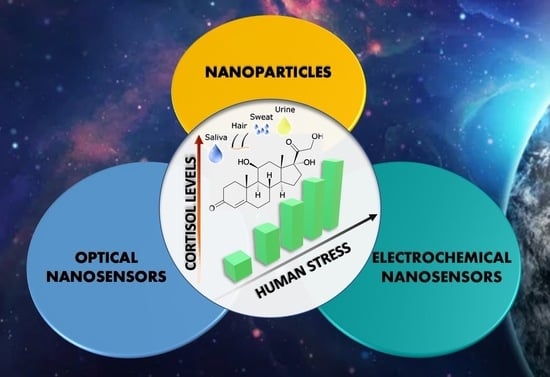
Nanomaterials for Cortisol Sensing
Abstract
:1. Introduction
2. Nanomaterials for Sensing
3. Optical Nanosensors
4. Electrochemical Nanosensors
5. Conclusions and Future Perspectives
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Glaser, R.; Kiecolt-Glaser, J.K. Stress-induced immune dysfunction: Implications for health. Nat. Rev. Immunol. 2005, 5, 243. [Google Scholar] [CrossRef] [PubMed]
- Sawyers, C.; Sheerin, C.; Eastman, M.; Burchett, J.; Howell, P.; Neigh, G.; Amstadter, A.B.; Hettema, J.; Roberson-Nay, R. Genetic, and Environmental Influences on Cortisol Reactivity to a Psychosocial Stressor in Adolescents and Young Adults. Psychoneuroendocrinology 2021, 127, 105195. [Google Scholar] [CrossRef] [PubMed]
- Quin, H.Y.; Cheng, C.W.; Tang, X.D.; Bian, Z.X. Impact of psychological stress on irritable bowel syndrome. World J. Gastroenterol. 2014, 20, 14126. [Google Scholar] [CrossRef]
- Zefferino, R.; Gioia, S.D.; Conese, M. Molecular links between endocrine, nervous and immune system during chronic stress. Brain Behav. 2020, 1, e01960. [Google Scholar] [CrossRef] [PubMed]
- Yao, B.-C.; Meng, L.-B.; Hao, M.-L.; Zhang, Y.-M.; Gong, T.; Guo, Z.-G. Chronic stress: A critical risk factor for atherosclerosis. J. Int. Med. Res. 2019, 47, 1429. [Google Scholar] [CrossRef]
- Charney, D.S. Psychobiological mechanisms of resilience and vulnerability: Implications for successful adaptation to extreme stress. Am. J. Psychiatry 2004, 161, 195–216. [Google Scholar] [CrossRef] [Green Version]
- Djuric, Z.; Bird, C.E.; Furumoto-Dawson, A.; Rauscher, G.H.; Ruffin, M.T.; Stowe, I.V.R.P.; Tucker, K.L.; Masi, C.M. Biomarkers of Psychological Stress in Health Disparities Research. Open Biomarkers J. 2008, 1, 7–19. [Google Scholar] [CrossRef]
- Pradhan, T.; Jung, H.S.; Jang, J.H.; Kim, T.W.; Kang, C.; Kim, J.S. Chemical sensing of neurotransmitters. Chem. Soc. Rev. 2014, 43, 4684–4713. [Google Scholar] [CrossRef]
- Taves, M.D.; Gomez-Sanchez, C.E.; Soma, K.K. Extra-adrenal glucocorticoids and mineralocorticoids: Evidence for local synthesis, regulation, and function. Am. J. Physiol. Endocrinol. Metab. 2011, 301, E11–E24. [Google Scholar] [CrossRef] [Green Version]
- Tsigos, C.; Chrousos, G.P. Hypothalamic-pituitary-adrenal axis, neuroendocrine factors and stress. J. Psychosom. Res. 2002, 53, 865–887. [Google Scholar] [CrossRef]
- Gallagher, T.F.; Yoshida, K.; Roffwarg, H.D.; Fukushima, D.K.; Weitzman, E.D.; Hellman, L. ACTH and cortisol secretory patterns in man. J. Clin. Endocrinol. Metab. 1973, 36, 1058–1068. [Google Scholar] [CrossRef] [PubMed]
- Chan, S.; Debono, M. Replication of cortisol circadian rhythm: New advances in hydrocortisone replacement therapy. Ther. Adv. Endocrinol. Metabol. 2010, 1, 129–138. [Google Scholar] [CrossRef] [PubMed]
- Clow, A.; Hucklebridge, F.; Stalder, T.; Evans, P.; Thorn, L. The cortisol awakening response: More than a measure of HPA axis function. Neurosci. Biobehav. Rev. 2010, 35, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Sephton, S.E.; Lush, E.; Dedert, E.A.; Floyd, A.R.; Rebholz, W.N.; Dhabhar, F.S.; Spiegel, D.; Salmon, P. Diurnal cortisol rhythm as a predictor of lung cancer survival. Brain Behav. Immun. 2013, 30, S163–S170. [Google Scholar] [CrossRef] [PubMed]
- Levine, A.; Zagoory-Sharon, O.; Feldman, R.; Lewis, J.G.; Weller, A. Measuring cortisol in human psychobiological studies. Physiol. Behav. 2007, 90, 43–53. [Google Scholar] [CrossRef]
- Khelifa, L.; Hu, Y.; Jiang, N.; Yetisen, A.K. Lateral flow assays for hormone detection. Lab Chip 2022, 22, 2451–2475. [Google Scholar] [CrossRef]
- Zea, M.; Bellagambi, F.G.; Halima, H.B.; Zine, N.; Jaffrezi-Renault, N.; Villa, R.; Gabriela, G.; Errachid, A. Electrochemical sensors for cortisol detections: Almost there. Trends Analyt. Chem. 2020, 132, 116058. [Google Scholar] [CrossRef]
- Xing, S.; Jiang, J.; Pan, T. Interfacial microfluidic transport on micropatterned superhydrophobic textile. Lab Chip 2013, 13, 1937–1947. [Google Scholar] [CrossRef]
- Bennett, A.; Hayssen, V. Hair as a biological indicator of drug use, drug abuse or chronic exposure to environmental toxicants. Int. J. Toxicol. 2006, 25, 143–163. [Google Scholar] [CrossRef]
- Venugopal, M.; Feuvrel, K.E.; Mongin, D.; Bambot, S.; Faupel, M.; Panangadan, A.; Talukder, A.; Pidva, R. Clinical evaluation of a novel interstitial fluid sensor system for remote continuous alcohol monitoring. Sens. J. IEEE 2008, 8, 71–80. [Google Scholar] [CrossRef]
- Kaushik, A.; Yndart, A.; Jayant, R.D.; Sagar, V.; Atluri, V.; Bhansali, S.; Nair, M. Electrochemical sensing method for point-of-care cortisol detection in human immunodeficiency virus-infected patients. Int. J. Nanomed. 2015, 10, 677–685. [Google Scholar] [CrossRef] [Green Version]
- Kim, H.T.; Jin, E.; Lee, M.H. Portable Chemiluminescence-Based Lateral Flow Assay Platform for the Detection of Cortisol in Human Serum. Biosensors 2021, 11, 191. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Zhang, Z. Capillary Electrophoresis-Based Immunoassay for the Determination of Brevetoxin-B in Shellfish using Electrochemical Detection. J. Chromatograp. Sci. 2013, 51, 107–111. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baraket, A.; Lee, M.; Zine, N.; Sigaud, M.; Yaakoubi, N.; Trivella, M.G.; Zabala, M.; Bausells, J.; Jaffrezic-Renault, N.; Errachid, A. Diazonium modified gold microelectrodes onto polyimide substrates for impedimetric cytokine detection with an integrated Ag/AgCl reference electrode. Sens. Actuator B Chem. 2013, 189, 165–172. [Google Scholar] [CrossRef]
- Stefan, R.I.; Van, J.S.; Aboul-Enein, H.Y. Design and Use of Electrochemical Sensors in Enantioselective High Throughput Screening of Drugs. A Minireview. Comb. Chem. High Throughput Screen 2000, 3, 445–454. [Google Scholar] [CrossRef]
- Lee, S.; Hwan, S.L.; Hye, J.S.; Seol, A.K.; Jimyeong, P.; Hyu, C.K.; Hyogyeong, K.; Hyung, J.K.; Yun, T.K.; Kyoung, R.L.; et al. Simultaneous Determination of Cortisol and Cortisone from Human Serum by Liquid Chromatography-Tandem Mass Spectrometry. J. Anal. Methods Chem. 2014, 2014, 787483. [Google Scholar] [CrossRef] [Green Version]
- Baid, S.K.; Sinaii, N.; Wade, M.; Rubino, D.; Nieman, L.K. Radioimmunoassay and Tandem Mass Spectrometry Measurement of Bedtime Salivary Cortisol Levels: A Comparison of Assays to Establish Hypercortisolism. J. Clin. Endocrinol. Metab. 2007, 92, 3102–3107. [Google Scholar] [CrossRef] [Green Version]
- Shim, B.S.; Chen, W.; Doty, C.; Xu, C.; Kotov, N.A. Smart electronic yarns and wearable fabrics for human biomonitoring made by carbon nanotube coating with polyelectrolytes. Nano Lett. 2018, 8, 4151–4157. [Google Scholar] [CrossRef]
- Koczula, K.M.; Gallotta, A. Lateral flow assays. Essays Biochem. 2016, 60, 111–120. [Google Scholar] [CrossRef]
- Kaushik, A.; Vasudev, A.; Arya, S.K.; Pasha, S.K.; Bhansali, S. Recent advances in cortisol sensing technologies for point-of-care application. Biosens. Bioelectr. 2014, 53, 499–512. [Google Scholar] [CrossRef]
- Abidin, A.S.Z.; Rahim, R.A.; Arshad, M.K.M.; Nabilah, M.F.F.; Voon, C.H.; Tang, T.-H.; Citartan, M. Current and Potential Developments of Cortisol Aptasensing towards Point-of-Care Diagnostics (POTC). Sensors 2017, 17, 1180. [Google Scholar] [CrossRef] [PubMed]
- Tuccitto, N.; Fichera, L.; Ruffino, R.; Cantaro, V.; Sfuncia, G.; Nicotra, G.; Sfrazzetto, G.T.; Li-Destri, G.; Valenti, A.; Licciardello, A.; et al. Carbon Quantum Dots as Fluorescence Nanochemosensors for Selective Detection of Amino Acids. ACS Appl. Nano Mater. 2021, 4, 6250–6256. [Google Scholar] [CrossRef]
- Santonocito, R.; Tuccitto, N.; Cantaro, V.; Carbonaro, A.B.; Pappalardo, A.; Greco, V.; Buccilli, V.; Maida, P.; Zavattaro, D.; Sfuncia, G.; et al. Smartphone-Assisted Sensing of Trinitrotoluene by Optical Array. ACS Omega ASAP 2022, 7, 37122–37132. [Google Scholar] [CrossRef] [PubMed]
- Tuccitto, N.; Spitaleri, L.; Destri, G.L.; Pappalardo, A.; Gulino, A.; Sfrazzetto, G.T. Supramolecular Sensing of a Chemical Warfare Agents Simulant by Functionalized Carbon Nanoparticles. Molecules 2020, 25, 5731. [Google Scholar] [CrossRef] [PubMed]
- Tuccitto, N.; Riela, L.; Zammataro, A.; Spitaleri, L.; Destri, G.L.; Sfuncia, G.; Nicotra, G.; Pappalardo, A.; Capizzi, G.; Sfrazzetto, G.T. Functionalized Carbon Nanoparticle-Based Sensors for Chemical Warfare Agents. ACS Appl. Nano Mater. 2020, 3, 8182–8191. [Google Scholar] [CrossRef]
- Qin, G.; Zhao, S.; Huang, Y.; Jiang, J.; Liu, Y.-M. A sensitive gold nanoparticles sensing platform based on resonance energy transfer for chemiluminescence light on detection of biomolecules. Biosens. Bioelectr. 2013, 46, 119–123. [Google Scholar] [CrossRef]
- Chen, S.; Liu, M.-X.; Yu, Y.-L.; Wang, J.-H. Room-temperature synthesis of fluorescent carbon-based nanoparticles and their application in multidimensional sensing. Sens. Actuators B Chem. 2019, 288, 749–756. [Google Scholar] [CrossRef]
- Santonocito, R.; Intravaia, M.; Caruso, I.M.; Pappalardo, A.; Sfrazzetto, G.T.; Tuccitto, N. Fluorescence sensing by carbon nanoparticles. Nanoscale Adv. 2022, 4, 1926–1948. [Google Scholar] [CrossRef]
- Testa, C.; Zammataro, A.; Pappalardo, A.; Sfrazzetto, G.T. Catalysis with carbon nanoparticles. RSC Adv. 2019, 9, 27659–27664. [Google Scholar] [CrossRef] [Green Version]
- Yadav, S.; Raman, A.P.S.; Meena, H.; Goswami, A.G.; Kumar, V.B.; Jain, P.; Kumar, G.; Sagar, M.; Rana, D.K.; Bahadur, I.; et al. An Update on Graphene Oxide: Applications and Toxicity. ACS Omega 2022, 7, 35387–35445. [Google Scholar] [CrossRef]
- Jafari-Nodoushan, H.; Mojtabavi, S.; Faramarzi, M.A.; Samadi, N. Organic-inorganic hybrid nanoflowers: The known, the unknown, and the future. Adv. Colloid Interface Sci. 2022, 309, 102780. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Liang, T.; Chen, L.; Chen, Y.; Bo-Ru, Y.; Luo, Y.; Gui-Shi, L. Self-assembly, alignment, and patterning of metal nanowires. Nanoscale Horiz. 2022, 7, 1299–1339. [Google Scholar] [CrossRef] [PubMed]
- Aspoukeh, P.K.; Barzinjy, A.A.; Hamad, S.M. Synthesis, Properties and uses of ZnO nanorods: A mini review. Int. Nano Lett. 2022, 12, 153–168. [Google Scholar] [CrossRef]
- Jiao, M.-Z.; Chen, X.-Y.; Hu, K.-X.; Qian, D.-Y.; Zhao, X.-H.; Ding, E.-J. Recent developments of nanomaterials-based conductive type methane sensors. Rare Met. 2021, 40, 1515–1527. [Google Scholar] [CrossRef]
- Walcarius, A.; Minteer, S.D.; Wang, J.; Lin, Y.; Merkoçi, A. Nanomaterials for bio-functionalized electrodes: Recent trends. J. Mater. Chem. B 2013, 1, 4878–4908. [Google Scholar] [CrossRef]
- Jeon, J.; Uthaman, S.; Lee, J.; Hwanga, H.; Kim, G.; Yoo, P.J.; Hammock, B.D.; Kim, C.S.; Park, Y.-S.; Park, I.-K. In-direct localized surface plasmon resonance (LSPR)-based nanosensors for highly sensitive and rapid detection of cortisol. Sens. Actuators B Chem. 2018, 266, 710–716. [Google Scholar] [CrossRef]
- Stevens, R.C.; Soelberg, S.D.; Near, S.; Furlong, C.E. Detection of cortisol in saliva with a flow-filtered, portable surface plasmon resonance biosensor system. Anal. Chem. 2008, 80, 6747–6751. [Google Scholar] [CrossRef] [Green Version]
- Tahara, Y.; Huang, Z.; Kiritoshi, T.; Onodera, T.; Toko, K. Development of indirect competitive immuno-assay method using SPR detection for rapid and highly sensitive measurement of salivary cortisol levels. Front. Bioeng. Biotechnol. 2014, 2, 15. [Google Scholar] [CrossRef]
- Liu, Y.; Wu, B.; Tanyi, E.K.; Yeasmin, S.; Cheng, L.-J. Label-Free Sensitive Detection of Steroid Hormone Cortisol Based on Target-Induced Fluorescence Quenching of Quantum Dots. Langmuir 2020, 36, 7781–7788. [Google Scholar] [CrossRef]
- Smith, A.M.; Nie, S. Semiconductor nanocrystals: Structure, properties, and band gap engineering. Acc. Chem. Res. 2010, 43, 190–200. [Google Scholar] [CrossRef]
- Liu, Y.; Kannegulla, A.; Wu, B.; Cheng, L.-J. Quantum dot fullerene-based molecular beacon nanosensors for rapid, highly sensitive nucleic acid detection. ACS Appl. Mater. Interfaces 2018, 10, 18524–18531. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.S.; Kim, H.J.; Lee, J.; Lee, T.; Yun, J.; Lee, G.; Hong, Y. Hand-Held Raman Spectrometer-Based Dual Detection of Creatinine and Cortisol in Human Sweat Using Silver Nanoflakes. Anal. Chem. 2021, 93, 14996–15004. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Leis, A.; Rivera-Arreba, I.; Sanchez-Cortes, S. Morphological tuning of plasmonic silver nanostars by controlling the nanoparticle growth mechanism: Application in the SERS detection of the amyloid marker Congo Red. Colloid Surf. Physicochem. Eng. Asp. 2017, 535, 49–60. [Google Scholar] [CrossRef]
- Barfidokht, A.; Mishra, R.K.; Seenivasan, R.; Shuyang, L.; Lee, J.H.; Wang, J.; Hall, D.A. Wearable electrochemical glove-based sensor for rapid and on-site detection of fentanyl. Sens. Actuators B Chem. 2019, 296, 126422. [Google Scholar] [CrossRef] [PubMed]
- Mohammad-Andashti, P.; Ramezani, Z.; Zare-Shahabadi, V.; Torabi, P. Rapid and green synthesis of highly luminescent MoS2 quantum dots via microwave exfoliation of MoS2 powder and its application as a fluorescence probe for cortisol detection in human saliva. Colloids Surf. A Physicochem. Eng. Asp. 2022, 64, 129048. [Google Scholar] [CrossRef]
- Yilmaz, G.; Saylan, Y.; Göktürk, I.; Yılmaz, F.; Denizli, A. Selective Amplification of Plasmonic Sensor Signal for Cortisol Detection Using Gold Nanoparticles. Biosensors 2022, 12, 482. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Dai, F.; Lu, L.; Yin, M.; Xue, L.; Feng, W.; Li, B.; Jiao, J.; Chen, Q. All-in-one calcium nanoflowers for dual outputs biosensor: A simultaneous strategy for depression drug evaluation and non-invasive stress assessment. Biosens. Bioelectr. 2022, 216, 114655. [Google Scholar] [CrossRef]
- Singh, N.K.; Arya, S.K.; Estrela, P.; Goswami, P. Capacitive malaria aptasensor using Plasmodium falciparum glutamate dehydrogenase as target antigen in undiluted human serum. Biosens. Bioelectr. 2018, 117, 246–252. [Google Scholar] [CrossRef]
- Sun, A.C.; Hall, D.A. Point-of-Care Smartphone-based Electrochemical Biosensing. Electroanalysis 2019, 31, 2–16. [Google Scholar] [CrossRef] [Green Version]
- Venkatesh, A.G.; Brickner, H.; Looney, D.; Hall, D.A.; Aronoff, S.E. Clinical detection of Hepatitis C viral infection by yeast-secreted HCV-core: Gold-binding-peptide. Biosens. Bioelectr. 2018, 119, 230–236. [Google Scholar] [CrossRef]
- Wang, J. Electrochemical biosensors: Towards point-of-care cancer diagnostics0. Biosens. Bioelectr. 2006, 21, 1887–1892. [Google Scholar] [CrossRef] [PubMed]
- Arya, S.K.; Dey, A.; Bhansali, S. Polyaniline protected gold nanoparticles based mediator and label free electrochemical cortisol biosensor. Biosens. Bioelectr. 2011, 28, 166–173. [Google Scholar] [CrossRef] [PubMed]
- Vabbina, P.K.; Kaushik, A.; Pokhrel, N.; Bhansali, S.; Pala, N. Electrochemical cortisol immunosensors based on sonochemically synthesized zinc oxide 1D nanorods and 2D nanoflakes. Biosens. Bioelectr. 2015, 63, 124–130. [Google Scholar] [CrossRef] [PubMed]
- Xu, S.; Wang, Z.L. One-dimensional ZnO nanostructures: Solution growth and functional properties. Nano Res. 2011, 4, 1013–1098. [Google Scholar] [CrossRef] [Green Version]
- Sanghavi, B.J.; Moore, J.A.; Chávez, J.L.; Hagen, J.A.; Loughnane, N.K.; Chou, C.-F.; Swami, N.S. Aptamer-functionalized nanoparticles for surface immobilization-free electrochemical detection of cortisol in a microfluidic device. Biosens. Bioelectr. 2016, 78, 244–252. [Google Scholar] [CrossRef]
- Nijhuis, J.; Schmidt, S.; Tran, N.N.; Hessel, V. Microfluidics and Macrofluidics in Space: ISS-Proven Fluidic Transport and Handling Concepts Front. Sp. Technol. 2022, 2, 779696. [Google Scholar] [CrossRef]
- Sun, B.; Gou, Y.; Ma, Y.; Zheng, X.; Bai, R.; Abdelmoaty, A.A.A.; Hu, F. Investigate electrochemical immunosensor of cortisol based on gold nanoparticles/magnetic functionalized reduced graphene oxide Author links open overlay panel. Biosens. Bioelectr. 2017, 88, 55–62. [Google Scholar] [CrossRef]
- Liu, X.; Hsu, S.P.C.; Liu, W.-C.; Wang, Y.-M.; Liu, X.; Lo, C.-S.; Lin, Y.-C.; Nabilla, S.C.; Li, Z.; Hong, Y.; et al. Salivary Electrochemical Cortisol Biosensor Based on Tin Disulfide Nanoflakes. Nanoscale Res. Lett. 2019, 14, 14–189. [Google Scholar] [CrossRef] [Green Version]
- Wang, C.; Tang, K.; Yang, Q.; Qian, Y. Raman scattering, far infrared spectrum and photoluminescence of SnS2 nanocrystallites. Chem. Phys. Lett. 2002, 357, 371–375. [Google Scholar] [CrossRef]
- Klinghammer, S.; Voitsekhivska, T.; Licciardello, N.; Kim, K.; Baek, C.-K.; Cho, H.; Wolter, K.-J.; Kirschbaum, C.; Baraban, L.; Cuniberti, G. Nanosensor-Based Real-Time Monitoring of Stress Biomarkers in Human Saliva Using a Portable Measurement System. ACS Sens. 2020, 5, 4081–4091. [Google Scholar] [CrossRef]
- Tran, D.P.; Winter, M.A.; Wolfrum, B.; Stockmann, R.; Yang, C.-T.; Pourhassan-Moghaddam, M.; Offenhaüsser, A.; Thierry, B. Toward Intraoperative Detection of Disseminated Tumor Cells in Lymph Nodes with Silicon Nanowire Field Effect Transistors. ACS Nano 2016, 10, 2357–2364. [Google Scholar] [CrossRef] [Green Version]
- Martin, J.A.; Chávez, J.L.; Chushak, Y.; Chapleau, R.R.; Hagen, J.; Kelley-Loughnane, N. Tunable Stringency Aptamer Selection and Gold Nanoparticle Assay for Detection of Cortisol. Anal. Bioanal. Chem. 2014, 406, 4637–4647. [Google Scholar] [CrossRef] [PubMed]
- Madhu, S.; Anthuuvan, A.J.; Ramasamy, S.; Manickam, P.; Bhansali, S.; Nagamony, P.; Chinnuswamy, V. ZnO Nanorod Integrated Flexible Carbon Fibers for Sweat Cortisol Detection. ACS Appl. Electron. Mater. 2020, 2, 499–509. [Google Scholar] [CrossRef]
- Rison, S.; Rajeev, R.; Bhat, V.S.; Mathews, A.T.; Varghese, A.; Hegde, G. Non-enzymatic electrochemical determination of salivary cortisol using ZnO-graphene nanocomposites. RSC Adv. 2021, 11, 37877. [Google Scholar] [CrossRef] [PubMed]
- Sonawane, A.; Mujawar, M.A.; Manickam, P.; Bhansali, S. Plasma-Induced Enhancement in Electronic Properties of Gold Nanoparticles: Application in Electrochemical Biosensing of Cortisol. ACS Appl. Electron. Mater. 2021, 3, 230–237. [Google Scholar] [CrossRef]
- Singh, N.K.; Chung, S.; Sveiven, M.; Hall, D.A. Cortisol Detection in Undiluted Human Serum Using a Sensitive Electrochemical Structure-Switching Aptamer over an Antifouling Nanocomposite Layer. ACS Omega 2021, 6, 27888–27897. [Google Scholar] [CrossRef]
- Madhu, S.; Ramasamy, S.; Magudeeswaran, V.; Manickam, P.; Nagamony, P.; Chinnuswamy, V. SnO2 nanoflakes deposited carbon yarn-based electrochemical immunosensor towards cortisol measurement. J. Nanostruct. Chem. 2022, in press. [Google Scholar] [CrossRef]
















| Sample | Cortisol Concentrations |
|---|---|
| Blood | 25 mg/mL (morning), 2 mg/mL (midnight) |
| Urine a | 21,458–149,696 ng/24 h 44,000–140,000 ng/24 h |
| Saliva | 1–12 ng/mL (morning), 0.1–3 ng/mL (evening) |
| Sweat | 8–142 ng/mL |
| Hair | 18–153 pg/mg |
| Interstitial fluid (ISF) | 12–34 ng/mL (morning), 9–13 ng/mL (evening) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Trusso Sfrazzetto, G.; Santonocito, R. Nanomaterials for Cortisol Sensing. Nanomaterials 2022, 12, 3790. https://doi.org/10.3390/nano12213790
Trusso Sfrazzetto G, Santonocito R. Nanomaterials for Cortisol Sensing. Nanomaterials. 2022; 12(21):3790. https://doi.org/10.3390/nano12213790
Chicago/Turabian StyleTrusso Sfrazzetto, Giuseppe, and Rossella Santonocito. 2022. "Nanomaterials for Cortisol Sensing" Nanomaterials 12, no. 21: 3790. https://doi.org/10.3390/nano12213790