Impact of Breast Density Awareness on Knowledge about Breast Cancer Risk Factors and the Self-Perceived Risk of Breast Cancer
Abstract
:1. Introduction
2. Participants and Methods
2.1. Subject Population
2.2. Study Design and Procedure
2.3. Statistical Analysis
3. Results
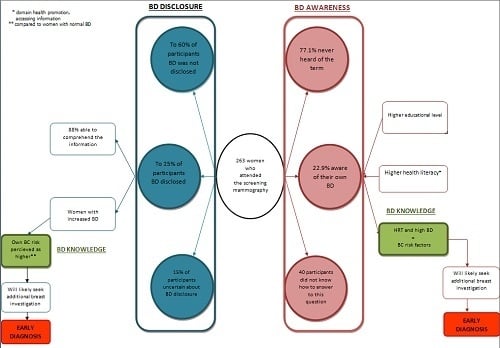
3.1. Women’s Demographic Characteristics, BD Data Disclosure and Differences in BD Awareness
3.2. Radiological Evaluation of BD
3.3. Knowledge about BC Risk Factors and BC Risk Perception According to BD Awareness
3.4. Health Literacy
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferlay, J.; Soerjomataram, I.; Dikshit, R.; Eser, S.; Mathers, C.; Rebelo, M.; Parkin, D.M.; Forman, D.; Bray, F. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int. J. Cancer 2015, 136, E359–E386. [Google Scholar] [CrossRef] [PubMed]
- Nyström, L.; Andersson, I.; Bjurstam, N.; Frisell, J.; Nordenskjöld, B.; Rutqvist, L.E. Long-term effects of mammography screening: Updated overview of the Swedish randomised trials. Lancet 2002, 359, 909–919. [Google Scholar] [CrossRef]
- Wang, A.T.; Vachon, C.M.; Brandt, K.R.; Ghosh, K. Breast density and breast cancer risk: A practical review. Mayo Clin. Proc. 2014, 89, 548–557. [Google Scholar] [CrossRef] [Green Version]
- Mendelson, E.B.; Böhm-Vélez, M.; Berg, W.A. ACR BI-RADS® mammography and ultrasound. In ACR BI-RADS® Atlas, Breast Imaging Reporting and Data System, 5th ed.; American College of Radiology: Reston, VA, USA, 2013. [Google Scholar]
- Lee, C.I.; Chen, L.E.; Elmore, J.G. Risk-based breast cancer screening: Implications of breast density. Med. Clin. North. Am. 2017, 101, 725–741. [Google Scholar] [CrossRef] [PubMed]
- Alomaim, W.; O’Leary, D.; Ryan, J.; Rainford, L.; Evanoff, M.; Foley, S. Subjective versus quantitative methods of assessing breast density. Diagnostics 2020, 10, 331. [Google Scholar] [CrossRef]
- Mandelson, M.T.; Oestreicher, N.; Porter, P.L.; White, D.; Finder, C.A.; Taplin, S.H.; White, E. Breast density as a predictor of mammographic detection: Comparison of interval- and screen-detected cancers. J. Natl. Cancer Inst. 2000, 92, 1081–1087. [Google Scholar] [CrossRef]
- Carney, P.A.; Miglioretti, D.L.; Yankaskas, B.C.; Kerlikowske, K.; Rosenberg, R.; Rutter, C.M.; Geller, B.M.; Abraham, L.A.; Taplin, S.H.; Dignan, M.; et al. Individual and combined effects of age, breast density, and hormone replacement therapy use on the accuracy of screening mammography. Ann. Intern. Med. 2003, 138, 168–175. [Google Scholar] [CrossRef]
- Yankaskas, B.C.; Cleveland, R.J.; Schell, M.J.; Kozar, R. Association of recall rates with sensitivity and positive predictive values of screening mammography. AJR Am. J. Roentgenol. 2001, 177, 543–549. [Google Scholar] [CrossRef]
- Boyd, N.F.; Martin, L.J.; Yaffe, M.J.; Minkin, S. Mammographic density and breast cancer risk: Current understanding and future prospects. Breast Cancer Res. 2011, 13, 223. [Google Scholar] [CrossRef] [Green Version]
- Vachon, C.M.; Pankratz, V.S.; Scott, C.G.; Haeberle, L.; Ziv, E.; Jensen, M.R.; Brandt, K.R.; Whaley, D.H.; Olson, J.E.; Heusinger, K.; et al. The contributions of breast density and common genetic variation to breast cancer risk. J. Natl. Cancer Inst. 2015, 107, dju397. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCormack, V.A.; dos Santos Silva, I. Breast density and parenchymal patterns as markers of breast cancer risk: A meta-analysis. Cancer Epidemiol. Biomarkers Prev. 2006, 15, 1159–1169. [Google Scholar] [CrossRef] [Green Version]
- Boyd, N.F. Mammographic density and risk of breast cancer. Am. Soc. Clin. Oncol. Educ. Book 2013. [Google Scholar] [CrossRef]
- Lee, C.I.; Bassett, L.W.; Lehman, C.D. Breast density legislation and opportunities for patient-centered outcomes research. Radiology 2012, 264, 632–636. [Google Scholar] [CrossRef] [PubMed]
- Santiago-Rivas, M.; Benjamin, S.; Jandorf, L. Breast density knowledge and awareness: A review of literature. J. Prim. Care Community Health 2016, 7, 207–214. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kerlikowske, K.; Zhu, W.; Hubbard, R.A.; Geller, B.; Dittus, K.; Braithwaite, D.; Wernli, K.J.; Miglioretti, D.L.; O’Meara, E.S. Outcomes of screening mammography by frequency, breast density, and postmenopausal hormone therapy. JAMA Intern. Med. 2013, 173, 807–816. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rhodes, D.J.; Radecki Breitkopf, C.; Ziegenfuss, J.Y.; Jenkins, S.M.; Vachon, C.M. Awareness of breast density and its impact on breast cancer detection and risk. J. Clin. Oncol. 2015, 33, 1143–1150. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guterbock, T.M.; Cohn, W.F.; Rexrode, D.L.; Eggleston, C.M.; Dean-McKinney, M.; Novicoff, W.M.; Yaffe, M.J.; Knaus, W.A.; Harvey, J.A. What do women know about breast density? Results from a population survey of Virginia women. J. Am. Coll. Radiol. 2017, 14, 34–44. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yeh, V.M.; Schnur, J.B.; Margolies, L.; Montgomery, G.H. Dense breast tissue notification: Impact on women’s perceived risk, anxiety, and intentions for future breast cancer screening. J. Am. Coll. Radiol. 2015, 12, 261–266. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Polacek, G.N.; Ramos, M.C.; Ferrer, R.L. Breast cancer disparities and decision-making among U.S. women. Patient Educ. Couns. 2007, 65, 158–165. [Google Scholar] [CrossRef] [Green Version]
- Sentell, T.; Braun, K.L.; Davis, J.; Davis, T. Health literacy and meeting breast and cervical cancer screening guidelines among Asians and whites in California. Springerplus 2015, 4, 432. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sørensen, K.; Van den Broucke, S.; Pelikan, J.M.; Fullam, J.; Doyle, G.; Slonska, Z.; Kondilis, B.; Stoffels, V.; Osborne, R.H.; Brand, H. Measuring health literacy in populations: Illuminating the design and development process of the European Health Literacy Survey Questionnaire (HLS-EU-Q). BMC Public Health 2013, 13, 948. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- MedCalc Statistical Software. Available online: https://www.medcalc.org.
- Katapodi, M.C.; Lee, K.A.; Facione, N.C.; Dodd, M.J. Predictors of perceived breast cancer risk and the relation between perceived risk and breast cancer screening: A meta-analytic review. Prev. Med. 2004, 38, 388–402. [Google Scholar] [CrossRef] [PubMed]
- Moothathu, N.S.; Philpotts, L.E.; Busch, S.H.; Gross, C.P.; Staib, L.H.; Hooley, R.J. Knowledge of density and screening ultrasound. Breast J. 2017, 23, 323–332. [Google Scholar] [CrossRef] [PubMed]
- Manning, M.A.; Duric, N.; Littrup, P.; Bey-Knight, L.; Penner, L.; Albrecht, T.L. Knowledge of breast density and awareness of related breast cancer risk. J. Cancer Educ. 2013, 28, 270–274. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Islami, F.; Torre, L.A.; Drope, J.M.; Ward, E.M.; Jemal, A. Global cancer in women: Cancer control priorities. Cancer Epidemiol. Biomarkers Prev. 2017, 26, 458–470. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Azam, S.; Lange, T.; Huynh, S.; Aro, A.R.; von Euler-Chelpin, M.; Vejborg, I.; Tjønneland, A.; Lynge, E.; Andersen, Z.J. Hormone replacement therapy, mammographic density, and breast cancer risk: A cohort study. Cancer Causes Control 2018, 29, 495–505. [Google Scholar] [CrossRef] [Green Version]
- Hack, C.C.; Emons, J.; Jud, S.M.; Heusinger, K.; Adler, W.; Gass, P.; Haeberle, L.; Heindl, F.; Hein, A.; Schulz-Wendtland, R.; et al. Association between mammographic density and pregnancies relative to age and BMI: A breast cancer case-only analysis. Breast Cancer Res. Treat 2017, 166, 701–708. [Google Scholar] [CrossRef]
- Vachon, C.M.; Kuni, C.C.; Anderson, K.; Anderson, V.E.; Sellers, T.A. Association of mammographically defined percent breast density with epidemiologic risk factors for breast cancer (United States). Cancer Causes Control 2000, 11, 653–662. [Google Scholar] [CrossRef]
- Miles, R.C.; Lehman, C.; Warner, E.; Tuttle, A.; Saksena, M. Patient-reported breast density awareness and knowledge after breast density legislation passage. Acad. Radiol. 2019, 26, 726–731. [Google Scholar] [CrossRef]
- Santiago-Rivas, M.; Benjamin, S.; Andrews, J.Z.; Jandorf, L. Breast density awareness and knowledge, and intentions for breast cancer screening in a diverse sample of women age eligible for mammography. J. Cancer Educ. 2019, 34, 90–97. [Google Scholar] [CrossRef] [PubMed]
- Komenaka, I.K.; Nodora, J.N.; Hsu, C.H.; Martinez, M.E.; Gandhi, S.G.; Bouton, M.E.; Klemens, A.E.; Wikholm, L.I.; Weiss, B.D. Association of health literacy with adherence to screening mammography guidelines. Obstet. Gynecol. 2015, 125, 852–859. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kamimura, A.; Chernenko, A.; Nourian, M.M.; Aguilera, G.; Assasnik, N.; Ashby, J. The role of health literacy in reducing negative perceptions of breast health and treatment among uninsured primary care patients. J. Community Health 2016, 41, 858–863. [Google Scholar] [CrossRef] [PubMed]


| BD Awareness (n (%)) | Not Aware of BD (n = 172 (77.1%)) | Aware of BD (n = 51 (22.9%)) | Total (n = 223) | p | |
|---|---|---|---|---|---|
| BD information disclosed (n (%)) | 20 (11.7) | 45 (88.2) | 65 (29.3) | <0.001 * | |
| Age (Median (25–75%)) | 58 (49–63) | 57 (49–63) | 58 (46.5–62) | 0.91 § | |
| BMI (Median (25–75%)) | 26.6 (24.4–30.1) | 25.1 (23.3–29.1) | 25.9 (24.1–29.3) | 0.11 § | |
| Live birth (Median (25–75%)) | 2 (1–2) | 2 (1–2) | 2 (1–2) | 0.94 § | |
| Education status (n (%)) | |||||
| Primary School Diploma | 29 (16.9) | 4 (7.8) | 33 (14.8) | 0.01 * | |
| High School Diploma | 111 (64.5) | 28 (54.9) | 144 (60) | ||
| Bachelor’s Degree | 13 (7.6) | 4 (7.8) | 17 (7.6) | ||
| Master’s Degree | 19 (11) | 15 (29.4) | 34 (15.2) | ||
| Doctorate | 0 | 0 | 0 | ||
| Work status (n (%)) | |||||
| Pupil | 1 (0.6) | 0 | 1 (0.4) | 0.08 * | |
| Student | 1 (0.6) | 0 | 1 (0.4) | ||
| Private Sector Employee | 28 (16.3) | 6 (11.8) | 34 (15.2) | ||
| Public Sector Employee | 42 (24.4) | 20 (39.2) | 62 (27.8) | ||
| Free profession | 2 (1.2) | 1 (2) | 3 (1.3) | ||
| Unemployed | 35 (20.3) | 3 (5.9) | 38 (17) | ||
| Retired | 63 (37) | 21 (41) | 84 (38) | ||
| Any type of cancer in first degree relative (n (%)) | 88 (51.5) | 28 (54.9) | 116 (52.3) | 0.67 * | |
| Family history of BC (n (%)) | 30 (17.4) | 9 (17.6) | 39 (17.5) | 0.97 * | |
| An active menstrual cycle (n (%)) | 44 (25.6) | 11 (21.6) | 55 (24.7) | 0.24 * | |
| Suffers from chronic illness for which daily therapy is required (n (%)) | 97 (56.4) | 27 (52.9) | 124 (55.6) | 0.66 * | |
| Cigarette smoker (n (%)) | 37 (21.5) | 11 (21.6) | 48 (21.5) | 0.99 * | |
| Regularly consumes alcoholic beverages ** (n (%)) | 2 (1.2) | 0 | 2 (0.9) | >0.99 * | |
| BD Awareness | Number (%) | p * | |||
|---|---|---|---|---|---|
| Not Aware of BD | Aware of BD | Total | |||
| ACR BI-RADS | |||||
| Non-dense breast | 114 (69.9) | 27 (56.3) | 141 (66.8) | 0.08 | |
| Dense breast | 49 (30.1) | 21 (43.8) | 70 (33.2) | ||
| Total | 163 (100) | 48 (100) | 211 (100) | ||
| BD information not disclosed | |||||
| Women with non-dense breast | 103 (72.5) | 5 (83.3) | 108 (73) | >0.99 | |
| Women with dense breast | 39 (27.5) | 1 (16.7) | 40 (27) | ||
| Total | 142 (100) | 6 (100) | 148 (100) | ||
| BD information disclosed | |||||
| Women with non-dense breast | 11 (55) | 22 (52.4) | 33 (53.2) | >0.099 | |
| Women with dense breast | 9 (45) | 20 (47.6) | 29 (46.8) | ||
| Total | 20 (100) | 42 (100) | 62 (100) | ||
| Median (25–75%) in Regard to Radiological Assessment of BD | p * | |||
|---|---|---|---|---|
| Non-Dense Breast | Dense Breast | Total | ||
| Age | 59 (54–63) | 47 (39–58) | 58 (46.5–62) | <0.001 |
| BMI | 27.5 (25.1–31.2) | 24.4 (22.1–23.0) | 25.9 (24.1–29.3) | <0.001 |
| Full-term pregnancies | 2 (2–2) | 2 (1–2) | 2 (1–2) | 0.003 |
| Not Aware of BD | Aware of BD | Total | p * | |
|---|---|---|---|---|
| † My risk of breast cancer | ||||
| In the succeeding 5 years | 3 (2–3) | 3 (2–3) | 3 (2–3) | 0.16 |
| Lifetime | 3 (2–3) | 3 (3–4) | 3 (2–3) | 0.08 |
| † My risk of breast cancer in comparison to BC risk of women of the same age | ||||
| In the succeeding 5 years | 3 (2–3) | 3 (2–3) | 3 (2–3) | 0.34 |
| Lifetime | 3 (2–3) | 3 (3–4) | 3 (2–3) | 0.16 |
| ** Breast cancer worry | ||||
| In the succeeding 5 years | 3 (1–3) | 3 (2– 4) | 3 (2–4) | 0.16 |
| Lifetime | 3 (2–4) | 3 (2–4) | 3 (2–4) | 0.18 |
| All Other Women n = 190 | Informed Women Aware of Their High BD (n = 21) | Total (n = 211) | p * | |
| † My risk of breast cancer | ||||
| In the succeeding 5 years | 3 (2–3) | 3 (2–4) | 3 (2–3) | 0.16 |
| Lifetime | 3 (2–3) | 3 (3–4) | 3 (2–3) | 0.07 |
| † My risk of breast cancer in comparison to BC risk of women of the same age | ||||
| In the succeeding 5 years | 3 (2–3) | 3 (2–4) | 3 (2–3) | 0.17 |
| Lifetime | 3 (2–3) | 3 (3–4) | 3 (2–3) | 0.03 |
| ** Breast cancer worry | ||||
| In the succeeding 5 years | 3 (1.25–4) | 3 (1.5–3) | 3 (1.5–3) | 0.64 |
| Lifetime | 3 (2–4) | 3 (2–3.75) | 3 (2–4) | 0.79 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bojanic, K.; Vukadin, S.; Sarcevic, F.; Malenica, L.; Grgic, K.; Smolic, R.; Kralik, K.; Bilic Curcic, I.; Ivanac, G.; Wu, G.Y.; et al. Impact of Breast Density Awareness on Knowledge about Breast Cancer Risk Factors and the Self-Perceived Risk of Breast Cancer. Diagnostics 2020, 10, 496. https://doi.org/10.3390/diagnostics10070496
Bojanic K, Vukadin S, Sarcevic F, Malenica L, Grgic K, Smolic R, Kralik K, Bilic Curcic I, Ivanac G, Wu GY, et al. Impact of Breast Density Awareness on Knowledge about Breast Cancer Risk Factors and the Self-Perceived Risk of Breast Cancer. Diagnostics. 2020; 10(7):496. https://doi.org/10.3390/diagnostics10070496
Chicago/Turabian StyleBojanic, Kristina, Sonja Vukadin, Filip Sarcevic, Luka Malenica, Kaja Grgic, Robert Smolic, Kristina Kralik, Ines Bilic Curcic, Gordana Ivanac, George Y. Wu, and et al. 2020. "Impact of Breast Density Awareness on Knowledge about Breast Cancer Risk Factors and the Self-Perceived Risk of Breast Cancer" Diagnostics 10, no. 7: 496. https://doi.org/10.3390/diagnostics10070496