Natural Polyphenol-Containing Gels against HSV-1 Infection: A Comparative Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
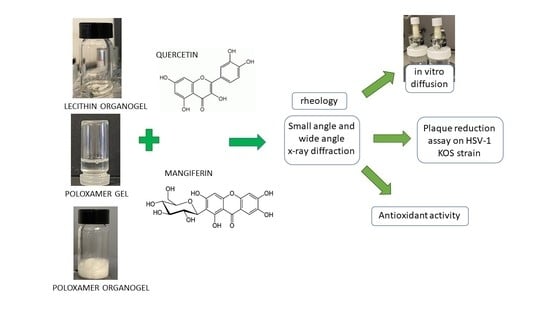
2.2. Preparation of Semisolid Forms
2.3. Rheological Measurements
2.4. X-ray Analyses
2.5. Polyphenol Content of Semisolid Forms
2.6. In Vitro Diffusion Experiments
2.7. HPLC Analysis
2.8. Photochemiluminescence (PCL) Test
2.9. Antiviral Activity Study against HSV-1
2.9.1. Cell Culture
2.9.2. Herpes Virus Stock Generation
2.9.3. Titration of Virus by Plaque Assay
2.9.4. Antiviral Assay
2.9.5. Virucidal Assay
2.9.6. Statistical Analysis
3. Results
3.1. Preparation and Characterization of Semisolid Forms
3.2. In Vitro Polyphenol Diffusion Study
3.3. Polyphenol Stability
3.4. Antioxidant Activity
3.5. In Vitro Antiviral Activity
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Musarra-Pizzo, M.; Ginestra, G.; Smeriglio, A.; Pennisi, R.; Sciortino, M.T.; Mandalari, G. The Antimicrobial and Antiviral Activity of Polyphenols from Almond (Prunus dulcis L.) Skin. Nutrients 2019, 11, 2355. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Othman, L.; Sleiman, A.; Abdel-Massih, R.M. Antimicrobial Activity of Polyphenols and Alkaloids in Middle Eastern Plants. Front. Microbiol. 2019, 10, 911. [Google Scholar] [CrossRef]
- Cushnie, T.P.T.; Lamb, A.J. Antimicrobial Activity of Flavonoids. Int. J. Antimicrob. Agents 2005, 26, 343–356. [Google Scholar] [CrossRef] [PubMed]
- Epstein, J.B.; Scully, C. Herpes Simplex Virus in Immunocompromised Patients: Growing Evidence of Drug Resistance. Oral Surg. Oral Med. Oral Pathol. 1991, 72, 47–50. [Google Scholar] [CrossRef]
- Roca, I.; Akova, M.; Baquero, F.; Carlet, J.; Cavaleri, M.; Coenen, S.; Cohen, J.; Findlay, D.; Gyssens, I.; Heure, O.E.; et al. The Global Threat of Antimicrobial Resistance: Science for Intervention. New Microbes New Infect. 2015, 6, 22–29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Field, H.J. Herpes Simplex Virus Antiviral Drug Resistance—Current Trends and Future Prospects. J. Clin. Virol. 2001, 21, 261–269. [Google Scholar] [CrossRef]
- Bradshaw, M.J.; Venkatesan, A. Herpes Simplex Virus-1 Encephalitis in Adults: Pathophysiology, Diagnosis, and Management. Neurotherapeutics 2016, 13, 493–508. [Google Scholar] [CrossRef] [Green Version]
- Gilbert, C.; Bestman-Smith, J.; Boivin, G. Resistance of Herpesviruses to Antiviral Drugs: Clinical Impacts and Molecular Mechanisms. Drug Resist. Updates 2002, 5, 88–114. [Google Scholar] [CrossRef]
- Jiang, Y.-C.; Feng, H.; Lin, Y.-C.; Guo, X.-R. New Strategies against Drug Resistance to Herpes Simplex Virus. Int. J. Oral Sci. 2016, 8, 1–6. [Google Scholar] [CrossRef]
- Allard, J.P.; Aghdassi, E.; Chau, J.; Tam, C.; Kovacs, C.M.; Salit, I.E.; Walmsley, S.L. Effects of Vitamin E and C Supplementation on Oxidative Stress and Viral Load in HIV-Infected Subjects. AIDS 1998, 12, 1653–1659. [Google Scholar] [CrossRef] [PubMed]
- Mathew, D.; Hsu, W.-L. Antiviral Potential of Curcumin. J. Funct. Foods 2018, 40, 692–699. [Google Scholar] [CrossRef]
- Di Sotto, A.; Checconi, P.; Celestino, I.; Locatelli, M.; Carissimi, S.; De Angelis, M.; Rossi, V.; Limongi, D.; Toniolo, C.; Martinoli, L.; et al. Antiviral and Antioxidant Activity of a Hydroalcoholic Extract from Humulus lupulus L. Oxid. Med. Cell. Longev. 2018, 2018, 5919237. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- El-Toumy, S.A.; Salib, J.Y.; El-Kashak, W.A.; Marty, C.; Bedoux, G.; Bourgougnon, N. Antiviral Effect of Polyphenol Rich Plant Extracts on Herpes Simplex Virus Type 1. Food Sci. Hum. Wellness 2018, 7, 91–101. [Google Scholar] [CrossRef]
- Zhou, Y.; Zheng, J.; Li, Y.; Xu, D.-P.; Li, S.; Chen, Y.-M.; Li, H.-B. Natural Polyphenols for Prevention and Treatment of Cancer. Nutrients 2016, 8, 515. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Lee, H.H.; Shin, Y.S.; Kang, H.; Cho, H. The Anti-HSV-1 Effect of Quercetin Is Dependent on the Suppression of TLR-3 in Raw 264.7 Cells. Arch. Pharm. Res. 2017, 40, 623–630. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.H.; Kim, J.-E.; Song, Y.-J. Antiviral Activities of Quercetin and Isoquercitrin Against Human Herpesviruses. Molecules 2020, 25, 2379. [Google Scholar] [CrossRef] [PubMed]
- Du, S.; Liu, H.; Lei, T.; Xie, X.; Wang, H.; He, X.; Tong, R.; Wang, Y. Mangiferin: An Effective Therapeutic Agent against Several Disorders (Review). Mol. Med. Rep. 2018, 18, 4775–4786. [Google Scholar] [CrossRef] [Green Version]
- Rechenchoski, D.Z.; Agostinho, K.F.; Faccin-Galhardi, L.C.; Lonni, A.A.S.G.; da Silva, J.V.H.; de Andrade, F.G.; Cunha, A.P.; Ricardo, N.M.P.S.; Nozawa, C.; Linhares, R.E.C. Mangiferin: A Promising Natural Xanthone from Mangifera Indica for the Control of Acyclovir—Resistant Herpes Simplex Virus 1 Infection. Bioorg. Med. Chem. 2020, 28, 115304. [Google Scholar] [CrossRef]
- Hatahet, T.; Morille, M.; Hommoss, A.; Devoisselle, J.M.; Müller, R.H.; Bégu, S. Quercetin Topical Application, from Conventional Dosage Forms to Nanodosage Forms. Eur. J. Pharm. Biopharm. 2016, 108, 41–53. [Google Scholar] [CrossRef]
- Sguizzato, M.; Ferrara, F.; Hallan, S.S.; Baldisserotto, A.; Drechsler, M.; Malatesta, M.; Costanzo, M.; Cortesi, R.; Puglia, C.; Valacchi, G.; et al. Ethosomes and Transethosomes for Mangiferin Transdermal Delivery. Antioxidants 2021, 10, 768. [Google Scholar] [CrossRef]
- Cunningham, A.; Griffiths, P.; Leone, P.; Mindel, A.; Patel, R.; Stanberry, L.; Whitley, R. Current Management and Recommendations for Access to Antiviral Therapy of Herpes Labialis. J. Clin. Virol. 2012, 53, 6–11. [Google Scholar] [CrossRef] [Green Version]
- Lipipun, V.; Sasivimolphan, P.; Yoshida, Y.; Daikoku, T.; Sritularak, B.; Ritthidej, G.; Likhitwitayawuid, K.; Pramyothin, P.; Hattori, M.; Shiraki, K. Topical Cream-Based Oxyresveratrol in the Treatment of Cutaneous HSV-1 Infection in Mice. Antivir. Res. 2011, 91, 154–160. [Google Scholar] [CrossRef]
- Miyazawa, T.; Itaya, M.; Burdeos, G.C.; Nakagawa, K.; Miyazawa, T. A Critical Review of the Use of Surfactant-Coated Nanoparticles in Nanomedicine and Food Nanotechnology. Int. J. Nanomed. 2021, 16, 3937–3999. [Google Scholar] [CrossRef]
- Tian, W.; Hu, Q.; Xu, Y.; Xu, Y. Effect of Soybean-Lecithin as an Enhancer of Buccal Mucosa Absorption of Insulin. Bio-Med. Mater. Eng. 2012, 22, 171–178. [Google Scholar] [CrossRef]
- McIntosh, T.J. Hydration Properties of Lamellar and Non-Lamellar Phases of Phosphatidylcholine and Phosphatidylethanolamine. Chem. Phys. Lipids 1996, 81, 117–131. [Google Scholar] [CrossRef]
- Wohlrab, J.; Klapperstück, T.; Reinhardt, H.-W.; Albrecht, M. Interaction of Epicutaneously Applied Lipids with Stratum Corneum Depends on the Presence of Either Emulsifiers or Hydrogenated Phosphatidylcholine. Skin Pharmacol. Physiol. 2010, 23, 298–305. [Google Scholar] [CrossRef] [PubMed]
- Willimann, H.; Walde, P.; Luisi, P.L.; Gazzaniga, A.; Stroppolo, F. Lecithin Organogel as Matrix for Transdermal Transport of Drugs. J. Pharm. Sci. 1992, 81, 871–874. [Google Scholar] [CrossRef]
- Esposito, E.; Drechsler, M.; Huang, N.; Pavoni, G.; Cortesi, R.; Santonocito, D.; Puglia, C. Ethosomes and Organogels for Cutaneous Administration of Crocin. Biomed. Microdevices 2016, 18, 108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Raut, S.; Bhadoriya, S.S.; Uplanchiwar, V.; Mishra, V.; Gahane, A.; Jain, S.K. Lecithin Organogel: A Unique Micellar System for the Delivery of Bioactive Agents in the Treatment of Skin Aging. Acta Pharm. Sin. B 2012, 2, 8–15. [Google Scholar] [CrossRef] [Green Version]
- Dumortier, G.; Grossiord, J.L.; Agnely, F.; Chaumeil, J.C. A Review of Poloxamer 407 Pharmaceutical and Pharmacological Characteristics. Pharm. Res. 2006, 23, 2709–2728. [Google Scholar] [CrossRef]
- Russo, E.; Villa, C. Poloxamer Hydrogels for Biomedical Applications. Pharmaceutics 2019, 11, 671. [Google Scholar] [CrossRef] [Green Version]
- Fakhari, A.; Corcoran, M.; Schwarz, A. Thermogelling Properties of Purified Poloxamer 407. Heliyon 2017, 3, e00390. [Google Scholar] [CrossRef] [PubMed]
- Almeida, H.; Amaral, M.H.; Lobão, P.; Lobo, J.M.S. Pluronic® F-127 and Pluronic Lecithin Organogel (PLO): Main Features and Their Applications in Topical and Transdermal Administration of Drugs. J. Pharm. Pharm. Sci. 2012, 15, 592. [Google Scholar] [CrossRef] [Green Version]
- Pandey, M.; Belgamwar, V.; Gattani, S.; Surana, S.; Tekade, A. Pluronic Lecithin Organogel as a Topical Drug Delivery System. Drug Deliv. 2010, 17, 38–47. [Google Scholar] [CrossRef]
- Sicurella, M.; Sguizzato, M.; Cortesi, R.; Huang, N.; Simelière, F.; Montesi, L.; Marconi, P.; Esposito, E. Mangiferin-Loaded Smart Gels for HSV-1 Treatment. Pharmaceutics 2021, 13, 1323. [Google Scholar] [CrossRef] [PubMed]
- Hallan, S.S.; Sguizzato, M.; Mariani, P.; Cortesi, R.; Huang, N.; Simelière, F.; Marchetti, N.; Drechsler, M.; Ruzgas, T.; Esposito, E. Design and Characterization of Ethosomes for Transdermal Delivery of Caffeic Acid. Pharmaceutics 2020, 12, 740. [Google Scholar] [CrossRef]
- FDA Guidance for Industry: SUPAC-SS: Nonsterile Semisolid Dosage Forms; Scale-Up and Post-Approval Changes: Chemistry, Manufacturing and Controls; In-Vitro Release Testing and In Vivo Bioequivalence Documentation—ECA Academy. Available online: https://www.gmp-compliance.org/guidelines/gmp-guideline/fda-guidance-for-industry-supac-ss-nonsterile-semisolid-dosage-forms-scale-up-and-post-approval-changes-chemistry-manufacturing- (accessed on 22 July 2021).
- Popov, I.; Lewin, G. Antioxidative Homeostasis: Characterization by Means of Chemiluminescent Technique. In Methods in Enzymology; Elsevier: Amsterdam, The Netherlands, 1999; Volume 300, pp. 437–456. ISBN 978-0-12-182201-9. [Google Scholar]
- Nohynek, G.J.; Antignac, E.; Re, T.; Toutain, H. Safety Assessment of Personal Care Products/Cosmetics and Their Ingredients. Toxicol. Appl. Pharmacol. 2010, 243, 239–259. [Google Scholar] [CrossRef]
- Houston, D.M.J.; Bugert, J.J.; Denyer, S.P.; Heard, C.M. Potentiated Virucidal Activity of Pomegranate Rind Extract (PRE) and Punicalagin against Herpes Simplex Virus (HSV) When Co-Administered with Zinc (II) Ions, and Antiviral Activity of PRE against HSV and Aciclovir-Resistant HSV. PLoS ONE 2017, 12, e0179291. [Google Scholar] [CrossRef] [Green Version]
- Mariani, P.; Luzzati, V.; Delacroix, H. Cubic Phases of Lipid-Containing Systems. J. Mol. Biol. 1988, 204, 165–189. [Google Scholar] [CrossRef]
- Sguizzato, M.; Mariani, P.; Ferrara, F.; Drechsler, M.; Hallan, S.S.; Huang, N.; Simelière, F.; Khunti, N.; Cortesi, R.; Marchetti, N.; et al. Nanoparticulate Gels for Cutaneous Administration of Caffeic Acid. Nanomaterials 2020, 10, 961. [Google Scholar] [CrossRef] [PubMed]
- Giuliano, E.; Paolino, D.; Fresta, M.; Cosco, D. Mucosal Applications of Poloxamer 407-Based Hydrogels: An Overview. Pharmaceutics 2018, 10, 159. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Artzner, F.; Geiger, S.; Olivier, A.; Allais, C.; Finet, S.; Agnely, F. Interactions between Poloxamers in Aqueous Solutions: Micellization and Gelation Studied by Differential Scanning Calorimetry, Small Angle X-ray Scattering, and Rheology. Langmuir 2007, 23, 5085–5092. [Google Scholar] [CrossRef] [PubMed]
- Vargas, R.; Mariani, P.; Gulik, A.; Luzzati, V. Cubic Phases of Lipid-Containing Systems. J. Mol. Biol. 1992, 225, 137–145. [Google Scholar] [CrossRef]
- Rothwell, J.A.; Day, A.J.; Morgan, M.R.A. Experimental Determination of Octanol−Water Partition Coefficients of Quercetin and Related Flavonoids. J. Agric. Food Chem. 2005, 53, 4355–4360. [Google Scholar] [CrossRef]
- Ma, H.; Chen, H.; Sun, L.; Tong, L.; Zhang, T. Improving Permeability and Oral Absorption of Mangiferin by Phospholipid Complexation. Fitoterapia 2014, 93, 54–61. [Google Scholar] [CrossRef]
- Srinivas, K.; King, J.W.; Howard, L.R.; Monrad, J.K. Solubility and Solution Thermodynamic Properties of Quercetin and Quercetin Dihydrate in Subcritical Water. J. Food Eng. 2010, 100, 208–218. [Google Scholar] [CrossRef]
- Kumar, R.; Katare, O.P. Lecithin Organogels as a Potential Phospholipid-Structured System for Topical Drug Delivery: A Review. AAPS PharmSciTech 2005, 6, E298–E310. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mancuso, R.; Sicurella, M.; Agostini, S.; Marconi, P.; Clerici, M. Herpes Simplex Virus Type 1 and Alzheimer’s Disease: Link and Potential Impact on Treatment. Expert Rev. Anti-Infect. Ther. 2019, 17, 715–731. [Google Scholar] [CrossRef]
- F.D.A. Guidance for Industry: Transdermal and Topical Delivery Systems—Product Development and Quality Considerations. Available online: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/transdermal-and-topical-delivery-systems-product-development-and-quality-considerations (accessed on 11 December 2021).
- Prausnitz, M.R.; Langer, R. Transdermal Drug Delivery. Nat. Biotechnol. 2008, 26, 1261–1268. [Google Scholar] [CrossRef]






| Vehicle Composition (% w/w) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Component | OG | POL | POG | OG-QT | POL-QT | POG-QT | OG-MG | POL-MG | POG-MG |
| PC 1 | 15.60 | - | 4.68 | 15.60 | - | 4.68 | 15.60 | - | 4.68 |
| P-407 2 | - | 20.0 | 14.00 | - | 20.00 | 14.00 | - | 20.0 | 14.00 |
| IPP 3 | 82.51 | - | 24.82 | 82.46 | - | 24.82 | 82.46 | - | 24.82 |
| water | 1.44 | 80.0 | 56.50 | 1.44 | 79.95 | 56.45 | 1.44 | 79.95 | 56.45 |
| QT 4 | - | - | - | 0.05 | 0.05 | 0.05 | - | - | - |
| MG 5 | - | - | - | - | - | - | 0.05 | 0.05 | 0.05 |
| Vehicle | Tsol–gel 1 (°C) | Structure 2 | SAXS Repeat Distance (Å) 2 | WAXS Repeat Distance (Å) 2 |
|---|---|---|---|---|
| OG | 11.5 ± 0.1 16.4 ± 0.7 | Disordered micellar | - | 4.59 |
| POL | 20.8 ± 0.7 | Cubic (space group Q223) | 282.08 | 3.29 |
| POG | 16.4 ± 2.1 | Ordered micellar | 196.34 | 3.34–4.83 |
| Vehicles | F 1 ± s.d. (μg/cm2/h) | QT (mg/mL) | MG (mg/mL) | D 2 ± s.d. (cm/h) × 10−3 | Q7 3 ± s.d. (μg/cm2) | Reduction Ratio 4 |
|---|---|---|---|---|---|---|
| OG-QT | 2.84 ± 1.1 | 0.5 | - | 5.68 ± 2.2 | 20 ± 4 | 21.5 |
| POL-QT | 9.16 ± 2.7 | 0.5 | - | 18.32 ± 5.4 | 66 ± 11 | 6.6 |
| POG-QT | 5.42 ± 4.3 | 0.5 | - | 10.84 ± 8.6 | 39 ± 17 | 12.2 |
| SOL-QT | 61.06 ± 2.8 | 0.5 | - | 122.13 ± 5.6 | 403 ± 32 | - |
| OG-MG | 38.69 ± 6.8 | - | 0.5 | 77.38 ± 13.6 | 257.14 ± 38 | 1.96 |
| POL-MG | 17.64 ± 2.4 | - | 0.5 | 35.28 ± 4.8 | 128.57 ± 10 | 4.3 |
| POG-MG | 5.02 ± 1.1 | - | 0.5 | 10.04 ± 2.2 | 36.43 ± 4 | 15.11 |
| SOL-MG | 75.86 ± 12 | - | 0.5 | 151.72 ± 24 | 271.43 ± 23 | - |
| Vehicles | ACL (μmol TE/g) | Plaque Reduction (%) | |
|---|---|---|---|
| 1 h | 6 h | ||
| OG-QT | 4.52 ± 0.34 | 50.0 ± 1.0 | 50.0 ± 1.0 |
| POL-QT | 6.76 ± 0.14 | 47.5 ± 1.0 | 93.5 ± 0.75 |
| POG-QT | 4.80 ± 0.23 | 46.0 ± 0.75 | 80.0 ± 0.75 |
| SOL- QT | 3.82 ± 0.05 | 89.0 ± 1.0 | 76.0 ± 1.0 |
| OG-MG | 2.48 ± 0.02 | - | - |
| POL-MG | 0.87 ± 0.02 | 40.0 ± 1.7 | 94.0 ± 0.74 |
| POG-MG | 1.26 ± 0.06 | 40.0 ± 1.0 | 98.0 ± 0.62 |
| SOL-MG | 0.65 ± 0.04 | 40.0 ± 1.7 | 93.0 ± 0.74 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sicurella, M.; Sguizzato, M.; Mariani, P.; Pepe, A.; Baldisserotto, A.; Buzzi, R.; Huang, N.; Simelière, F.; Burholt, S.; Marconi, P.; et al. Natural Polyphenol-Containing Gels against HSV-1 Infection: A Comparative Study. Nanomaterials 2022, 12, 227. https://doi.org/10.3390/nano12020227
Sicurella M, Sguizzato M, Mariani P, Pepe A, Baldisserotto A, Buzzi R, Huang N, Simelière F, Burholt S, Marconi P, et al. Natural Polyphenol-Containing Gels against HSV-1 Infection: A Comparative Study. Nanomaterials. 2022; 12(2):227. https://doi.org/10.3390/nano12020227
Chicago/Turabian StyleSicurella, Mariaconcetta, Maddalena Sguizzato, Paolo Mariani, Alessia Pepe, Anna Baldisserotto, Raissa Buzzi, Nicolas Huang, Fanny Simelière, Sam Burholt, Peggy Marconi, and et al. 2022. "Natural Polyphenol-Containing Gels against HSV-1 Infection: A Comparative Study" Nanomaterials 12, no. 2: 227. https://doi.org/10.3390/nano12020227