Interaction between Air Pollutants and Pollen Grains: Effects on Public and Occupational Health
Abstract
:1. Introduction
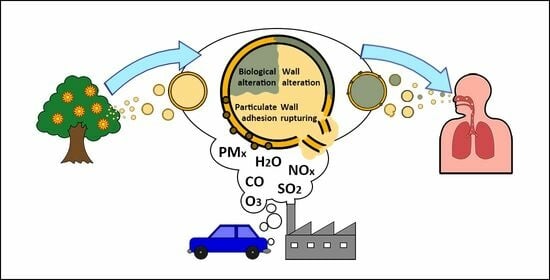
2. Interaction between Air Pollutants and Pollen
2.1. Effects of Air Pollutants on Physical and Chemical Properties of Pollen
2.2. Effects of Air Pollutants on Biological Properties of Pollen
3. Air Pollutants, Pollen and Human Health
3.1. Air Pollutants, Pollen and Public Health
3.2. Air Pollutants, Pollen and Occupational Health
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kolek, F.; Plaza, M.D.P.; Leier-Wirtz, V.; Friedmann, A.; Traidl-Hoffmann, C.; Damialis, A. Earlier Flowering of Betula pendula Roth in Augsburg, Germany, Due to Higher Temperature, NO2 and Urbanity, and Relationship with Betula spp. Pollen Season. Int. J. Environ. Res. Public Health 2021, 18, 10325. [Google Scholar] [CrossRef] [PubMed]
- Monsalve, F.; Tomás, C.; Fraile, R. Influence of meteorological parameters and air pollutants onto the morbidity due to respiratory diseases in Castilla-La Mancha, Spain. Aerosol Air Qual. Res. 2013, 13, 1297–1312. [Google Scholar] [CrossRef]
- Oduber, F.; Calvo, A.I.; Blanco-Alegre, C.; Castro, A.; Vega-Maray, A.M.; Valencia-Barrera, R.M.; Fernández-González, D.; Fraile, R. Links between recent trends in airborne pollen concentration, meteorological parameters and air pollutants. Agric. For. Meteorol. 2019, 264, 16–26. [Google Scholar] [CrossRef]
- Gisler, A. Allergies in urban areas on the rise: The combined effect of air pollution and pollen. Int. J. Public Health 2021, 66, 1604022. [Google Scholar] [CrossRef] [PubMed]
- Bobrowska-Korzeniowska, M.; Jerzyńska, J.; Polańska, K.; Kaleta, D.; Stelmach, I.; Kunert, A.; Stelmach, W. The effect of air pollution on the respiratory system in preschool children with contribution of urban heat islands and geographic data–the aim of the study and methodological assumptions. Int. J. Occup. Med. Environ. Health 2021, 34, 453–460. [Google Scholar] [CrossRef] [PubMed]
- Sedghy, F.; Varasteh, A.R.; Sankian, M.; Moghadam, M. Interaction between air pollutants and pollen grains: The role on the rising trend in allergy. Rep. Biochem. Mol. Biol. 2018, 6, 219–224. [Google Scholar]
- Madaniyazi, L.; Xerxes, S. Outdoor air pollution and the onset and exacerbation of asthma. Chronic Dis. Transl. Med. 2021, 7, 100–106. [Google Scholar] [CrossRef]
- Luschkova, D.; Traidl-Hoffmann, C.; Ludwig, A. Climate change and allergies. Allergo J. Int. 2022, 31, 114–120. [Google Scholar] [CrossRef]
- De Weger, L.A.; Bruffaerts, N.; Koenders, M.M.J.F.; Verstraeten, W.W.; Delcloo, A.W.; Hentges, P.; Hentges, F. Long-term pollen monitoring in the Benelux: Evaluation of allergenic pollen levels and temporal variations of pollen seasons. Front. Allergy 2021, 2, 676176. [Google Scholar] [CrossRef]
- Reinmuth-Selzle, K.; Kampf, C.J.; Lucas, K.; Lang-Yona, N.; Fröhlich-Nowoisky, J.; Shiraiwa, M.; Lakey, P.S.J.; Lai, S.; Liu, F.; Kunert, A.T.; et al. Air pollution and climate change effects on allergies in the anthropocene: Abundance, interaction, and modification of allergens and adjuvants. Environ. Sci. Technol. 2017, 51, 4119–4141. [Google Scholar] [CrossRef]
- Puc, M. Influence of meteorological parameters and air pollution on hourly fluctuation of birch (Betula L.) and ash (Fraxinus L.) airborne pollen. Ann. Agric. Environ. Med. 2012, 19, 660–665. [Google Scholar]
- Bosch-Cano, F.; Bernard, N.; Sudre, B.; Gillet, F.; Thibaudon, M.; Richard, H.; Badot, P.M.; Ruffaldi, P. Human exposure to allergenic pollens: A comparison between urban and rural areas. Environ. Res. 2011, 111, 619–625. [Google Scholar] [CrossRef]
- Jiang, F.; Yan, A. Correlation of pollen concentration and meteorological factors with medical condition of allergic rhinitis in Shenyang area. Comput. Math. Methods Med. 2022, 2022, 4619693. [Google Scholar] [CrossRef] [PubMed]
- Plaza, M.P.; Alcázar, P.; Oteros, J.; Galán, C. Atmospheric pollutants and their association with olive and grass aeroallergen concentrations in Córdoba (Spain). Environ. Sci. Pollut. Res. Int. 2020, 27, 45447–45459. [Google Scholar] [CrossRef] [PubMed]
- Anenberg, S.C.; Haines, S.; Wang, E.; Nassikas, N.; Kinney, P.L. Synergistic health effects of air pollution, temperature, and pollen exposure: A systematic review of epidemiological evidence. Environ. Health 2020, 19, 130. [Google Scholar] [CrossRef] [PubMed]
- Sabo, N.Č.; Popović, A.; Dordević, D. Air pollution by pollen grains of anemophilous species: Influence of chemical and meteorological parameters. Water Air Soil Pollut. 2015, 226, 292. [Google Scholar] [CrossRef]
- Piotrowska-Weryszko, K.; Weryszko-Chmielewska, E.; Sulborska, A.; Konarska, A.; Dmitruk, M.; Kaszewski, B.M. Amaranthaceae pollen grains as indicator of climate change in Lublin (Poland). Environ. Res. 2021, 193, 110542. [Google Scholar] [CrossRef] [PubMed]
- Adams-Groom, B.; Selby, K.; Derrett, S.; Frisk, C.A.; Pashley, C.H.; Satchwell, J.; King, D.; McKenzie, G.; Neilson, R. Pollen season trends as markers of climate change impact: Betula, Quercus and Poaceae. Sci. Total Environ. 2022, 831, 154882. [Google Scholar] [CrossRef]
- Batos, B.; Veselinović, M.; Rakonjac, L.; Miljković, D. Morphological properties of pollen as bioindicators of deciduous woody species in Belgrade Parks (Serbia). Topola 2019, 203, 19–30. [Google Scholar]
- Kaur, M.; Nagpal, A.K. Effect of vehicular traffic on pollen size and viability of Apocynaceous plant species. Trop. Plant Res. 2017, 4, 235–241. [Google Scholar] [CrossRef]
- Skjøth, C.A.; Kurganskiy, A.; Grundström, M.; Werner, M.; Adams-Groom, B. Air pollution affecting pollen concentrations through radiative feedback in the atmosphere. Atmosphere 2021, 12, 1376. [Google Scholar] [CrossRef]
- Baldacci, S.; Maio, S.; Cerrai, S.; Sarno, G.; Baïz, N.; Simoni, M.; Annesi-Maesano, I.; Viegi, G. Allergy and asthma: Effects of the exposure to particulate matter and biological allergens. Respir. Med. 2015, 109, 1089–1104. [Google Scholar] [CrossRef] [PubMed]
- Schiavoni, G.; D’Amato, G.; Afferni, C. The dangerous liaison between pollens and pollution in respiratory allergy. Ann. Allergy Asthma Immunol. 2017, 118, 269–275. [Google Scholar] [CrossRef] [PubMed]
- Vasilevskaya, N. Pollution of the environment and pollen: A review. Stresses 2022, 2, 515–530. [Google Scholar] [CrossRef]
- Zhou, S.; Wang, X.; Lu, S.; Yao, C.; Zhang, L.; Rao, L.; Liu, X.; Zhang, W.; Li, S.; Wang, W.; et al. Characterization of allergenicity of Platanus pollen allergen a 3 (Pla a 3) after exposure to NO2 and O3. Environ. Pollut. 2021, 278, 116913. [Google Scholar] [CrossRef]
- Beggs, P.J. Climate change, aeroallergens, and the aeroexposome. Environ. Res. Lett. 2021, 16, 035006. [Google Scholar] [CrossRef]
- Zhao, F.; Elkelish, A.; Durner, J.; Lindermayr, C.; Winkler, J.B.; Ruёff, F.; Behrendt, H.; Traidl-Hoffmann, C.; Holzinger, A.; Kofler, W.; et al. Common ragweed (Ambrosia artemisiifolia L.): Allergenicity and molecular characterization of pollen after plant exposure to elevated NO2. Plant Cell Environ. 2016, 39, 147–164. [Google Scholar] [CrossRef]
- Hong, Q.; Zhou, S.; Zhao, H.; Peng, J.; Li, Y.; Shang, Y.; Wu, M.; Zhang, W.; Lu, S.; Li, S.; et al. Allergenicity of recombinant Humulus japonicus pollen allergen 1 after combined exposure to ozone and nitrogen dioxide. Environ. Pollut. 2018, 234, 707–715. [Google Scholar] [CrossRef] [PubMed]
- Grundström, M.; Dahl, Å.; Ou, T.; Chen, D.; Pleijel, H. The relationship between birch pollen, air pollution and weather types and their effect on antihistamine purchase in two Swedish cities. Aerobiologia 2017, 33, 457–471. [Google Scholar] [CrossRef]
- Elagoz, W.; Manning, W.J. Responses of sensitive and tolerant bush beans (Phaseolus vulgaris L.) to ozone in open-top chambers are influenced by phenotypic differences, morphological characteristics, and the chamber environment. Environ. Pollut. 2005, 136, 371–383. [Google Scholar] [CrossRef]
- Cuinica, L.G.; Abreu, I.; Gomes, C.R.; Esteves da Silva, J.C.G. Exposure of Betula pendula Roth pollen to atmospheric pollutants 2013. CO, O3 and SO2. Grana 2013, 52, 299–304. [Google Scholar] [CrossRef]
- Depciuch, J.; Kasprzyk, I.; Roga, E.; Parlinska-Wojtan, M. Analysis of morphological and molecular composition changes in allergenic Artemisia vulgaris L. pollen under traffic pollution using SEM and FTIR spectroscopy. Environ. Sci. Pollut. Res. Int. 2016, 23, 23203–23214. [Google Scholar] [CrossRef]
- Grewling, L.; Frątczak, A.; Kostecki, L.; Nowak, M.; Szymańska, A.; Bogawski, P. Biological and chemical air pollutants in an urban area of central Europe: Co-exposure assessment. Aerosol Air Qual. Res. 2019, 19, 1526–1537. [Google Scholar] [CrossRef]
- Pereira, S.; Fernández-González, M.; Guedes, A.; Abreu, I.; Ribeiro, H. The strong and the stronger: The effects of increasing ozone and nitrogen dioxide concentrations in pollen of different forest species. Forests 2021, 12, 88. [Google Scholar] [CrossRef]
- Fröhlich-Nowoisky, J.; Kampf, C.J.; Weber, B.; Huffman, J.A.; Pöhlker, C.; Andreae, M.O.; Lang-Yona, N.; Burrows, S.M.; Gunthe, S.S.; Elbert, W.; et al. Bioaerosols in the Earth System: Climate, Health, and Ecosystem Interactions. Atmos. Res. 2016, 182, 346–376. [Google Scholar] [CrossRef]
- Malayeri, B.E.; Noori, M.; Jafari, M. Using the pollen viability and morphology for fluoride pollution biomonitoring. Biol. Trace Elem. Res. 2012, 147, 315–319. [Google Scholar] [CrossRef] [PubMed]
- Mahillon, V.; Saussez, S.; Michel, O. High incidence of sensitization to ornamental plants in allergic rhinitis. Allergy 2006, 61, 1138–1140. [Google Scholar] [CrossRef]
- Sénéchal, H.; Visez, N.; Charpin, D.; Shahali, Y.; Peltre, G.; Biolley, J.P.; Lhuissier, F.; Couderc, R.; Yamada, O.; Malrat-Domenge, A.; et al. A review of the effects of major atmospheric pollutants on pollen grains, pollen content, and allergenicity. Sci. World J. 2015, 2015, 940243. [Google Scholar] [CrossRef] [PubMed]
- Chehregani, A.; Majde, A.; Moin, M.; Gholami, M.; Shariatzadeh, M.A.; Nassiri, H. Increasing allergy potency of Zinnia pollen grains in polluted areas. Ecotoxicol. Environ. Saf. 2004, 58, 267–272. [Google Scholar] [CrossRef]
- Lu, S.; Ren, J.; Hao, X.; Liu, D.; Zhang, R.; Wu, M.; Yi, F.; Lin, J.; Shinich, Y.; Wag, Q. Characterisation of proteins expression of Platanus pollen following exposure to gaseous pollutants and vehicle exhaust particles. Aerobiologia 2014, 30, 281–291. [Google Scholar] [CrossRef]
- Mousavi, F.; Youcef, S.; Pourpak, Z.; Majd, A.; Ghahremaninejad, F. Year-to-year variation of the elemental and allergenic contents of Ailanthus altissima pollen grains: An allergomic study. Environ. Monit. Assess. 2019, 191, 362. [Google Scholar] [CrossRef]
- Visez, N.; Ivanovsky, A.; Roose, A.; Gosselin, S.; Senechal, H.; Poncet, P.; Choël, M. Atmospheric particulate matter adhesion onto pollen: A review. Aerobiologia 2020, 36, 49–62. [Google Scholar] [CrossRef]
- Rezanejad, F.; Ahmad, M.; Seyed, M.; Mostafa, M.; Masoud, A.; Maryam, M. Effect of air pollution on soluble proteins, structure and cellular material release in pollen of Lagerstroemia indica L. (Lytraceae). Acta Biol. Cracoviensia Ser. Bot. 2003, 45, 129–132. [Google Scholar]
- Azzazy, M.F. Environmental impacts of industrial pollution on pollen morphology of Eucalyptus globulus Labill. (Myrtaceae). J. Appl. Biol. Biotechnol. 2016, 4, 57–62. [Google Scholar] [CrossRef]
- Galveias, A.; Costa, A.R.; Bortoli, D.; Alpizar-Jara, R.; Salgado, R.; Costa, M.J.; Antunes, C.M. Cupressaceae pollen in the city of Évora, South of Portugal: Disruption of the pollen during air transport facilitates allergen exposure. Forests 2021, 12, 64. [Google Scholar] [CrossRef]
- Ganga Kailas, J.; Ramakrishna, H.; Seva, B. Pollution effect on pollen morphology in industrial areas of Hyderabad, Telangana state, India. J. Ind. Pollut. Control 2015, 31, 311–314. [Google Scholar]
- Majd, A.; Chehregani, A.; Moin, M.; Gholami, M.; Kohno, S.; Nabe, T.; Shariatzade, M.A. The effects of air pollution on structures, proteins and allergenicity of pollen grains. Aerobiologia 2004, 20, 111–118. [Google Scholar] [CrossRef]
- Rezanejad, F. Air pollution effects on structure, proteins and flavonoids in pollen grains of Thuja orientalis L. (Cupressaceae). Grana 2009, 48, 205–213. [Google Scholar] [CrossRef]
- Shahali, Y.; Pourpak, Z.; Moin, M.; Mari, A.; Majd, A. Instability of the structure and allergenic protein content in Arizona cypress pollen. Allergy 2009, 64, 1773–1779. [Google Scholar] [CrossRef]
- Motta, A.C.; Marliere, M.; Peltre, G.; Sterenberg, P.A.; Lacroix, G. Traffic-related air pollutants induce the release of allergen containing cytoplasmic granules from grass pollen. Int. Arch. Allergy Immunol. 2006, 139, 294–298. [Google Scholar] [CrossRef]
- Kanter, U.; Heller, W.; Durner, J.; Winkler, J.B.; Engel, M.; Behrendt, H.; Holzinger, A.; Braun, P.; Hauser, M.; Ferreira, F.; et al. Molecular and immunological characterization of ragweed (Ambrosia artemisiifolia L.) pollen after exposure of the plants to elevated ozone over a whole growing season. PLoS ONE 2013, 8, e61518. [Google Scholar] [CrossRef] [PubMed]
- Franze, T.; Weller, M.G.; Niessner, R.; Pöschl, U. Protein nitration by polluted air. Environ. Sci. Technol. 2005, 39, 1673–1678. [Google Scholar] [CrossRef] [PubMed]
- Zhu, C.; Farah, J.; Choel, M.; Gosselin, S.; Baroudi, M.; Petitprez, D.; Visez, N. Uptake of ozone and modification of lipids in Betula Pendula pollen. Environ. Pollut. 2018, 242, 880–886. [Google Scholar] [CrossRef]
- Pukacki, P.M.; Chałupka, W. Environmental pollution changes in membrane lipids, antioxidants and vitality of scots pine (Pinus sylvestris L.) pollen. Acta Soc. Bot. Pol. 2003, 72, 99–104. [Google Scholar] [CrossRef]
- Sousa, R.; Duque, L.; Duarte, A.J.; Gomes, C.R.; Ribeiro, H.; Cruz, A.; Silva, J.C.G.E.; Abreu, I. In vitro exposure of Acer negundo pollen to atmospheric levels of SO2 and NO2: Effects on allergenicity and germination. Environ. Sci. Technol. 2012, 46, 2406–2412. [Google Scholar] [CrossRef] [PubMed]
- Sinha, M.; Singh, R.P.; Kushwaha, G.S.; Iqbal, N.; Singh, A.; Kaushink, S.; Kaur, P.; Sharma, S.; Sigh, T.P. Current overview of allergens of plant pathogenesis related protein families. Sci. World J. 2014, 2014, 543195. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, H.; Costa, C.; Abreu, I.; da Silva, J.C.E. Effect of O3 and NO2 atmospheric pollutants on Platanus x acerifolia pollen: Immunochemical and spectroscopic analysis. Sci. Total Environ. 2017, 599–600, 291–297. [Google Scholar] [CrossRef]
- Alscher, R.G.; Donahue, J.L.; Cramer, C.L. Reactive oxygen species and antioxidants: Relationships in green cells. Physiol. Plant 1997, 100, 224–233. [Google Scholar] [CrossRef]
- Ackaert, C.; Kofler, S.; Horejs-Hoeck, J.; Zulehner, N.; Asam, C.; von Grafenstein, S.; Fuchs, J.E.; Briza, P.; Liedl, K.R.; Bohle, B.; et al. The impact of nitration on the structure and immunogenicity of the major birch pollen allergen Bet v 1.0101. PLoS ONE 2014, 9, e104520. [Google Scholar] [CrossRef]
- Karle, A.C.; Oostingh, G.J.; Mutschlechner, S.; Ferreira, F.; Lackner, P.; Bohle, B.; Fischer, G.F.; Vogt, A.B.; Dusch, A. Nitration of the pollen allergen bet v10101 enhances the presentation of bet v1-derived peptides by HLA-DR onhuman dendritic cells. PLoS ONE 2012, 7, e31483. [Google Scholar] [CrossRef]
- Møller, I.M.; Jensen, P.E.; Hansson, A. Oxidative Modifications to Cellular Components in Plants. Annu. Rev. Plant Biol. 2007, 58, 459–481. [Google Scholar] [CrossRef]
- Gupta, M.K.; Uhm, S.J.; Lee, H.T. Effect of vitrification and beta-mercaptoethanol on reactive oxygen species activity and in vitro development of oocytes vitrified before or after in vitro fertilization. Fertil. Steril. 2010, 93, 2602–2607. [Google Scholar] [CrossRef] [PubMed]
- Risse, U.; Tomczok, J.; Huss-Marp, J.; Darsow, U.; Behrendt, H. Health relevant interaction between airborne particulate matter and aeroallergens pollen. J. Aerosol Sci. 2000, 31, 27–28. [Google Scholar] [CrossRef]
- Bashir, M.E.H.; Lui, J.H.; Palnivelu, R.; Naclerio, R.M.; Preuss, D. Pollen lipidomics: Lipid profiling exposes a notable diversity in 22 allergenic pollen and potential biomarkers of the allergic immune response. PLoS ONE 2013, 8, e57566. [Google Scholar] [CrossRef]
- Traidl-Hoffmann, C.; Kasche, A.; Menzel, A.; Jakob, T.; Thiel, M.; Ring, J.; Behrendt, H. Impact of pollen on human health: More than allergen carriers? Int. Arch. Allergy Immunol. 2003, 131, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Gilles-Stein, S.; Beck, I.; Chaker, A.; Bas, M.; McIntyre, M.; Cifuentes, L.; Petersen, A.; Gutermuth, J.; Schmidt-Weber, C.; Behrendt, H.; et al. Pollen derived low molecular compounds enhance the human allergen specific immune response in vivo. Clin. Exp. Allergy 2016, 46, 1355–1365. [Google Scholar] [CrossRef]
- Beck, I.; Jochner, S.; Gilles, S.; McIntyre, M.; Buters, J.T.; Schmidt-Weber, C.; Behrendt, H.; Ring, J.; Menzel, A.; Traidl-Hoffmann, C. High environmental ozone levels lead to enhanced allergenicity of birch pollen. PLoS ONE 2013, 8, e80147. [Google Scholar] [CrossRef]
- Frank, U.; Ernst, D. Effects of NO2 and ozone on pollen allergenicity. Front. Plant Sci. 2016, 7, 91. [Google Scholar] [CrossRef]
- Mogensen, J.E.; Wimmer, R.; Larsen, J.N.; Spangfort, M.D.; Otzen, D.E. The major birch allergen, Bet v 1, shows affinity for a broad spectrum of physiological ligands. J. Biol. Chem. 2002, 277, 23684–23692. [Google Scholar] [CrossRef]
- Henricsson, S.; Westerholm, R.; Nilsson, S.; Berggren, B. Chemical characterisation of extractable compounds found in the coating of birch (betula) pollen. Grana 1996, 35, 179–184. [Google Scholar] [CrossRef]
- Naas, O.; Mendez, M.; Quijada, M.; Gosselin, S.; Farah, J.; Choukri, A.; Visez, N. Chemical modification of coating of Pinus halepensis pollen by ozone exposure. Environ. Pollut. 2016, 214, 816–821. [Google Scholar] [CrossRef] [PubMed]
- Chichiriccò, G.; Picozzi, P. Reversible inhibition of the pollen germination and the stigma penetration in Crocus vernus ssp. vernus (Iridaceae) following fumigations with NO2, CO, and O3 gases. Plant Biol. 2007, 9, 730–735. [Google Scholar] [CrossRef] [PubMed]
- Darbah, J.N.; Kubiske, M.E.; Nelson, N.; Oksanen, E.; Vaapavuori, E.; Karnosky, D.F. Impacts of elevated atmospheric CO2 and O3 on paper birch (Betula papyrifera): Reproductive fitness. Sci.World J. 2007, 7, 240–246. [Google Scholar] [CrossRef] [PubMed]
- Wolters, J.H.B.; Martens, M.J.M. Effects of air pollutants on pollen. Bot. Rev. 1987, 53, 372–414. [Google Scholar] [CrossRef]
- Pasqualini, S.; Tedeschini, E.; Frenguelli, G.; Wopfner, N.; Ferreira, F.; D’Amato, G.; Ederli, L. Ozone affects pollen viability and NAD(P)H oxidase release from Ambrosia artemisiifolia pollen. Environ. Pollut. 2011, 159, 2823–2830. [Google Scholar] [CrossRef]
- Leghari, S.K.; Saeed, S.; Asrar, M.; Ahmed, A.; Tariq, I.; Marri, A.A.; Sadiq, N.; Baloch, A.; Latif, A.; Shawani, N.A. Response of sweet cherry (Prunus avium L.) pollen grains to vehicular exhaust pollution at quetta, balochistan, pakistan. Appl. Ecol. Environ. Res. 2018, 16, 4387–4399. [Google Scholar] [CrossRef]
- Du Bay, D.T.; Murdy, W.H. The impact of sulfur dioxide on plant sexual reproduction: In vivo and in vitro effects compared. J. Environ. Qual. 1983, 12, 147–149. [Google Scholar] [CrossRef]
- Gottardini, E.; Cristofolini, F.; Paoletti, E.; Lazzeri, P.; Pepponi, G. Pollen viability for air pollution bio-monitoring. J. Atmos. Chem. 2004, 49, 149–159. [Google Scholar] [CrossRef]
- Black, V.J.; Black, C.R.; Roberts, J.A.; Stewart, C.A. Impact of the ozone on the reproductive development of plants. New Phytol. 2000, 147, 421–447. [Google Scholar] [CrossRef]
- Stone, S.L.; Gifford, D.J. Structural and biochemical changes in loblolly pine (Pinus taeda L.) seeds during germination and early seedling growth. II. Storage triacylglycerols and carbohydrates. Int. J. Plant Sci. 1999, 160, 663–671. [Google Scholar] [CrossRef]
- Hussain, M.; Kubiske, M.E.; Connor, K.F. Germination of CO2 enriched Pinus taeda L. seeds and subsequent seedling growth responses to CO2 enrichment. Funct. Ecol. 2001, 15, 344–350. [Google Scholar] [CrossRef]
- Ladeau, S.L.; Clark, J.S. Elevated CO2 and tree fecundity: The role of tree size, interannual variability, and population heterogeneity. Glob. Chang. Biol. 2006, 12, 822–833. [Google Scholar] [CrossRef]
- Ziemianin, M.; Waga, J.; Czarnobilska, E.; Myszkowska, D. Changes in qualitative and quantitative traits of birch (Betula pendula) pollen allergenic proteins in relation to the pollution contamination. Environ. Sci. Pollut. Res. 2021, 28, 39952–39965. [Google Scholar] [CrossRef]
- Ouyang, Y.; Xu, Z.; Fan, E.; Li, Y.; Zhang, L. Effect of nitrogen dioxide and sulfur dioxide on viability and morphology of oak pollen. Int. Forum Allergy Rhinol. 2016, 6, 95–100. [Google Scholar] [CrossRef] [PubMed]
- Tashpulatov, A.S.; Clement, P.; Akimcheva, S.A.; Belogradova, K.A.; Barinova, I.; Rakhmawaty, F.D.; Heberle-Bors, E.; Touraev, A. A model system to study the environment-dependent expression of the Bet v 1a gene encoding the major birch pollen allergen. Int. Arch. Allergy Immunol. 2004, 134, 1–9. [Google Scholar] [CrossRef]
- Overmyer, K.; Brosché, M.; Pellinen, R.; Kuittinen, T.; Tuominen, H.; Ahlfors, R.; Keinänen, M.; Saarma, M.; Scheel, D.; Kangasjärvi, J. Ozone-induced programmed cell death in the Arabidopsis radical-induced cell death1 mutant. Plant Physiol. 2005, 137, 1092–1104. [Google Scholar] [CrossRef] [PubMed]
- Bryce, M.; Drews, O.; Schenk, M.; Menzel, A.; Estrella, N.; Wiechenmeier, I.; Smulders, M.J.M.; Buters, J.; Ring, J.; Gorg, A.; et al. Impact of urbanization on the proteome of birch pollen and its chemotactic activity on human granulocytes. Int. Arch. Allergy Immunol. 2010, 151, 46–55. [Google Scholar] [CrossRef]
- Chichiriccò, G. Viability-germinability of Crocus (Iridaceae) pollen in relation to cyto- and ecophysiological factors. Flora 2000, 195, 193–199. [Google Scholar] [CrossRef]
- Roshchina, V.V.; Mel’nikova, E.V. Pollen chemosensitivity to ozone and peroxides. Russ. J. Plant Physiol. 2001, 48, 74–83. [Google Scholar] [CrossRef]
- Tiotiu, A.I.; Novakova, P.; Nedeva, D.; Chong-Neto, H.J.; Novakova, S.; Steiropoulos, P.; Kowal, K. Impact of air pollution on asthma outcomes. Int. J. Environ. Res. Public Health. 2020, 17, 6212. [Google Scholar] [CrossRef] [PubMed]
- Guarnieri, M.; Balmes, J.R. Outdoor air pollution and asthma. Lancet 2014, 383, 1581–1592. [Google Scholar] [CrossRef] [PubMed]
- Urrutia-Pereira, M.; Guidos-Fogelbach, G.; Solé, D. Climate changes, air pollution and allergic diseases in childhood and adolescence. J. Pediatr. 2022, 98 (Suppl. S1), S47–S54. [Google Scholar] [CrossRef] [PubMed]
- Aldakheel, F.M. Allergic diseases: A comprehensive review on risk factors, immunological mechanisms, link with COVID-19, potential treatments, and role of allergen bioinformatics. Int. J. Environ. Res. Public Health 2021, 18, 12105. [Google Scholar] [CrossRef] [PubMed]
- Bartra, J.; Mullol, J.; del Cuvillo, A.; Dávila, I.; Ferrer, M.; Jáuregui, I.; Montoro, J.; Sastre, J.; Valero, A. Air pollution and allergens. J. Investig. Allergol. Clin. Immunol. 2007, 17, 3–8. [Google Scholar] [PubMed]
- Shin, Y.H.; Hwang, J.; Kwon, R.; Lee, S.W.; Kim, M.S.; Shin, J.I.; Yon, D.K.; GBD 2019 Allergic Disorders Collaborators. Global, regional, and national burden of allergic disorders and their risk factors in 204 countries and territories, from 1990 to 2019: A systematic analysis for the Global Burden of Disease Study 2019. Allergy 2023, 78, 2232–2254. [Google Scholar] [CrossRef] [PubMed]
- Mazur, M.; Czarnobilska, M.; Dyga, W.; Czarnobilska, E. Trends in the epidemiology of allergic diseases of the airways in children growing up in an urban agglomeration. J. Clin. Med. 2022, 11, 2188. [Google Scholar] [CrossRef] [PubMed]
- González-Díaz, S.N.; Arias-Cruz, A.; Macouzet-Sánchez, C.; Partida-Ortega, A.B. Impact of air pollution in respiratory allergic diseases. Med. Univ. 2016, 18, 212–215. [Google Scholar] [CrossRef]
- D’Amato, G.; Bergmann, K.C.; Cecchi, L.; Annesi-Maesano, I.; Sanduzzi, A.; Liccardi, G.; Vitale, C.; Stanziola, A.; D’Amato, M. Climate change and air pollution: Effects on pollen allergy and other allergic respiratory diseases. Allergo J. Int. 2014, 23, 17–23. [Google Scholar] [CrossRef]
- Takizawa, H. Impact of air pollution on allergic diseases. Korean J. Intern. Med. 2011, 26, 262–273. [Google Scholar] [CrossRef]
- Gleason, J.A.; Bielory, L.; Fagliano, J.A. Associations between ozone, PM2.5, and four pollen types on emergency department pediatric asthma events during the warm season in New Jersey: A case-crossover study. Environ. Res. 2014, 132, 421–429. [Google Scholar] [CrossRef]
- Zhang, R.; Duhl, T.; Salam, M.T.; House, J.M.; Flagan, R.C.; Avol, E.L.; Gilliland, F.D.; Guenther, A.; Chung, S.H.; Lamb, B.K.; et al. Development of a regional-scale pollen emission and transport modeling framework for investigating the impact of climate change on allergic airway disease. Biogeosciences 2013, 10, 3977–4023. [Google Scholar] [CrossRef]
- Li, C.H.; Sayeau, K.; Ellis, A.K. Air pollution and allergic rhinitis: Role in symptom exacerbation and strategies for management. J. Asthma Allergy 2020, 13, 285–292. [Google Scholar] [CrossRef] [PubMed]
- Licari, A.; Castagnoli, R.; Brambilla, I.; Marseglia, A.; Tosca, M.A.; Marseglia, G.L.; Ciprandi, G. Asthma endotyping and biomarkers in childhood asthma. Pediatr. Allergy Immunol. Pulmonol. 2018, 31, 44–55. [Google Scholar] [CrossRef]
- D’Amato, G.; Holgate, S.T.; Pawankar, R.; Ledford, D.K.; Cecchi, L.; Al-Ahmad, M.; Al-Enezi, F.; Al-Muhsen, S.; Ansotegui, I.; Baena-Cagnani, C.E.; et al. Meteorological conditions, climate change, new emerging factors, and asthma and related allergic disorders. A statement of the World Allergy Organization. World Allergy Organ J. 2015, 8, 25. [Google Scholar] [CrossRef]
- Gehrig, R.; Clot, B. 50 years of pollen monitoring in Basel (Switzerland) demonstrate the influence of climate change on airborne pollen. Front. Allergy 2021, 2, 677159. [Google Scholar] [CrossRef]
- López-Orozco, R.; García-Mozo, H.; Oteros, J.; Galan, C. Long-term trends in atmospheric quercus pollen related to climate change in southern Spain: A 25-year perspective. Atmos. Environ. 2021, 262, 118637. [Google Scholar] [CrossRef]
- Hoflich, C.; Balakirski, G.; Hajdu, Z.; Baron, J.M.; Kaiser, L.; Czaja, K.; Merk, H.F.; Gerdsen, S.; Strassen, U.; Bas, M.; et al. Potential health risk of allergenic pollen with climate change associated spreading capacity: Ragweed and olive sensitization in two German federal states. Int. J. Hyg. Environ. Health. 2016, 219, 252–260. [Google Scholar] [CrossRef] [PubMed]
- Price, D.; Hughes, K.M.; Thien, F.; Suphioglu, C. Epidemic Thunderstorm Asthma: Lessons learned from the storm down-under. J. Allergy Clin. Immunol. Pract. 2021, 9, 1510–1515. [Google Scholar] [CrossRef]
- D’Amato, G.; Annesi-Maesano, I.; Urrutia-Pereira, M.; Del Giacco, S.; Rosario Filho, N.A.; Chong-Neto, H.J.; Solé, D.; Ansotegui, I.; Cecchi, L.; Sanduzzi Zamparelli, A.; et al. Thunderstorm allergy and asthma: State of the art. Multidiscip. Respir. Med. 2021, 16, 806. [Google Scholar] [CrossRef] [PubMed]
- Knox, R.B. Grass pollen, thunderstorms and asthma. Clin. Exp. Allergy 1993, 23, 354–359. [Google Scholar] [CrossRef]
- Stępalska, D.; Myszkowska, D.; Piotrowicz, K.; Kasprzyk, I. The phenological phases of flowering and pollen seasons of spring flowering tree taxa against a background of meteorological conditions in Kraków, Poland. Acta Agrobot. 2016, 65, 1678. [Google Scholar] [CrossRef]
- Puc, M.; Kasprzyk, I. The patterns of Corylus and Alnus pollen seasons and pollination periods in two Polish cities located in different climatic regions. Aerobiologia 2013, 29, 495–511. [Google Scholar] [CrossRef]
- Bogdziewicz, M.; Fernandez-Martinez, M.; Bonal, R.; Belmonte, J.; Espelta, J.M. The moran effect and environmental vetoes: Phenological synchrony and drought drive seed production in a mediterranean oak. Proc. R. Soc. B 2017, 284, 20171784. [Google Scholar] [CrossRef] [PubMed]
- Levetin, E.; Van de Water, P. Changing pollen types/concentrations/distribution in the United States: Fact or fiction? Curr. Allergy Asthma Rep. 2008, 8, 418–424. [Google Scholar] [CrossRef] [PubMed]
- Zemmer, F.; Dahl, Å.; Galán, C. The duration and severity of the allergenic pollen season in Istanbul, and the role of meteorological factors. Aerobiologia 2022, 38, 195–215. [Google Scholar] [CrossRef]
- Galan, C.; Alcazar, P.; Oteros, J.; Garcia-Mozo, H.; Aira, M.J.; Belmonte, J.; Diaz de la Guardia, C.; Fernandez-Gonzalez, D.; Gutierrez-Bustillo, M.; Moreno-Grau, S.; et al. Airborne pollen trends in the Iberian Peninsula. Sci. Total Environ. 2016, 550, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Aboulaich, N.; Achmakh, L.; Bouziane, H.; Trigo, M.M.; Recio, M.; Kadiri, M.; Cabezudo, B.; Riadi, H.; Kazzaz, M. Effect of meteorological parameters on Poaceae pollen in the atmosphere of Tetouan (NW Morocco). Int. J. Biometeorol. 2013, 57, 197–205. [Google Scholar] [CrossRef]
- Ślusarczyk, J.; Kopacz-Bednarska, A.; Posłowska, J. Influence of meteorological factors on the dynamics of hazel, alder, birch and poplar pollen in the 2021 season in Kielce, Poland. Ann. Agric. Environ. Med. 2022, 29, 502–512. [Google Scholar] [CrossRef]
- Makra, L.; Csepe, Z.; Matyasovszky, I.; Deak, A.J.; Sumeghy, Z.; Tusnady, G. The effects of the current and past meteorological elements influencing the current pollen concentrations for different taxa. Bot. Stud. 2014, 55, 43. [Google Scholar] [CrossRef]
- Ščevková, J.; Dušička, J.; Zahradníková, E.; Sepšiová, R.; Kováč, J.; Vašková, Z. Impact of meteorological parameters and air pollutants on airborne concentration of Betula pollen and Bet v 1 allergen. Environ. Sci. Pollut. Res. Int. 2023, 30, 95438–95448. [Google Scholar] [CrossRef]
- Heinrich, J.; Wichmann, H.E. Traffic related pollutants in Europe and their effect on allergic disease. Curr. Opinion Allergy Clin. Immunol. 2004, 4, 341–348. [Google Scholar] [CrossRef] [PubMed]
- Gonzalo-Garijo, M.A.; Tormo-Molina, R.; Muńoz-Rodrìguez, A.F.; Silva-Palacios, I. Differences in the spatial distribution of airborne pollen concentrations at different urban locations within a city. J. Investig. Allergol. Clin. Immunol. 2006, 16, 37–43. [Google Scholar]
- Platts-Mills, T.A.; Erwin, E.; Heymann, P.; Woodfolk, J. Is the hygiene hypothesis still a viable explanation for the increased prevalence of asthma? Allergy 2005, 60, 25–31. [Google Scholar] [CrossRef]
- Nicolaou, N.; Siddique, N.; Custovic, A. Allergic disease in urban and rural populations: Increasing prevalence with increasing urbanization. Allergy 2005, 60, 1357–1360. [Google Scholar] [CrossRef] [PubMed]
- Czarnobilska, E.; Bulanda, M.; Bulanda, D.; Mazur, M. The Influence of air pollution on the development of allergic inflammation in the airways in Krakow’s atopic and Non-atopic residents. J. Clin. Med. 2021, 10, 2383. [Google Scholar] [CrossRef] [PubMed]
- Veremchuk, L.V.; Tsarouhas, K.; Vitkina, T.I.; Mineeva, E.E.; Gvozdenko, T.A.; Antonyuk, M.V.; Rakitskii, V.N.; Sidletskaya, K.A.; Tsatsakis, A.M.; Golokhvast, K.S. Impact evaluation of environmental factors on respiratory function of asthma patients living in urban territory. Environ. Pollut. 2018, 235, 489–496. [Google Scholar] [CrossRef]
- Stróżek, J.; Samoliński, B.K.; Kłak, A.; Gawińska-Drużba, E.; Izdebski, R.; Krzych-Fałta, E.; Raciborski, F. The indirect costs of allergic diseases. Int. J. Occup. Med. Environ. Health. 2019, 32, 281–290. [Google Scholar] [CrossRef]
- Mimet, A.; Pellsier, V.; Quènol, H.; Aguejdad, R.; Dubreuil, V.; Roze, H. Urbanisation induces early flowering: Evidence from Platanus acerifolia and Prunus cerasus. Int. J. Biometeorol. 2009, 53, 287–298. [Google Scholar] [CrossRef]
- Oliveira, M.; Ribeiro, H.; Delgado, J.L.; Abreu, I. Seasonal and intradiurnal variation of allergenic fungal spores in urban and rural areas of the North of Portugal. Aerobiologia 2009, 25, 85–98. [Google Scholar] [CrossRef]
- Carińanos, P.; Sànchez-Mesa, J.A.; Prieto-Baena, J.C.; López, A.; Guerra, F.; Moreno, C.; Dominguez, E.; Galan, C. Pollen allergy related to the area of residence in the city of Còrdoba, south-west Spain. J. Environ. Monit. 2002, 4, 734–738. [Google Scholar] [CrossRef]
- Kasprzyk, I. Comparative study of seasonal and intradiurnal variation of airborne herbaceous pollen in urban and rural areas. Aerobiologia 2006, 22, 185–195. [Google Scholar] [CrossRef]
- Rodríguez-Rajo, F.J.; Fdez-Sevilla, D.; Stach, A.; Jato, V. Assessment between pollen seasons in areas with different urbanization level related to local vegetation sources and differences in allergen exposure. Aerobiologia 2010, 26, 1–14. [Google Scholar] [CrossRef]
- Ring, J.; Kramer, U.; Schafer, T.; Behrendt, H. Why are allergies increasing? Curr. Opin. Immunol. 2001, 13, 701–708. [Google Scholar] [CrossRef] [PubMed]
- Goyal, A.; Ravindra, K.; Mor, S. Occupational exposure to airborne pollen and associated health risks among gardeners: A perception-based survey. Environ. Sci. Pollut. Res. Int. 2022, 29, 70084–70098. [Google Scholar] [CrossRef] [PubMed]
- Tsui, H.C.; Ronsmans, S.; Hoet, P.H.M.; Nemery, B.; Vanoirbeek, J.A.J. Occupational asthma caused by low-molecular-weight chemicals associated with contact dermatitis: A retrospective study. J. Allergy Clin. Immunol. Pract. 2022, 10, 2346–2354.e4. [Google Scholar] [CrossRef] [PubMed]
- Siegel, J.; Gill, N.; Ramanathan, M., Jr.; Patadia, M. Unified airway disease: Environmental factors. Otolaryngol. Clin. N. Am. 2023, 56, 39–53. [Google Scholar] [CrossRef] [PubMed]
- Anderson, S.E.; Long, C.; Dotson, G.S. Occupational Allergy. Eur. Med. J. 2017, 2, 65–71. [Google Scholar] [CrossRef]
- Peden, D.; Reed, C.E. Environmental and occupational allergies. J. Allergy Clin. Immunol. 2010, 125 (Suppl. S2), S150–S160. [Google Scholar] [CrossRef]
- Tiotiu, A.I.; Novakova, S.; Labor, M.; Emelyanov, A.; Mihaicuta, S.; Novakova, P.; Nedeva, D. Progress in occupational asthma. Int. J. Environ. Res. Public Health 2020, 17, 4553. [Google Scholar] [CrossRef]
- Petsonk, E.L. Work-related asthma and implications for the general public. Environ. Health Perspect. 2002, 110, 569–572. [Google Scholar] [CrossRef]
- Cormier, M.; Lemière, C. Occupational asthma. Int. J. Tuberc. Lung Dis. 2020, 24, 8–21. [Google Scholar] [CrossRef]
- Rabe, K.F.; Adachi, M.; Lai, C.K.W.; Soriano, J.B.; Vermeire, P.A.; Weiss, K.B.; Weiss, S.T. Worldwide severity and control of asthma in children and adults: The global asthma insights and reality surveys. J. Allergy Clin. Immunol. 2004, 114, 40–47. [Google Scholar] [CrossRef]
- Lim, T.; Liss, G.M.; Vernich, L.; Buyantseva, L.; Tarlo, S.M. Work-exacerbated asthma in a workers’ compensation population. Occup. Med. 2014, 64, 206–210. [Google Scholar] [CrossRef] [PubMed]
- D’Ovidio, M.C.; Annesi-Maesano, I.; D’Amato, G.; Cecchi, L. Climate change and occupational allergies: An overview on biological pollution, exposure and prevention. Ann. Ist. Super. Sanità 2016, 52, 406–414. [Google Scholar] [CrossRef]
- Vimercati, L.; Gatti, M.F.; Baldassarre, A.; Nettis, E.; Favia, N.; Palma, M.; Martina, G.L.; Di Leo, E.; Musti, M. Occupational exposure to urban air pollution and allergic diseases. Int. J. Environ. Res. Public Health 2015, 12, 12977–12987. [Google Scholar] [CrossRef]
- Vimercati, L.; Carrus, A.; Bisceglia, L.; Tato, I.; Bellotta, M.R.; Russo, A.; Martina, G.; Daprile, C.; di Leo, E.; Nettis, E.; et al. Biological monitoring and allergic sensitization in traffic police officers exposed to urban air pollution. Int. J. Immunopathol. Pharmacol. 2006, 19, 57–60. [Google Scholar] [PubMed]
- Hu, H.; Xue, M.; Wei, N.; Zheng, P.; Wu, G.; An, N.; Huang, H.; Sun, B. Sensitisation of severe asthma in different occupations: A multicentre study in China. Clin. Respir. J. 2021, 15, 177–186. [Google Scholar] [CrossRef] [PubMed]
- D’Amato, G.; Annesi-Maesano, I.; Biagioni, B.; Lancia, A.; Cecchi, L.; D’Ovidio, M.C.; D’Amato, M. New Developments in climate change, air pollution, pollen allergy, and interaction with SARS-CoV-2. Atmosphere 2023, 14, 848. [Google Scholar] [CrossRef]
- Pelliccioni, A.; Ciardini, V.; Lancia, A.; Di Renzi, S.; Brighetti, M.A.; Travaglini, A.; Capone, P.; D’Ovidio, M.C. Intercomparison of indoor and outdoor pollen concentrations in rural and suburban research workplaces. Sustainability 2021, 13, 8776. [Google Scholar] [CrossRef]
- Ouyang, Y.; Yin, Z.; Li, Y.; Fan, E.; Zhang, L. Associations among air pollutants, grass pollens, and daily number of grass pollen allergen-positive patients: A longitudinal study from 2012 to 2016. Int. Forum Allergy Rhinol. 2019, 9, 1297–1303. [Google Scholar] [CrossRef]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Capone, P.; Lancia, A.; D’Ovidio, M.C. Interaction between Air Pollutants and Pollen Grains: Effects on Public and Occupational Health. Atmosphere 2023, 14, 1544. https://doi.org/10.3390/atmos14101544
Capone P, Lancia A, D’Ovidio MC. Interaction between Air Pollutants and Pollen Grains: Effects on Public and Occupational Health. Atmosphere. 2023; 14(10):1544. https://doi.org/10.3390/atmos14101544
Chicago/Turabian StyleCapone, Pasquale, Andrea Lancia, and Maria Concetta D’Ovidio. 2023. "Interaction between Air Pollutants and Pollen Grains: Effects on Public and Occupational Health" Atmosphere 14, no. 10: 1544. https://doi.org/10.3390/atmos14101544