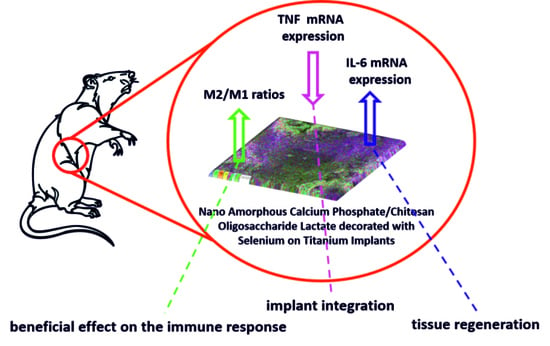
Immunomodulatory Effects Mediated by Nano Amorphous Calcium Phosphate/Chitosan Oligosaccharide Lactate Coatings Decorated with Selenium on Titanium Implants
Abstract
:1. Introduction
2. Materials and Methods
2.1. Synthesis
2.2. Animal Implantation
2.3. Isolation of RNA, Reverse Transcription and Real-Time Polymerase Chain Reaction (RT-PCR)
2.4. Data Display and Statistical Analysis
3. Results
In Vivo Study
4. Discussion
Results of In Vivo Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sarraf, M.; Rezvani Ghomi, E.; Alipour, S.; Ramakrishna, S.; Liana Sukiman, N. A State-of-the-Art Review of the Fabrication and Characteristics of Titanium and Its Alloys for Biomedical Applications. Bio-Des. Manuf. 2022, 5, 371–395. [Google Scholar] [CrossRef] [PubMed]
- Rack, H.J.; Qazi, J.I. Titanium Alloys for Biomedical Applications. Mater. Sci. Eng. C 2006, 26, 1269–1277. [Google Scholar] [CrossRef]
- Cook, S.D.; Thomas, K.A.; Kay, J.F.; Jarcho, M. Hydroxyapatite-Coated Titanium for Orthopedic Implant Applications. Clin. Orthop. Relat. Res. 1988, 232, 225–243. [Google Scholar] [CrossRef]
- Bose, S.; Tarafder, S.; Bandyopadhyay, A. 7-Hydroxyapatite Coatings for Metallic Implants. In Woodhead Publishing Series in Biomaterials; Mucalo, M.B.T., Ed.; Woodhead Publishing: Sawston, UK, 2015; pp. 143–157. ISBN 978-1-78242-033-0. [Google Scholar]
- Dorozhkin, S.V. Nanosized and Nanocrystalline Calcium Orthophosphates. Acta Biomater. 2010, 6, 715–734. [Google Scholar] [CrossRef]
- Wu, V.M.; Tang, S.; Uskoković, V. Calcium Phosphate Nanoparticles as Intrinsic Inorganic Antimicrobials: The Antibacterial Effect. ACS Appl. Mater. Interfaces 2018, 10, 34013–34028. [Google Scholar] [CrossRef]
- Combes, C.; Rey, C. Amorphous Calcium Phosphates: Synthesis, Properties and Uses in Biomaterials. Acta Biomater. 2010, 6, 3362–3378. [Google Scholar] [CrossRef]
- Besra, L.; Liu, M. A Review on Fundamentals and Applications of Electrophoretic Deposition (EPD). Prog. Mater. Sci. 2007, 52, 1–61. [Google Scholar] [CrossRef]
- Pantović Pavlović, M.R.; Stanojević, B.P.; Pavlović, M.M.; Mihailović, M.D.; Stevanović, J.S.; Panić, V.V.; Ignjatović, N.L. Anodizing/Anaphoretic Electrodeposition of Nano-Calcium Phosphate/Chitosan Lactate Multifunctional Coatings on Titanium with Advanced Corrosion Resistance, Bioactivity, and Antibacterial Properties. ACS Biomater. Sci. Eng. 2021, 7, 3088–3102. [Google Scholar] [CrossRef]
- Pantović Pavlović, M.R.; Pavlović, M.M. In Situ Synthesis and Characterization of Anaphoretic Multifunctional Coatings on Titanium with Advanced Properties. In Advances in Materials Science Research; Wythers, M.C., Ed.; Nova Science Publishers: New York, NY, USA, 2022; Volume 54, pp. 53–95. ISBN 979-8-88697-241-2. [Google Scholar]
- Eraković, S.; Janković, A.; Veljović, D.; Palcevskis, E.; Mitrić, M.; Stevanović, T.; Janaćković, D.; Mišković-Stanković, V. Corrosion Stability and Bioactivity in Simulated Body Fluid of Silver/Hydroxyapatite and Silver/Hydroxyapatite/Lignin Coatings on Titanium Obtained by Electrophoretic Deposition. J. Phys. Chem. B 2013, 117, 1633–1643. [Google Scholar] [CrossRef]
- Pantović Pavlović, M.R.; Eraković, S.G.; Pavlović, M.M.; Stevanović, J.S.; Panić, V.V.; Ignjatović, N.L. Anaphoretical/Oxidative Approach to the in-Situ Synthesis of Adherent Hydroxyapatite/Titanium Oxide Composite Coatings on Titanium. Surf. Coat. Technol. 2019, 358, 688–694. [Google Scholar] [CrossRef]
- Pantović Pavlović, M.R.; Pavlović, M.M.; Eraković, S.; Stevanović, J.S.; Panić, V.V.; Ignjatović, N. Simultaneous Anodization/Anaphoretic Electrodeposition Synthesis of Nano Calcium Phosphate/Titanium Oxide Composite Coatings Assisted with Chitosan Oligosaccharide Lactate. Mater. Lett. 2020, 261, 127121. [Google Scholar] [CrossRef]
- Lotsari, A.; Rajasekharan, A.K.; Halvarsson, M.; Andersson, M. Transformation of Amorphous Calcium Phosphate to Bone-like Apatite. Nat. Commun. 2018, 9, 4170. [Google Scholar] [CrossRef] [PubMed]
- Jin, B.; Liu, Z.; Shao, C.; Chen, J.; Liu, L.; Tang, R.; De Yoreo, J.J. Phase Transformation Mechanism of Amorphous Calcium Phosphate to Hydroxyapatite Investigated by Liquid-Cell Transmission Electron Microscopy. Cryst. Growth Des. 2021, 21, 5126–5134. [Google Scholar] [CrossRef]
- Kumar, M.N.V.R.; Muzzarelli, R.A.A.; Muzzarelli, C.; Sashiwa, H.; Domb, A.J. Chitosan Chemistry and Pharmaceutical Perspectives. Chem. Rev. 2004, 104, 6017–6084. [Google Scholar] [CrossRef]
- Riaz Rajoka, M.S.; Mehwish, H.M.; Wu, Y.; Zhao, L.; Arfat, Y.; Majeed, K.; Anwaar, S. Chitin/Chitosan Derivatives and Their Interactions with Microorganisms: A Comprehensive Review and Future Perspectives. Crit. Rev. Biotechnol. 2020, 40, 365–379. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Xia, X.; Guo, M.; Jiang, Y.; Li, Y.; Zhang, Z.; Liu, S.; Li, H.; Liang, C.; Wang, H. Biological and Antibacterial Properties of the Micro-Nanostructured Hydroxyapatite/Chitosan Coating on Titanium. Sci. Rep. 2019, 9, 14052. [Google Scholar] [CrossRef]
- Pawlik, A.; Rehman, M.A.U.; Nawaz, Q.; Bastan, F.E.; Sulka, G.D.; Boccaccini, A.R. Fabrication and Characterization of Electrophoretically Deposited Chitosan-Hydroxyapatite Composite Coatings on Anodic Titanium Dioxide Layers. Electrochim. Acta 2019, 307, 465–473. [Google Scholar] [CrossRef]
- Galvão, R.A.; de Santa-Cruz, L.A.; Barreto, P.B.; dos Santos Horta, M.K.; de Andrade, A.M.H.; Moura, F.J.; Aguilar, M.S.; Peripolli, S.B.; de Campos, J.B.; de Souza Arruda, I.R.; et al. Electrochemical Single-Step Obtention and Characterization of a Biomimetic TiO2-HA NTs Covered by Chitosan. J. Mater. Res. 2019, 34, 1868–1878. [Google Scholar] [CrossRef]
- Stevanović, M.; Đošić, M.; Janković, A.; Kojić, V.; Vukašinović-Sekulić, M.; Stojanović, J.; Odović, J.; Crevar Sakač, M.; Rhee, K.Y.; Mišković-Stanković, V. Gentamicin-Loaded Bioactive Hydroxyapatite/Chitosan Composite Coating Electrodeposited on Titanium. ACS Biomater. Sci. Eng. 2018, 4, 3994–4007. [Google Scholar] [CrossRef]
- Yan, L.; Xiang, Y.; Yu, J.; Wang, Y.; Cui, W. Fabrication of Antibacterial and Antiwear Hydroxyapatite Coatings via In Situ Chitosan-Mediated Pulse Electrochemical Deposition. ACS Appl. Mater. Interfaces 2017, 9, 5023–5030. [Google Scholar] [CrossRef]
- Chandorkar, Y.; K, R.; Basu, B. The Foreign Body Response Demystified. ACS Biomater. Sci. Eng. 2019, 5, 19–44. [Google Scholar] [CrossRef] [PubMed]
- Lebaudy, E.; Fournel, S.; Lavalle, P.; Vrana, N.E.; Gribova, V. Recent Advances in Antiinflammatory Material Design. Adv. Healthc. Mater. 2021, 10, 2001373. [Google Scholar] [CrossRef] [PubMed]
- Bauza-Mayol, G.; Quintela, M.; Brozovich, A.; Hopson, M.; Shaikh, S.; Cabrera, F.; Shi, A.; Niclot, F.B.; Paradiso, F.; Combellack, E.; et al. Biomimetic Scaffolds Modulate the Posttraumatic Inflammatory Response in Articular Cartilage Contributing to Enhanced Neoformation of Cartilaginous Tissue In Vivo. Adv. Healthc. Mater. 2022, 11, 2101127. [Google Scholar] [CrossRef]
- Zhang, B.; Su, Y.; Zhou, J.; Zheng, Y.; Zhu, D. Toward a Better Regeneration through Implant-Mediated Immunomodulation: Harnessing the Immune Responses. Adv. Sci. 2021, 8, 2100446. [Google Scholar] [CrossRef]
- Qi, H.; Chen, Q.; Ren, H.; Wu, X.; Liu, X.; Lu, T. Electrophoretic Deposition of Dexamethasone-Loaded Gelatin Nanospheres/Chitosan Coating and Its Dual Function in Anti-Inflammation and Osteogenesis. Colloids Surf. B Biointerfaces 2018, 169, 249–256. [Google Scholar] [CrossRef] [PubMed]
- Chang, S.-H.; Lin, Y.-Y.; Wu, G.-J.; Huang, C.-H.; Tsai, G.J. Effect of Chitosan Molecular Weight on Anti-Inflammatory Activity in the RAW 264.7 Macrophage Model. Int. J. Biol. Macromol. 2019, 131, 167–175. [Google Scholar] [CrossRef]
- Razaghi, A.; Poorebrahim, M.; Sarhan, D.; Björnstedt, M. Selenium Stimulates the Antitumour Immunity: Insights to Future Research. Eur. J. Cancer 2021, 155, 256–267. [Google Scholar] [CrossRef]
- Huang, Z.; Rose, A.H.; Hoffmann, P.R. The Role of Selenium in Inflammation and Immunity: From Molecular Mechanisms to Therapeutic Opportunities. Antioxid. Redox Signal. 2011, 16, 705–743. [Google Scholar] [CrossRef]
- Pantovc Pavlovic, M.R.; Pavlovic, M.M.; Kovacina, J.N.; Stanojevic, B.P.; Stevanovic, J.S.; Panic, V.V.; Ignjatovic, N.L. Cytotoxicity of Amorphous Calcium Phosphate Multifunctional Composite Coatings on Titanium Obtained by in Situ Anodization/Anaphoretic Deposition. J. Serbian Chem. Soc. 2021, 86, 555–559. [Google Scholar] [CrossRef]
- ISO 10993-1:2018; Biological Evaluation of Medical Devices—Part 1: Evaluation and Testing within a Risk Management Process. ISO: Geneva, Switzerland. Available online: https://www.iso.org/standard/68936.html (accessed on 6 December 2022).
- Muhamed, J.; Revi, D.; Rajan, A.; Geetha, S.; Anilkumar, T. V Biocompatibility and Immunophenotypic Characterization of a Porcine Cholecyst-Derived Scaffold Implanted in Rats. Toxicol. Pathol. 2015, 43, 536–545. [Google Scholar] [CrossRef] [PubMed]
- Muhamed, J.; Revi, D.; Rajan, A.; Anilkumar, T.V. Comparative Local Immunogenic Potential of Scaffolds Prepared from Porcine Cholecyst, Jejunum, and Urinary Bladder in Rat Subcutaneous Model. J. Biomed. Mater. Res. B Appl. Biomater. 2015, 103, 1302–1311. [Google Scholar] [CrossRef] [PubMed]
- Barbeck, M.; Alkildani, S.; Mandlule, A.; Radenković, M.; Najman, S.; Stojanović, S.; Jung, O.; Ren, Y.; Cai, B.; Görke, O.; et al. In Vivo Analysis of the Immune Response to Strontium- and Copper-Doped Bioglass. In Vivo 2022, 36, 2149–2165. [Google Scholar] [CrossRef] [PubMed]
- Lužajić Božinovski, T.; Todorović, V.; Milošević, I.; Prokić, B.B.; Gajdov, V.; Nešović, K.; Mišković-Stanković, V.; Marković, D. Macrophages, the Main Marker in Biocompatibility Evaluation of New Hydrogels after Subcutaneous Implantation in Rats. J. Biomater. Appl. 2022, 36, 1111–1125. [Google Scholar] [CrossRef]
- Santos, J.M.; Coelho, C.M.; Sequeira, D.B.; Marques, J.A.; Pereira, J.F.; Sousa, V.; Palma, P.J.; Santos, A.C. Subcutaneous Implantation Assessment of New Calcium-Silicate Based Sealer for Warm Obturation. Biomedicines 2021, 9, 24. [Google Scholar] [CrossRef]
- Hwang, Y.-J.; Choi, Y.-S.; Hwang, Y.-H.; Cho, H.-W.; Lee, D.-G. Biocompatibility and Biological Corrosion Resistance of Ti–39Nb–6Zr+0.45Al Implant Alloy. J. Funct. Biomater. 2021, 12, 9. [Google Scholar] [CrossRef]
- Crawford, L.; Wyatt, M.; Bryers, J.; Ratner, B. Biocompatibility Evolves: Phenomenology to Toxicology to Regeneration. Adv. Healthc. Mater. 2021, 10, e2002153. [Google Scholar] [CrossRef] [PubMed]
- Abbas, A.K.; Lichtman, A.H.; Pillai, S.; Baker, D.L. Cellular and Molecular Immunology, 10th ed.; Elsevier Saunders: Philadelphia, PA, USA, 2022. [Google Scholar]
- Trivedi, M.K.; Sethi, K.K.; Panda, P.; Jana, S. Sodyum Selenat’ın XRD, PSD, DSC, TGA/DTG, UV-VIS ve FT-IR Yöntemleri Ile Fizikokimyasal, Termal ve Spektroskopik Karakterizasyonu. Marmara Pharm. J. 2017, 21, 311. [Google Scholar] [CrossRef]
- Nakamoto, K. Infrared and Raman Spectra of Inorganic and Coordination Compounds. In Handbook of Vibrational Spectroscopy, 6th ed.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2009. [Google Scholar]
- Saadi, A.; Dalir-Naghadeh, B.; Asri-Rezaei, S.; Anassori, E. Platelet Selenium Indices as Useful Diagnostic Surrogate for Assessment of Selenium Status in Lambs: An Experimental Comparative Study on the Efficacy of Sodium Selenite vs. Selenium Nanoparticles. Biol. Trace Elem. Res. 2020, 194, 401–409. [Google Scholar] [CrossRef]
- Ruiz Fresneda, M.A.; Delgado Martín, J.; Gómez Bolívar, J.; Fernández Cantos, M.V.; Bosch-Estévez, G.; Martínez Moreno, M.F.; Merroun, M.L. Green Synthesis and Biotransformation of Amorphous Se Nanospheres to Trigonal 1D Se Nanostructures: Impact on Se Mobility within the Concept of Radioactive Waste Disposal. Environ. Sci. Nano 2018, 5, 2103–2116. [Google Scholar] [CrossRef]
- Kzhyshkowska, J.; Gudima, A.; Riabov, V.; Dollinger, C.; Lavalle, P.; Vrana, N.E. Macrophage Responses to Implants: Prospects for Personalized Medicine. J. Leukoc. Biol. 2015, 98, 953–962. [Google Scholar] [CrossRef]
- Hachim, D.; LoPresti, S.T.; Rege, R.D.; Umeda, Y.; Iftikhar, A.; Nolfi, A.L.; Skillen, C.D.; Brown, B.N. Distinct Macrophage Populations and Phenotypes Associated with IL-4 Mediated Immunomodulation at the Host Implant Interface. Biomater. Sci. 2020, 8, 5751–5762. [Google Scholar] [CrossRef] [PubMed]
- Perala, D.G.; Chapman, R.J.; Gelfand, J.A.; Callahan, M.V.; Adams, D.F.; Lie, T. Relative Production of IL-1β and TNFα by Mononuclear Cells After Exposure to Dental Implants. J. Periodontol. 1992, 63, 426–430. [Google Scholar] [CrossRef] [PubMed]
- Eger, M.; Hiram-Bab, S.; Liron, T.; Sterer, N.; Carmi, Y.; Kohavi, D.; Gabet, Y. Mechanism and Prevention of Titanium Particle-Induced Inflammation and Osteolysis. Front. Immunol. 2018, 9, 2963. [Google Scholar] [CrossRef]
- Johnson, B.Z.; Stevenson, A.W.; Prêle, C.M.; Fear, M.W.; Wood, F.M. The Role of IL-6 in Skin Fibrosis and Cutaneous Wound Healing. Biomedicines 2020, 8, 101. [Google Scholar] [CrossRef]
- Park, C.; Lee, S.-W.; Kim, J.; Song, E.-H.; Jung, H.-D.; Park, J.-U.; Kim, H.-E.; Kim, S.; Jang, T.-S. Reduced Fibrous Capsule Formation at Nano-Engineered Silicone Surfaces via Tantalum Ion Implantation. Biomater. Sci. 2019, 7, 2907–2919. [Google Scholar] [CrossRef] [PubMed]
- Cornelini, R.; Rubini, C.; Fioroni, M.; Favero, G.A.; Strocchi, R.; Piattelli, A. Transforming Growth Factor-Beta 1 Expression in the Peri-Implant Soft Tissues of Healthy and Failing Dental Implants. J. Periodontol. 2003, 74, 446–450. [Google Scholar] [CrossRef] [PubMed]
- Emami, E.; de Grandmont, P.; Menassa, M.; Audy, N.; Durand, R. Anti-Vascular Endothelial Growth Factors as a Potential Risk for Implant Failure: A Clinical Report. Case Rep. Med. 2020, 2020, 6141493. [Google Scholar] [CrossRef] [PubMed]
- Cornelini, R.; Artese, L.; Rubini, C.; Fioroni, M.; Ferrero, G.; Santinelli, A.; Piattelli, A. Vascular Endothelial Growth Factor and Microvessel Density around Healthy and Failing Dental Implants. Int. J. Oral Maxillofac. Implants 2001, 16, 389–393. [Google Scholar]
- Guang, M.; Huang, B.; Yao, Y.; Zhang, L.; Yang, B.; Gong, P. Effects of Vascular Endothelial Growth Factor on Osteoblasts around Dental Implants in Vitro and in Vivo. J. Oral Sci. 2017, 59, 215–223. [Google Scholar] [CrossRef]





| Gene | Forward | Reverse |
|---|---|---|
| β-actin * | 5′−CCCTGGCTCCTAGCACCAT-3′ | 5′-GAGCCACCAATCCACACAGA-3′ |
| IL-1β | 5′-CACCTCTCAAGCAGAGCA-3′ | 5′-GGGTTCCATGGTGAAGTCAAC-3′ |
| IL-6 | 5′-CCCTTCAGGAACAGCTATGA-3′ | 5′-TGTCAACAACATCAGTCCCAAG-3′ |
| TNF | 5′-TCGAGTGACAAGCCCGTAGC-3′ | 5′-CTCAGCCACTCCAGCTGCTC-3′ |
| iNOS | 5′-TTCCCATCGCTCCGCTG-3′ | 5′-CCGGAGCTGTAGCACTGCA-3′ |
| Arg1 | 5′-TGGACCCTGGGGAACACTAT-3′ | 5′- GTAGCCGGGGTGAATACTGG-3′ |
| VEGF | 5′-GGGCCTCTGAAACCATGAACT-3′ | 5′-ACGTCCATGAACTTCACCACTTC-3′ |
| TGF-β | 5′-CCCTGCCCCTACATTTGGA-3′ | 5′-ACGGTGATGCGGAAGCAC-3′ |
| Elemental Analysis, at.% | C | O | Na | P | Ca | Ti | Se | Total |
|---|---|---|---|---|---|---|---|---|
| Hybrid ACP/ChOL/Se | 9.32 | 28.10 | 2.11 | 3.64 | 6.10 | 34.98 | 15.75 | 100.00 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pantović Pavlović, M.R.; Ignjatović, N.L.; Panić, V.V.; Mirkov, I.I.; Kulaš, J.B.; Malešević, A.L.; Pavlović, M.M. Immunomodulatory Effects Mediated by Nano Amorphous Calcium Phosphate/Chitosan Oligosaccharide Lactate Coatings Decorated with Selenium on Titanium Implants. J. Funct. Biomater. 2023, 14, 227. https://doi.org/10.3390/jfb14040227
Pantović Pavlović MR, Ignjatović NL, Panić VV, Mirkov II, Kulaš JB, Malešević AL, Pavlović MM. Immunomodulatory Effects Mediated by Nano Amorphous Calcium Phosphate/Chitosan Oligosaccharide Lactate Coatings Decorated with Selenium on Titanium Implants. Journal of Functional Biomaterials. 2023; 14(4):227. https://doi.org/10.3390/jfb14040227
Chicago/Turabian StylePantović Pavlović, Marijana R., Nenad L. Ignjatović, Vladimir V. Panić, Ivana I. Mirkov, Jelena B. Kulaš, Anastasija Lj. Malešević, and Miroslav M. Pavlović. 2023. "Immunomodulatory Effects Mediated by Nano Amorphous Calcium Phosphate/Chitosan Oligosaccharide Lactate Coatings Decorated with Selenium on Titanium Implants" Journal of Functional Biomaterials 14, no. 4: 227. https://doi.org/10.3390/jfb14040227