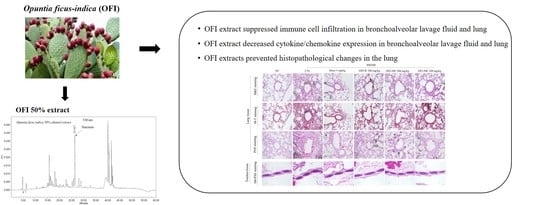
Opuntia ficus-indica Alleviates Particulate Matter 10 Plus Diesel Exhaust Particles (PM10D)—Induced Airway Inflammation by Suppressing the Expression of Inflammatory Cytokines and Chemokines
Abstract
:1. Introduction
2. Results
2.1. Chromatographic Analysis of OFI Extracted with 50% Ethanol
2.2. Effects of OFI-W, OFI-30E, and OFI-50E Administration on Immune Cell Numbers in BALF and Lung Tissues
2.3. Effects of OFI-W, OFI-30E, and OFI-50E Administration on Inflammatory Cytokines in BALF
2.4. Effects of OFI-W, OFI-30E, and OFI-50E Administration on ADMA and SDMA in Serum
2.5. Effects of OFI-W, OFI-30E, and OFI-50E Administration on the Expression of Inflammatory Cytokines in the Lungs
2.6. Effect of OFI-W, OFI-30E, and OFI-50E Administration on IRAK-1, TNF-α, and CXCL-1 Expression
2.7. Effect of OFI-W, OFI-30E, and OFI-50E Administration on Lung Tissue Damage
2.8. Effects of PM10D on the Inflammatory Response in the Lung
3. Discussion
4. Materials and Methods
4.1. Preparation of OFI Extract
4.2. High-Performance Liquid Chromatography (HPLC) Analysis of a 50% Ethanolic Extract of OFI (OFI-50E)
4.3. Animals and Treatments
4.4. Collection of Lung Cells and BALF and Cytological Analysis
4.5. Measurement of Inflammatory Mediators in BALF and Serum
4.6. Flow Cytometry
4.7. Quantitative Reverse Transcription-Polymerase Chain Reaction (qRT-PCR)
4.8. Western Blot Analysis
4.9. Immunofluorescence Staining
4.10. Histopathological Analysis of Lung and Tracheal Tissues
4.11. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Ambient Air Pollution: A Global Assessment of Exposure and Burden of Disease; World Health Organization: Geneva, Switzerland, 2016; pp. 1–121. ISBN 9789241511353. [Google Scholar]
- Pirani, M.; Best, N.; Blangiardo, M.; Liverani, S.; Atkinson, R.W.; Fuller, G.W. Analyzing the health effects of simultaneous exposure to physical and chemical properties of air particles. Environ. Int. 2015, 79, 56–64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thompson, J.E. Airborne particulate matter: Human exposure and health effects. J. Occup. Environ. Med. 2018, 60, 392–423. [Google Scholar] [CrossRef] [PubMed]
- Miller, M.R.; Shaw, C.A.; Langrish, J.P. From particles to patients: Oxidative stress and the cardiovascular effects of air pollution. Future Cardiol. 2012, 8, 577–602. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mei, M.; Song, H.; Chen, L.; Hu, B.; Xu, D.; Liu, Y.; Zhao, Y.; Chen, C. Early life exposure to three size-fractionated ultrafine and fine atmospheric particulates in Beijing exacerbates asthma development in mature mice. Part. Fibre Toxicol. 2018, 15, 13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dufka, M.; Docekal, B. Characterization of urban particulate matter by diffusive gradients in thin film technique. J. Anal. Methods Chem. 2018, 2018, 9698710. [Google Scholar] [CrossRef] [Green Version]
- Leikauf, G.D.; Kim, S.H.; Jang, A.S. Mechanisms of ultrafine particle-induced respiratory health effects. Exp. Mol. Med. 2020, 52, 329–337. [Google Scholar] [CrossRef]
- Kim, K.H.; Kabir, E.; Kabir, S. A review on the human health impact of airborne particulate matter. Environ. Int. 2015, 74, 136–143. [Google Scholar] [CrossRef]
- El-Mostafa, K.; El Kharrassi, Y.; Badreddine, A.; Andreoletti, P.; Vamecq, J.; El Kebbaj, M.S.; Latruffe, N.; Lizard, G.; Nasser, B.; Cherkaoui-Malki, M. Nopal cactus (Opuntia ficus-indica) as a source of bioactive compounds for nutrition, health and disease. Molecules 2014, 19, 14879–14901. [Google Scholar] [CrossRef] [Green Version]
- Matias, A.; Nunes, S.L.; Poejo, J.; Mecha, E.; Serra, A.T.; Madeira, P.J.; Bronze, M.R.; Duarte, C.M. Antioxidant and anti-inflammatory activity of a flavonoid-rich concentrate recovered from Opuntia ficus-indica juice. Food Funct. 2014, 5, 3269–3280. [Google Scholar] [CrossRef]
- Kuroda, E.; Ozasa, K.; Temizoz, B.; Ohata, K.; Koo, C.X.; Kanuma, T.; Kusakabe, T.; Kobari, S.; Horie, M.; Morimoto, Y.; et al. Inhaled fine particles induce alveolar macrophage death and interleukin-1α release to promote inducible bronchus-associated lymphoid tissue formation. Immunity 2016, 45, 1299–1310. [Google Scholar] [CrossRef] [Green Version]
- Robinson, N.; Ganesan, R.; Hegedus, C.; Kovács, K.; Kufer, T.A.; Virág, L. Programmed necrotic cell death of macrophages: Focus on pyroptosis, necroptosis, and parthanatos. Redox Biol. 2019, 26, 101239. [Google Scholar] [CrossRef] [PubMed]
- Seagrave, J. Mechanisms and implications of air pollution particle associations with chemokines. Toxicol. Appl. Pharmacol. 2008, 232, 469–477. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, W.; Omaye, S.T. Air pollutants, oxidative stress and human health. Mutat. Res. 2009, 674, 45–54. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Ren, W.; Jiang, Z.; Zhu, L. Regulation of the NLRP3 inflammasome and macrophage pyroptosis by the p38 MAPK signaling pathway in a mouse model of acute lung injury. Mol. Med. Rep. 2018, 18, 4399–4409. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kelley, N.; Jeltema, D.; Duan, Y.; He, Y. The NLRP3 inflammasome: An overview of mechanisms of activation and regulation. Int. J. Mol. Sci. 2019, 20, 3328. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Walters, D.M.; Breysse, P.N.; Wills-Karp, M. Ambient urban baltimore particulate-induced airway hyperresponsiveness and inflammation in mice. Am. J. Respir. Crit. Care Med. 2001, 164, 1438–1443. [Google Scholar] [CrossRef] [PubMed]
- Saba, E.; Lee, Y.S.; Yang, W.K.; Lee, Y.Y.; Kim, M.; Woo, S.M.; Kim, K.; Kwon, Y.S.; Kim, T.H.; Kwak, D.; et al. Effects of a herbal formulation, KGC3P, and its individual component, nepetin, on coal fly dust-induced airway inflammation. Sci. Rep. 2020, 10, 14036. [Google Scholar] [CrossRef]
- Yang, W.K.; Lyu, Y.R.; Kim, S.H.; Chae, S.W.; Kim, K.M.; Jung, I.C.; Park, Y.C. Protective Effect of GHX02 Extract on Particulate Matter-Induced Lung Injury. J. Med. Food 2020, 23, 611–632. [Google Scholar] [CrossRef]
- Curtis, J.L.; Byrd, P.K.; Warnock, M.L.; Kaltreider, H.B. Requirement of CD4-positive T cells for cellular recruitment to the lungs of mice in response to a particulate intratracheal antigen. J. Clin. Investig. 1991, 88, 1244–1254. [Google Scholar] [CrossRef]
- Ricciardolo, F.L.M.; Sterk, P.J.; Gaston, B.; Folkerts, G. Nitric oxide in health and disease of the respiratory system. Physiol. Rev. 2004, 84, 731–765. [Google Scholar] [CrossRef]
- McEvovy, M.A.; Schofield, P.W.; Smith, W.T.; Agho, K.; Mangoni, A.A.; Soiza, R.L.; Peel, R.; Hancock, S.J.; Carru, C.; Zinellu, A.; et al. Serum methylarginines and spirometry-measured lung function in older adults. PLoS ONE 2013, 8, e58390. [Google Scholar]
- Arlouskaya, Y.; Sawicka, A.; Głowala, M.; Giebułtowicz, J.; Korytowska, N.; Tałałaj, M.; Nowicka, G.; Wrzosek, M. Asymmetric dimethylarginine (ADMA) and symmetric dimethylarginine (SDMA) concentrations in patients with obesity and the risk of obstructive sleep apnea (OSA). J. Clin. Med. 2019, 8, 897. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bonser, L.R.; Zlock, L.; Finkbeiner, W.; Erle, D.J. Epithelial tethering of MUC5AC-rich mucus impairs mucociliary transport in asthma. J. Clin. Investig. 2016, 126, 2367–2371. [Google Scholar] [CrossRef] [PubMed]
- Bonser, L.R.; Erle, D.J. Airway mucus and asthma: The role of MUC5AC and MUC5B. J. Clin. Med. 2017, 6, 112. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ozaki, Y.; Xing, L.; Satake, M. Antiinflammatory effect of Trichosanthis kirilowii Maxim, and its effective parts. Biol. Pharm. Bull. 1996, 19, 1046–1048. [Google Scholar] [CrossRef] [Green Version]
- Maria, E.R.Q.; Gonzalo, A.; Javier, S.; Consuelo, S.M.; Isabel, G.; Juan, J.; Remedios, R.; José, M.N.; Elizabeth, P.; Francisco, S. Oleic acid modulates mRNA expression of liver X receptor (LXR) and its target genes ABCA1 and SREBP1c in human neutrophils. Eur. J. Nutr. 2014, 53, 1707–1717. [Google Scholar]












| Cell Phenotype (FACS Analysis) (×104 mL) | PM10D | ||||||
|---|---|---|---|---|---|---|---|
| NC | CTL | Dexa −3 mg/kg | OFI-W 200 mg/kg | OFI-30E 200 mg/kg | OFI-50E 200 mg/kg | ||
| Lymphocyte | Lung | 33.08 ± 1.81 | 79.23 ± 14.64 ## | 43.94 ± 2.18 * | 65.61 ± 10.80 | 56.03 ± 18.89 | 65.82 ± 4.67 |
| Neutrophils | 14.63 ± 4.04 | 43.50 ± 7.81 ## | 54.79 ± 6.58 | 35.68 ± 8.54 | 52.20 ± 1.97 * | 11.09 ± 0.74 *** | |
| CD3+/CD4+ | 25.10 ± 1.11 | 63.80 ± 14.24 ## | 37.8 ± 2.52 | 51.37 ± 11.08 | 58.04 ± 13.81 | 31.07 ± 3.05 | |
| CD3+/CD8+ | 9.55 ± 1.09 | 24.23 ± 4.27 ### | 21.36 ± 1.98 | 21.03 ± 3.74 | 25.41 ± 5.23 | 15.07 ± 0.44 * | |
| Gr-1+/CD11b+ | 3.83 ± 0.35 | 38.35 ± 7.57 ### | 13.86 ± 1.18 ** | 10.11 ± 1.38 ** | 11.96 ± 0.31 ** | 5.80 ± 0.32 *** | |
| CD3+/CD4+ | BALF | 0.02 ± 0.02 | 56.00 ± 1.90 ### | 3.77 ± 2.57 *** | 27.00 ± 1.61 *** | 28.45 ± 1.37 *** | 16.96 ± 2.33 *** |
| CD3+/CD8+ | 0.01 ± 0.01 | 24.25 ± 2.90 ### | 1.00 ± 0.28 *** | 15.52 ± 3.24 * | 27.33 ± 9.65 | 9.77 ± 2.09 *** | |
| Gr-1+/CD11b+ | 0.08 ± 0.00 | 166.72 ± 1.80 ### | 16.74 ± 0.98 *** | 84.72 ± 23.55 ** | 95.46 ± 10.46 *** | 33.5 ± 18.25 *** | |
| Gene | Sequence (5′-3′) |
|---|---|
| IL-6 | Forward: TCCAGTTGCCTTCTTGGGAC Reverse: GTGTAATTAAGCCTCCGACTTG |
| IL-5 | Forward: AGCACAGTGGTGAAAGAGACCTT Reverse: TCCAATGCATAGCTGGTGATTT |
| IL-1β | Forward: CAGGGTGGGTGTGCCGTCTTTC Reverse: TGCTTCCAAACCTTTGACCTGGGC |
| TNF-α | Forward: GGCTTTCCGAATTCACTGGAGCCT Reverse: CCCCGGCCTTCCAAATAAATACATTCATA |
| MUC5AC | Forward: AGAATATCTTTCAGGACCCCTGCT Reverse: ACACCAGTGCTGAGCATACTTTT |
| CXCL-1 | Forward: CCGAAGTCATAGCCACAC Reverse: GTGCCATCAGAGCAGTCT |
| TRPV1 | Forward: CATCTTCACCACGGCTGCTTAC Reverse: CAGACAGGATCTCTCCAGTGAC |
| MIP-2 (CXCL-2) | Forward: ATGCCTGAAGACCCTGCCAAG Reverse: GGTCAGTTAGCCTTGCCTTTG |
| COX-2 | Forward: GGGTGTCCCTTCACTTCTTTCA Reverse: TGGGAGGCACTTGCATTGA |
| GAPDH-Probe | Applied Biosystems® Mouse GAPDH Endogenous Control (VIC®/MGB Probe, 4352339E) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, Y.-S.; Yang, W.-K.; Park, Y.-R.; Park, Y.-C.; Park, I.-J.; Lee, G.-J.; Kang, H.-S.; Kim, B.-K.; Kim, S.-H. Opuntia ficus-indica Alleviates Particulate Matter 10 Plus Diesel Exhaust Particles (PM10D)—Induced Airway Inflammation by Suppressing the Expression of Inflammatory Cytokines and Chemokines. Plants 2022, 11, 520. https://doi.org/10.3390/plants11040520
Lee Y-S, Yang W-K, Park Y-R, Park Y-C, Park I-J, Lee G-J, Kang H-S, Kim B-K, Kim S-H. Opuntia ficus-indica Alleviates Particulate Matter 10 Plus Diesel Exhaust Particles (PM10D)—Induced Airway Inflammation by Suppressing the Expression of Inflammatory Cytokines and Chemokines. Plants. 2022; 11(4):520. https://doi.org/10.3390/plants11040520
Chicago/Turabian StyleLee, Young-Sil, Won-Kyung Yang, Ye-Rin Park, Yang-Chun Park, In-Jae Park, Geung-Joo Lee, Hyung-Sik Kang, Bong-Kyun Kim, and Seung-Hyung Kim. 2022. "Opuntia ficus-indica Alleviates Particulate Matter 10 Plus Diesel Exhaust Particles (PM10D)—Induced Airway Inflammation by Suppressing the Expression of Inflammatory Cytokines and Chemokines" Plants 11, no. 4: 520. https://doi.org/10.3390/plants11040520