G.N.; Popov, A.I.; Fesyun, A.D.; Ivanova, E.P.; Maccarone, M.C.; Masiero, S. Can aquatic exercises contribute to the improvement of the gait stereotype function in patients with Long COVID outcomes? Eur. J. Transl. Myol. 2022, 32. [Google Scholar] [CrossRef]
- Martin, I.; Braem, F.; Baudet, L.; Poncin, W.; Fizaine, S.; Aboubakar, F.; Froidure, A.; Pilette, C.; Liistro, G.; De Greef, J.; et al. Follow-up of functional exercise capacity in patients with COVID-19: It is improved by telerehabilitation. Respir. Med. 2021, 183, 106438. [Google Scholar] [CrossRef]
- Nagy, E.N.; Elimy, D.A.; Ali, A.Y.; Ezzelregal, H.G.; Elsayed, M.M. Influence of Manual Diaphragm Release Technique Combined with Inspiratory Muscle Training on Selected Persistent Symptoms in Men with Post-Covid-19 Syndrome: A Randomized Controlled Trial. J. Rehabil. Med. 2022, 54, jrm00330. [Google Scholar] [CrossRef] [PubMed]
- Nambi, G.; Abdelbasset, W.K.; Alrawaili, S.M.; Elsayed, S.H.; Verma, A.; Vellaiyan, A.; Eid, M.M.; Aldhafian, O.R.; Nwihadh, N.B.; Saleh, A.K. Comparative effectiveness study of low versus high-intensity aerobic training with resistance training in community-dwelling older men with post-COVID 19 sarcopenia: A randomized controlled trial. Clin. Rehabil. 2022, 36, 59–68. [Google Scholar] [CrossRef]
- Pehlivan, E.; Palalı, İ.; Atan, S.G.; Turan, D.; Çınarka, H.; Çetinkaya, E. The effectiveness of POST-DISCHARGE telerehabilitation practices in COVID-19 patients: Tele-COVID study-randomized controlled trial. Ann. Thorac. Med. 2022, 17, 110–117. [Google Scholar] [CrossRef]
- Puchner, B.; Sahanic, S.; Kirchmair, R.; Pizzini, A.; Sonnweber, B.; Wöll, E.; Mühlbacher, A.; Garimorth, K.; Dareb, B.; Ehling, R.; et al. Beneficial effects of multi-disciplinary rehabilitation in postacute COVID-19: An observational cohort study. Eur. J. Phys. Rehabilitation Med. 2021, 57, 189–198. [Google Scholar] [CrossRef]
- Rodriguez-Blanco, C.; Gonzalez-Gerez, J.J.; Bernal-Utrera, C.; Anarte-Lazo, E.; Perez-Ale, M.; Saavedra-Hernandez, M. Short-Term Effects of a Conditioning Telerehabilitation Program in Confined Patients Affected by COVID-19 in the Acute Phase. A Pilot Randomized Controlled Trial. Medicina 2021, 57, 684. [Google Scholar] [CrossRef]
- Rutkowski, S.; Bogacz, K.; Rutkowska, A.; Szczegielniak, J.; Casaburi, R. Inpatient post-COVID-19 rehabilitation program featuring virtual reality—Preliminary results of randomized controlled trial. Front. Public Health 2023, 11, 1121554. [Google Scholar] [CrossRef] [PubMed]
- Do Amaral, V.T.; Viana, A.A.; Heubel, A.D.; Linares, S.N.; Martinelli, B.; Witzler, P.H.C.; de Souza Zanini, G.; Mendes, R.G.; Ciolac, E.G. Published ahead of Print Cardiovascular, Respiratory, and Functional Effects of Home-based Exercise Training after COVID-19 Hospitalization. Med. Sci. Sports Exerc. 2022, 54, 1795–1803. [Google Scholar] [CrossRef] [PubMed]
- Albu, S.; Zozaya, N.R.; Murillo, N.; García-Molina, A.; Chacón, C.A.F.; Kumru, H. Multidisciplinary outpatient rehabilitation of physical and neurological sequelae and persistent symptoms of covid-19: A prospective, observational cohort study. Disabil. Rehabil. 2021, 44, 6833–6840. [Google Scholar] [CrossRef]
- Cahalan, R.M.; Meade, C.; Mockler, S. SingStrong-A singing and breathing retraining intervention for respiratory and other common symptoms of long COVID: A pilot study. Can. J. Respir. Ther. 2022, 58, 20–27. [Google Scholar] [CrossRef]
- Calvo-Paniagua, J.; Díaz-Arribas, M.J.; Valera-Calero, J.A.; Gallardo-Vidal, M.I.; Fernández-De-Las-Peñas, C.; López-De-Uralde-Villanueva, I.; del Corral, T.; Plaza-Manzano, G. A tele-health primary care rehabilitation program improves self-perceived exertion in COVID-19 survivors experiencing Post-COVID fatigue and dyspnea: A quasi-experimental study. PLoS ONE 2022, 17, e0271802. [Google Scholar] [CrossRef]
- Compagno, S.; Palermi, S.; Pescatore, V.; Brugin, E.; Sarto, M.; Marin, R.; Calzavara, V.; Nizzetto, M.; Scevola, M.; Aloi, A.; et al. Physical and psychological reconditioning in long COVID syndrome: Results of an out-of-hospital exercise and psychological-based rehabilitation program. IJC Heart Vasc. 2022, 41, 101080. [Google Scholar] [CrossRef]
- Daynes, E.; Gerlis, C.; Chaplin, E.; Gardiner, N.; Singh, S.J. Early experiences of rehabilitation for individuals post-COVID to improve fatigue, breathlessness exercise capacity and cognition—A cohort study. Chronic Respir. Dis. 2021, 18. [Google Scholar] [CrossRef]
- Del Corral, T.; Fabero-Garrido, R.; Plaza-Manzano, G.; Fernández-de-Las-Peñas, C.; Navarro-Santana, M.; López-de-Uralde-Villanueva, I. Home-based respiratory muscle training on quality of life and exercise tolerance in long-term post-COVID-19: Randomized controlled trial. Ann. Phys. Rehabil. Med. 2022, 66, 101709. [Google Scholar] [CrossRef] [PubMed]
- Estebanez-Pérez, M.J.; Pastora-Bernal, J.M.; Martín-Valero, R. The Effectiveness of a Four-Week Digital Physiotherapy Intervention to Improve Functional Capacity and Adherence to Intervention in Patients with Long COVID-19. Int. J. Environ. Res. Public Health 2022, 19, 9566. [Google Scholar] [CrossRef]
- Groenveld, T.; Achttien, R.; Smits, M.; de Vries, M.; van Heerde, R.; Staal, B.; van Goor, H. COVID Rehab Group Feasibility of Virtual Reality Exercises at Home for Post–COVID-19 Condition: Cohort Study. JMIR Rehabilitation Assist. Technol. 2022, 9, e36836. [Google Scholar] [CrossRef]
- Hasenoehrl, T.; Palma, S.; Huber, D.F.-X.; Kastl, S.; Steiner, M.; Jordakieva, G.; Crevenna, R. Post-COVID: Effects of physical exercise on functional status and work ability in health care personnel. Disabil. Rehabil. 2022. [Google Scholar] [CrossRef] [PubMed]
- Jimeno-Almazán, A.; Franco-López, F.; Buendía-Romero, Á.; Martínez-Cava, A.; Sánchez-Agar, J.A.; Martínez, B.J.S.; Courel-Ibáñez, J.; Pallarés, J.G. Rehabilitation for post-COVID-19 condition through a supervised exercise intervention: A randomized controlled trial. Scand. J. Med. Sci. Sports 2022, 32, 1791–1801. [Google Scholar] [CrossRef] [PubMed]
- Lloyd-Evans, P.H.I.; Baldwin, M.M.; Daynes, E.; Hong, A.; Mills, G.; Goddard, A.C.N.; Chaplin, E.; Gardiner, N.; Singh, S.J. Early experiences of the Your COVID Recovery® digital programme for individuals with long COVID. BMJ Open Respir. Res. 2022, 9, e001237. [Google Scholar] [CrossRef]
- McNarry, M.A.; Berg, R.M.; Shelley, J.; Hudson, J.; Saynor, Z.L.; Duckers, J.; Lewis, K.; Davies, G.A.; Mackintosh, K.A. Inspiratory muscle training enhances recovery post-COVID-19: A randomised controlled trial. Eur. Respir. J. 2022, 60, 2103101. [Google Scholar] [CrossRef]
- Nopp, S.; Moik, F.; Klok, F.A.; Gattinger, D.; Petrovic, M.; Vonbank, K.; Koczulla, A.R.; Ay, C.; Zwick, R.H. Outpatient Pulmonary Rehabilitation in Patients with Long COVID Improves Exercise Capacity, Functional Status, Dyspnea, Fatigue, and Quality of Life. Respiration 2022, 101, 593–601. [Google Scholar] [CrossRef] [PubMed]
- Okan, F.; Okan, S.; Duran Yücesoy, F. Evaluating the Efficiency of Breathing Exercises via Telemedicine in Post-Covid-19 Patients: Randomized Controlled Study. Clin. Nurs. Res. 2022, 31, 771–781. [Google Scholar] [CrossRef]
- Philip, K.E.J.; Owles, H.; McVey, S.; Pagnuco, T.; Bruce, K.; Brunjes, H.; Banya, W.; Mollica, J.; Lound, A.; Zumpe, S.; et al. An online breathing and wellbeing programme (ENO Breathe) for people with persistent symptoms following COVID-19: A parallel-group, single-blind, randomised controlled trial. Lancet Respir. Med. 2022, 10, 851–862. [Google Scholar] [CrossRef]
- Chen, H.; Shi, H.; Liu, X.; Sun, T.; Wu, J.; Liu, Z. Effect of Pulmonary Rehabilitation for Patients with Post-COVID-19: A Systematic Review and Meta-Analysis. Front. Med. 2022, 9, 837420. [Google Scholar] [CrossRef]
- Rahmati, M.; Shamsi, M.M.; Woo, W.; Koyanagi, A.; Lee, S.W.; Yon, D.K.; Shin, J.I.; Smith, L. Effects of physical rehabilitation interventions in COVID-19 patients following discharge from hospital: A systematic review. J. Integr. Med. 2023, 21, 149–158. [Google Scholar] [CrossRef] [PubMed]
- Cosco, T.D.; Doyle, F.; Ward, M.; McGee, H. Latent structure of the Hospital Anxiety and Depression Scale: A 10-year systematic review. J. Psychosom. Res. 2012, 72, 180–184. [Google Scholar] [CrossRef] [PubMed]
- Coyne, J.C.; van Sonderen, E. No further research needed: Abandoning the Hospital and Anxiety Depression Scale (HADS). J. Psychosom. Res. 2012, 72, 173–174. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Menges, D.; Ballouz, T.; Anagnostopoulos, A.; Aschmann, H.E.; Domenghino, A.; Fehr, J.S.; Puhan, M.A. Burden of post-COVID-19 syndrome and implications for healthcare service planning: A population-based cohort study. PLoS ONE 2021, 16, e0254523. [Google Scholar] [CrossRef] [PubMed]
- Premraj, L.; Kannapadi, N.V.; Briggs, J.; Seal, S.M.; Battaglini, D.; Fanning, J.; Suen, J.; Robba, C.; Fraser, J.; Cho, S.-M. Mid and long-term neurological and neuropsychiatric manifestations of post-COVID-19 syndrome: A meta-analysis. J. Neurol. Sci. 2022, 434, 120162. [Google Scholar] [CrossRef]
- Johnston, S.A.; Roskowski, C.; He, Z.; Kong, L.; Chen, W. Effects of team sports on anxiety, depression, perceived stress, and sleep quality in college students. J. Am. Coll. Health 2020, 69, 791–797. [Google Scholar] [CrossRef]
- Petruzzello, S.J.; Landers, D.M.; Hatfield, B.D.; Kubitz, K.A.; Salazar, W. A Meta-Analysis on the Anxiety-Reducing Effects of Acute and Chronic Exercise: Outcomes and Mechanisms. Sports Med. 1991, 11, 143–182. [Google Scholar] [CrossRef]
- Dale, L.P.; Vanderloo, L.; Moore, S.; Faulkner, G. Physical activity and depression, anxiety, and self-esteem in children and youth: An umbrella systematic review. Ment. Health Phys. Act. 2019, 16, 66–79. [Google Scholar] [CrossRef]
- Wolf, S.; Seiffer, B.; Zeibig, J.-M.; Welkerling, J.; Brokmeier, L.; Atrott, B.; Ehring, T.; Schuch, F.B. Is Physical Activity Associated with Less Depression and Anxiety During the COVID-19 Pandemic? A Rapid Systematic Review. Sports Med. 2021, 51, 1771–1783. [Google Scholar] [CrossRef]
- Cénat, J.M.; Blais-Rochette, C.; Kokou-Kpolou, C.K.; Noorishad, P.-G.; Mukunzi, J.N.; McIntee, S.-E.; Dalexis, R.D.; Goulet, M.-A.; Labelle, P.R. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Res. 2021, 295, 113599. [Google Scholar] [CrossRef]
- Liu, Z.; Qiao, D.; Xu, Y.; Zhao, W.; Yang, Y.; Wen, D.; Li, X.; Nie, X.; Dong, Y.; Tang, S.; et al. The Efficacy of Computerized Cognitive Behavioral Therapy for Depressive and Anxiety Symptoms in Patients with COVID-19: Randomized Controlled Trial. J. Med. Internet Res. 2021, 23, e26883. [Google Scholar] [CrossRef] [PubMed]
- Pedersini, P.; Corbellini, C.; Villafañe, J.H. Italian Physical Therapists’ Response to the Novel COVID-19 Emergency. Phys. Ther. 2020, 100, 1049–1051. [Google Scholar] [CrossRef] [PubMed]





| Author (Year) | Study Design | Population | Sample Size | Intervention | Control Group | Outcomes | Results |
|---|---|---|---|---|---|---|---|
| Studies with Subacute COVID-19 Patients | |||||||
| Abodonya et al. (2021) [39] | RCT | Adults with subacute COVID-19 | n = 42 Int: n = 21 (19% F), Age: 48.3 ± 8.5 Con: n = 21 (23.8% F) Age: 47.8 ± 9.2 | Duration 2 weeks. Intervention Breathing exercises. | Usual care | Dyspnea (DS-12) Quality of life (EQ-5D) Physical function (6MWT) | Intra-group analysis found statistically differences in intervention group in dyspnea (p = 0.001), quality of life (p < 0.001) and 6MWT (p < 0.001). Between group comparison, intervention group reported statistically significant differences compared to control in all outcomes with medium-large size effects. |
| Barhagi et al. (2021) [40] | RCT | Adults with subacute COVID-19 | n = 80 (38.75% F) Int: n = 40, Age: 57.1 ± 18.7 Con: n = 40 Age: 58 ± 17.13 | Duration Three days. Intervention Breathing exercises. | Usual care | Dyspnea (MBS) | After end of treatment, intervention group improved dyspnea with statistically differences compared to usual care (p = 0.007). |
| Fereydounnia et al. (2022) [41] | RCT | Adults with subacute COVID-19 | n = 50 (42% F) Int: n = 25, Age: 49.44 ± 14.78 Con: n = 25, Age: 45 ± 12.75 | Duration 1 week. Intervention Myofascial release and breathing exercises. | Breathing exercises | Dyspnea (MBS) Physical function (6MWT) Fatigue (Borg) | Intervention group improved dyspnea with statistically differences at the end of the treatment compared to control (p < 0.01). No statistically differences were found in terms of physical function (p = 0.033) or fatigue (p = 0.034) improvement compared to control. |
| González-Gerez et al. (2021) [42] | RCT | Adults with subacute COVID-19 | n = 38 Int: n = 19 (47.4% F), Age: 40.79 ± 9.84 Con: n = 19 (42.1% F), Age: 40.32 ± 12.53 | Duration 1 week. Intervention Breathing exercises. Telerehabilitation. | Usual care | Physical function (6MWT; 30STS) Dyspnea (MD12; BS) | Statistically differences were found in terms of improving dyspnea (p < 0.001) and physical function (p = 0.001), in intervention, with no differences in control group. Between group analysis found statistically differences favoring intervention compared to control improving dyspnea (p < 0.001) and physical function (p = 0.001). |
| Hayden et al. (2021) [43] | Observational | Adults with subacute COVID-19 | n = 108 (45.4% F) Age: 55.6 ± 10.1 | Duration 3 weeks. Intervention Aerobic and strength training. Nutritional, psychological, and physical therapy support were included. | No control | Dyspnea (NRS/mMRC) Physical function (6MWT) Quality of life (EQ-5D) Fatigue (BFI) Depression and Anxiety (PHQ-9, GAD-7) | Dyspnea improved at rest (p < 0.001) and on exertion (p < 0.001) after treatment. Physical function improved after treatment (p < 0.001). Quality of life, fatigue, anxiety, and depression improved after treatment (p < 0.001) |
| Hockele et al. (2022) [44] | Observational | Adults with subacute COVID-19 | n = 29 (51.7% F) Age: 54.4 ± 14.6 | Duration 6–8 weeks. Intervention Aerobic and strength training. | No control | Physical function (6MWT, TUG) Dyspnea (mMRC) | Physical function improved after treatment with statistically significant differences compared to baseline in 6MWT (p < 0.001) and TUG (p = 0.023). Dyspnea improved after treatment with differences compared to baseline (p = 0.003). |
| Li et al. (2021) [45] | RCT | Adults with subacute COVID-19 | n = 119 (55.46% F) Int: n = 59, Age: 49.17 ± 10.75 Con: n = 60, Age: 52.03 ± 11.10 | Duration 6 weeks. 6 months follow-up. Intervention Aerobic, strength and breathing exercises. Telerehabilitation. | Usual care | Physical function (6 MWT) Dyspnea (mMRC) Quality of life (SF-12) | Intervention group improved physical function after treatment (p < 0.001) and at follow-up with statistically differences (p < 0.001). Perceived dyspnea improved after treatment with differences compared to control (p = 0.001) but without differences at follow-up (p = 0.162). Physical component of SF-12 improved with differences after treatment (p = 0.004) and at follow-up (p = 0.045). However, mental component found no differences at any point (p = 0.116; p = 0.164). |
| Liu et al. (2020) [46] | RCT | Adults with subacute COVID-19 | n = 72 Int: n = 36 (33.3% F), Age: 69.4 ± 8 Con: n = 36 (30.6% F) Age: 68.9 ± 7.6 | Duration 6 weeks. Intervention Breathing exercises. | Usual care | Physical function (6MWT) Quality of life (SF-36) Anxiety and Depression (SDS, SAS) | Physical function improved with statistically differences in intervention group compared with baseline (p < 0.05), without statistically improvements in control group. Intervention group improved with statistically differences compared to control group (p < 0.05). Quality of life improved with statistically differences compared to baseline in intervention group (p < 0.05) and not on control group. Between group analysis found that intervention group improved with statistically differences in all items of SF-36 compared to control group (p < 0.05). Anxiety improved with statistically significant differences between groups favoring intervention (p < 0.05), but not depression. |
| Llurda-Almuzara et al. (2022) [47] | RCT | Adults with subacute COVID-19 | n = 70 Int: n = 35, Age: 49.5 ± 13.7 Con: n = 35 Age: 55.1 ± 20.9 | Duration 8 weeks. Intervention Aerobic, strength and breathing exercises. Telerehabilitation. | Usual care | Physical function (SPPB, 4MWT) | Physical function improved with moderate significant effects in intervention group compared to control. |
| Lobanov et al. (2022) [48] | RCT | Adults with subacute COVID-19 | n = 23 Int: n = 14 Con: n= 9 | Duration 2 weeks. Intervention Aerobic exercises in pool. | Exercise without pool. | Physical function (6MWT) Quality of life (EQ-5D) Dyspnea (BS) | Physical function improved with statistically significant differences compared to baseline (p = 0.047 both groups), with greater improvement in intervention group. Quality of life improved in anxiety/depression domain with statistically differences in control group (p = 0.043), but not in intervention group (p = 0.69). Dyspnea improved after treatment, but without statistical differences compared to baseline in any group. |
| Martín et al. (2021) [49] | Observational | Adults with subacute COVID-19 | n = 27 Int: n = 14 (21.4% F), Age: 60.8 ± 10.4 Con: n = 13 (53.8% F), Age: 61.9 ± 10.7 | Duration 6 weeks. Intervention Aerobic and strength exercises. | Usual Care | Physical function (1MSTST) Dyspnea (BS) | After treatment, statistically differences were found in 1min-STS favoring intervention group (p = 0.004). No differences were found in terms of dyspnea improvement (p = 0.560). |
| Nagy et al. (2022) [50] | RCT | Adults with subacute COVID-19 | n = 52 Int: n = 26, Age: 40 ± 3.36 Con: n = 26, Age: 39.7 ± 3.55 | Duration 6 weeks. Intervention Myofascial release and breathing exercises. | Breathing exercises | Dyspnea (mMRC) Physical function (6MWT) Fatigue (FSS) | Dyspnea, physical function, and fatigue improved with statistical differences compared to baseline in both groups (p < 0.05). Additionally, intervention group resulted in statistically significant differences compared to control (p < 0.001). |
| Nambi et al. (2022) [51] | RCT | Adults with subacute COVID-19 | n = 76 Int: n = 38, Age: 63.2 ± 3.1 Con: n = 38 Age: 64.1 ± 3.2 | Duration 8 weeks. Intervention Exercise at low intensity | Exercise at high intensity | Quality of life (SarQol) | Both groups improved quality of life after treatment with statistical differences compared to baseline (p = 0.001). However, patients allocated to low intensity group improved with better results in SarQol compared to baseline than those allocated to high intensity training. |
| Pehlivan et al. (2022) [52] | RCT | Adults with subacute COVID-19 | n = 34 Int: n = 17 (18% F), Age: 50.76 (32–82) Con: n = 17 (35% F), Age: 43.24 (23–71) | Duration 6 weeks. Intervention Aerobic, strength and breathing exercises. Telerehabilitation. | Usual care | Physical function (TUG/SPPB) Dyspnea (mMRC) Fatigue (VAS) Quality of life (SGRQ) Depression (BDI) | Although both groups improved outcomes, intra-group differences were only found mMRC (p = 0.035), TUG (p = 0.005) and SGRQ (p = 0.002) at intervention group, while not statistically differences were found in control group at the end of treatment. Between-groups analysis revealed statistically significant differences in terms of SGRQ improvement favor to intervention (p = 0.042). No significant changes were found after treatment in depression levels neither intra-group or between group comparison. |
| Puchner et al. (2021) [53] | Observational | Adults with subacute COVID-19 | n = 23 (30% F) Age: 57 ± 10 | Duration 3–4 weeks. Intervention Aerobic, strength and breathing exercises. Nutritional and psychological counseling. | No control | Physical function (6MWT) | Physical function improved after treatment with statistically differences compared to baseline (p < 0.001). |
| Rodríguez-Blanco et al. (2021) [54] | RCT | Adults with subacute COVID-19 | n = 36 Int: n = 18 (50% F), Age: 39.39 ± 11.74 Con: n = 18 (55.5% F), Age: 41.33 ± 12.13 | Duration 1 week. Intervention Strength exercises. Telerehabilitation. | Usual care | Physical function (6MWT/30STS) Dyspnea (BS) | Intervention group improved physical function after treatment with statistically differences compared to usual care (p < 0.001). However, although dyspnea improved in intervention group and did not improve in control group after treatment, differences were not significant (p = 0.074). |
| Rutkowski et al. (2022) [55] | RCT | Adults with subacute COVID-19 | n = 32 (68% F) Age: 57.8 ± 4.9 | Duration 3 weeks. Intervention Virtual reality exercise | Exercise without virtual reality | Depression and Anxiety (HADS) Quality of life (WHOQOL-BREF) Physical function (6MWT) | Intervention group (p < 0.001) and control group (p < 0.05) improved anxiety and depression after treatment compared to baseline levels. No significant changes were found in any group in terms of quality-of-life improvement after treatment. Physical function improved in both groups. However, patients in intervention group showed more improvements in walked distance after treatment than control group. |
| Teixeira do Amaral et al. (2022) [56] | RCT | Adults with subacute COVID-19 | n = 32 Int: n = 12, Age: 51.9 ± 10.2 Con: n = 20, Age: 53.3 ± 11.6 | Duration 12 weeks. Intervention Aerobic and strength exercises. Telerehabilitation. | Usual care | Physical function (6MWT, TUG, 5TSTS) | Both groups all physical function outcomes compared to baseline, but without statistically significant differences within-group or between groups. |
| Studies with long COVID-19 patients | |||||||
| Albu et al., 2022 [57] | Observational | Adults with long COVID-19 | n = 40 (40% female) Mean Age: 52 ± 11.4 y/o | Duration 8 weeks Intervention Education Aerobic, strength and breathing exercises. Psychological counseling. Intensity Personalized according to patient status. | No control | Physical performance (SPPB) Fatigue (MFIS) Quality of life (WHOQOL-BREF) | After 8 weeks of rehabilitation, significant improvements in physical performance were found in SPPB compared to baseline with statistically differences (p = 0.001). Fatigue was improved after intervention with statistically differences for all measured domains (p = 0.001). Quality of life improved in physical, psychological, and environmental domains with statistical differences (p = 0.001), but not at social domain (p = 0.15). |
| Cahalan et al., 2022 [58] | Observational | Adults with long COVID-19 | n = 27 (85% f) Mean age: 48.4 ± 10.1 y/o | Duration 10 weeks. Intervention Breathing exercises, psychological advice. Telerehabilitation. Intensity Not reported. | None | Dyspnea (C19YRS) Fatigue (C19YRS) Anxiety/Depression (C19YRS) | Statistical improvements were found after treatment in terms of dyspnea (p < 0.001), as well as in fatigue (p = 0.03). Although anxiety and depression improved after treatment, no significant differences were found (p = 0.08 for anxiety, p = 0.337 for depression). |
| Calvo-Paniagua 2022 [59] | Quasi-experimental | Adults with long COVID-19 | n = 68 (61.8% f) Mean age: 48.5 ± 9.7 y/o | Duration 7 weeks. Intervention Aerobic, strength and breathing exercises. Telerehabilitation. Intensity Not reported. | None | Dyspnea (mMRC) Quality of life (SGRQ) Physical performance (6MWT) | Dyspnea improved significantly after intervention and at follow-up (p < 0.001). Quality of life improved significantly after intervention and at follow-up (p < 0.001). Physical performance improved with statistically differences after intervention and at follow-up (p < 0.001). |
| Compagno et al., 2022 [60] | Observational | Adults with long COVID-19 | n = 30 (40% female) Mean Age: 58.37 ± 11.6 y/o | Duration 8–20 weeks Intervention Aerobic and strength exercises. Psychological counseling. Intensity Aerobic exercise at low and mid intensity. Strength at 30–50% 1RM. | No control | Quality of life (SF-36) Anxiety (SAS) Depression (SDS) | Quality of life improved after intervention with statistically differences (p < 0.05). Anxiety and depression improved with statistically differences after treatment (both p < 0.05). |
| Daynes et al., 2021 [61] | Observational | Adults with long COVID-19 | n = 30 (48% female) Mean Age: 58 ± 16 y/o | Duration 6 weeks, with two supervised sessions per week. Intervention Aerobic and strength exercises. Intensity Not reported. | No control | Physical performance (ISWT) Fatigue (FACIT) Anxiety and depression (HADS) Quality of life (EQ-5D) | ISWT improved after treatment with statistically differences compared to baseline (p < 0.01). Fatigue improved with statistical differences at the end of treatment (p < 0.01), while anxiety and depression improved, but without statistically significant differences (p = 0.5 for anxiety and p = 0.1 for depression). Quality of life improved after treatment compared to baseline (p = 0.05). |
| Del Corral 2022 [62] | RCT | Adults with long COVID-19 | G1: n = 22, mean age: 48.9 ± 8.3 y/o; 77% f G2: n = 22, mean age: 45.3 ± 12.8 y/o; 73% f G3: n = 22, mean age: 46.5 ± 9.6 y/o, 64% f G4: n = 22, mean age: 45 ± 10.2 y/o, 73% f | Duration 8 weeks. Intervention Group 1: Inspiratory breathing exercises. Group 2: Inspiratory and expiratory breathing exercises. Telerehabilitation. Intensity 20–80% of maximal inspiratory pressure | Group 3: Sham inspiratory exercises. Group 4: Sham inspiratory and expiratory exercises. Sham procedures were with device without resistance | Quality of life (EQ-5D) Physical performance (1MSTST) Anxiety/Depression (HADS) | All groups improved quality of life after intervention compared to baseline (p < 0.05), except group 4. At 4 weeks follow-up, no statistical differences were found between groups improving quality of life. Physical performance improved with large effects in intervention groups compared with sham groups after intervention (p < 0.01), but without differences when comparing both intervention groups. Differences were not found between groups after 4 weeks follow-up in terms of physical performance improving. Although all groups improved psychological status, no statistical differences were found across groups. |
| Estébanez-Pérez 2022 [63] | Quasi-Experimental | Adults with long COVID-19 | n = 32 (71.9% f) Mean age: 45.93 ± 10.65 y/o | Duration 4 weeks. Intervention Aerobic and strength training. Telerehabilitation. Intensity Aerobic exercises at low to moderate intensity. Strength training not reported. | None | Physical performance (SPPB, 1MSTST) | 1mSTS and SPPB improved with statistically significant effects after treatment (p < 0.05). |
| Groenveld 2022 [64] | Observational | Adults with long COVID-19 | n = 47 (68% f) Mean age: 54 (21–70) | Duration 6 weeks Intervention Virtual reality-based exercise. Telerehabilitation. Intensity Adjusted to patient. | None | Fatigue (BS) Physical performance (6MWT, TUG, 30CST) Quality of life (SF-12, PHQ) Anxiety/Depression (HADS) | Fatigue improved with clinical differences after treatment (p = 0.03). Significant differences were found in 6MWT (p < 0.001) and 30CST (p = 0.02) after intervention. Three patients performed TUG instead of 6MWT, with improvements after treatment. Statistical differences were found improving quality of life for physical sphere (p < 0.049) and mental sphere (p < 0.01) measured with SF-12, as well as with PHQ (p = 0.04) Symptoms measured with HADS decreased, but without statistical differences (p = 0.08). |
| Hasenoehrl et al., 2022 [65] | Quasi-experimental | Adults with long COVID-19 | Group 1 (mild symptoms): n = 10 (60% female), mean age: 42.9 ± 12.4 y/o Group 2 (severe symptoms): n = 18 (89% female), mean age: 47.4 ± 10.1 y/o | Duration 8 weeks of supervised strength training, 2 times per week Intervention Aerobic and strength exercises. Intensity Strength exercises performed at 7–10 RPE. Aerobic exercises at moderate intensity. | No control | Physical performance (6 MWT/30 STST) | Both groups improved significantly 30 STST (p < 0.001) and 6 MWT (p < 0.001) after intervention. |
| Jimeno-Almanzán et al., 2022 [36] | RCT | Adults with long COVID-19 | n = 80 (69% female) Mean Age: 45.3 ± 8.0 y/o | Duration 8 weeks. Intervention G1: Strength and breathing exercises. G2: Strength exercises. G3: Breathing exercises. Intensity Strength at 50% 1 RM. Breathing exercises at 12–15 RPE. | G4: Usual care | Dyspnea (mMRC) Quality of life (SF-12) Anxiety and Depression (GAD-7/PHQ-9) Fatigue (FSS) | All outcomes improved in all study groups after intervention. After 8 weeks of intervention, no differences between groups were detected in mMRC, GAD-7 and SF-12. Fatigue and depression improved with differences in training groups (G1 and G2, p = 0.007). Breathing training group (G3) improved with differences in physical domain of SF-12 (p < 0.05). No relevant changes were observed in control group (G4) pre-post intervention. |
| Jimeno-Almanzán et al., 2022a [66] | RCT | Adults with long COVID-19 | n = 39 (74.4% female) Mean Age: 45.2 ± 9.5 y/o | Duration 8 weeks. Intervention Strength exercises. Intensity 50% 1RM. | Usual care | Dyspnea (mMRC) Quality of life (SF-12) Anxiety and Depression (GAD-7/PHQ-9) Fatigue (FSS) Physical performance (5TSTST) | Intervention group resulted in statistically differences compared to control in physical domain of SF-12 (p = 0.024), fatigue (p < 0.05), depression symptoms (p = 0.021), and physical performance (p = 0.009). Although all studied outcomes improved in both groups, no statistical differences were found in other outcomes such as dyspnea improvement or anxiety. |
| Lloyd-Evans 2022 [67] | Observational | Adults with long COVID-19 | n = 110 (68.1% f) Mean age: 46.3 ± 10.8 | Duration 8–12 weeks Intervention Aerobic and strength exercises. Telerehabilitation. Intensity Not reported. | None | Quality of life (EQ-5D) | Statistically significant differences were found improving quality of life (p < 0.01). |
| McNarry 2022 [68] | RCT | Adults with long COVID-19 | n = 148 (111 int, 86% f/37 con, 95% f) Mean age: 46.76 ± 12.03 (int)/46.13 ± 12.73 (con) | Duration 8 weeks, unsupervised. Intervention Breathing exercises. Telerehabilitation. Intensity 80% of sustained maximal inspiratory pressure. | Usual care | Quality of life (K-BILD) Dyspnea (TDI) | Although quality of life improved within-group, no statistically significant differences were found between groups. Dyspnea improved with statistical differences favoring intervention compared to control (p = 0.005). |
| Nopp et al., 2022 [69] | Observational | Adults with long COVID-19 | n = 58 (43.1% female) Mean Age: 46.8 ± 12.6 y/o | Duration 6 weeks. Intervention Aerobic, strength and breathing exercises. Intensity Not reported. | No Control | Physical performance (6 MWT/1 MSTST) Dyspnea (mMRC) Quality of life (EQ-5D) Fatigue (FAS) | After intervention, patients improved 6 MWT and 1 MSTST with statistical differences (p < 0.001). Dyspnea improved with statistical differences compared to baseline (p < 0.001). Quality of life improved after treatment (p < 0.001). Fatigue improved after treatment with statistical differences (p < 0.001). |
| Okan 2022 [70] | RCT | Adults with long COVID-19 | n = 52 (26 int, 42.3% f/26 con, 53.8% f) Mean age: 48.85 ± 10.85 (int)/52.19 ± 14.84 (con) | Duration 5 weeks, one session supervised. Intervention Aerobic and breathing exercises. Telerehabilitation. Intensity Aerobic exercises at moderate intensity. Breathing not reported. | Usual care | Dyspnea (mMRC) Physical performance (6 MWT) Quality of life (SGRQ) | Both groups improved dyspnea. However, it was significantly lower in intervention group than in control group (p < 0.001). Quality of life improved with statistical differences in intervention group compared to control after treatment (p < 0.001). Physical performance improved with statistically significant differences in intervention group compared to control (p < 0.001). |
| Philip 2022 [71] | RCT | Adults with long COVID-19 | n = 150 (81% f) Mean age: 49 ± 12 | Duration 6 weeks. Intervention Breathing exercises. Telerehabilitation. Intensity Not reported. | Usual care | Quality of life (SF-36) Dyspnea (DS-12) Anxiety (GAD-7) | Intervention group improved mental component of SF-36 with statistical differences compared to control (p = 0.047), while no differences in physical component (p = 0.54). Dyspnea improved in both groups compared to baseline, but without differences between groups (p = 0.38). Although anxiety improved in both groups, no statistical differences were found between group (p = 0.085). |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Meléndez-Oliva, E.; Martínez-Pozas, O.; Cuenca-Zaldívar, J.N.; Villafañe, J.H.; Jiménez-Ortega, L.; Sánchez-Romero, E.A. Efficacy of Pulmonary Rehabilitation in Post-COVID-19: A Systematic Review and Meta-Analysis. Biomedicines 2023, 11, 2213. https://doi.org/10.3390/biomedicines11082213
Meléndez-Oliva E, Martínez-Pozas O, Cuenca-Zaldívar JN, Villafañe JH, Jiménez-Ortega L, Sánchez-Romero EA. Efficacy of Pulmonary Rehabilitation in Post-COVID-19: A Systematic Review and Meta-Analysis. Biomedicines. 2023; 11(8):2213. https://doi.org/10.3390/biomedicines11082213
Chicago/Turabian StyleMeléndez-Oliva, Erika, Oliver Martínez-Pozas, Juan Nicolás Cuenca-Zaldívar, Jorge Hugo Villafañe, Laura Jiménez-Ortega, and Eleuterio A. Sánchez-Romero. 2023. "Efficacy of Pulmonary Rehabilitation in Post-COVID-19: A Systematic Review and Meta-Analysis" Biomedicines 11, no. 8: 2213. https://doi.org/10.3390/biomedicines11082213