The Genomics and Metagenomics of Asthma Severity (GEMAS) Study: Rationale and Design
Abstract
:1. Introduction
2. Materials and Methods
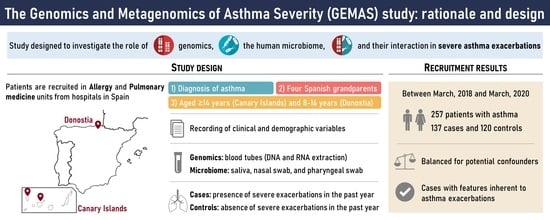
2.1. Study Design and Data Collection
2.2. Clinical Assessment
2.3. Biological Sample Collection and Storage
2.4. Processing of Samples for Future Genomic and Metagenomic Studies
2.5. Statistical Analysis for the Comparison of Demographic and Clinical Characteristics between Cases and Controls
3. Results
- A total of 257 individuals with asthma have been recruited between March 2018 and March 2020 (137 cases and 120 controls).
- Cases and controls recruited in the Canary Islands and in the Basque Country did not differ for many potential confounders for the future genomic and microbiome analyses (e.g., age, gender, tobacco exposure, comorbidities, etc.).
- Cases from the Canary Islands have clinical characteristics that support the definition of asthma exacerbations (i.e., impaired lung function, severe and uncontrolled asthma, coexistence of GERD, and use of asthma medication).
- Children from the Basque Country who had asthma exacerbations in the past year have higher proportion of severe asthma and OCS use, and worse medication adherence than controls.
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| 16S rRNA | 16S ribosomal ribonucleic acid |
| ACQ | Asthma Control Questionnaire |
| ATS | American Thoracic Society |
| BDR | Bronchodilator response |
| BMI | Body mass index |
| DNA | Deoxyribonucleic acid |
| EDTA | Ethylenediaminetetraacetic acid |
| ER | Emergency room |
| ERS | European Respiratory Society |
| FeNO | Fraction of exhaled nitric oxide |
| FEV1 | Forced expiratory volume in the first second |
| FVC | Forced vital capacity |
| GEMAS | Genomics and Metagenomics of Asthma Severity |
| GERD | Gastroesophageal reflux disease |
| GINA | Global Initiative for Asthma |
| GLI | Global Lung Function Initiative |
| GWAS | Genome-wide association study |
| ICS | Inhaled corticosteroids |
| IgE | Immunoglobulin E |
| LABA | Long-acting beta agonists |
| LTRA | Leukotriene receptor antagonists |
| MARS-5 | Medication Adherence Report Scale |
| MEGA | Mechanisms Involved in the Genesis and Disease Course of Asthma |
| NIH | National Institutes of Health |
| NGS | Next-generation sequencing |
| OCS | Oral corticosteroids |
| RNA | Ribonucleic acid |
| SABA | Short-acting beta agonists |
| SAMA | Short-acting muscarinic antagonists |
| SEPAR | Sociedad Española de Neumología y Cirugía Torácica |
| SNP | Single nucleotide polymorphism |
| WHO | World Health Organization |
References
- The Global Asthma Report 2018; Global Asthma Network: Auckland, New Zealand, 2018; ISBN 978-0-473-46523-0/978-0-473-46524-7.
- GEMA 5.0. Guía Española Para El Manejo Del Asma; Sociedad Española de Neumología y Cirugía Torácica: Barcelona, Spain, 2020; ISBN 978-84-17372-97-2.
- Juliá-Serdá, G.; Cabrera-Navarro, P.; Acosta-Fernández, O.; Martín-Pérez, P.; Losada-Cabrera, P.; García-Bello, M.A.; Carrillo-Díaz, T.; Antó-Boqué, J. High Prevalence of Asthma and Atopy in the Canary Islands, Spain. Int. J. Tuberc. Lung Dis. 2011, 15, 536–541. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Lerma, B.; Morales-Chirivella, F.J.; Peñuelas, I.; Blanco Guerra, C.; Mesa Lugo, F.; Aguinaga-Ontoso, I.; Guillén-Grima, F. High Prevalence of Asthma and Allergic Diseases in Children Aged 6 to 7 Years from the Canary Islands. J. Investig. Allergol. Clin. Immunol. 2009, 19, 383–390. [Google Scholar] [PubMed]
- Global Strategy for Asthma Management and Prevention; Global Initiative for Asthma: Fontana, WI, USA, 2020.
- Nunes, C.; Pereira, A.M.; Morais-Almeida, M. Asthma Costs and Social Impact. Asthma Res. Pract. 2017, 3, 1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bloom, C.I.; Palmer, T.; Feary, J.; Quint, J.K.; Cullinan, P. Exacerbation Patterns in Adults with Asthma in England A Population-Based Study. Am. J. Respir. Crit. Care Med. 2019, 199, 446–453. [Google Scholar] [CrossRef] [PubMed]
- Puranik, S.; Forno, E.; Bush, A.; Celedón, J.C. Predicting Severe Asthma Exacerbations in Children. Am. J. Respir. Crit. Care Med. 2017, 195, 854–859. [Google Scholar] [CrossRef] [PubMed]
- Hernandez-Pacheco, N.; Pino-Yanes, M.; Flores, C. Genomic Predictors of Asthma Phenotypes and Treatment Response. Front. Pediatr. 2019, 7, 6. [Google Scholar] [CrossRef] [Green Version]
- García-Sánchez, A.; Isidoro-García, M.; García-Solaesa, V.; Sanz, C.; Hernández-Hernández, L.; Padrón-Morales, J.; Lorente-Toledano, F.; Dávila, I. Genome-Wide Association Studies (GWAS) and Their Importance in Asthma. Allergol. Immunopathol. 2015, 43, 601–608. [Google Scholar] [CrossRef]
- Herrera-Luis, E.; Hernandez-Pacheco, N.; Vijverberg, S.J.; Flores, C.; Pino-Yanes, M. Role of Genomics in Asthma Exacerbations. Curr. Opin. Pulm. Med. 2019, 25, 101–112. [Google Scholar] [CrossRef]
- Perez-Garcia, J.; Espuela-Ortiz, A.; Lorenzo-Diaz, F.; Pino-Yanes, M. Pharmacogenetics of Pediatric Asthma: Current Perspectives. Pharmgenomics Pers. Med. 2020, 13, 89–103. [Google Scholar] [CrossRef] [Green Version]
- Perez-Garcia, J.; Herrera-Luis, E.; Lorenzo-Diaz, F.; González, M.; Sardón, O.; Villar, J.; Pino-Yanes, M. Precision Medicine in Childhood Asthma: Omic Studies of Treatment Response. Int. J. Mol. Sci. 2020, 21, 2908. [Google Scholar] [CrossRef] [Green Version]
- Brooks, C.; Pearce, N.; Douwes, J. The Hygiene Hypothesis in Allergy and Asthma: An Update. Curr. Opin. Allergy Clin. Immunol. 2013, 13, 70–77. [Google Scholar] [CrossRef] [PubMed]
- Weinstock, G.M. Genomic Approaches to Studying the Human Microbiota. Nature 2012, 489, 250–256. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hilty, M.; Burke, C.; Pedro, H.; Cardenas, P.; Bush, A.; Bossley, C.; Davies, J.; Ervine, A.; Poulter, L.; Pachter, L.; et al. Disordered Microbial Communities in Asthmatic Airways. PLoS ONE 2010, 5, e8578. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Charlson, E.S.; Bittinger, K.; Haas, A.R.; Fitzgerald, A.S.; Frank, I.; Yadav, A.; Bushman, F.D.; Collman, R.G. Topographical Continuity of Bacterial Populations in the Healthy Human Respiratory Tract. Am. J. Respir. Crit. Care Med. 2011, 184, 957–963. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Depner, M.; Ege, M.J.; Cox, M.J.; Dwyer, S.; Walker, A.W.; Birzele, L.T.; Genuneit, J.; Horak, E.; Braun-Fahrländer, C.; Danielewicz, H.; et al. Bacterial Microbiota of the Upper Respiratory Tract and Childhood Asthma. J. Allergy Clin. Immunol. 2017, 139, 826–834.e13. [Google Scholar] [CrossRef] [Green Version]
- Teo, S.M.; Mok, D.; Pham, K.; Kusel, M.; Serralha, M.; Troy, N.; Holt, B.J.; Hales, B.J.; Walker, M.L.; Hollams, E.; et al. The Infant Nasopharyngeal Microbiome Impacts Severity of Lower Respiratory Infection and Risk of Asthma Development. Cell Host Microbe 2015, 17, 704–715. [Google Scholar] [CrossRef] [Green Version]
- Espuela-Ortiz, A.; Lorenzo-Diaz, F.; Baez-Ortega, A.; Eng, C.; Hernandez-Pacheco, N.; Oh, S.S.; Lenoir, M.; Burchard, E.G.; Flores, C.; Pino-Yanes, M. Bacterial Salivary Microbiome Associates with Asthma among African American Children and Young Adults. Pediatr. Pulmonol. 2019, 54, 1948–1956. [Google Scholar] [CrossRef]
- Good, J.T.; Kolakowski, C.A.; Groshong, S.D.; Murphy, J.R.; Martin, R.J. Refractory Asthma: Importance of Bronchoscopy to Identify Phenotypes and Direct Therapy. Chest 2012, 141, 599–606. [Google Scholar] [CrossRef] [Green Version]
- Zhou, Y.; Jackson, D.; Bacharier, L.B.; Mauger, D.; Boushey, H.; Castro, M.; Durack, J.; Huang, Y.; Lemanske, R.F.; Storch, G.A.; et al. The Upper-Airway Microbiota and Loss of Asthma Control among Asthmatic Children. Nat. Commun. 2019, 10, 5714. [Google Scholar] [CrossRef] [Green Version]
- Fazlollahi, M.; Lee, T.D.; Andrade, J.; Oguntuyo, K.; Chun, Y.; Grishina, G.; Grishin, A.; Bunyavanich, S. The Nasal Microbiome in Asthma. J. Allergy Clin. Immunol. 2018, 142, 834–843.e2. [Google Scholar] [CrossRef] [Green Version]
- McCauley, K.; Durack, J.; Valladares, R.; Fadrosh, D.W.; Lin, D.L.; Calatroni, A.; LeBeau, P.K.; Tran, H.T.; Fujimura, K.E.; LaMere, B.; et al. Distinct Nasal Airway Bacterial Microbiotas Differentially Relate to Exacerbation in Pediatric Patients with Asthma. J. Allergy Clin. Immunol. 2019, 144, 1187–1197. [Google Scholar] [CrossRef] [PubMed]
- Hall, A.B.; Tolonen, A.C.; Xavier, R.J. Human Genetic Variation and the Gut Microbiome in Disease. Nat. Rev. Genet. 2017, 18, 690–699. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.J. Asthma Microbiome Studies and the Potential for New Therapeutic Strategies. Curr. Allergy Asthma Rep. 2013, 13, 453–461. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johnson, D.; Hughes, D.; Pirmohamed, S.M.; Jorgensen, A. Evidence to Support Inclusion of Pharmacogenetic Biomarkers in Randomised Controlled Trials. J. Pers. Med. 2019, 9, 42. [Google Scholar] [CrossRef] [Green Version]
- Graham, B.L.; Steenbruggen, I.; Barjaktarevic, I.Z.; Cooper, B.G.; Hall, G.L.; Hallstrand, T.S.; Kaminsky, D.A.; McCarthy, K.; McCormack, M.C.; Miller, M.R.; et al. Standardization of Spirometry 2019 Update an Official American Thoracic Society and European Respiratory Society Technical Statement. Am. J. Respir. Crit. Care Med. 2019, 200, e70–e88. [Google Scholar] [CrossRef]
- Manual SEPAR de Procedimientos. Módulo 3. In Procedimientos de Evaluación de la Función Pulmonar; Sociedad Española de Neumología y Cirugía Torácica: Barcelona, Spain, 2002; ISBN 84-7989-155-6.
- Quanjer, P.H.; Stanojevic, S.; Cole, T.J.; Baur, X.; Hall, G.L.; Culver, B.H.; Enright, P.L.; Hankinson, J.L.; Ip, M.S.M.; Zheng, J.; et al. Multi-Ethnic Reference Values for Spirometry for the 3-95-Yr Age Range: The Global Lung Function 2012 Equations. Eur. Respir. J. 2012, 40, 1324–1343. [Google Scholar] [CrossRef] [PubMed]
- American Thoracic Society; European Respiratory Society. ATS/ERS Recommendations for Standardized Procedures for the Online and Offline Measurement of Exhaled Lower Respiratory Nitric Oxide and Nasal Nitric Oxide, 2005. Am. J. Respir. Crit. Care Med. 2005, 171, 912–930. [Google Scholar] [CrossRef]
- De Onis, M.; Onyango, A.W.; Borghi, E.; Siyam, A.; Nishida, C.; Siekmann, J. Development of a WHO Growth Reference for School-Aged Children and Adolescents. Bull. World Health Organ. 2007, 85, 660–667. [Google Scholar] [CrossRef]
- Klindworth, A.; Pruesse, E.; Schweer, T.; Peplies, J.; Quast, C.; Horn, M.; Glöckner, F.O. Evaluation of General 16S Ribosomal RNA Gene PCR Primers for Classical and Next-Generation Sequencing-Based Diversity Studies. Nucleic Acids Res. 2013, 41, e1. [Google Scholar] [CrossRef]
- Papi, A.; Brightling, C.; Pedersen, S.E.; Reddel, H.K. Asthma. Lancet 2018, 391, 783–800. [Google Scholar] [CrossRef]
- Sears, M.R. Lung Function Decline in Asthma. Eur. Respir. J. 2007, 30, 411–413. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Trivedi, M.; Denton, E. Asthma in Children and Adults—What Are the Differences and What Can They Tell Us about Asthma? Front. Pediatr. 2019, 7, 256. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wenzel, S.E. Asthma Phenotypes: The Evolution from Clinical to Molecular Approaches. Nat. Med. 2012, 18, 716–725. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, M.A.R.; Mathur, R.; Vonk, J.M.; Szwajda, A.; Brumpton, B.; Granell, R.; Brew, B.K.; Ullemar, V.; Lu, Y.; Jiang, Y.; et al. Genetic Architectures of Childhood- and Adult-Onset Asthma Are Partly Distinct. Am. J. Hum. Genet. 2019, 104, 665–684. [Google Scholar] [CrossRef] [Green Version]
- Burcham, Z.M.; Garneau, N.L.; Comstock, S.S.; Tucker, R.M.; Knight, R.; Metcalf, J.L.; Miranda, A.; Reinhart, B.; Meyers, D.; Woltkamp, D.; et al. Patterns of Oral Microbiota Diversity in Adults and Children: A Crowdsourced Population Study. Sci. Rep. 2020, 10, 2133. [Google Scholar] [CrossRef] [Green Version]
- Muñoz, X.; Álvarez-Puebla, M.J.; Arismendi, E.; Arochena, L.; Ausín, M.d.P.; Barranco, P.; Bobolea, I.; Cañas, J.A.; Cardaba, B.; Crespo, A.; et al. The MEGA Project: A Study of the Mechanisms Involved in the Genesis and Disease Course of Asthma. Asthma Cohort Creation and Long-Term Follow-Up. Arch. Bronconeumol. 2018, 54, 378–385. [Google Scholar] [CrossRef]
- Human Microbiome Project Consortium. A Framework for Human Microbiome Research. Nature 2012, 486, 215–221. [Google Scholar] [CrossRef] [Green Version]
- Dethlefsen, L.; Relman, D.A. Incomplete Recovery and Individualized Responses of the Human Distal Gut Microbiota to Repeated Antibiotic Perturbation. Proc. Natl. Acad. Sci. USA 2011, 108, 4554–4561. [Google Scholar] [CrossRef] [Green Version]
- Gupta, V.K.; Paul, S.; Dutta, C. Geography, Ethnicity or Subsistence-Specific Variations in Human Microbiome Composition and Diversity. Front. Microbiol. 2017, 8, 1162. [Google Scholar] [CrossRef] [Green Version]
| Canary Islands Patients | Basque Country Patients | |||||||
|---|---|---|---|---|---|---|---|---|
| Sample Size (n) | Controls (n = 102) | Cases (n = 103) | p-Value | Sample Size (n) | Controls (n = 18) | Cases (n = 34) | p-Value | |
| Age (years) | 205 | 50.5 (33.0–62.0) | 46.0 (29.5–59.5) | 0.253 | 52 | 10.0 (9.0–11.8) | 11.0 (9.0–12.8) | 0.507 |
| Gender (female) | 205 | 65 (63.7) | 71 (68.9) | 0.462 | 52 | 4 (22.2) | 16 (47.1) | 0.133 |
| Ever smoker or secondhand smoke exposure a | 202 | 29 (28.7) | 38 (37.6) | 0.232 | 52 | 9 (50.0) | 19 (55.9) | 0.774 |
| Lung function | ||||||||
| pre-FEV1 (% predicted) | 197 | 90.3 (76.1–101.9) | 83.4 (69.2–92.6) | 0.003 | 48 | 95.8 (89.2–102.3) | 99.4 (89.4–106.4) | 0.455 |
| pre-FEV1 (z-score) | 197 | −0.8 (1.3) | −1.3 (1.3) | 0.006 | 48 | −0.3 (0.8) | −0.1 (1.2) | 0.415 |
| pre-FVC (% predicted) | 196 | 94.2 (81.3–102.6) | 87.7 (79.3–96.5) | 0.020 | 48 | 102.2 (92.9–108.3) | 104.4 (92.1–109.9) | 0.579 |
| pre-FVC (z-score) | 196 | −0.5 (1.1) | −0.9 (1.1) | 0.012 | 48 | 0.0 (0.8) | 0.2 (1.0) | 0.511 |
| pre-FEV1/FVC (%) | 196 | 79.1 (72.4–83.5) | 75.9 (68.3–83.2) | 0.138 | 48 | 83.9 (79.2–86.9) | 83.8 (80.4–89.2) | 0.429 |
| BDR (%) | 71 | 4.7 (1.8–10.5) | 9.0 (3.1–15.0) | 0.166 | 48 | 3.4 (1.8–5.3) | 2.4 (−0.5–3.6) | 0.344 |
| FeNO (ppb) | NA | NA | NA | NA | 48 | 15.0 (9.0–39.7) | 14.9 (8.6–28.1) | 0.491 |
| Total IgE levels (UI/mL) | 187 | 149.8 (42.1–434.5) | 125.7 (39.3–449.3) | 0.641 | 17 | 902.5 (287.5–2402.5) | 450.0 (172.5–635.5) | 0.216 |
| Absolute eosinophil count (cells/µL) | 192 | 300.0 (200.0–500.0) | 300.0 (100.0–500.0) | 0.209 | 15 | 750.0 (467.5–1027.5) | 500.0 (425.0–710.0) | 0.412 |
| Eosinophil percentage (%) | 186 | 4.3 (2.6–6.8) | 3.7 (1.5–7.0) | 0.190 | 10 | 5.1 (5.0–11.3) | 6.0 (3.8–8.7) | 0.933 |
| Comorbidities | 52 | |||||||
| Otorhinolaryngology disease | 202 | 24 (23.8) | 29 (28.7) | 0.523 | 51 | 2 (11.8) | 5 (14.7) | 1.000 |
| Gastroesophageal reflux | 203 | 16 (15.7) | 33 (32.7) | 0.005 | 52 | 1 (5.6) | 0 (0) | 0.346 |
| Sleep apnea | 202 | 15 (15.0) | 12 (11.8) | 0.540 | 52 | 1 (5.6) | 1 (2.9) | 1.000 |
| Obesity | 197 | 37 (36.6) | 33 (34.4) | 0.768 | 49 | 3 (17.6) | 4 (12.5) | 0.681 |
| Atopy | 179 | 69 (76.7) | 70 (78.7) | 0.858 | 50 | 14 (82.4) | 26 (78.8) | 1.000 |
| Other allergic phenotypes | 202 | 72 (70.6) | 74 (74.0) | 0.639 | 52 | 15 (83.3) | 28 (82.4) | 1.000 |
| Rhinitis | 202 | 65 (63.7) | 67 (67.0) | 0.659 | 52 | 10 (55.6) | 23 (67.6) | 0.546 |
| Dermatitis | 202 | 18 (17.6) | 20 (20.0) | 0.721 | 52 | 6 (33.3) | 9 (26.5) | 0.749 |
| Drug allergy | 202 | 17 (16.7) | 22 (22.0) | 0.376 | 52 | 1 (5.6) | 0 (0) | 0.346 |
| Food allergy | 202 | 7 (6.9) | 12 (12.0) | 0.236 | 52 | 6 (33.3) | 5 (14.7) | 0.159 |
| Age of asthma onset (years) | 188 | 16.0 (5.0–40.0) | 20.0 (6.0–44.8) | 0.572 | 48 | 2.5 (1.8–4.8) | 2.3 (1.0–4.0) | 0.423 |
| Family history | ||||||||
| Allergy | 205 | 70 (68.6) | 71 (68.9) | 1.000 | 52 | 15 (83.3) | 27 (79.4) | 1.000 |
| Asthma | 205 | 44 (43.1) | 46 (44.7) | 0.888 | 52 | 11 (61.1) | 18 (52.9) | 0.770 |
| Asthma exacerbations | 205 | 52 | ||||||
| OCS use | 205 | 0 (0) | 70 (68.0) | NA | 52 | 0 (0) | 34 (100) | NA |
| ER visits | 205 | 0 (0) | 93 (90.3) | NA | 52 | 0 (0) | 20 (58.8) | NA |
| Hospitalizations | 205 | 0 (0) | 20 (19.4) | NA | 52 | 0 (0) | 5 (14.7) | NA |
| Asthma severity | 200 | 52 | ||||||
| Mild | 8 (7.9) | 0 (0) | 0.007 | 3 (16.7) | 1 (2.9) | 0.113 | ||
| Moderate | 9 (8.9) | 4 (4.0) | 0.251 | 11 (61.1) | 1 (2.9) | 5.3 × 10−6 | ||
| Severe | 84 (83.2) | 95 (96) | 0.005 | 4 (22.2) | 32 (94.1) | 1.7 × 10−7 | ||
| Asthma control | 191 | 48 | ||||||
| Well controlled | 55 (56.1) | 26 (28.0) | 1.3 × 10−4 | 14 (82.4) | 26 (83.9) | 1.000 | ||
| Partially controlled | 29 (29.6) | 27 (29.0) | 1.000 | 3 (17.6) | 2 (6.5) | 0.331 | ||
| Poorly controlled | 14 (14.3) | 40 (43.0) | 1.2 × 10−5 | 0 (0) | 3 (9.7) | 0.543 | ||
| Pharmacological treatment | ||||||||
| SABA | 205 | 47 (46.1) | 79 (77.5) | 6.5 × 10−6 | 52 | 13 (72.2) | 31 (91.2) | 0.108 |
| ICS | 205 | 95 (93.1) | 103 (100) | 0.007 | 52 | 18 (100) | 34 (100) | NA |
| LABA | 205 | 90 (88.2) | 101 (98.1) | 0.006 | 52 | 11 (61.1) | 26 (76.5) | 0.337 |
| LTRA | 205 | 50 (49.0) | 63 (61.8) | 0.091 | 51 | 0 (0) | 1 (3.0) | 1.000 |
| OCS | 204 | 7 (6.9) | 51 (50.5) | 1.3 × 10−12 | 52 | 1 (5.6) | 32 (94.1) | 1.3 × 10−10 |
| SAMA | 205 | 19 (18.6) | 42 (41.2) | 7.0 × 10−4 | 52 | 0 (0) | 0 (0) | NA |
| LAMA | 205 | 25 (24.5) | 31 (30.4) | 0.433 | 51 | 0 (0) | 0 (0) | NA |
| Theophylline | 205 | 0 (0) | 9 (8.8) | 0.003 | 52 | 0 (0) | 0 (0) | NA |
| Antihistamines | 205 | 58 (56.9) | 74 (72.5) | 0.028 | 52 | 3 (16.7) | 14 (41.2) | 0.120 |
| Azithromycin | 205 | 5 (4.9) | 15 (14.7) | 0.032 | 52 | 1 (5.6) | 10 (29.4) | 0.073 |
| Biological therapies | 205 | 14 (13.7) | 16 (15.7) | 0.844 | 52 | 0 (0) | 1 (2.9) | 1.000 |
| Immunotherapy | 204 | 21 (20.6) | 17 (16.8) | 0.590 | 51 | 0 (0) | 0 (0) | NA |
| Antibiotics | 205 | 18 (17.8) | 45 (44.1) | 6.8 × 10−5 | 52 | 1 (5.6) | 6 (17.6) | 0.399 |
| Medication adherence | 203 | 25.0 (23.0–25.0) | 25.0 (23.0–25.0) | 0.121 | 52 | 24.0 (24.0–25.0) | 24.0 (22.3–25.0) | 0.033 |
| Home environment (rural) | 204 | 52 (51.0) | 60 (58.8) | 0.325 | 52 | 6 (33.3) | 4 (11.8) | 0.076 |
| Household pets | 201 | 48 (48.5) | 49 (48.0) | 1.000 | 52 | 1 (5.6) | 9 (26.5) | 0.136 |
| Education level a | 204 | 51 | ||||||
| No schooling completed | 2 (2.0) | 1 (1.0) | 1.000 | 0 (0) | 0 (0) | NA | ||
| Lower secondary education | 40 (39.2) | 39 (38.2) | 1.000 | 3 (17.6) | 7 (20.6) | 1.000 | ||
| Higher secondary education | 37 (36.3) | 41 (40.2) | 0.666 | 8 (47.1) | 9 (26.5) | 0.208 | ||
| Higher education | 23 (22.5) | 21 (20.6) | 0.865 | 6 (35.3) | 18 (52.9) | 0.372 | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Perez-Garcia, J.; Hernández-Pérez, J.M.; González-Pérez, R.; Sardón, O.; Martin-Gonzalez, E.; Espuela-Ortiz, A.; Mederos-Luis, E.; Callero, A.; Herrera-Luis, E.; Corcuera, P.; et al. The Genomics and Metagenomics of Asthma Severity (GEMAS) Study: Rationale and Design. J. Pers. Med. 2020, 10, 123. https://doi.org/10.3390/jpm10030123
Perez-Garcia J, Hernández-Pérez JM, González-Pérez R, Sardón O, Martin-Gonzalez E, Espuela-Ortiz A, Mederos-Luis E, Callero A, Herrera-Luis E, Corcuera P, et al. The Genomics and Metagenomics of Asthma Severity (GEMAS) Study: Rationale and Design. Journal of Personalized Medicine. 2020; 10(3):123. https://doi.org/10.3390/jpm10030123
Chicago/Turabian StylePerez-Garcia, Javier, José M. Hernández-Pérez, Ruperto González-Pérez, Olaia Sardón, Elena Martin-Gonzalez, Antonio Espuela-Ortiz, Elena Mederos-Luis, Ariel Callero, Esther Herrera-Luis, Paula Corcuera, and et al. 2020. "The Genomics and Metagenomics of Asthma Severity (GEMAS) Study: Rationale and Design" Journal of Personalized Medicine 10, no. 3: 123. https://doi.org/10.3390/jpm10030123