Polymeric Nanoparticles for Inhaled Vaccines
Abstract
:1. Introduction
2. Nanoparticles for Inhaled Vaccines
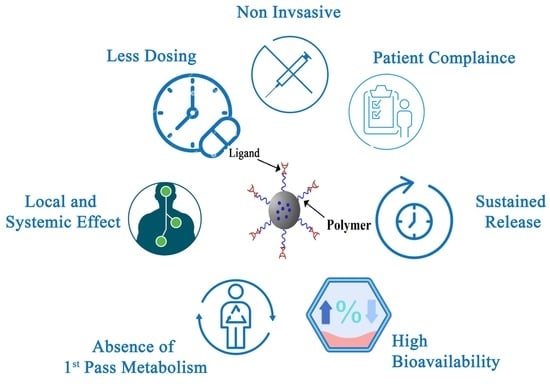
2.1. Polymeric Nanoparticles and Drug Delivery
2.2. Nanoparticles Drug Delivery to the Lungs
2.2.1. Nanoparticles through Different Pulmonary Routes of Administration
Intranasal Delivery
Intratracheal Delivery
Nebulization Delivery
2.2.2. Polymeric Nanoparticles Delivery to the Lungs
Particle Size
Particle Morphology
Electrical Charge
3. Polymeric Nanoparticles Used for Inhaled Vaccination
3.1. Nanoparticles for Inhaled Vaccines
3.2. Chitosan and Chitosan Derivatives Nanoparticles
3.3. Polyesters: PLGA and PLA
4. Polymeric Nanoparticles as Vaccine Adjuvants
5. Challenges of Polymeric Nanoparticles Delivery for Inhaled Vaccination
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kunda, N.K.; Somavarapu, S.; Gordon, S.B.; Hutcheon, G.A.; Saleem, I.Y. Nanocarriers targeting dendritic cells for pulmonary vaccine delivery. Pharm. Res. 2013, 30, 325–341. [Google Scholar] [CrossRef]
- Blank, F.; Stumbles, P.; von Garnier, C. Opportunities and challenges of the pulmonary route for vaccination. Expert Opin. Drug Deliv. 2011, 8, 547–563. [Google Scholar] [CrossRef] [PubMed]
- Kaneko, K.; Osman, N.; Carini, V.; Scagnetti, G.; Saleem, I. Overview of the advantages and disadvantages of different mucosal sites for the delivery of nanoparticles. Mucosal Deliv. Drugs Biol. Nanopart. 2020, 41, 61. [Google Scholar]
- Hellfritzsch, M.; Scherließ, R. Mucosal vaccination via the respiratory tract. Pharmaceutics 2019, 11, 375. [Google Scholar] [CrossRef] [Green Version]
- Trincado, V.; Gala, R.P.; Morales, J.O. Buccal and sublingual vaccines: A review on oral mucosal immunization and delivery systems. Vaccines 2021, 9, 1177. [Google Scholar] [CrossRef] [PubMed]
- Dewangan, H.K. Rational application of nanoadjuvant for mucosal vaccine delivery system. J. Immunol. Methods 2020, 481, 112791. [Google Scholar] [CrossRef]
- Savelkoul, H.F.; Ferro, V.A.; Strioga, M.M.; Schijns, V.E. Choice and design of adjuvants for parenteral and mucosal vaccines. Vaccines 2015, 3, 148–171. [Google Scholar] [CrossRef] [Green Version]
- Han, J.; Zhao, D.; Li, D.; Wang, X.; Jin, Z.; Zhao, K. Polymer-based nanomaterials and applications for vaccines and drugs. Polymers 2018, 10, 31. [Google Scholar] [CrossRef] [Green Version]
- Farzaneh, S.; Ida Idayu, M.; Razieh, N.; Pritam Kumar, D.; Beom Soo, K. Recent progress in polymeric non-invasive insulin delivery. Int. J. Biol. Macromol. 2022, 203, 222–243. [Google Scholar] [CrossRef]
- Li, M.; Wang, Y.; Sun, Y.; Cui, H.; Zhu, S.J.; Qiu, H.-J. Mucosal vaccines: Strategies and challenges. Immunol. Lett. 2020, 217, 116–125. [Google Scholar] [CrossRef]
- Adomako, M.; St-Hilaire, S.; Zheng, Y.; Eley, J.; Marcum, R.; Sealey, W.; Donahower, B.; LaPatra, S.; Sheridan, P. Oral DNA vaccination of rainbow trout, Oncorhynchus mykiss (Walbaum), against infectious haematopoietic necrosis virus using PLGA [Poly (D, L-Lactic-Co-Glycolic Acid)] nanoparticles. J. Fish Dis. 2012, 35, 203–214. [Google Scholar] [CrossRef]
- Jana, P.; Shyam, M.; Singh, S.; Jayaprakash, V.; Dev, A. Biodegradable polymers in drug delivery and oral vaccination. Eur. Polym. J. 2021, 142, 110155. [Google Scholar]
- Jabbal-Gill, I.; Watts, P.; Smith, A. Chitosan-based delivery systems for mucosal vaccines. Expert Opin. Drug Deliv. 2012, 9, 1051–1067. [Google Scholar] [CrossRef] [PubMed]
- Allahyari, M.; Mohit, E. Peptide/protein vaccine delivery system based on PLGA particles. Hum. Vaccines Immunother. 2016, 12, 806–828. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Al-Nemrawi, N.K.; Marques, J.; Tavares, C.J.; Oweis, R.J.; Al-Fandi, M. Synthesis and characterization of photocatalytic polyurethane and poly (methyl methacrylate) microcapsules for the controlled release of methotrexate. Drug Dev. Ind. Pharm. 2018, 44, 2083–2088. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.K.; Upadhyay, P.K.; Kumar, M. Viability of Nanostructured Lipid Carrier System in Overcoming the Barriers Associated with Chemotherapeutic Delivery. Curr. Nanosci. 2022, 18, 587–603. [Google Scholar]
- Pulliam, B.; Sung, J.C.; Edwards, D.A. Design of nanoparticle-based dry powder pulmonary vaccines. Expert Opin. Drug Deliv. 2007, 4, 651–663. [Google Scholar] [CrossRef] [PubMed]
- Mora-Huertas, C.E.; Fessi, H.; Elaissari, A. Polymer-based nanocapsules for drug delivery. Int. J. Pharm. 2010, 385, 113–142. [Google Scholar] [CrossRef] [PubMed]
- Nagavarma, B.; Yadav, H.K.; Ayaz, A.; Vasudha, L.; Shivakumar, H. Different techniques for preparation of polymeric nanoparticles-a review. Asian J. Pharm. Clin. Res. 2012, 5, 16–23. [Google Scholar]
- García, J.M.; García, F.C.; Ruiz, J.A.R.; Vallejos, S.; Trigo-López, M. Smart Polymers: Principles and Applications; Walter de Gruyter GmbH & Co KG: Berlin, Germany, 2022. [Google Scholar]
- Al-Nemrawi, N.; Alsharif, S.; Dave, R.J. Preparation of chitosan-TPP nanoparticles: The influence of chitosan polymeric properties and formulation variables. Int. J. Appl. Pharm. 2018, 10, 60–65. [Google Scholar] [CrossRef] [Green Version]
- Al-Nemrawi, N.K.; Okour, A.R.; Dave, R.H. Surface modification of PLGA nanoparticles using chitosan: Effect of molecular weight, concentration, and degree of deacetylation. Adv. Polym. Technol. 2018, 37, 3066–3075. [Google Scholar] [CrossRef]
- Noreen, S.; Ma, J.-X.; Saeed, M.; Pervaiz, F.; Hanif, M.F.; Ahmed, B.; Farooq, M.I.; Akram, F.; Safdar, M.; Madni, A. Natural polysaccharide-based biodegradable polymeric platforms for transdermal drug delivery system: A critical analysis. Drug Deliv. Transl. Res. 2022, 12, 1–18. [Google Scholar]
- Rytting, E.; Nguyen, J.; Wang, X.; Kissel, T. Biodegradable polymeric nanocarriers for pulmonary drug delivery. Expert Opin. Drug Deliv. 2008, 5, 629–639. [Google Scholar] [CrossRef]
- Wang, M.; Hu, L.; Xu, C. Recent advances in the design of polymeric microneedles for transdermal drug delivery and biosensing. Lab Chip 2017, 17, 1373–1387. [Google Scholar] [CrossRef]
- Vigani, B.; Rossi, S.; Sandri, G.; Bonferoni, M.C.; Caramella, C.M.; Ferrari, F. Recent advances in the development of in situ gelling drug delivery systems for non-parenteral administration routes. Pharmaceutics 2020, 12, 859. [Google Scholar] [CrossRef]
- Rao, J.P.; Geckeler, K.E. Polymer nanoparticles: Preparation techniques and size-control parameters. Prog. Polym. Sci. 2011, 36, 887–913. [Google Scholar]
- Li, Q.; Cai, T.; Huang, Y.; Xia, X.; Cole, S.P.; Cai, Y. A review of the structure, preparation, and application of NLCs, PNPs, and PLNs. Nanomaterials 2017, 7, 122. [Google Scholar] [CrossRef] [PubMed]
- Brown, L.R. Commercial challenges of protein drug delivery. Expert Opin. Drug Deliv. 2005, 2, 29–42. [Google Scholar] [CrossRef]
- Jaradat, E.; Weaver, E.; Meziane, A.; Lamprou, D.A. Microfluidics technology for the design and formulation of nanomedicines. Nanomaterials 2021, 11, 3440. [Google Scholar] [CrossRef]
- Al-Nemrawi, N.K.; Alshraiedeh, N.A.H.; Zayed, A.L.; Altaani, B.M. Low molecular weight chitosan-coated PLGA nanoparticles for pulmonary delivery of tobramycin for cystic fibrosis. Pharmaceuticals 2018, 11, 28. [Google Scholar] [CrossRef] [Green Version]
- Lim, Y.H.; Tiemann, K.M.; Hunstad, D.A.; Elsabahy, M.; Wooley, K.L. Polymeric nanoparticles in development for treatment of pulmonary infectious diseases. WIREs Nanomed. Nanobiotechnol. 2016, 8, 842–871. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steichen, S.D.; Caldorera-Moore, M.; Peppas, N.A. A review of current nanoparticle and targeting moieties for the delivery of cancer therapeutics. Eur. J. Pharm. Sci. 2013, 48, 416–427. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zazo, H.; Colino, C.I.; Lanao, J.M. Current applications of nanoparticles in infectious diseases. J. Control. Release 2016, 224, 86–102. [Google Scholar] [PubMed]
- Nasir, A.; Kausar, A.; Younus, A. A review on preparation, properties and applications of polymeric nanoparticle-based materials. Polym.-Plast. Technol. Eng. 2015, 54, 325–341. [Google Scholar] [CrossRef]
- Pulingam, T.; Foroozandeh, P.; Chuah, J.-A.; Sudesh, K. Exploring Various Techniques for the Chemical and Biological Synthesis of Polymeric Nanoparticles. Nanomaterials 2022, 12, 576. [Google Scholar] [CrossRef]
- Dammak, I.; Sobral, P.J.d.A.; Aquino, A.; Neves, M.A.d.; Conte-Junior, C.A. Nanoemulsions: Using emulsifiers from natural sources replacing synthetic ones—A review. Compr. Rev. Food Sci. Food Saf. 2020, 19, 2721–2746. [Google Scholar] [CrossRef]
- Paliwal, R.; Babu, R.J.; Palakurthi, S. Nanomedicine scale-up technologies: Feasibilities and challenges. Aaps Pharmscitech 2014, 15, 1527–1534. [Google Scholar] [CrossRef] [Green Version]
- Dormont, F.; Rouquette, M.; Mahatsekake, C.; Gobeaux, F.; Peramo, A.; Brusini, R.; Calet, S.; Testard, F.; Lepetre-Mouelhi, S.; Desmaële, D. Translation of nanomedicines from lab to industrial scale synthesis: The case of squalene-adenosine nanoparticles. J. Control. Release 2019, 307, 302–314. [Google Scholar] [CrossRef]
- Tena, A.F.; Clarà, P.C. Deposition of inhaled particles in the lungs. Arch. Bronconeumol. 2012, 48, 240–246. [Google Scholar] [CrossRef]
- Koullapis, P.; Kassinos, S.C.; Bivolarova, M.P.; Melikov, A.K. Particle deposition in a realistic geometry of the human conducting airways: Effects of inlet velocity profile, inhalation flowrate and electrostatic charge. J. Biomech. 2016, 49, 2201–2212. [Google Scholar] [CrossRef] [Green Version]
- Paranjpe, M.; Müller-Goymann, C.C. Nanoparticle-mediated pulmonary drug delivery: A review. Int. J. Mol. Sci. 2014, 15, 5852–5873. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Müller-Goymann, C.C.; Paranjpe, M. Nanodrugs in medicine and healthcare: Pulmonary, nasal and ophthalmic routes, and vaccination. Pharm. Nanotechnol. Innov. Prod. Innov. Prod. 2017, 633–648. [Google Scholar]
- Blank, F.; Fytianos, K.; Seydoux, E.; Rodriguez-Lorenzo, L.; Petri-Fink, A.; Von Garnier, C.; Rothen-Rutishauser, B. Interaction of biomedical nanoparticles with the pulmonary immune system. J. Nanobiotechnol. 2017, 15, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carvalho, T.C.; Peters, J.I.; Williams, R.O., III. Influence of particle size on regional lung deposition–what evidence is there? Int. J. Pharm. 2011, 406, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Sosnowski, T.R. Inhaled aerosols: Their role in COVID-19 transmission, including biophysical interactions in the lungs. Curr. Opin. Colloid Interface Sci. 2021, 54, 101451. [Google Scholar] [CrossRef]
- Ngan, C.L.; Asmawi, A.A. Lipid-based pulmonary delivery system: A review and future considerations of formulation strategies and limitations. Drug Deliv. Transl. Res. 2018, 8, 1527–1544. [Google Scholar] [CrossRef]
- Forest, V.; Pourchez, J. Nano-delivery to the lung-by inhalation or other routes and why nano when micro is largely sufficient? Adv. Drug Deliv. Rev. 2022, 183, 114173. [Google Scholar]
- Forest, V.; Pourchez, J. Preferential binding of positive nanoparticles on cell membranes is due to electrostatic interactions: A too simplistic explanation that does not take into account the nanoparticle protein corona. Mater. Sci. Eng. C 2017, 70, 889–896. [Google Scholar] [CrossRef]
- Amidi, M.; Mastrobattista, E.; Jiskoot, W.; Hennink, W.E. Chitosan-based delivery systems for protein therapeutics and antigens. Adv. Drug Deliv. Rev. 2010, 62, 59–82. [Google Scholar] [CrossRef]
- Illum, L. Nasal drug delivery—Possibilities, problems and solutions. J. Control. Release 2003, 87, 187–198. [Google Scholar] [CrossRef]
- Soane, R.; Hinchcliffe, M.; Davis, S.; Illum, L. Clearance characteristics of chitosan based formulations in the sheep nasal cavity. Int. J. Pharm. 2001, 217, 183–191. [Google Scholar] [CrossRef]
- Johansson, P.; Wang, T.; Collet, B.; Corripio-Miyar, Y.; Monte, M.M.; Secombes, C.J.; Zou, J. Identification and expression modulation of a C-type lectin domain family 4 homologue that is highly expressed in monocytes/macrophages in rainbow trout (Oncorhynchus mykiss). Dev. Comp. Immunol. 2016, 54, 55–65. [Google Scholar] [CrossRef] [PubMed]
- Patton, J.S.; Byron, P.R. Inhaling medicines: Delivering drugs to the body through the lungs. Nat. Rev. Drug Discov. 2007, 6, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Jones, A.T.; Gumbleton, M.; Duncan, R. Understanding endocytic pathways and intracellular trafficking: A prerequisite for effective design of advanced drug delivery systems. Adv. Drug Deliv. Rev. 2003, 55, 1353–1357. [Google Scholar] [CrossRef]
- Xiang, S.D.; Scholzen, A.; Minigo, G.; David, C.; Apostolopoulos, V.; Mottram, P.L.; Plebanski, M. Pathogen recognition and development of particulate vaccines: Does size matter? Methods 2006, 40, 1–9. [Google Scholar] [CrossRef]
- Hardy, C.L.; LeMasurier, J.S.; Belz, G.T.; Scalzo-Inguanti, K.; Yao, J.; Xiang, S.D.; Kanellakis, P.; Bobik, A.; Strickland, D.H.; Rolland, J.M. Inert 50-nm polystyrene nanoparticles that modify pulmonary dendritic cell function and inhibit allergic airway inflammation. J. Immunol. 2012, 188, 1431–1441. [Google Scholar] [CrossRef] [Green Version]
- Holt, P.G.; Strickland, D.H.; Wikström, M.E.; Jahnsen, F.L. Regulation of immunological homeostasis in the respiratory tract. Nat. Rev. Immunol. 2008, 8, 142–152. [Google Scholar] [CrossRef]
- Kopf, M.; Schneider, C.; Nobs, S.P. The development and function of lung-resident macrophages and dendritic cells. Nat. Immunol. 2015, 16, 36–44. [Google Scholar] [CrossRef]
- Vermaelen, K.; Pauwels, R. Pulmonary dendritic cells. Am. J. Respir. Crit. Care Med. 2005, 172, 530–551. [Google Scholar] [CrossRef]
- Fytianos, K.; Drasler, B.; Blank, F.; Garnier, C.v.; Seydoux, E.; Rodriguez-Lorenzo, L.; Petri-Fink, A.; Rothen-Rutishauser, B. Current in vitro approaches to assess nanoparticle interactions with lung cells. Nanomedicine 2016, 11, 2457–2469. [Google Scholar] [CrossRef] [Green Version]
- Joana, M.S.; Mafalda, V.; Rogério, G.; Véronique, P.; Helena, F.F. Immune system targeting by biodegradable nanoparticles for cancer vaccines. J. Control. Release 2013, 168, 179–199. [Google Scholar] [CrossRef]
- Zhou, Y.; Zhang, Y.; Yao, Z.; Moorman, J.P.; Jia, Z. Dendritic cell-based immunity and vaccination against hepatitis C virus infection. Immunology 2012, 136, 385–396. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mao, L.; Chen, Z.; Wang, Y.; Chen, C. Design and application of nanoparticles as vaccine adjuvants against human corona virus infection. J. Inorg. Biochem. 2021, 219, 111454. [Google Scholar] [CrossRef] [PubMed]
- Kuek, L.E.; Lee, R.J. First contact: The role of respiratory cilia in host-pathogen interactions in the airways. Am. J. Physiol. Lung Cell. Mol. Physiol. 2020, 319, L603–L619. [Google Scholar] [CrossRef]
- Grassin-Delyle, S.; Buenestado, A.; Naline, E.; Faisy, C.; Blouquit-Laye, S.; Couderc, L.-J.; Le Guen, M.; Fischler, M.; Devillier, P. Intranasal drug delivery: An efficient and non-invasive route for systemic administration: Focus on opioids. Pharmacol. Ther. 2012, 134, 366–379. [Google Scholar] [CrossRef]
- Veronesi, M.C.; Alhamami, M.; Miedema, S.B.; Yun, Y.; Ruiz-Cardozo, M.; Vannier, M.W. Imaging of intranasal drug delivery to the brain. Am. J. Nucl. Med. Mol. Imaging 2020, 10, 1. [Google Scholar]
- Ali, J.; Ali, M.; Baboota, S.; Kaur Sahni, J.; Ramassamy, C.; Dao, L. Potential of nanoparticulate drug delivery systems by intranasal administration. Curr. Pharm. Des. 2010, 16, 1644–1653. [Google Scholar] [CrossRef]
- Popescu, R.; Ghica, M.V.; Dinu-Pîrvu, C.-E.; Anuța, V.; Lupuliasa, D.; Popa, L. New opportunity to formulate intranasal vaccines and drug delivery systems based on chitosan. Int. J. Mol. Sci. 2020, 21, 5016. [Google Scholar] [CrossRef]
- Petkar, K.C.; Patil, S.M.; Chavhan, S.S.; Kaneko, K.; Sawant, K.K.; Kunda, N.K.; Saleem, I.Y. An overview of nanocarrier-based adjuvants for vaccine delivery. Pharmaceutics 2021, 13, 455. [Google Scholar] [CrossRef]
- Boroumand, H.; Badie, F.; Mazaheri, S.; Seyedi, Z.S.; Nahand, J.S.; Nejati, M.; Baghi, H.B.; Abbasi-Kolli, M.; Badehnoosh, B.; Ghandali, M. Chitosan-based nanoparticles against viral infections. Front. Cell. Infect. Microbiol. 2021, 11, 643953. [Google Scholar] [CrossRef]
- Chaturvedi, M.; Kumar, M.; Pathak, K. A review on mucoadhesive polymer used in nasal drug delivery system. J. Adv. Pharm. Technol. Res. 2011, 2, 215. [Google Scholar] [CrossRef] [PubMed]
- Morimoto, Y.; Izumi, H.; Yoshiura, Y.; Fujishima, K.; Yatera, K.; Yamamoto, K. Usefulness of intratracheal instillation studies for estimating nanoparticle-induced pulmonary toxicity. Int. J. Mol. Sci. 2016, 17, 165. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chatzikleanthous, D.; O’Hagan, D.T.; Adamo, R. Lipid-based nanoparticles for delivery of vaccine adjuvants and antigens: Toward multicomponent vaccines. Mol. Pharm. 2021, 18, 2867–2888. [Google Scholar] [CrossRef] [PubMed]
- Song, X.; Zhang, W.; Zhai, L.; Guo, J.; Zhao, Y.; Zhang, L.; Hu, L.; Xiong, X.; Zhou, D.; Lv, M. Aerosolized Intratracheal Inoculation of Recombinant Protective Antigen (rPA) Vaccine Provides Protection Against Inhalational Anthrax in B10. D2-Hc0 Mice. Front. Immunol. 2022, 103. [Google Scholar] [CrossRef]
- Chesson, C.B.; Ekpo-Otu, S.; Endsley, J.J.; Rudra, J.S. Biomaterials-based vaccination strategies for the induction of CD8+ T cell responses. ACS Biomater. Sci. Eng. 2017, 3, 126–143. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.H.; Brooks, P.; Johnson, S.; Tompkins, S.M.; Custer, K.M.; Haas, D.L.; Mair, R.; Papania, M.; Tripp, R.A. Aerosol vaccination induces robust protective immunity to homologous and heterologous influenza infection in mice. Vaccine 2011, 29, 2568–2575. [Google Scholar] [CrossRef] [Green Version]
- Lu, D.; Hickey, A.J. Pulmonary vaccine delivery. Expert Rev. Vaccines 2007, 6, 213–226. [Google Scholar] [CrossRef]
- Thomas, C.; Rawat, A.; Hope-Weeks, L.; Ahsan, F. Aerosolized PLA and PLGA nanoparticles enhance humoral, mucosal and cytokine responses to hepatitis B vaccine. Mol. Pharm. 2011, 8, 405–415. [Google Scholar] [CrossRef]
- Khatri, L.; Taylor, K.; Craig, D.; Palin, K. An assessment of jet and ultrasonic nebulisers for the delivery of lactate dehydrogenase solutions. Int. J. Pharm. 2001, 227, 121–131. [Google Scholar] [CrossRef]
- Bennett, J.V.; Fernandez de Castro, J.; Valdespino-Gomez, J.L.; Garcia-Garcia, M.d.L.; Islas-Romero, R.; Echaniz-Aviles, G.; Jimenez-Corona, A.; Sepulveda-Amor, J. Aerosolized measles and measles-rubella vaccines induce better measles antibody booster responses than injected vaccines: Randomized trials in Mexican schoolchildren. Bull. World Health Organ. 2002, 80, 806–812. [Google Scholar]
- Wong-Chew, R.M.; Islas-Romero, R.; de Lourdes García-García, M.; Beeler, J.A.; Audet, S.; Santos-Preciado, J.I.; Gans, H.; Lew-Yasukawa, L.; Maldonado, Y.A.; Arvin, A.M. Immunogenicity of aerosol measles vaccine given as the primary measles immunization to nine-month-old Mexican children. Vaccine 2006, 24, 683–690. [Google Scholar] [CrossRef] [PubMed]
- Ely, L.; Roa, W.; Finlay, W.H.; Löbenberg, R. Effervescent dry powder for respiratory drug delivery. Eur. J. Pharm. Biopharm. 2007, 65, 346–353. [Google Scholar] [CrossRef] [PubMed]
- Pandey, M.; Choudhury, H.; Yi, C.X.; Mun, C.W.; Phing, G.K.; Rou, G.X.; Singh, B.J.K.A.; Jeet, P.A.; Jhee, A.N.; Chin, L.K. Recent updates on novel approaches in insulin drug delivery: A review of challenges and pharmaceutical implications. Curr. Drug Targets 2018, 19, 1782–1800. [Google Scholar] [CrossRef]
- Gill, S.; Löbenberg, R.; Ku, T.; Azarmi, S.; Roa, W.; Prenner, E.J. Characteristics, mechanisms of action, and toxicity in pulmonary drug delivery—A review. J. Biomed. Nanotechnol. 2007, 3, 107–119. [Google Scholar] [CrossRef]
- Ponkshe, P.; Thakkar, R.A.; Mulay, T.; Joshi, R.; Javia, A.; Amrutiya, J.; Chougule, M. Nasal and pulmonary drug delivery systems. Vitr. Vivo Tools Drug Deliv. Res. Optim. Clin. Outcomes 2018, 10, 79–134. [Google Scholar]
- Sharma, M.; Waghela, S.; Mhatre, R.; Saraogi, G.K. A Recent Update on Intranasal Delivery of High Molecular Weight Proteins, Peptides, and Hormones. Curr. Pharm. Des. 2021, 27, 4279–4299. [Google Scholar] [CrossRef] [PubMed]
- Douafer, H.; Andrieu, V.; Brunel, J.M. Scope and limitations on aerosol drug delivery for the treatment of infectious respiratory diseases. J. Control. Release 2020, 325, 276–292. [Google Scholar] [CrossRef] [PubMed]
- Demoly, P.; Hagedoorn, P.; de Boer, A.H.; Frijlink, H.W. The clinical relevance of dry powder inhaler performance for drug delivery. Respir. Med. 2014, 108, 1195–1203. [Google Scholar] [CrossRef] [Green Version]
- Dessanges, J.-F. A history of nebulization. J. Aerosol Med. 2001, 14, 65–71. [Google Scholar] [CrossRef]
- de Boer, A.H.; Hagedoorn, P.; Hoppentocht, M.; Buttini, F.; Grasmeijer, F.; Frijlink, H.W. Dry powder inhalation: Past, present and future. Expert Opin. Drug Deliv. 2017, 14, 499–512. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- LiCalsi, C.; Christensen, T.; Bennett, J.V.; Phillips, E.; Witham, C.J.V. Dry powder inhalation as a potential delivery method for vaccines. Vaccine 1999, 17, 1796–1803. [Google Scholar] [CrossRef]
- White, S.; Bennett, D.B.; Cheu, S.; Conley, P.W.; Guzek, D.B.; Gray, S.; Howard, J.; Malcolmson, R.; Parker, J.M.; Roberts, P.; et al. EXUBERA®: Pharmaceutical development of a novel product for pulmonary delivery of insulin. Diabetes Technol. Ther. 2005, 7, 896–906. [Google Scholar] [CrossRef] [PubMed]
- Newman, S.P. Drug delivery to the lungs: Challenges and opportunities. Ther. Deliv. 2017, 8, 647–661. [Google Scholar] [CrossRef] [PubMed]
- Lederer, K.; Castaño, D.; Atria, D.G.; Oguin, T.H., 3rd; Wang, S.; Manzoni, T.B.; Muramatsu, H.; Hogan, M.J.; Amanat, F.; Cherubin, P.; et al. SARS-CoV-2 mRNA Vaccines Foster Potent Antigen-Specific Germinal Center Responses Associated with Neutralizing Antibody Generation. Immunity 2020, 53, 1281–1295.e1285. [Google Scholar] [CrossRef]
- Kis, Z.; Shattock, R.; Shah, N.; Kontoravdi, C. Emerging Technologies for Low-Cost, Rapid Vaccine Manufacture. Biotechnol. J. 2019, 14, 1800376. [Google Scholar] [CrossRef] [Green Version]
- Park, J.W.; Lagniton, P.N.P.; Liu, Y.; Xu, R.H. mRNA vaccines for COVID-19: What, why and how. Int. J. Biol. Sci. 2021, 17, 1446–1460. [Google Scholar] [CrossRef]
- Lim, M.; Badruddoza, A.Z.M.; Firdous, J.; Azad, M.; Mannan, A.; Al-Hilal, T.A.; Cho, C.-S.; Islam, M.A. Engineered Nanodelivery Systems to Improve DNA Vaccine Technologies. Pharmaceutics 2020, 12, 30. [Google Scholar] [CrossRef] [Green Version]
- Rauch, S.; Jasny, E.; Schmidt, K.E.; Petsch, B. New Vaccine Technologies to Combat Outbreak Situations. Front. Immunol. 2018, 9, 1963. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tenchov, R.; Bird, R.; Curtze, A.E.; Zhou, Q. Lipid Nanoparticles─From Liposomes to mRNA Vaccine Delivery, a Landscape of Research Diversity and Advancement. ACS Nano 2021, 15, 16982–17015. [Google Scholar] [CrossRef] [PubMed]
- Liang, Y.; Huang, L.; Liu, T. Development and Delivery Systems of mRNA Vaccines. Front. Bioeng. Biotechnol. 2021, 9, 718753. [Google Scholar] [CrossRef] [PubMed]
- Pardi, N.; Hogan, M.J.; Naradikian, M.S.; Parkhouse, K.; Cain, D.W.; Jones, L.; Moody, M.A.; Verkerke, H.P.; Myles, A.; Willis, E.; et al. Nucleoside-modified mRNA vaccines induce potent T follicular helper and germinal center B cell responses. J. Exp. Med. 2018, 215, 1571–1588. [Google Scholar] [CrossRef]
- Hassani, Z.; Lemkine, G.F.; Erbacher, P.; Palmier, K.; Alfama, G.; Giovannangeli, C.; Behr, J.-P.; Demeneix, B.A. Lipid-mediated siRNA delivery down-regulates exogenous gene expression in the mouse brain at picomolar levels. J. Gene Med. 2005, 7, 198–207. [Google Scholar] [CrossRef] [PubMed]
- Zhao, M.; Li, M.; Zhang, Z.; Gong, T.; Sun, X. Induction of HIV-1 gag specific immune responses by cationic micelles mediated delivery of gag mRNA. Drug Deliv. 2016, 23, 2596–2607. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, M.Q.; Alves, P.M.; Roldão, A. Functionalizing Ferritin Nanoparticles for Vaccine Development. Pharmaceutics 2021, 13, 1621. [Google Scholar] [CrossRef] [PubMed]
- Muralidharan, P.; Malapit, M.; Mallory, E.; Hayes, D., Jr.; Mansour, H.M. Inhalable nanoparticulate powders for respiratory delivery. Nanomed. Nanotechnol. Biol. Med. 2015, 11, 1189–1199. [Google Scholar] [CrossRef] [Green Version]
- Sung, J.C.; Pulliam, B.L.; Edwards, D.A. Nanoparticles for drug delivery to the lungs. Trends Biotechnol. 2007, 25, 563–570. [Google Scholar] [CrossRef] [PubMed]
- Heyder, J.; Gebhart, J.; Rudolf, G.; Schiller, C.F.; Stahlhofen, W.J. Deposition of particles in the human respiratory tract in the size range 0.005–15 μm. J. Aerosol Sci. 1986, 17, 811–825. [Google Scholar] [CrossRef]
- Byron, P.R. Prediction of drug residence times in regions of the human respiratory tract following aerosol inhalation. J. Pharm. Sci. 1986, 75, 433–438. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; Guan, J.; Qin, L.; Zhang, X.; Mao, S. Physicochemical properties affecting the fate of nanoparticles in pulmonary drug delivery. Drug Discov. Today 2020, 25, 150–159. [Google Scholar] [CrossRef] [PubMed]
- Patton, J.S.; Brain, J.D.; Davies, L.A.; Fiegel, J.; Gumbleton, M.; Kim, K.-J.; Sakagami, M.; Vanbever, R.; Ehrhardt, C. The particle has landed—Characterizing the fate of inhaled pharmaceuticals. J. Aerosol Med. Pulm. Drug Deliv. 2010, 23, S71–S87. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Praphawatvet, T.; Peters, J.I.; Williams, R.O., III. Inhaled nanoparticles—An updated review. Int. J. Pharm. 2020, 587, 119671. [Google Scholar] [CrossRef] [PubMed]
- Best, J.P.; Yan, Y.; Caruso, F. The role of particle geometry and mechanics in the biological domain. Adv. Healthc. Mater. 2012, 1, 35–47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chatterjee, N.; Flury, M. Effect of particle shape on capillary forces acting on particles at the air–water interface. Langmuir 2013, 29, 7903–7911. [Google Scholar] [CrossRef] [PubMed]
- Mazumdar, S.; Chitkara, D.; Mittal, A. Exploration and insights into the cellular internalization and intracellular fate of amphiphilic polymeric nanocarriers. Acta Pharm. Sin. B 2021, 11, 903–924. [Google Scholar] [CrossRef] [PubMed]
- Lin, X.; Zuo, Y.Y.; Gu, N. Shape affects the interactions of nanoparticles with pulmonary surfactant. Sci. China Mater. 2015, 58, 28–37. [Google Scholar] [CrossRef] [PubMed]
- Aramrak, S.; Flury, M.; Harsh, J.B.; Zollars, R.L.; Davis, H.P. Does colloid shape affect detachment of colloids by a moving air–water interface? Langmuir 2013, 29, 5770–5780. [Google Scholar] [CrossRef] [PubMed]
- Kato, T.; Yashiro, T.; Murata, Y.; Herbert, D.C.; Oshikawa, K.; Bando, M.; Ohno, S.; Sugiyama, Y. Evidence that exogenous substances can be phagocytized by alveolar epithelial cells and transported into blood capillaries. Cell Tissue Res. 2003, 311, 47–51. [Google Scholar] [CrossRef] [PubMed]
- Nemmar, A.; Vanbilloen, H.; Hoylaerts, M.; Hoet, P.; Verbruggen, A.; Nemery, B. Passage of intratracheally instilled ultrafine particles from the lung into the systemic circulation in hamster. Am. J. Respir. Crit. Care Med. 2001, 164, 1665–1668. [Google Scholar] [CrossRef]
- Harush-Frenkel, O.; Bivas-Benita, M.; Nassar, T.; Springer, C.; Sherman, Y.; Avital, A.; Altschuler, Y.; Borlak, J.; Benita, S. A safety and tolerability study of differently-charged nanoparticles for local pulmonary drug delivery. Toxicol. Appl. Pharmacol. 2010, 246, 83–90. [Google Scholar] [CrossRef]
- Bivas-Benita, M.; Ottenhoff, T.H.; Junginger, H.E.; Borchard, G. Pulmonary DNA vaccination: Concepts, possibilities and perspectives. J. Control. Release 2005, 107, 1–29. [Google Scholar] [CrossRef]
- Xing, L.; Zhou, T.-J.; Fan, Y.-T.; He, Y.-j.; Pang, T.; Cho, K.-H.; Lu, J.-J.; Jiang, H.-L.; Cho, C.-S. Efficient mucosal immunization by mucoadhesive and ph-sensitive polymeric vaccine delivery system. Macromol. Res. 2019, 27, 215–226. [Google Scholar] [CrossRef]
- Stevceva, L.; Abimiku, A.; Franchini, G. Targeting the mucosa: Genetically engineered vaccines and mucosal immune responses. Genes Immun. 2000, 1, 308–315. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- López-Santiago, R.; Sánchez-Argáez, A.B.; De Alba-Núñez, L.G.; Baltierra-Uribe, S.L.; Moreno-Lafont, M.C. Immune response to mucosal brucella infection. Front. Immunol. 2019, 10, 1759. [Google Scholar] [CrossRef] [PubMed]
- Ogra, P.L.; Faden, H.; Welliver, R.C. Vaccination strategies for mucosal immune responses. Clin. Microbiol. Rev. 2001, 14, 430–445. [Google Scholar] [CrossRef] [Green Version]
- McNeela, E.A.; Mills, K.H. Manipulating the immune system: Humoral versus cell-mediated immunity. Adv. Drug Deliv. Rev. 2001, 51, 43–54. [Google Scholar] [CrossRef]
- Manjarrez-Zavala, M.E.; Rosete-Olvera, D.P.; Gutiérrez-González, L.H.; Ocadiz-Delgado, R.; Cabello-Gutiérrez, C. Pathogenesis of viral respiratory infection. Respir. Dis. Infect. A New Insight 2013, 1, 3–32. [Google Scholar]
- Mitchell, M.J.; Billingsley, M.M.; Haley, R.M.; Wechsler, M.E.; Peppas, N.A.; Langer, R. Engineering precision nanoparticles for drug delivery. Nat. Rev. Drug Discov. 2021, 20, 101–124. [Google Scholar] [CrossRef]
- Mahler, H.-C.; Müller, R.; Frieβ, W.; Delille, A.; Matheus, S. Induction and analysis of aggregates in a liquid IgG1-antibody formulation. Eur. J. Pharm. Biopharm. 2005, 59, 407–417. [Google Scholar] [CrossRef] [PubMed]
- Schüle, S.; Schulz-Fademrecht, T.; Garidel, P.; Bechtold-Peters, K.; Frieß, W. Stabilization of IgG1 in spray-dried powders for inhalation. Eur. J. Pharm. Biopharm. 2008, 69, 793–807. [Google Scholar] [CrossRef]
- Ohtake, S.; Martin, R.A.; Yee, L.; Chen, D.; Kristensen, D.D.; Lechuga-Ballesteros, D.; Truong-Le, V.J.V. Heat-stable measles vaccine produced by spray drying. Vaccine 2010, 28, 1275–1284. [Google Scholar] [CrossRef]
- Garmise, R.J.; Hickey, A.J. Dry powder nasal vaccines as an alternative to needle-based delivery. Crit. Rev. Ther. Drug Carr. Syst. 2009, 26, 1–27. [Google Scholar]
- Garcia-Contreras, L.; Wong, Y.-L.; Muttil, P.; Padilla, D.; Sadoff, J.; DeRousse, J.; Germishuizen, W.A.; Goonesekera, S.; Elbert, K.; Bloom, B.R. Immunization by a bacterial aerosol. Proc. Natl. Acad. Sci. USA 2008, 105, 4656–4660. [Google Scholar] [CrossRef] [Green Version]
- Smith, D.J.; Bot, S.; Dellamary, L.; Bot, A. Evaluation of novel aerosol formulations designed for mucosal vaccination against influenza virus. Vaccine 2003, 21, 2805–2812. [Google Scholar] [CrossRef]
- Niwa, T.; Takeuchi, H.; Hino, T.; Kunou, N.; Kawashima, Y. Preparations of biodegradable nanospheres of water-soluble and insoluble drugs with D, L-lactide/glycolide copolymer by a novel spontaneous emulsification solvent diffusion method, and the drug release behavior. J. Control. Release 1993, 25, 89–98. [Google Scholar] [CrossRef]
- Bolhassani, A.; Safaiyan, S.; Rafati, S. Improvement of different vaccine delivery systems for cancer therapy. Mol. Cancer 2011, 10, 1–20. [Google Scholar] [CrossRef]
- Krishnamachari, Y.; Geary, S.M.; Lemke, C.D.; Salem, A.K. Nanoparticle delivery systems in cancer vaccines. Pharm. Res. 2011, 28, 215–236. [Google Scholar] [CrossRef] [PubMed]
- Hamdy, S.; Haddadi, A.; Hung, R.W.; Lavasanifar, A. Targeting dendritic cells with nano-particulate PLGA cancer vaccine formulations. Adv. Drug Deliv. Rev. 2011, 63, 943–955. [Google Scholar] [CrossRef] [PubMed]
- Mody, K.T.; Popat, A.; Mahony, D.; Cavallaro, A.S.; Yu, C.; Mitter, N.J.N. Mesoporous silica nanoparticles as antigen carriers and adjuvants for vaccine delivery. Nanoscale 2013, 5, 5167–5179. [Google Scholar] [CrossRef] [PubMed]
- Juan, A.; Cimas, F.J.; Bravo, I.; Pandiella, A.; Ocaña, A.; Alonso-Moreno, C. An overview of antibody conjugated polymeric nanoparticles for breast cancer therapy. Pharmaceutics 2020, 12, 802. [Google Scholar] [CrossRef] [PubMed]
- Ye, Q.N.; Wang, Y.; Shen, S.; Xu, C.F.; Wang, J. Biomaterials-Based Delivery of Therapeutic Antibodies for Cancer Therapy. Adv. Healthc. Mater. 2021, 10, 2002139. [Google Scholar] [CrossRef] [PubMed]
- He, Q.; Mitchell, A.R.; Johnson, S.L.; Wagner-Bartak, C.; Morcol, T.; Bell, S.J.D. Calcium phosphate nanoparticle adjuvant. Clin. Diagn. Lab. Immunol. 2000, 7, 899–903. [Google Scholar] [CrossRef] [Green Version]
- Slütter, B.; Soema, P.C.; Ding, Z.; Verheul, R.; Hennink, W.; Jiskoot, W. Conjugation of ovalbumin to trimethyl chitosan improves immunogenicity of the antigen. J. Control. Release 2010, 143, 207–214. [Google Scholar] [CrossRef]
- Ghotbi, Z.; Haddadi, A.; Hamdy, S.; Hung, R.W.; Samuel, J.; Lavasanifar, A. Active targeting of dendritic cells with mannan-decorated PLGA nanoparticles. J. Drug Target. 2011, 19, 281–292. [Google Scholar] [CrossRef] [PubMed]
- Wibowo, N. Engineering Viral Capsomeres as a Vaccine Platform. Ph.D. Thesis, The University of Queensland, Brisbane, Australia, 2012. [Google Scholar]
- Shima, F.; Uto, T.; Akagi, T.; Akashi, M. Synergistic stimulation of antigen presenting cells via TLR by combining CpG ODN and poly (γ-glutamic acid)-based nanoparticles as vaccine adjuvants. Bioconjug. Chem. 2013, 24, 926–933. [Google Scholar] [CrossRef] [PubMed]
- Foged, C.; Brodin, B.; Frokjaer, S.; Sundblad, A. Particle size and surface charge affect particle uptake by human dendritic cells in an in vitro model. Int. J. Pharm. 2005, 298, 315–322. [Google Scholar] [CrossRef] [PubMed]
- Joshi, V.B.; Geary, S.M.; Salem, A.K. Biodegradable particles as vaccine delivery systems: Size matters. AAPS J. 2013, 15, 85–94. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, H.; Uto, T.; Akagi, T.; Baba, M.; Akashi, M. Amphiphilic Poly (Amino Acid) Nanoparticles Induce Size-Dependent Dendritic Cell Maturation. Adv. Funct. Mater. 2010, 20, 3925–3931. [Google Scholar] [CrossRef]
- Kohli, A.; Alpar, H. Potential use of nanoparticles for transcutaneous vaccine delivery: Effect of particle size and charge. Int. J. Pharm. 2004, 275, 13–17. [Google Scholar] [CrossRef] [PubMed]
- Gheibi Hayat, S.M.; Darroudi, M. Nanovaccine: A novel approach in immunization. J. Cell. Physiol. 2019, 234, 12530–12536. [Google Scholar] [CrossRef]
- Figueiredo, L.; Cadete, A.; Gonçalves, L.; Corvo, M.; Almeida, A. Intranasal immunisation of mice against Streptococcus equi using positively charged nanoparticulate carrier systems. Vaccine 2012, 30, 6551–6558. [Google Scholar] [CrossRef] [PubMed]
- Champion, J.A.; Mitragotri, S.J. Role of target geometry in phagocytosis. Proc. Natl. Acad. Sci. USA 2006, 103, 4930–4934. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Niikura, K.; Matsunaga, T.; Suzuki, T.; Kobayashi, S.; Yamaguchi, H.; Orba, Y.; Kawaguchi, A.; Hasegawa, H.; Kajino, K.; Ninomiya, T. Gold nanoparticles as a vaccine platform: Influence of size and shape on immunological responses in vitro and in vivo. ACS Nano 2013, 7, 3926–3938. [Google Scholar] [CrossRef] [PubMed]
- Mansoor, F.; Earley, B.; Cassidy, J.P.; Markey, B.; Foster, C.; Doherty, S.; Welsh, M.D. Intranasal delivery of nanoparticles encapsulating BPI3V proteins induces an early humoral immune response in mice. Res. Vet. Sci. 2014, 96, 551–557. [Google Scholar] [CrossRef] [PubMed]
- Gebril, A.M.; Lamprou, D.A.; Alsaadi, M.M.; Stimson, W.H.; Mullen, A.B.; Ferro, V.A. Assessment of the antigen-specific antibody response induced by mucosal administration of a GnRH conjugate entrapped in lipid nanoparticles. Nanomed. Nanotechnol. Biol. Med. 2014, 10, e971–e979. [Google Scholar] [CrossRef] [PubMed]
- Yao, W.; Peng, Y.; Du, M.; Luo, J.; Zong, L. Preventative vaccine-loaded mannosylated chitosan nanoparticles intended for nasal mucosal delivery enhance immune responses and potent tumor immunity. Mol. Pharm. 2013, 10, 2904–2914. [Google Scholar] [CrossRef] [PubMed]
- Nanda, R.K.; Hajam, I.A.; Edao, B.M.; Ramya, K.; Rajangam, M.; Sekar, S.C.; Ganesh, K.; Bhanuprakash, V.; Kishore, S. Immunological evaluation of mannosylated chitosan nanoparticles based foot and mouth disease virus DNA vaccine, pVAC FMDV VP1–OmpA in guinea pigs. Biologicals 2014, 42, 153–159. [Google Scholar] [CrossRef]
- Sawaengsak, C.; Mori, Y.; Yamanishi, K.; Mitrevej, A.; Sinchaipanid, N. Chitosan nanoparticle encapsulated hemagglutinin-split influenza virus mucosal vaccine. AAPS PharmSciTech 2014, 15, 317–325. [Google Scholar] [CrossRef] [Green Version]
- Verma, A.; Gupta, A.; Mittal, A. Development and Characterization of Bipolymer Based Nanoparticulate Carrier System as Vaccine Adjuvant for Effective Immunization. Ph.D. Thesis, Lovely Professional University, Punjab, India, 2015. [Google Scholar]
- Sharma, S.; Benson, H.A.; Mukkur, T.K.; Rigby, P.; Chen, Y. Preliminary studies on the development of IgA-loaded chitosan–dextran sulphate nanoparticles as a potential nasal delivery system for protein antigens. J. Microencapsul. 2013, 30, 283–294. [Google Scholar] [CrossRef] [PubMed]
- Tafaghodi, M.; Saluja, V.; Kersten, G.F.; Kraan, H.; Slütter, B.; Amorij, J.-P.; Jiskoot, W. Hepatitis B surface antigen nanoparticles coated with chitosan and trimethyl chitosan: Impact of formulation on physicochemical and immunological characteristics. Vaccine 2012, 30, 5341–5348. [Google Scholar] [CrossRef]
- Dhillon, G.S.; Kaur, S.; Brar, S.K.; Verma, M. Green synthesis approach: Extraction of chitosan from fungus mycelia. Crit. Rev. Biotechnol. 2013, 33, 379–403. [Google Scholar] [CrossRef] [PubMed]
- Zargar, V.; Asghari, M.; Dashti, A. A review on chitin and chitosan polymers: Structure, chemistry, solubility, derivatives, and applications. ChemBioEng Rev. 2015, 2, 204–226. [Google Scholar] [CrossRef]
- Al-Nemrawi, N.; Nimrawi, S. A novel formulation of chitosan nanoparticles functionalized with titanium dioxide nanoparticles. J. Adv. Pharm. Technol. Res. 2021, 12, 402. [Google Scholar] [CrossRef] [PubMed]
- Gao, P.; Xia, G.; Bao, Z.; Feng, C.; Cheng, X.; Kong, M.; Liu, Y.; Chen, X. Chitosan based nanoparticles as protein carriers for efficient oral antigen delivery. Int. J. Biol. Macromol. 2016, 91, 716–723. [Google Scholar] [CrossRef] [PubMed]
- Justin, T.H.; Samuel, K.L. PEGylation for enhancing nanoparticle diffusion in mucus. Adv. Drug Deliv. Rev. 2018, 124, 125–139. [Google Scholar] [CrossRef]
- Twana Mohammed, M.W.; Sergey, K.F.; Samarendra, M.; Mathias, G.; Michal, C.; Richard, H.; Stephen, K.; Wing Man, L.; Vitaliy, V.K. Mucus-penetrating nanoparticles based on chitosan grafted with various non-ionic polymers: Synthesis, structural characterisation and diffusion studies. J. Colloid Interface Sci. 2022, 626, 251–264. [Google Scholar] [CrossRef]
- Watts, P.; Smith, A.; Hinchcliffe, M. ChiSys® as a chitosan-based delivery platform for nasal vaccination. In Mucosal Delivery of Biopharmaceuticals; Springer: Berlin/Heidelberg, Germany, 2014; pp. 499–516. [Google Scholar]
- Al-Nemrawi, N.K.; Alsharif, S.S.; Alzoubi, K.H.; Alkhatib, R.Q. Preparation and characterization of insulin chitosan-nanoparticles loaded in buccal films. Pharm. Dev. Technol. 2019, 24, 967–974. [Google Scholar] [CrossRef] [PubMed]
- Lebre, F.; Borchard, G.; Faneca, H.; Pedroso de Lima, M.; Borges, O. Intranasal administration of novel chitosan nanoparticle/DNA complexes induces antibody response to hepatitis B surface antigen in mice. Mol. Pharm. 2016, 13, 472–482. [Google Scholar] [CrossRef] [PubMed]
- Rampino, A.; Borgogna, M.; Blasi, P.; Bellich, B.; Cesàro, A. Chitosan nanoparticles: Preparation, size evolution and stability. Int. J. Pharm. 2013, 455, 219–228. [Google Scholar] [CrossRef] [PubMed]
- Lai, W.-F.; Lin, M.C.-M. Nucleic acid delivery with chitosan and its derivatives. J. Control. Release 2009, 134, 158–168. [Google Scholar] [CrossRef] [PubMed]
- Bivas-Benita, M.; van Meijgaarden, K.E.; Franken, K.L.; Junginger, H.E.; Borchard, G.; Ottenhoff, T.H.; Geluk, A. Pulmonary delivery of chitosan-DNA nanoparticles enhances the immunogenicity of a DNA vaccine encoding HLA-A* 0201-restricted T-cell epitopes of Mycobacterium tuberculosis. Vaccine 2004, 22, 1609–1615. [Google Scholar] [CrossRef] [PubMed]
- Van der Lubben, I.; Verhoef, J.; Borchard, G.; Junginger, H. Chitosan for mucosal vaccination. Adv. Drug Deliv. Rev. 2001, 52, 139–144. [Google Scholar] [CrossRef]
- Zhao, K.; Chen, G.; Shi, X.-m.; Gao, T.-t.; Li, W.; Zhao, Y.; Zhang, F.-q.; Wu, J.; Cui, X.; Wang, Y.-F. Preparation and efficacy of a live newcastle disease virus vaccine encapsulated in chitosan nanoparticles. PLoS ONE 2012, 7, e53314. [Google Scholar] [CrossRef] [Green Version]
- Jabbal-Gill, I.; Fisher, A.N.; Rappuoli, R.; Davis, S.S.; Illum, L. Stimulation of mucosal and systemic antibody responses against Bordetella pertussis filamentous haemagglutinin and recombinant pertussis toxin after nasal administration with chitosan in mice. Vaccine 1998, 16, 2039–2046. [Google Scholar] [CrossRef]
- Ilium, L. Chitosan and its use as a pharmaceutical excipient. Pharm. Res. 1998, 15, 1326–1331. [Google Scholar] [CrossRef] [PubMed]
- Dhakal, S.; Renu, S.; Ghimire, S.; Shaan Lakshmanappa, Y.; Hogshead, B.T.; Feliciano-Ruiz, N.; Lu, F.; HogenEsch, H.; Krakowka, S.; Lee, C.W. Mucosal immunity and protective efficacy of intranasal inactivated influenza vaccine is improved by chitosan nanoparticle delivery in pigs. Front. Immunol. 2018, 9, 934. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Borges, O.; Cordeiro-da-Silva, A.; Tavares, J.; Santarém, N.; de Sousa, A.; Borchard, G.; Junginger, H.E. Immune response by nasal delivery of hepatitis B surface antigen and codelivery of a CpG ODN in alginate coated chitosan nanoparticles. Eur. J. Pharm. Biopharm. 2008, 69, 405–416. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McNeela, E.A.; O’Connor, D.; Jabbal-Gill, I.; Illum, L.; Davis, S.S.; Pizza, M.; Peppoloni, S.; Rappuoli, R.; Mills, K.H. A mucosal vaccine against diphtheria: Formulation of cross reacting material (CRM197) of diphtheria toxin with chitosan enhances local and systemic antibody and Th2 responses following nasal delivery. Vaccine 2000, 19, 1188–1198. [Google Scholar] [CrossRef]
- Xu, J.; Dai, W.; Wang, Z.; Chen, B.; Li, Z.; Fan, X. Intranasal vaccination with chitosan-DNA nanoparticles expressing pneumococcal surface antigen a protects mice against nasopharyngeal colonization by Streptococcus pneumoniae. Clin. Vaccine Immunol. 2011, 18, 75–81. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vila, A.; Sánchez, A.; Janes, K.; Behrens, I.; Kissel, T.; Jato, J.L.V.; Alonso, M.J. Low molecular weight chitosan nanoparticles as new carriers for nasal vaccine delivery in mice. Eur. J. Pharm. Biopharm. 2004, 57, 123–131. [Google Scholar] [CrossRef] [PubMed]
- Vila, A.; Sanchez, A.; Tobıo, M.; Calvo, P.; Alonso, M. Design of biodegradable particles for protein delivery. J. Control. Release 2002, 78, 15–24. [Google Scholar] [CrossRef]
- Sogias, I.A.; Khutoryanskiy, V.V.; Williams, A.C. Exploring the factors affecting the solubility of chitosan in water. Chem. Phys. 2010, 211, 426–433. [Google Scholar] [CrossRef]
- Riva, R.; Ragelle, H.; des Rieux, A.; Duhem, N.; Jérôme, C.; Préat, V. Chitosan and chitosan derivatives in drug delivery and tissue engineering. Chitosan Biomater. II 2011, 7, 19–44. [Google Scholar]
- Kotze, A.; Luessen, H.; De Boer, A.; Verhoef, J.; Junginger, H. Chitosan for enhanced intestinal permeability: Prospects for derivatives soluble in neutral and basic environments. Eur. J. Pharm. Sci. 1999, 7, 145–151. [Google Scholar] [CrossRef]
- Kotzé, A.R.; Lueβen, H.L.; de Leeuw, B.J.; Verhoef, J.C.; Junginger, H.E. N-trimethyl chitosan chloride as a potential absorption enhancer across mucosal surfaces: In vitro evaluation in intestinal epithelial cells (Caco-2). Pharm. Res. 1997, 14, 1197–1202. [Google Scholar] [CrossRef] [PubMed]
- Amidi, M.; Romeijn, S.G.; Borchard, G.; Junginger, H.E.; Hennink, W.E.; Jiskoot, W. Preparation and characterization of protein-loaded N-trimethyl chitosan nanoparticles as nasal delivery system. J. Control. Release 2006, 111, 107–116. [Google Scholar] [CrossRef] [PubMed]
- Slütter, B.; Plapied, L.; Fievez, V.; Sande, M.A.; des Rieux, A.; Schneider, Y.-J.; Van Riet, E.; Jiskoot, W.; Préat, V. Mechanistic study of the adjuvant effect of biodegradable nanoparticles in mucosal vaccination. J. Control. Release 2009, 138, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Amidi, M.; Romeijn, S.G.; Verhoef, J.C.; Junginger, H.E.; Bungener, L.; Huckriede, A.; Crommelin, D.J.; Jiskoot, W. N-trimethyl chitosan (TMC) nanoparticles loaded with influenza subunit antigen for intranasal vaccination: Biological properties and immunogenicity in a mouse model. Vaccine 2007, 25, 144–153. [Google Scholar] [CrossRef] [PubMed]
- Nagamoto, T.; Hattori, Y.; Takayama, K.; Maitani, Y. Novel chitosan particles and chitosan-coated emulsions inducing immune response via intranasal vaccine delivery. Pharm. Res. 2004, 21, 671–674. [Google Scholar] [CrossRef] [PubMed]
- Makadia, H.K.; Siegel, S.J. Poly lactic-co-glycolic acid (PLGA) as biodegradable controlled drug delivery carrier. Polymers 2011, 3, 1377–1397. [Google Scholar] [CrossRef] [PubMed]
- Prajapati, S.K.; Jain, A.; Jain, A.; Jain, S. Biodegradable polymers and constructs: A novel approach in drug delivery. Eur. Polym. J. 2019, 120, 109191. [Google Scholar] [CrossRef]
- Köping-Höggård, M.; Sánchez, A.; Alonso, M.J. Nanoparticles as carriers for nasal vaccine delivery. Expert Rev. Vaccines 2005, 4, 185–196. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Cui, L.; Luo, Y.; Zhou, X.; Liu, R.; Chen, Q.; Guan, Y.; Zhang, Y. Construction of single-injection vaccine using new time-controlled release system. Biomater. Adv. 2022, 137, 212812. [Google Scholar] [CrossRef] [PubMed]
- Hiremath, J.; Kang, K.-i.; Xia, M.; Elaish, M.; Binjawadagi, B.; Ouyang, K.; Dhakal, S.; Arcos, J.; Torrelles, J.B.; Jiang, X. Entrapment of H1N1 influenza virus derived conserved peptides in PLGA nanoparticles enhances T cell response and vaccine efficacy in pigs. PLoS ONE 2016, 11, e0151922. [Google Scholar] [CrossRef] [Green Version]
- Mansoor, F.; Earley, B.; Cassidy, J.P.; Markey, B.; Doherty, S.; Welsh, M.D. Comparing the immune response to a novel intranasal nanoparticle PLGA vaccine and a commercial BPI3V vaccine in dairy calves. BMC Vet. Res. 2015, 11, 220. [Google Scholar] [CrossRef] [PubMed]
- Somavarapu, S.; Alpar, H.; Song, C. Biodegradable nanoparticles in nasal vaccine delivery: Effect of particle size and loading. Proceed. Int. Symp. Control. Rel. Bioact. Mater 1998, 25, 645–646. [Google Scholar]
- Kabiri, M.; Sankian, M.; Sadri, K.; Tafaghodi, M. Robust mucosal and systemic responses against HTLV-1 by delivery of multi-epitope vaccine in PLGA nanoparticles. Eur. J. Pharm. Biopharm. 2018, 133, 321–330. [Google Scholar] [CrossRef] [PubMed]
- Pawar, D.; Mangal, S.; Goswami, R.; Jaganathan, K. Development and characterization of surface modified PLGA nanoparticles for nasal vaccine delivery: Effect of mucoadhesive coating on antigen uptake and immune adjuvant activity. Eur. J. Pharm. Biopharm. 2013, 85, 550–559. [Google Scholar] [CrossRef]
- Hejazi, R.; Amiji, M. Chitosan-based gastrointestinal delivery systems. J. Control. Release 2003, 89, 151–165. [Google Scholar] [CrossRef]
- Vila, A.; Sanchez, A.; Evora, C.; Soriano, I.; McCallion, O.; Alonso, M. PLA-PEG particles as nasal protein carriers: The influence of the particle size. Int. J. Pharm. 2005, 292, 43–52. [Google Scholar] [CrossRef]
- Sosnik, A.; das Neves, J.; Sarmento, B. Mucoadhesive polymers in the design of nano-drug delivery systems for administration by non-parenteral routes: A review. Prog. Polym. Sci. 2014, 39, 2030–2075. [Google Scholar] [CrossRef]
- Samkange, T.; D’Souza, S.; Obikeze, K.; Dube, A. Influence of PEGylation on PLGA nanoparticle properties, hydrophobic drug release and interactions with human serum albumin. J. Pharm. Pharmacol. 2019, 71, 1497–1507. [Google Scholar] [CrossRef]
- Pawar, D.; Goyal, A.K.; Mangal, S.; Mishra, N.; Vaidya, B.; Tiwari, S.; Jain, A.K.; Vyas, S.P. Evaluation of mucoadhesive PLGA microparticles for nasal immunization. AAPS J. 2010, 12, 130–137. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Slütter, B.; Bal, S.; Keijzer, C.; Mallants, R.; Hagenaars, N.; Que, I.; Kaijzel, E.; van Eden, W.; Augustijns, P.; Löwik, C. Nasal vaccination with N-trimethyl chitosan and PLGA based nanoparticles: Nanoparticle characteristics determine quality and strength of the antibody response in mice against the encapsulated antigen. Vaccine 2010, 28, 6282–6291. [Google Scholar] [CrossRef] [PubMed]
- Pawar, D.; Jaganathan, K. Mucoadhesive glycol chitosan nanoparticles for intranasal delivery of hepatitis B vaccine: Enhancement of mucosal and systemic immune response. Drug Deliv. 2016, 23, 185–194. [Google Scholar] [CrossRef] [PubMed]
- Plotkin, S.A. Vaccines: Past, present and future. Nat. Med. 2005, 11, S5–S11. [Google Scholar] [CrossRef] [PubMed]
- Petrovsky, N.; Aguilar, J.C. Vaccine adjuvants: Current state and future trends. Immunol. Cell Biol. 2004, 82, 488–496. [Google Scholar] [CrossRef]
- Azmi, F.; Ahmad Fuaad, A.A.H.; Skwarczynski, M.; Toth, I. Recent progress in adjuvant discovery for peptide-based subunit vaccines. Hum. Vaccines Immunother. 2014, 10, 778–796. [Google Scholar] [CrossRef] [Green Version]
- Coffman, R.L.; Sher, A.; Seder, R.A. Vaccine adjuvants: Putting innate immunity to work. Immunity 2010, 33, 492–503. [Google Scholar] [CrossRef] [Green Version]
- Reed, S.G.; Orr, M.T.; Fox, C.B. Key roles of adjuvants in modern vaccines. Nat. Med. 2013, 19, 1597–1608. [Google Scholar] [CrossRef]
- Oleszycka, E.; Lavelle, E.C. Immunomodulatory properties of the vaccine adjuvant alum. Curr. Opin. Immunol. 2014, 28, 1–5. [Google Scholar] [CrossRef]
- Wilson-Welder, J.H.; Torres, M.P.; Kipper, M.J.; Mallapragada, S.K.; Wannemuehler, M.J.; Narasimhan, B. Vaccine adjuvants: Current challenges and future approaches. J. Pharm. Sci. 2009, 98, 1278–1316. [Google Scholar] [CrossRef]
- Moyer, T.J.; Zmolek, A.C.; Irvine, D.J. Beyond antigens and adjuvants: Formulating future vaccines. J. Clin. Investig. 2016, 126, 799–808. [Google Scholar] [CrossRef] [Green Version]
- Chen, W.; Patel, G.B.; Yan, H.; Zhang, J. Recent advances in the development of novel mucosal adjuvants and antigen delivery systems. Hum. Vaccines 2010, 6, 706–714. [Google Scholar] [CrossRef] [PubMed]
- Guo, S.; Fu, D.; Utupova, A.; Sun, D.; Zhou, M.; Jin, Z.; Zhao, K. Applications of polymer-based nanoparticles in vaccine field. Nanotechnol. Rev. 2019, 8, 143–155. [Google Scholar] [CrossRef] [Green Version]
- Smith, A.; Perelman, M.; Hinchcliffe, M. Chitosan: A promising safe and immune-enhancing adjuvant for intranasal vaccines. Hum. Vaccines Immunother. 2014, 10, 797–807. [Google Scholar] [CrossRef] [PubMed]
- Scherließ, R.; Buske, S.; Young, K.; Weber, B.; Rades, T.; Hook, S. In vivo evaluation of chitosan as an adjuvant in subcutaneous vaccine formulations. Vaccine 2013, 31, 4812–4819. [Google Scholar] [CrossRef] [PubMed]
- Bueter, C.L.; Lee, C.K.; Wang, J.P.; Ostroff, G.R.; Specht, C.A.; Levitz, S.M. Spectrum and mechanisms of inflammasome activation by chitosan. J. Immunol. 2014, 192, 5943–5951. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhao, K.; Sun, Y.; Chen, G.; Rong, G.; Kang, H.; Jin, Z.; Wang, X. Biological evaluation of N-2-hydroxypropyl trimethyl ammonium chloride chitosan as a carrier for the delivery of live Newcastle disease vaccine. Carbohydr. Polym. 2016, 149, 28–39. [Google Scholar] [CrossRef]
- Woodrow, K.A.; Bennett, K.M.; Lo, D.D. Mucosal vaccine design and delivery. Annu. Rev. Biomed. Eng. 2012, 14, 17–46. [Google Scholar] [CrossRef] [Green Version]
- Santos, D.M.; Carneiro, M.W.; de Moura, T.R.; Soto, M.; Luz, N.F.; Prates, D.B.; Irache, J.M.; Brodskyn, C.; Barral, A.; Barral-Netto, M. PLGA nanoparticles loaded with KMP-11 stimulate innate immunity and induce the killing of Leishmania. Nanomed. Nanotechnol. Biol. Med. 2013, 9, 985–995. [Google Scholar] [CrossRef] [PubMed]
- Rhee, J.H. Current and New Approaches for Mucosal Vaccine Delivery. In Mucosal Vaccines; Elsevier: Amsterdam, The Netherlands, 2020; pp. 325–356. [Google Scholar]
- Vauthier, C.; Bouchemal, K. Methods for the preparation and manufacture of polymeric nanoparticles. Pharm. Res. 2009, 26, 1025–1058. [Google Scholar] [CrossRef] [PubMed]
- Vyas, S.P.; Gupta, P.N. Implication of nanoparticles/microparticles in mucosal vaccine delivery. Expert Rev. Vaccines 2007, 6, 401–418. [Google Scholar] [CrossRef]
- Herdiana, Y.; Wathoni, N.; Shamsuddin, S.; Muchtaridi, M. Drug release study of the chitosan-based nanoparticles. Heliyon 2021, 8, e08674. [Google Scholar] [CrossRef] [PubMed]
- Ghobadi, N.; Ghobadi, S.; Burkholder, M.B.; Habibypour, R. Nanoparticles development for pulmonary vaccination: Challenges and opportunities. Nanomed. J. 2021, 8, 1–13. [Google Scholar]
- Tonnis, W.F.; Kersten, G.F.; Frijlink, H.W.; Hinrichs, W.L.; de Boer, A.H.; Amorij, J.-P. Pulmonary vaccine delivery: A realistic approach? J. Aerosol Med. Pulm. Drug Deliv. 2012, 25, 249–260. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mamo, T.; Poland, G.A. Nanovaccinology: The next generation of vaccines meets 21st century materials science and engineering. Vaccine 2012, 30, 6609. [Google Scholar] [CrossRef] [PubMed]
- Trierweiler, L.F.; Trierweiler, J.O. Industrial production of polymeric nanoparticles: Alternatives and economic analysis. In Nanocosmetics and Nanomedicines; Springer: Berlin/Heidelberg, Germany, 2011; pp. 123–138. [Google Scholar]


| The Composition of Nanoparticles | Antigen | Type of Immunity | Reference |
|---|---|---|---|
| PLGA (1) (50:50) | Synthetic bovine parainfluenza virus type-3 (BPI3V) peptide motifs | Induce stronger IgG (2) antibody | [155] |
| PLGA | Inactivated PRRS (3) virus | IgG1 and IgG2 antibody, T-helper (Th)-1 and Th2 (4) cytokines | [156] |
| Chitosan (mannose) | Tumor pGRP (5) DNA | Anti-GRP IgG antibody | [157] |
| Mannosylated chitosan | Foot and mouth disease virus DNA, pVAC FMDV (6) VP1-OmpA | Induction of virus-neutralizing antibodies, Th1(IgG2) and Th2 (IgG1) responses | [158] |
| CS/TPP (7) | Subunit/split influenza | Higher systemic and mucosal antibody | [159] |
| PLGA coated gelatin (PGNPs) (8) | Tetanus Toxoid antigen | Humoral, cellular and mucosal immunity | [160] |
| Chitosan dextran sulfate | Pertussis toxin (PTX) | - | [161] |
| Trimethylated chitosan (TMC) and chitosan | Hepatitis B surface antigen | IgG, IgG1, IgG2a, IgA (9) antibodies | [162] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Nemrawi, N.K.; Darweesh, R.S.; Al-shriem, L.A.; Al-Qawasmi, F.S.; Emran, S.O.; Khafajah, A.S.; Abu-Dalo, M.A. Polymeric Nanoparticles for Inhaled Vaccines. Polymers 2022, 14, 4450. https://doi.org/10.3390/polym14204450
Al-Nemrawi NK, Darweesh RS, Al-shriem LA, Al-Qawasmi FS, Emran SO, Khafajah AS, Abu-Dalo MA. Polymeric Nanoparticles for Inhaled Vaccines. Polymers. 2022; 14(20):4450. https://doi.org/10.3390/polym14204450
Chicago/Turabian StyleAl-Nemrawi, Nusaiba K., Ruba S. Darweesh, Lubna A. Al-shriem, Farah S. Al-Qawasmi, Sereen O. Emran, Areej S. Khafajah, and Muna A. Abu-Dalo. 2022. "Polymeric Nanoparticles for Inhaled Vaccines" Polymers 14, no. 20: 4450. https://doi.org/10.3390/polym14204450