Longitudinal Patterns of Beverage Intake in Treatment-Seeking Children with Obesity in Eastern NC Using the Validated BEVQ-15
Abstract
:1. Introduction
2. Material and Methods
2.1. Study Setting
2.2. Inclusion and Exclusion Criteria
2.3. Outcomes
2.4. Independent Variables
2.5. Data Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wickham, E.P.; DeBoer, M.D. Evaluation and treatment of severe obesity in childhood. Clin. Pediatr. 2015, 54, 929–940. [Google Scholar] [CrossRef] [PubMed]
- Skinner, A.C.; Ravanbakht, S.N.; Skelton, J.A.; Perrin, E.M.; Armstrong, S.C. Prevalence of obesity and severe obesity in US children, 1999–2016. Pediatrics 2018, 141, e20173459. [Google Scholar] [CrossRef] [PubMed]
- Kit, B.K.; Fakhouri, T.H.; Park, S.; Nielsen, S.J.; Ogden, C.L. Trends in sugar-sweetened beverage consumption among youth and adults in the United States: 1999–2010. Am. J. Clin. Nutr. 2013, 98, 180–188. [Google Scholar] [CrossRef]
- Vercammen, K.A.; Moran, A.J.; Soto, M.J.; Kennedy-Shaffer, L.; Bleich, S.N. Decreasing trends in heavy sugar-sweetened beverage consumption in the United States, 2003 to 2016. J. Acad. Nutr. Diet. 2020, 120, 1974.e5–1985.e5. [Google Scholar] [CrossRef] [PubMed]
- Ebbeling, C.B.; Feldman, H.A.; Osganian, S.K.; Chomitz, V.R.; Ellenbogen, S.J.; Ludwig, D.S. Effects of decreasing sugar-sweetened beverage consumption on body weight in adolescents: A randomized, controlled pilot study. J. Am. Acad. Child Adolesc. Psychiatry 2006, 45, 1353. [Google Scholar] [CrossRef]
- Nguyen, M.; Jarvis, S.E.; Tinajero, M.G.; Yu, J.; Chiavaroli, L.; Mejia, S.B.; Khan, T.A.; Tobias, D.K.; Willett, W.C.; Hu, F.B.; et al. Sugar-sweetened beverage consumption and weight gain in children and adults: A systematic review and meta-analysis of prospective cohort studies and randomized controlled trials. Am. J. Clin. Nutr. 2023, 117, 160–174. [Google Scholar] [CrossRef]
- Hedrick, V.E.; Comber, D.L.; Ferguson, K.E.; Estabrooks, P.A.; Savla, J.; Dietrich, A.M.; Serrano, E.; Davy, B.M. A rapid beverage intake questionnaire can detect changes in beverage intake. Eat. Behav. Int. J. 2013, 14, 90–94. [Google Scholar] [CrossRef]
- Berkey, C.S.; Rockett, H.R.H.; Field, A.E.; Gillman, M.W.; Colditz, G.A. Sugar-added beverages and adolescent weight change. Obesity 2004, 12, 778–788. [Google Scholar] [CrossRef]
- Palmer, J.R.; Boggs, D.A.; Krishnan, S.; Hu, F.B.; Singer, M.; Rosenberg, L. Sugar-sweetened beverages and incidence of type 2 diabetes mellitus in african american women. Arch. Intern. Med. 2008, 168, 1487–1492. [Google Scholar] [CrossRef]
- Laska, M.N.; Murray, D.M.; Lytle, L.A.; Harnack, L.J. Longitudinal associations between key dietary behaviors and weight gain over time: Transitions through the adolescent years. Obesity 2012, 20, 118–125. [Google Scholar] [CrossRef]
- Olsen, N.J.; Andersen, L.B.; Wedderkopp, N.; Kristensen, P.L.; Heitmann, B.L. Intake of liquid and solid sucrose in relation to changes in body fatness over 6 years among 8- to 10-year-old children: The European youth heart study. Obes. Facts 2012, 5, 506–512. [Google Scholar] [CrossRef]
- Carlson, J.A.; Crespo, N.C.; Sallis, J.F.; Patterson, R.E.; Elder, J.P. Dietary-related and physical activity-related predictors of obesity in children: A 2-year prospective study. Child. Obes. 2012, 8, 110–115. [Google Scholar] [CrossRef]
- Laurson, K.; Eisenmann, J.C.; Moore, S. Lack of association between television viewing, soft drinks, physical activity and body mass index in children. Acta Paediatr. 2008, 97, 795–800. [Google Scholar] [CrossRef]
- Hedrick, V.; Savla, J.; Comber, D.L.; Flack, K.D.; Estabrooks, P.A.; Nsiah-Kumi, P.A.; Ortmeier, S.; Davy, B.M. Development of a brief questionnaire to assess habitual beverage intake (BEVQ-15): Sugar-sweetened beverages and total beverage energy intake. J. Am. Diet. Assoc. 2012, 112, 840. [Google Scholar] [CrossRef]
- Hedrick, V.E.; Comber, D.L.; Estabrooks, P.A.; Savla, J.; Davy, B.M. The beverage intake questionnaire: Initial validity and reliability. J. Am. Diet. Assoc. 2010, 110, 1227–1232. [Google Scholar] [CrossRef]
- Hill, C.E.; MacDougall, C.R.; Riebl, S.K.; Savla, J.; Hedrick, V.E.; Davy, B.M. Evaluation of the relative validity and Test–Retest reliability of a 15-item beverage intake questionnaire in children and adolescents. J. Acad. Nutr. Diet. 2017, 117, 1757.e5–1766.e5. [Google Scholar] [CrossRef]
- Taft, N.; Collier, D.; Tanenberg, R.; Kolasa, K. How sweet it is: Traditional sweet iced tea and the diabesity epidemic. Nutr. Today 2015, 50, 28–39. [Google Scholar] [CrossRef]
- Skelton, J.; Cook, S.; Auinger, P.; Klein, J.; Barlow, S. Prevalence and trends of severe obesity among US children and adolescents. Ambul. Pediatr. Off. J. Ambul. Pediatr. Assoc. 2009, 9, 322. [Google Scholar] [CrossRef]
- Hager, E.R.; Quigg, A.M.; Black, M.M.; Coleman, S.M.; Heeren, T.; Rose-Jacobs, R.; Cook, J.T.; Ettinger de Cuba, S.A.; Casey, P.H.; Chilton, M.; et al. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics 2010, 126, e26–e32. [Google Scholar] [CrossRef]
- Parente, P.M.D.C.; Santos Silva, J.M.C. Quantile regression with clustered data. J. Econom. Methods 2016, 5, 1–15. [Google Scholar] [CrossRef]
- Wang, M.L.; Sprague Martinez, L.S.; Weinberg, J.; Alatorre, S.; Lemon, S.C.; Rosal, M.C. A youth empowerment intervention to prevent childhood obesity: Design and methods for a cluster randomized trial of the H2GO! program. BMC Public Health 2021, 21, 1–1675. [Google Scholar] [CrossRef] [PubMed]
- Mendez, M.A.; Miles, D.R.; Poti, J.M.; Sotres-Alvarez, D.; Popkin, B.M. Persistent disparities over time in the distribution of sugar-sweetened beverage intake among children in the united states. Am. J. Clin. Nutr. 2019, 109, 79–89. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.I.; Ritchie, L. Striving for meaningful policies to reduce sugar-sweetened beverage intake among young children. Pediatrics 2013, 132, 566–568. [Google Scholar] [CrossRef] [PubMed]
- Sanyaolu, A.; Okorie, C.; Qi, X.; Locke, J.; Rehman, S. Childhood and adolescent obesity in the United States: A public health concern. Glob. Pediatr. Health 2019, 6, 2333794X19891305. [Google Scholar] [CrossRef] [PubMed]
- Vinke, P.C.; Blijleven, K.A.; Luitjens, M.H.H.S.; Corpeleijn, E. Young children’s sugar-sweetened beverage consumption and 5-year change in BMI: Lessons learned from the timing of consumption. Nutrients 2020, 12, 2486. [Google Scholar] [CrossRef]
- Millar, L.; Rowland, B.; Nichols, M.; Swinburn, B.; Bennett, C.; Skouteris, H.; Allender, S. Relationship between raised BMI and sugar sweetened beverage and high fat food consumption among children. Obesity 2014, 22, E96–E103. [Google Scholar] [CrossRef]
- Keller, A.; Bucher Della Torre, S. Sugar-sweetened beverages and obesity among children and adolescents: A review of systematic literature reviews. Child. Obes. 2015, 11, 338–346. [Google Scholar] [CrossRef]
- Bleich, S.N.; Vercammen, K.A.; Koma, J.W.; Li, Z. Trends in beverage consumption among children and adults, 2003–2014. Obesity 2018, 26, 432–441. [Google Scholar] [CrossRef]
- Kumar, S.; Kelly, A.S. Review of childhood obesity: From epidemiology, etiology, and comorbidities to clinical assessment and treatment. Mayo Clin. Proc. 2017, 92, 251–265. [Google Scholar] [CrossRef]
- Scharf, R.J.; DeBoer, M.D. Sugar-sweetened beverages and children’s health. Annu. Rev. Public Health 2016, 37, 273–293. [Google Scholar] [CrossRef]
- Haynes-Maslow, L.; Ray, S.; Giombi, K. Perceptions of sugar-sweetened beverages among adolescents in north carolina. Front. Public Health 2022, 10, 943295. [Google Scholar] [CrossRef] [PubMed]
| Variable | Initial Sample (N = 625) | Final Sample (N = 155) |
|---|---|---|
| Median (IQR) or N (%) | Median (IQR) or N (%) | |
| Sex a | ||
| Female | 356 (57%) | 93 (60%) |
| Male | 268 (43%) | 62 (40%) |
| Age (years) a | 13 (10, 14) | 11 (9, 14) |
| Race/ethnicity | ||
| Non-Hispanic Black | 345 (55%) | 99 (64%) |
| Non-Hispanic White | 114 (18%) | 13 (8%) |
| Hispanic or Latino | 128 (20%) | 35 (23%) |
| Other | 38 (6%) | 8 (5%) |
| Medicaid insurance | 492 (79%) | 135 (87%) |
| Family composition b,c | ||
| Two parents | 323 (53%) | 72 (47%) |
| Mother only | 175 (29%) | 50 (33%) |
| Other | 115 (19%) | 30 (20%) |
| Food insecurity b,d | 173 (29%) | 53 (35%) |
| Meals out (days/week) e,f | 2.5 (0.5, 2.5) | 2.5 (0.5, 2.5) |
| Breakfast (days/week) g,h | 7 (2, 7) | 7 (2, 7) |
| BMI as percent of 95th percentile | 131 (115, 148) | 135 (121, 152) |
| Initial Sample (N = 625) | Final Sample (N = 155) | ||
|---|---|---|---|
| Beverage type (kcal/day) | Baseline visit | Baseline visit | Most recent visit |
| Median (IQR) | Median (IQR) | Median (IQR) | |
| SSB + 100% fruit juice | 270 (126, 554) | 436 (248, 765) | 133 (72, 237) |
| SSBs only | 172 (68, 372) | 263 (130, 602) | 78 (31, 153) |
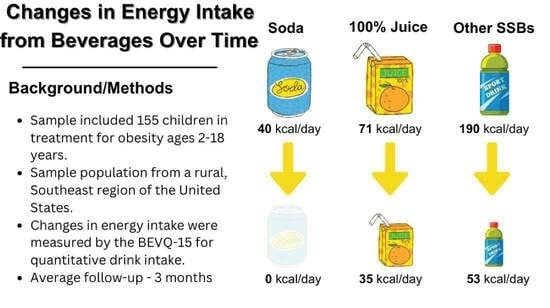
| Soda | 27 (0, 53) | 40 (0, 93) | 0 (0, 27) |
| Other SSBs | 124 (44, 285) | 190 (73, 403) | 53 (18, 118) |
| 100% fruit juice | 53 (0, 124) | 71 (18, 212) | 35 (0, 71) |
| Variable | Coefficient | 95% CI | p |
|---|---|---|---|
| Time since baseline (months) | −6.8 | −11.6, −2.0 | 0.005 |
| Sex | |||
| Female | Ref. | ||
| Male | 29.9 | −46.2, 106.0 | 0.440 |
| Age (years) | 4.2 | −7.6, 16.0 | 0.483 |
| Race/ethnicity | |||
| Non-Hispanic Black | Ref. | ||
| Non-Hispanic White | −66.0 | −218.4, 86.3 | 0.394 |
| Hispanic or Latino | −123.8 | −225.9, −21.6 | 0.018 |
| Other | −80.4 | −208.7, 47.9 | 0.219 |
| Medicaid insurance | 108.8 | 12.5, 205.0 | 0.027 |
| Family composition | |||
| Two parents | Ref. | ||
| Mother only | 32.4 | −62.4, 127.1 | 0.502 |
| Other | −47.6 | −162.3, 67.0 | 0.414 |
| Food insecurity | −29.7 | −112.5, 53.1 | 0.481 |
| Meals out (days/week) | 52.2 | 18.4, 86.0 | 0.003 |
| Breakfast (days/week) | −10.7 | −24.7, 3.3 | 0.134 |
| Variable | Coefficient | 95% CI | p |
|---|---|---|---|
| Time since baseline (months) | 0.5 | 0.1, 1.0 | 0.012 |
| Calories from SSB + 100% fruit juice (100 kcal/day) | 1.4 | 0.8, 2.0 | <0.001 |
| Sex | |||
| Female | Ref. | ||
| Male | −3.2 | −12.1, 5.6 | 0.471 |
| Age (years) | −0.2 | −1.9, 1.4 | 0.784 |
| Race/ethnicity | |||
| Non-Hispanic Black | Ref. | ||
| Non-Hispanic White | −16.3 | −31.6, −1.0 | 0.036 |
| Hispanic or Latino | −3.8 | −17.3, 9.8 | 0.587 |
| Other | 2.5 | −22.2, 27.3 | 0.840 |
| Medicaid insurance | −4.6 | −20.7, 11.4 | 0.571 |
| Family composition | |||
| Two parents | Ref. | ||
| Mother only | 0.7 | −11.3, 12.7 | 0.913 |
| Other | 10.3 | −1.7, 22.4 | 0.091 |
| Food insecurity | 6.3 | −3.6, 16.3 | 0.212 |
| Meals out (days/week) | −0.8 | −2.9, 1.3 | 0.459 |
| Breakfast (days/week) | −1.5 | −4.3, 1.3 | 0.302 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mohseni, Z.; Tumin, D.; Collier, D.N.; Taft, N.; Lazorick, S. Longitudinal Patterns of Beverage Intake in Treatment-Seeking Children with Obesity in Eastern NC Using the Validated BEVQ-15. Nutrients 2023, 15, 4171. https://doi.org/10.3390/nu15194171
Mohseni Z, Tumin D, Collier DN, Taft N, Lazorick S. Longitudinal Patterns of Beverage Intake in Treatment-Seeking Children with Obesity in Eastern NC Using the Validated BEVQ-15. Nutrients. 2023; 15(19):4171. https://doi.org/10.3390/nu15194171
Chicago/Turabian StyleMohseni, Zahra, Dmitry Tumin, David N. Collier, Natalie Taft, and Suzanne Lazorick. 2023. "Longitudinal Patterns of Beverage Intake in Treatment-Seeking Children with Obesity in Eastern NC Using the Validated BEVQ-15" Nutrients 15, no. 19: 4171. https://doi.org/10.3390/nu15194171