Photoplethysmography Enabled Wearable Devices and Stress Detection: A Scoping Review
Abstract
:1. Introduction
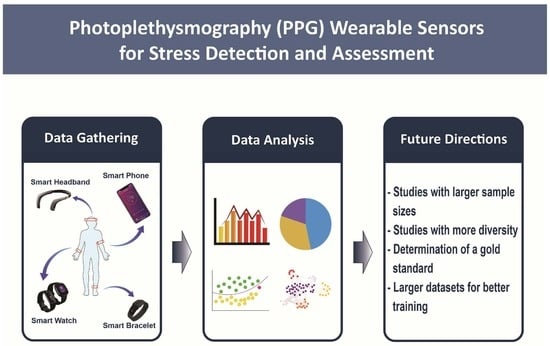
- Report on recent achievements and advancements in mental health monitoring and stress detection using non-invasive wearable devices equipped with PPG sensors.
- Identify the existing limitations and gaps in detection of stress using PPG-based wearable devices.
- Provide direction for future research in this area.
2. Methods
- The trials could be in clinical or real-life environments.
- Any wearable device type was included.
- The wearable device used PPG-based technologies to assess mental health, although additional peripheral sensors were permitted.
- The area of mental health included mental health, mental disorders, psychological distress, stress, anxiety, generalized anxiety disorders, depression, or major depressive disorders.
- The study was published between January 2017 and April 2021.
- The study evaluated mental health in humans.
- The study was published in English.
- The study was not a review paper.
- The study was not an abstract paper or conference paper with no full text available.
- The study did not collect data by placing a finger on a camera.
3. Results
3.1. Brief Summary of Anxiety and Depression-Related Papers
3.2. Stress Detection and PPG
3.3. Ground-Truth Methods
3.4. Common Methodologies for Detecting Stress from PPG
3.4.1. Hardware-Based Methodologies
3.4.2. Machine Learning-Based Methods
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ritchie, H.; Roser, M. Mental Health. Available online: https://ourworldindata.org/mental-health (accessed on 20 May 2022).
- Definition of Stress. Available online: https://www.stress.org/daily-life (accessed on 20 May 2022).
- The Three Types of Stress. Available online: https://www.psychologytoday.com/us/blog/open-gently/201812/the-three-types-stress#:~:text=According%20to%20the%20American%20Psychological,Acute%20Stress (accessed on 20 May 2022).
- Dai, X.; Ding, Y. Mental Health Monitoring Based on Multiperception Intelligent Wearable Devices. Contrast Media Mol. Imaging 2021, 2021, 8307576. [Google Scholar] [CrossRef]
- Knight, S.; Lipoth, J.; Namvari, M.; Gu, C.; Hedayati Ch, M.; Syed-Abdul, S.; Spiteri, R.J. The Accuracy of Wearable Photoplethysmography Sensors for Telehealth Monitoring: A Scoping Review. Telemed e-Health 2022, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Waxenbaum, J.A.R.V.; Varacallo, M. Anatomy, Autonomic Nervous System; StatPearls Publishing: Tampa, FL, USA, 2021. [Google Scholar]
- Celka, P.; Charlton, P.H.; Farukh, B.; Chowienczyk, P.; Alastruey, J. Influence of mental stress on the pulse wave features of photoplethysmograms. Healthc. Technol. Lett. 2019, 7, 7–12. [Google Scholar] [CrossRef] [PubMed]
- Castaneda, D.; Esparza, A.; Ghamari, M.; Soltanpur, C.; Nazeran, H. A review on wearable photoplethysmography sensors and their potential future applications in health care. Int. J. Biosens. Bioelectron. 2018, 4, 195–202. [Google Scholar] [CrossRef] [Green Version]
- Perna, G.; Riva, A.; Defillo, A.; Sangiorgio, E.; Nobile, M.; Caldirola, D. Heart rate variability: Can it serve as a marker of mental health resilience? J. Affect. Disord. 2020, 263, 754–761. [Google Scholar] [CrossRef] [PubMed]
- Umair, M.; Chalabianloo, N.; Sas, C.; Ersoy, C. HRV and Stress: A Mixed-Methods Approach for Comparison of Wearable Heart Rate Sensors for Biofeedback. IEEE Access 2021, 9, 14005–14024. [Google Scholar] [CrossRef]
- Kucera, M.; Wolfová, K.; Cermakova, P. Changes in depressive symptoms of older adults in the Czech Republic. J. Affect. Disord. 2020, 261, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Hao, T.; Chang, H.; Ball, M.; Lin, K.; Zhu, X. cHRV Uncovering Daily Stress Dynamics Using Bio-Signal from Consumer Wearables. Stud. Health Technol. Inform. 2017, 245, 98–102. [Google Scholar] [PubMed]
- Park, J.; Kim, J.; Kim, S. A Study on the Development of a Day-to-Day Mental Stress Monitoring System using Personal Physiological Data. In Proceedings of the 2018 18th International Conference on Control, Automation and Systems (ICCAS), PyeongChang, Korea, 17–20 October 2018; pp. 900–903. [Google Scholar]
- Zangróniz, R.; Martínez-Rodrigo, A.; López, M.T.; Pastor, J.M.; Fernández-Caballero, A. Estimation of Mental Distress from Photoplethysmography. Appl. Sci. 2018, 8, 69. [Google Scholar] [CrossRef] [Green Version]
- Correia, B.; Dias, N.; Costa, P.; Pêgo, J.M. Validation of a Wireless Bluetooth Photoplethysmography Sensor Used on the Earlobe for Monitoring Heart Rate Variability Features during a Stress-Inducing Mental Task in Healthy Individuals. Sensors 2020, 20, 3905. [Google Scholar] [CrossRef]
- Singstad, B.-J.; Azulay, N.; Bjurstedt, A.; Bjørndal, S.S.; Drageseth, M.F.; Engeset, P.; Eriksen, K.; Gidey, M.Y.; Granum, E.O.; Greaker, M.G.; et al. Estimation of Heart Rate Variability from Finger Photoplethysmography During Rest, Mild Exercise and Mild Mental Stress. J. Electr. Bioimpedance 2021, 12, 89–102. [Google Scholar] [CrossRef]
- Baek, H.J.; Cho, J. Novel heart rate variability index for wrist-worn wearable devices subject to motion artifacts that complicate measurement of the continuous pulse interval. Physiol. Meas. 2019, 40, 105010. [Google Scholar] [CrossRef]
- Tazarv, A.; Labbaf, S.; Reich, S.M.; Dutt, N.; Rahmani, A.M.; Levorato, M. Personalized Stress Monitoring using Wearable Sensors in Everyday Settings. In Proceedings of the 43rd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Glasgow, UK, 1–5 November 2021; pp. 7332–7335. [Google Scholar]
- Chauhan, U.; Reithinger, N.; Mackey, J.R. Real-time stress assessment through PPG sensor for VR biofeedback. In Proceedings of the 20th International Conference on Multimodal Interaction: Adjunct, Boulder, CO, USA, 16–20 October 2018; p. 5. [Google Scholar]
- Rashid, N.; Chen, L.; Dautta, M.; Jimenez, A.; Tseng, P.; Faruque, M.A.A. Feature Augmented Hybrid CNN for Stress Recognition Using Wrist-based Photoplethysmography Sensor. In Proceedings of the 2021 43rd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Guadalajara, Mexico, 1–5 November 2021; pp. 2374–2377. [Google Scholar]
- Chuenchom, T.; Tretriluxana, S.; Chitsakul, K. Changes in Pulse Transit Time During Psychological Stress Test. In Proceedings of the 2018 International Electrical Engineering Congress (iEECON), Krabi, Thailand, 7–9 March 2018; pp. 1–4. [Google Scholar]
- Tomita, Y.; Mitsukura, Y. An Earbud-Based Photoplethysmography and its Application. Electron. Commun. Jpn. 2018, 101, 32–38. [Google Scholar] [CrossRef] [Green Version]
- Golgouneh, A.; Tarvirdizadeh, B. Fabrication of a portable device for stress monitoring using wearable sensors and soft computing algorithms. Neural Comput. Appl. 2020, 32, 7515–7537. [Google Scholar] [CrossRef]
- Nath, R.K.; Thapliyal, H. Wearable Health Monitoring System for Older Adults in a Smart Home Environment. In Proceedings of the 2021 IEEE Computer Society Annual Symposium on VLSI (ISVLSI), Tampa, FL, USA, 7–9 July 2021; pp. 390–395. [Google Scholar]
- Han, H.J.; Labbaf, S.; Borelli, J.L.; Dutt, N.; Rahmani, A.M. Objective stress monitoring based on wearable sensors in everyday settings. J. Med. Eng. Technol. 2020, 44, 177–189. [Google Scholar] [CrossRef]
- Arsalan, A.; Majid, M. Human stress classification during public speaking using physiological signals. Comput. Biol. Med. 2021, 133, 104377. [Google Scholar] [CrossRef] [PubMed]
- Akbar, F.; Mark, G.; Pavlidis, I.; Gutierrez-Osuna, R. An Empirical Study Comparing Unobtrusive Physiological Sensors for Stress Detection in Computer Work. Sensors 2019, 19, 3766. [Google Scholar] [CrossRef] [Green Version]
- Can, Y.S.; Chalabianloo, N.; Ekiz, D.; Ersoy, C. Continuous Stress Detection Using Wearable Sensors in Real Life: Algorithmic Programming Contest Case Study. Sensors 2019, 19, 1849. [Google Scholar] [CrossRef] [Green Version]
- Choi, M.; Koo, G.; Seo, M.; Kim, S.W. Wearable Device-Based System to Monitor a Driver’s Stress, Fatigue, and Drowsiness. IEEE Trans. Instrum. Meas. 2018, 67, 634–645. [Google Scholar] [CrossRef]
- Gurel, N.Z.; Jung, H.; Hersek, S.; Inan, O.T. Fusing Near-Infrared Spectroscopy With Wearable Hemodynamic Measurements Improves Classification of Mental Stress. IEEE Sens. J. 2019, 19, 8522–8531. [Google Scholar] [CrossRef] [PubMed]
- Sheridan, D.C.; Baker, S.; Dehart, R.; Lin, A.; Hansen, M.; Tereshchenko, L.G.; Le, N.; Newgard, C.D.; Nagel, B. Heart Rate Variability and Its Ability to Detect Worsening Suicidality in Adolescents: A Pilot Trial of Wearable Technology. Psychiatry Investig. 2021, 18, 928–935. [Google Scholar] [CrossRef]
- Beh, W.K.; Wu, Y.H.; Wu, A.Y.A. Robust PPG-based Mental Workload Assessment System using Wearable Devices. IEEE J. Biomed. Health Inform. 2021. [Google Scholar] [CrossRef] [PubMed]
- Cakmak, A.S.; Alday, E.A.P.; Da Poian, G.; Rad, A.B.; Metzler, T.J.; Neylan, T.C.; House, S.L.; Beaudoin, F.L.; An, X.; Stevens, J.S.; et al. Classification and Prediction of Post-Trauma Outcomes Related to PTSD Using Circadian Rhythm Changes Measured via Wrist-Worn Research Watch in a Large Longitudinal Cohort. IEEE J. Biomed. Health Inform. 2021, 25, 2866–2876. [Google Scholar] [CrossRef]
- Schmidt, P.; Reiss, A.; Duerichen, R.; Marberger, C.; Laerhoven, K.V. Introducing WESAD, a Multimodal Dataset for Wearable Stress and Affect Detection. In Proceedings of the 20th ACM International Conference on Multimodal Interaction, Boulder, CO, USA, 16–20 October 2018; pp. 400–408. [Google Scholar]
- Davis, A.K.; Maney, D.L.; Maerz, J.C. The use of leukocyte profiles to measure stress in vertebrates: A review for ecologists. Funct. Ecol. 2008, 22, 760–772. [Google Scholar] [CrossRef]
- Depression. Available online: https://www.who.int/news-room/fact-sheets/detail/depression (accessed on 20 May 2022).
- Campo, I.d.; Echanobe, J.; Bosque, G.; Tarela, J.M. Efficient Hardware/Software Implementation of an Adaptive Neuro-Fuzzy System. IEEE Trans. Fuzzy Syst. 2008, 16, 761–778. [Google Scholar] [CrossRef]
- Ueafuea, K.; Boonnag, C.; Sudhawiyangkul, T.; Leelaarporn, P.; Gulistan, A.; Chen, W.; Mukhopadhyay, S.C.; Wilaiprasitporn, T.; Piyayotai, S. Potential Applications of Mobile and Wearable Devices for Psychological Support During the COVID-19 Pandemic: A Review. IEEE Sens. J. 2021, 21, 7162–7178. [Google Scholar] [CrossRef]

| Nomenclature | Referred To | Nomenclature | Referred To |
|---|---|---|---|
| ACC | Accelerometer | PASAT | Paced Auditory Serial Addition Test |
| ANN | Artificial Neural Network | PAT | Pulse Arrival Time |
| ANS | Autonomic Nervous System | PCA | Principal Component Analysis |
| AUC | Area Under the Curve | PEP | Pre-ejection Period |
| BVP | Blood Volume Pulse | PFC | Prefrontal Cortex |
| CNN | Convolutional Neural Network | PNS | Parasympathetic nervous system |
| CSSRS | Columbia Suicide Severity Scale | PP | Perinasal Perspiration |
| DBP | Diastolic Blood Pressure | PPG | Photoplethysmography |
| DT | Decision Tree | PRV | Positive Predictive Value |
| DWT | Discrete Wavelet Transform | PSS | Perceived Stress Scale |
| ECG | Electrocardiography | PTSD | Post-Traumatic Stress Disorder |
| EDA | Electrodermal Activity | PTT | Pulse Transit Time |
| EEG | Electroencephalogram | RF | Random Forest |
| GSR | Galvanic Skin Response | RR | Respiratory Rate |
| HF | High Frequency | SBP | Systolic Blood Pressure |
| HR | Heart Rate | SC | Skin Conductance |
| HRV | Heart rate Variability | SCG | Seismocardiogram |
| IAPS | International Affective Picture System | SCWT | Stroop Color-Word Test |
| IBI | Interbeat Interval | SFFS | Sequential Forward F Selection |
| kNN | k-Nearest Neighbors | SI | Stress Index |
| LDA | Linear Discriminant Analysis | SNS | Sympathetic Nervous System |
| LR | Logistic Regression | ST | Skin Temperature |
| MDD | Major Depressive Disorder | SVM | Support Vector Machine |
| ML | Machine Learning | TNR | True Negative Rate |
| Study | Study Type | Sample Size | Average Age of Participants (Years) | Medical Condition |
|---|---|---|---|---|
| [12] | Clinical | 12 | NR | Healthy |
| [13] | Real Life | 8 | 21–25 | Individuals with no history of cardiac diseases |
| [14] | Clinical | 45 | 20 to 28 | Healthy |
| [15] | Clinical | 18 | 31.1 | Healthy |
| [16] | Clinical | 21 | 26.3 | NR |
| [17] | Clinical and Real Life | Stress study: 15 Real Life study: 5 | NR | NR |
| [18] | Real Life | 14 | NR | NR |
| [19] | Clinical | 10 | 30–58 | NR |
| [20] | Clinical | 15 | NR (WESAD database) | NR |
| [21] | Clinical | 6 | NR (college students) | Healthy |
| [22] | Clinical | 1 | A male in his 20′s | NR |
| [7] | Clinical | 10 | 23–31 | Healthy |
| [23] | Clinical | 37–RCDAT dataset | 24–27 | Healthy |
| [24] | Clinical | 40 | 73.63 | Healthy |
| [25] | Clinical | control group:17 real-life setting: 1 | 20–27 | NR |
| [26] | Real Life | 40 | 24.85 | Healthy |
| [27] | Clinical | 61 | 18 to 54 (23.75) | NR |
| [28] | Real Life | 21 | NR | NR |
| [29] | Clinical | 26 | Males: 20–32 Females: 28–31 | Healthy |
| [30] | Clinical | 16 | 26.7 | Healthy |
| [31] | Clinical | 51 | 13–19 | Suicidal adolescent patients |
| [32] | Clinical | 31–CLAS dataset 19–MAUS dataset | NR | NR |
| [33] | Real Life | 1618–AURORA dataset | 18–75 | Individuals experienced traumatic events |
| Study | Sensor (Location) | Stress Signal | Stress Test | # of Classes | Ground-Truth Method |
|---|---|---|---|---|---|
| [12] | PPG (wristband) | HRV | Non-trivial arithmetic task | 3 (Baseline, Stress, Recovery) | Perceived stress level (PSL) 0–10 |
| [13] | PPG (wristband) | HRV | Real Life | NR (Stress level) | PSS |
| [14] | PPG (wristband) | HRV | International Affective Picture System (IAPS) | 2 (Distress, Calmness) | NR |
| [15] | PPG (earlobe) | HRV | Computerized SCWT | 2 (Stress, Not-stress) | ECG |
| [16] | PPG (finger clip) | HRV | Game (python-based program LARA) | 2 (Stress, Not-stress) | ECG |
| [17] | PPG (wristband) | HRV | Modified TSST and Real Life | NA (baseline, Speech, Recovery) | Stress study: ECG Real-life: Polar H7 (ECG) |
| [18] | PPG (wristwatch) | HRV, HR | Real Life | 2 (Stress, Non-stress) | Self-reported questionnaire |
| [19] | PPG (earlobe) | HRV | Paced Auditory Serial Addition Test (PASAT) | 3 (Rest, PASAT, Rest) | NR |
| [20] | PPG (wristwatch) | BVP | NR | 3 (Baseline, Stress, Amusement) 2 (Stress, Non-stress) | WESAD dataset |
| [21] | PPG (finger clip) | PTT | Modified TSST | NA (Baseline, Speech, Math, Recovery) | ECG |
| [22] | PPG (earbud) | Pulse Wave | Two-digit addition problems | NA (Stress level) | NR |
| [7] | PPG (wristband, upper arm, temporal region) | Pulse Wave | Stroop tests | 5 (Baseline, Stroop1, Relaxation, Stroop 2, Recovery) | BP and Visual Analogue Scale (VAS) questionnaire |
| [23] | PPG, GSR (all wristband and finger clip) | HRV, Cardiotach | Audible and visual clips | 3 (Relaxing, Normal, Stressful) | Stress state questionnaire on a 0–4 scale |
| [24] | PPG, EDA, ST (all wristband) | BVP, IBI, EDA, ST | TSST | 2 (Stress, Not-stress) | Salivary cortisol measurement |
| [25] | PPG (wristband), ECG (chest strap), GSR (wristband) | HR, HRV, SC | 1- Memory Game, Mosquito Sound, IAPS, Plank, Ice Test, TSST, SCWT 2- Real Life | 2 (Stress, Not-stress) | Everyday self-reported stress label |
| [26] | PPG (earlobe), EEG (headband), GSR (finger clip) | HR, SC, Brain Activity | Real-Life Public Speaking | 2 (Stress, Not-stress) | NR |
| [27] | PPG (wristband), ECG (chest strap), EDA (wristband) | HR, EDA, RR, PP (thermal camera) | Computer task: Essay Writing, Calming Video/Stroop Test, Dual task, Online Presentation | NR | NR |
| [28] | PPG, EDA, ACC (all wristwatch) | HR, SC, ST, ACC | Real Life | 3 (Low stress, Medium stress, High stress) | NASA-TLX and self-reported questionnaires |
| [29] | PPG, GSR, ST, ACC, GYRO (all wristband) | HRV, ST, ACC | Simulated Indoor Driving Environment | 4 (Normal, Stress, Fatigue, Drowsiness) | Self-reported Stress feedback on a 1–5 scale |
| [30] | PPG (headband), ECG (chest and hips), SCG (chest) | HR, PEP, PTT, PAT PPG amplitude PFC Oxygenation Markers | Mental arithmetic tasks, N-back memory tasks | 3 (Easy, Medium, Hard) | NASA-TLX questionnaire |
| Study | Signal Pre-Processing | Stress Detection Methodology |
|---|---|---|
| [12] | Butterworth low pass filter (2 Hz). Distribution filter, threshold detection | RR interval detection with time domain analysis |
| [30] | Finite Impulse Bandpass (0.8 Hz- 10 Hz) | Machine Learning |
| [15] | Low pass filter (5 Hz). Linear extrapolation based on rolling average | RR interval detection with time domain analysis |
| [18] | Butterband band pass (0.7 Hz–3.5 Hz); moving average filter | Machine Learning |
| [16] | Cubic spline interpolation on clipped signals, Savitsky-Golay filter | RR interval detection with time domain analysis |
| [26] | Savitsky-Golay filter | Support Vector Machine |
| [7] | Moving average filter | RR interval detection with time domain analysis |
| [27] | Normalization via subtracting baseline signal | T-test |
| [13] | 3 stage band pass (0.5 Hz–11 Hz, 0.8 Hz–3 Hz, 0.9 Hz–1.6 Hz) | Sliding window RR detection with time domain analysis |
| [22] | Moving average filter | Sliding window PPG and PPG velocity signal analysis |
| [21] | None | RR interval detection |
| [17] | Noise removal via least mean squares | HR frequency analysis using IIR Bandpass filter and sinusoidal modeling. |
| Study | Methods | Classification Classes | Best Performance |
|---|---|---|---|
| [23] | 1- Normalization 2- Feature extraction 3- Feature selection using:
| 1- Stressful 2- Relaxing 3- Normal | PPG ONLY: (kNN = 5 with Chi-square, Accuracy = 80.74) FUSED PPG: PPG + GSR: (kNN = 3 with Chi-square, Accuracy = 85.03) |
| [29] | 1- Normalization using 5 methods 2- Feature construction 3- Feature extraction using:
| 1- Normal 2- Stress 3- Fatigue 4- Drowsiness | PPG ONLY: MLP (Accuracy = 98.43) |
| [33] | 1- Feature extraction: 2- Classification using:
| 1- PROM-Pain4a ≥ 66.6 and PCL-5 ≥ 31 2- PROM-Pain4a < 55.6 and PCL-5 < 31 | PPG ONLY PTSD: (A) Linear SVM (AUC = 0.73 ± 0.03) (B) LR (AUC = 0.73 ± 0.03) (C) MLP (AUC = 0.73 ± 0.03) PTSD Sleep Anx./Panic: MLP (AUC = 0.79 ± 0.05) PTSD Pain Int.: Linear SVM (AUC = 0.76 ± 0.04) |
| [26] | 1- Feature construction 2- Feature extraction using:
| 1- Not stressed 2- Stressed | PPG ONLY: SVM (Accuracy = 80.00, f-measure = 0.79, Kappa Values = 0.72) FUSED PPG: SVM (Accuracy = 96.25, f-measure = 0.96, Kappa Values = 0.87) |
| [18] | 1- Feature extraction 2- Feature selection 3- Classification using:
| 1- Not stressed 2- Stressed | PPG ONLY: 1- A little bit VS. baseline MLP (F-measure = 0.73 ± 0.06) 2- Some VS. baseline Random Forest (RF) (F-measure = 0.71 ± 0.05) 3- Extremely VS. baseline: RF (F-measure = 0.76 ± 0.05) 4- Some, a lot or extremely VS. a little bit or not at all XGBoost (F-measure = 0.63 ± 0.04) |
| [14] | 1- Feature Extraction 2- Classification using:
| 1- Distress 2- Calmness | PPG ONLY DT (AUC = 0.75) |
| [19] | 1- Feature extraction 2- Feature selection 3- Classification using:
| 1- Not stressed 2- Stressed | PPG ONLY AdaBoost (Accuracy = 0.93, Precision = 0.93) |
| [32] | 1- Feature extraction 2- Feature selection 3- Relationship between stress or drowsiness using:
| 1- High MW state 2- Low MW state | PPG ONLY SVM (Accuracy = 0.78) |
| [20] | 1- Feature extraction 2- Feature selection:
| 1- class classification: (A) Baseline (B) Stress (C) Amusement 2-class classification: (A) Not stressed (B) Stressed | PPG ONLY Two-class Hybrid CNN (Accuracy = 0.89, F-measure = 0.87) Three-class Hybrid CNN (Accuracy = 0.75, F-measure = 0.64) |
| [28] | 1- Feature Extraction
| 1- Stress Level 1 (index: 0–30) 2– Stress Level 2 (index: 35–75) 3– stress Level 3 (index: 80–100) | FUSED PPG: HR + accelerometer for Empatica E4 MLP (Accuracy = 92.19, f-Measure = 90.3, Precision = 91.4, Recall = 90.2) |
| [30] | 1- Feature extraction 2- Feature selection
| 1- Rest 2- Arithmetic 3- N-back task | FUSED PPG: PPG + ECG + SCG RF (Accuracy = 0.85 ± 0.09, Recall = 0.84 ± 0.14, Precision = 0.83 ± 0.1, F1 = 0.80 ± 0.13) |
| [25] | 1- Feature extraction 2- Feature selection
| 1- Not stressed 2- Stressed | FUSED PPG: PPG + ECG + GSR SVM (Accuracy = 0.95) |
| [24] | (I) WRISTBAND BASED STRESS DETECTION 1- Feature extraction 2- Feature selection
PRESSURE ESTIMATION 1- Feature extraction 2- Feature selection
| 1- Not stressed 2- Stressed | FUSED PPG: PPG + EDA RF (Accuracy = 0.94, F-measure = 0.92) |
| Category | Limitations |
|---|---|
Experimental Limitations
| (1) Small participant sample sizes (2) Relatively homogenous population (3) Failure to report participants’ medical history or additional conditions (4) Exclusion of participants with health conditions (5) Lack of a ground-truth method (6) Use of subjective stress evaluations (7) Poorly designed stress induction process (8) Non-automated process for noisy signal processing (9) Neglected to account for motion and motion artifacts |
Device Design
| (1) Device was obtrusive (2) Lack of built-in battery; the device did not have an integrated battery (3) Lack of accompanying user-friendly app to communicate data (4) Lack of consistent cut off values for filters (5) The absence of commonly used commercial devices (e.g., Apple Watch and FitBit) among the studies (6) Use of small datasets that cannot reliably train a generalized ML model (7) Lack of continuum measurement of stress level |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Namvari, M.; Lipoth, J.; Knight, S.; Jamali, A.A.; Hedayati, M.; Spiteri, R.J.; Syed-Abdul, S. Photoplethysmography Enabled Wearable Devices and Stress Detection: A Scoping Review. J. Pers. Med. 2022, 12, 1792. https://doi.org/10.3390/jpm12111792
Namvari M, Lipoth J, Knight S, Jamali AA, Hedayati M, Spiteri RJ, Syed-Abdul S. Photoplethysmography Enabled Wearable Devices and Stress Detection: A Scoping Review. Journal of Personalized Medicine. 2022; 12(11):1792. https://doi.org/10.3390/jpm12111792
Chicago/Turabian StyleNamvari, Mina, Jessica Lipoth, Sheida Knight, Ali Akbar Jamali, Mojtaba Hedayati, Raymond J. Spiteri, and Shabbir Syed-Abdul. 2022. "Photoplethysmography Enabled Wearable Devices and Stress Detection: A Scoping Review" Journal of Personalized Medicine 12, no. 11: 1792. https://doi.org/10.3390/jpm12111792