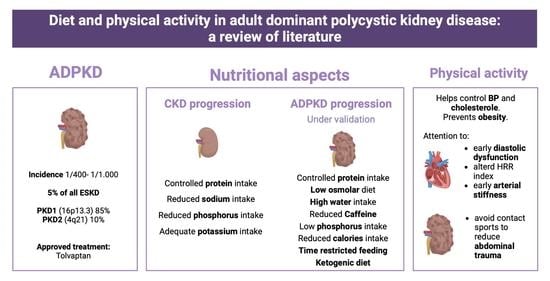
Diet and Physical Activity in Adult Dominant Polycystic Kidney Disease: A Review of the Literature
Abstract
:1. Introduction
2. Epidemiology and Pathogenesis of ADPKD
3. Diet in ADPKD
3.1. Nutritional Aspects for the Management of CKD in ADPKD Patients
3.1.1. Proteins
3.1.2. Sodium
3.1.3. Phosphorus and Potassium
3.2. Nutritional Aspects with Possible Impact on the Pathogenesis of ADPKD
3.2.1. Proteins
3.2.2. Water Intake
3.2.3. Sodium
3.2.4. Phosphorus
3.2.5. Caffeine
3.2.6. Calories and Body Weight
3.2.7. Ketogenic Diet
4. Physical Activity
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ho, M.; Ho, J.W.C.; Fong, D.Y.T.; Lee, C.F.; Macfarlane, D.J.; Cerin, E.; Lee, A.M.; Leung, S.; Chan, W.Y.Y.; Leung, I.P.F.; et al. Effects of dietary and physical activity interventions on generic and cancer-specific health-related quality of life, anxiety, and depression in colorectal cancer survivors: A randomized controlled trial. J. Cancer Surviv. 2020, 14, 424–433. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cohen, C.W.; Fontaine, K.R.; Arend, R.C.; Soleymani, T.; Gower, B.A. Favorable Effects of a Ketogenic Diet on Physical Function, Perceived Energy, and Food Cravings in Women with Ovarian or Endometrial Cancer: A Randomized, Controlled Trial. Nutrients 2018, 10, 1187. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khodabakhshi, A.; Seyfried, T.N.; Kalamian, M.; Beheshti, M.; Davoodi, S.H. Does a ketogenic diet have beneficial effects on quality of life, physical activity or biomarkers in patients with breast cancer: A randomized controlled clinical trial. Nutr. J. 2020, 19, 87. [Google Scholar] [CrossRef] [PubMed]
- Chapman, A.B.; Devuyst, O.; Eckardt, K.-U.; Gansevoort, R.T.; Harris, T.; Horie, S.; Kasiske, B.L.; Odland, D.; Pei, Y.; Perrone, R.D.; et al. Autosomal-dominant polycystic kidney disease (ADPKD): Executive summary from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kidney Int. 2015, 88, 17–27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Willey, C.J.; Blais, J.D.; Hall, A.K.; Krasa, H.B.; Makin, A.J.; Czerwiec, F.S. Prevalence of autosomal dominant polycystic kidney disease in the European Union. Nephrol. Dial. Transplant. 2017, 32, 1356–1363. [Google Scholar] [CrossRef] [Green Version]
- Blair, H.A. Tolvaptan: A Review in Autosomal Dominant Polycystic Kidney Disease. Drugs 2019, 79, 303–313. [Google Scholar] [CrossRef]
- Chebib, F.T.; Torres, V.E. Autosomal Dominant Polycystic Kidney Disease: Core Curriculum 2016. Am. J. Kidney Dis. 2016, 67, 792–810. [Google Scholar] [CrossRef] [Green Version]
- Paterson, A.D.; Magistroni, R.; He, N.; Wang, K.; Johnson, A.; Fain, P.R.; Dicks, E.; Parfrey, P.; George-Hyslop, P.S.; Pei, Y. Progressive loss of renal function is an age-dependent heritable trait in type 1 autosomal dominant polycystic kidney disease. J. Am. Soc. Nephrol. 2005, 16, 755–762. [Google Scholar] [CrossRef] [Green Version]
- Lanktree, M.B.; Guiard, E.; Li, W.; Akbari, P.; Haghighi, A.; Iliuta, I.-A.; Shi, B.; Chen, C.; He, N.; Song, X.; et al. Intrafamilial Variability of ADPKD. Kidney Int. Rep. 2019, 4, 995–1003. [Google Scholar] [CrossRef] [Green Version]
- Ma, M.; Tian, X.; Igarashi, P.; Pazour, G.J.; Somlo, S. Loss of cilia suppresses cyst growth in genetic models of autosomal dominant polycystic kidney disease. Nat. Genet. 2013, 45, 1004–1012. [Google Scholar] [CrossRef] [Green Version]
- Praetorius, H.; Spring, K. Bending the MDCK cell primary cilium increases intracellular calcium. J. Membr. Biol. 2001, 184, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Cornec-Le Gall, E.; Alam, A.; Perrone, R.D. Autosomal dominant polycystic kidney disease. Lancet 2019, 393, 919–935. [Google Scholar] [CrossRef] [PubMed]
- Clegg, D.J.; Gallant, K.M.H. Plant-Based Diets in CKD. Clin. J. Am. Soc. Nephrol. 2019, 14, 141–143. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, H.; Caulfield, L.E.; Garcia-Larsen, V.; Steffen, L.M.; Grams, M.E.; Coresh, J.; Rebholz, C.M. Plant-Based Diets and Incident CKD and Kidney Function. Clin. J. Am. Soc. Nephrol. 2019, 14, 682–691. [Google Scholar] [CrossRef] [Green Version]
- Gallieni, M.; Cupisti, A. DASH and Mediterranean Diets as Nutritional Interventions for CKD Patients. Am. J. Kidney Dis. 2016, 68, 828–830. [Google Scholar] [CrossRef] [Green Version]
- Rebholz, C.M.; Crews, D.C.; Grams, M.E.; Steffen, L.M.; Levey, A.S.; Miller, E.R.; Appel, L.J.; Coresh, J. DASH (Dietary Approaches to Stop Hypertension) Diet and Risk of Subsequent Kidney Disease. Am. J. Kidney Dis. 2016, 68, 853–861. [Google Scholar] [CrossRef] [Green Version]
- Billingsley, H.E.; Carbone, S. The antioxidant potential of the Mediterranean diet in patients at high cardiovascular risk: An in-depth review of the PREDIMED. Nutr. Diabetes 2018, 8, 13. [Google Scholar] [CrossRef] [Green Version]
- Rysz, J.; Franczyk, B.; Ciałkowska-Rysz, A.; Gluba-Brzózka, A. The Effect of Diet on the Survival of Patients with Chronic Kidney Disease. Nutrients 2017, 9, 495. [Google Scholar] [CrossRef] [Green Version]
- Fouque, D.; Ikizler, T.A. Editorial: Implementing low protein diets in clinical practice in patients with chronic kidney disease. Nephrol. Dial. Transpl. 2020, 35, 1643–1645. [Google Scholar] [CrossRef]
- Klahr, S.; A Breyer, J.; Beck, G.J.; Dennis, V.W.; A Hartman, J.; Roth, D.; I Steinman, T.; Wang, S.R.; E Yamamoto, M. Dietary protein restriction, blood pressure control, and the progression of polycystic kidney disease. Modification of Diet in Renal Disease Study Group. J. Am. Soc. Nephrol. 1995, 5, 2037–2047. [Google Scholar] [CrossRef]
- Kramers, B.J.; Koorevaar, I.W.; Drenth, J.P.; de Fijter, J.W.; Neto, A.G.; Peters, D.J.; Vart, P.; Wetzels, J.F.; Zietse, R.; Gansevoort, R.T.; et al. Salt, but not protein intake, is associated with accelerated disease progression in autosomal dominant polycystic kidney disease. Kidney Int. 2020, 98, 989–998. [Google Scholar] [CrossRef] [PubMed]
- Torres, V.E.; Grantham, J.J.; Chapman, A.B.; Mrug, M.; Bae, K.T.; King, B.F.; Wetzel, L.H.; Martin, D.; Lockhart, M.E.; Bennett, W.M.; et al. Potentially modifiable factors affecting the progression of autosomal dominant polycystic kidney disease. Clin. J. Am. Soc. Nephrol. 2011, 6, 640–647. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heida, J.E.; Gansevoort, R.T.; Messchendorp, A.L.; Meijer, E.; Casteleijn, N.F.; Boertien, W.E.; Zittema, D.; on behalf of the DIPAK Consortium. Use of the Urine-to-Plasma Urea Ratio to Predict ADPKD Progression. Clin. J. Am. Soc. Nephrol. 2021, 16, 204–212. [Google Scholar] [CrossRef] [PubMed]
- Dietary Recommendations for Patients with Nondialysis Chronic Kidney Disease—Up To Date. Available online: https://www-uptodate-com.ezproxy.unibo.it/contents/dietary-recommendations-for-patients-with-nondialysis-chronic-kidney-disease?search=Dietary%20recommendations%20for%20patients%20with%20nondialysis%20chronic%20kidney%20disease&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1#H1107315266 (accessed on 29 May 2023).
- Judd, E.; Calhoun, D.A. Management of hypertension in CKD: Beyond the guidelines. Adv. Chronic Kidney Dis. 2015, 22, 116–122. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Naber, T.; Purohit, S. Chronic Kidney Disease: Role of Diet for a Reduction in the Severity of the Disease. Nutrients 2021, 13, 3277. [Google Scholar] [CrossRef]
- Bankir, L.; Roussel, R.; Bouby, N. Protein-and diabetes-induced glomerular hyperfiltration: Role of glucagon, vasopressin, and urea. Am. J. Physiol. Renal Physiol. 2015, 309, 2–23. [Google Scholar] [CrossRef] [Green Version]
- Aukema, H.M.; Ogborn, M.R.; Tomobe, K.; Takahashi, H.; Hibino, T.; Holub, B.J. Effects of dietary protein restriction and oil type on the early progression of murine polycystic kidney disease. Kidney Int. 1992, 42, 837–842. [Google Scholar] [CrossRef] [Green Version]
- Aukema, H.M.; Housini, I.; Rawling, J.M. Dietary soy protein effects on inherited polycystic kidney disease are influenced by gender and protein level. J. Am. Soc. Nephrol. 1999, 10, 300–308. [Google Scholar] [CrossRef]
- Hopp, K.; Wang, X.F.; Ye, H.; Irazabal, M.V.; Harris, P.C.; Torres, V.E. Effects of hydration in rats and mice with polycystic kidney disease. Am. J. Physiol. Renal Physiol. 2015, 308, F261–F266. [Google Scholar] [CrossRef] [Green Version]
- Nagao, S.; Nishii, K.; Katsuyama, M.; Kurahashi, H.; Marunouchi, T.; Takahashi, H.; Wallace, D.P. Increased water intake decreases progression of polycystic kidney disease in the PCK rat. J. Am. Soc. Nephrol. 2006, 17, 2220–2227. [Google Scholar] [CrossRef] [Green Version]
- El-Damanawi, R.; Lee, M.; Harris, T.; Cowley, L.B.; Bond, S.; Pavey, H.; Sandford, R.N.; Wilkinson, I.B.; Frankl, F.E.K.; Hiemstra, T.F. High water vs. ad libitum water intake for autosomal dominant polycystic kidney disease: A randomized controlled feasibility trial. QJM 2020, 113, 258–265. [Google Scholar] [CrossRef] [Green Version]
- Rangan, G.K.; Wong, A.T.; Munt, A.; Zhang, J.Q.; Saravanabavan, S.; Louw, S.; Allman-Farinelli, M.; Badve, S.V.; Boudville, N.; Chan, J.; et al. Prescribed Water Intake in Autosomal Dominant Polycystic Kidney Disease. NEJM Evid. 2021, 1, EVIDoa2100021. [Google Scholar] [CrossRef]
- Hoorn, E.J.; Zietse, R. ADPKD, Tolvaptan, and Nephrolithiasis Risk. Clin. J. Am. Soc. Nephrol. 2020, 15, 923. [Google Scholar] [CrossRef]
- Hian, C.K.; Lee, C.L.; Thomas, W. Renin-Angiotensin-Aldosterone System Antagonism and Polycystic Kidney Disease Progression. Nephron 2016, 134, 59–63. [Google Scholar] [CrossRef] [PubMed]
- Schrier, R.W.; Abebe, K.Z.; Perrone, R.D.; Torres, V.E.; Braun, W.E.; Steinman, T.I.; Winklhofer, F.T.; Brosnahan, G.; Czarnecki, P.G.; Hogan, M.C.; et al. Blood pressure in early autosomal dominant polycystic kidney disease. N. Engl. J. Med. 2014, 371, 2255–2266. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Amro, O.W.; Paulus, J.K.; Noubary, F.; Perrone, R.D. Low-Osmolar Diet and Adjusted Water Intake for Vasopressin Reduction in Autosomal Dominant Polycystic Kidney Disease: A Pilot Randomized Controlled Trial. Am. J. Kidney Dis. 2016, 68, 882–891. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Keith, D.S.; Torres, V.E.; Johnson, C.M.; Holley, K.E. Effect of sodium chloride, enalapril, and losartan on the development of polycystic kidney disease in Han:SPRD rats. Am. J. Kidney Dis. 1994, 24, 491–498. [Google Scholar] [CrossRef] [PubMed]
- Torres, V.E.; Abebe, K.Z.; Schrier, R.W.; Perrone, R.D.; Chapman, A.B.; Yu, A.S.; Braun, W.E.; Steinman, T.I.; Brosnahan, G.; Hogan, M.C.; et al. Dietary salt restriction is beneficial to the management of autosomal dominant polycystic kidney disease. Kidney Int. 2017, 91, 493–500. [Google Scholar] [CrossRef] [Green Version]
- Omede, F.; Zhang, S.; Johnson, C.; Daniel, E.; Zhang, Y.; Fields, T.A.; Boulanger, J.; Liu, S.; Ahmed, I.; Umar, S.; et al. Dietary phosphate restriction attenuates polycystic kidney disease in mice. Am. J. Physiol. Renal Physiol. 2020, 318, F35–F42. [Google Scholar] [CrossRef]
- McKenzie, K.A.; El Ters, M.; Torres, V.E.; Harris, P.C.; Chapman, A.B.; Mrug, M.; Rahbari-Oskoui, F.F.; Bae, K.T.; Landsittel, D.P.; Bennett, W.M.; et al. Relationship between caffeine intake and autosomal dominant polycystic kidney disease progression: A retrospective analysis using the CRISP cohort. BMC Nephrol. 2018, 19, 378. [Google Scholar] [CrossRef] [Green Version]
- Girardat-Rotar, L.; Puhan, M.A.; Braun, J.; Serra, A.L. Long-term effect of coffee consumption on autosomal dominant polycystic kidneys disease progression: Results from the Suisse ADPKD, a Prospective Longitudinal Cohort Study. J. Nephrol. 2018, 31, 87–94. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nowak, K.L.; Steele, C.; Gitomer, B.; Wang, W.; Ouyang, J.; Chonchol, M.B. Overweight and Obesity and Progression of ADPKD. Clin. J. Am. Soc. Nephrol. 2021, 16, 908–915. [Google Scholar] [CrossRef] [PubMed]
- Nowak, K.L.; Hopp, K. Metabolic Reprogramming in Autosomal Dominant Polycystic Kidney Disease: Evidence and Therapeutic Potential. Clin. J. Am. Soc. Nephrol. 2020, 15, 577–584. [Google Scholar] [CrossRef] [PubMed]
- Kipp, K.R.; Rezaei, M.; Lin, L.; Dewey, E.C.; Weimbs, T. A mild reduction of food intake slows disease progression in an orthologous mouse model of polycystic kidney disease. Am. J. Physiol. Renal Physiol. 2016, 310, F726–F731. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hopp, K.; Catenacci, V.A.; Dwivedi, N.; Kline, T.L.; Wang, W.; You, Z.; Nguyen, D.T.; Bing, K.; Poudyal, B.; Johnson, G.C.; et al. Weight loss and cystic disease progression in autosomal dominant polycystic kidney disease. iScience 2021, 25, 103697. [Google Scholar] [CrossRef]
- Kashyap, S.; Zeidler, J.D.; Chini, C.C.; Chini, E.N. Implications of the PAPP-A-IGFBP-IGF-1 pathway in the pathogenesis and treatment of polycystic kidney disease. Cell Signal. 2020, 73, 109698. [Google Scholar] [CrossRef]
- Kashyap, S.; Hein, K.Z.; Chini, C.C.; Lika, J.; Warner, G.M.; Bale, L.K.; Torres, V.E.; Harris, P.C.; Oxvig, C.; Conover, C.A.; et al. Metalloproteinase PAPP-A regulation of IGF-1 contributes to polycystic kidney disease pathogenesis. JCI Insight. 2020, 54, e135700. [Google Scholar] [CrossRef] [Green Version]
- Barry, D.; Ellul, S.; Watters, L.; Lee, D.; Haluska, R.; White, R. The ketogenic diet in disease and development. Int. J. Dev. Neurosci. 2018, 68, 53–58. [Google Scholar] [CrossRef]
- Warner, G.; Hein, K.Z.; Nin, V.; Edwards, M.; Chini, C.C.; Hopp, K.; Harris, P.C.; Torres, V.E.; Chini, E.N. Food Restriction Ameliorates the Development of Polycystic Kidney Disease. J. Am. Soc. Nephrol. 2016, 27, 1437–1447. [Google Scholar] [CrossRef] [Green Version]
- Weimbs, T.; Shillingford, J.M.; Torres, J.; Kruger, S.L.; Bourgeois, B.C. Emerging targeted strategies for the treatment of autosomal dominant polycystic kidney disease. Clin. Kidney J. 2018, 11 (Suppl. S1), I27–I38. [Google Scholar] [CrossRef] [Green Version]
- Lonardo, M.S.; Guida, B.; Cacciapuoti, N.; Di Lauro, M.; Cataldi, M. Adult dominant polycystic kidney disease: A prototypical disease for pharmanutrition interventions. PharmaNutrition 2022, 20, 100294. [Google Scholar] [CrossRef]
- Dachy, A.; Decuypere, J.-P.; Vennekens, R.; Jouret, F.; Mekahli, D. Is autosomal dominant polycystic kidney disease an early sweet disease? Pediatr. Nephrol. 2022, 37, 1945–1955. [Google Scholar] [CrossRef] [PubMed]
- Torres, J.A.; Kruger, S.L.; Broderick, C.; Amarlkhagva, T.; Agrawal, S.; Dodam, J.R.; Mrug, M.; Lyons, L.A.; Weimbs, T. Ketosis Ameliorates Renal Cyst Growth in Polycystic Kidney Disease. Cell. Metab. 2019, 30, 1007–1023.e5. [Google Scholar] [CrossRef] [PubMed]
- Carriazo, S.; Perez-Gomez, M.V.; Cordido, A.; García-González, M.A.; Sanz, A.B.; Ortiz, A.; Sanchez-Niño, M.D. Dietary Care for ADPKD Patients: Current Status and Future Directions. Nutrients 2019, 11, 1576. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ong, A.C.M.; Torra, R. Can ketogenic dietary interventions slow disease progression in ADPKD: What we know and what we don’t. Clin. Kidney J. 2022, 15, 1034–1036. [Google Scholar] [CrossRef]
- Strubl, S.; Oehm, S.; Torres, J.A.; Grundmann, F.; Haratani, J.; Decker, M.; Vuong, S.; Bhandal, A.K.; Methot, N.; Haynie-Cion, R.; et al. Ketogenic dietary interventions in autosomal dominant polycystic kidney disease-a retrospective case series study: First insights into feasibility, safety and effects. Clin. Kidney J. 2021, 15, 1079–1092. [Google Scholar] [CrossRef]
- Testa, F.; Marchiò, M.; D’amico, R.; Giovanella, S.; Ligabue, G.; Fontana, F.; Alfano, G.; Cappelli, G.; Biagini, G.; Magistroni, R. GREASE II. A phase II randomized, 12-month, parallel-group, superiority study to evaluate the efficacy of a Modified Atkins Diet in Autosomal Dominant Polycystic Kidney Disease patients. PharmaNutrition 2020, 13, 100206. [Google Scholar] [CrossRef]
- Bruen, D.M.; Kingaard, J.J.; Munits, M.; Paimanta, C.S.; Torres, J.A.; Saville, J.; Weimbs, T. Ren.Nu, a Dietary Program for Individuals with Autosomal-Dominant Polycystic Kidney Disease Implementing a Sustainable, Plant-Focused, Kidney-Safe, Ketogenic Approach with Avoidance of Renal Stressors. Kidney Dial. 2022, 2, 183–203. [Google Scholar] [CrossRef]
- Testa, F.; Marchiò, M.; Belli, M.; Giovanella, S.; Ligabue, G.; Cappelli, G.; Biagini, G.; Magistroni, R. A pilot study to evaluate tolerability and safety of a modified Atkins diet in ADPKD patients. PharmaNutrition 2019, 9, 100154. [Google Scholar] [CrossRef]
- Oehm, S.; Steinke, K.; Schmidt, J.; Arjune, S.; Todorova, P.; Lindemann, C.H.; Wöstmann, F.; Meyer, F.; Siedek, F.; Weimbs, T.; et al. RESET-PKD: A pilot trial on short-term ketogenic interventions in autosomal dominant polycystic kidney disease. Nephrol. Dial. Transplant. 2022. [Google Scholar] [CrossRef]
- Time Restricted Feeding in Autosomal Dominant Polycystic Kidney Disease—Full Text View—ClinicalTrials.gov. Available online: https://clinicaltrials.gov/ct2/show/NCT04534985?term=diet&cond=ADPKD&draw=2&rank=7 (accessed on 9 February 2023).
- Daily Caloric Restriction in ADPKD—Full Text View—ClinicalTrials.gov. Available online: https://clinicaltrials.gov/ct2/show/NCT04907799?term=diet&cond=ADPKD&draw=3&rank=17 (accessed on 9 February 2023).
- Ketogenic Dietary Interventions in Autosomal Dominant Polycystic Kidney Disease (ADPKD)—Full Text View—ClinicalTrials.gov. Available online: https://clinicaltrials.gov/ct2/show/NCT04680780 (accessed on 9 February 2023).
- Cheung, A.K.; Chang, T.I.; Cushman, W.C.; Furth, S.L.; Hou, F.F.; Ix, J.H.; Knoll, G.A.; Muntner, P.; Pecoits-Filho, R.; Sarnak, M.J.; et al. KDIGO 2021 Clinical Practice Guideline for the Management of Blood Pressure in Chronic Kidney Disease. Kidney Int. 2021, 99, S1–S87. [Google Scholar] [CrossRef] [PubMed]
- Mustata, S.; Groeneveld, S.; Davidson, W.; Ford, G.; Kiland, K.; Manns, B. Effects of exercise training on physical impairment, arterial stiffness and health-related quality of life in patients with chronic kidney disease: A pilot study. Int. Urol. Nephrol. 2011, 43, 1133–1141. [Google Scholar] [CrossRef] [PubMed]
- Aucella, F. Physical Activity in ADPKD and CKD Patient. G. Di Tec. Nefrol. E Dial. 2015, 27, 204–209. [Google Scholar] [CrossRef]
- Reinecke, N.L.; Cunha, T.M.; Heilberg, I.P.; Higa, E.M.S.; Nishiura, J.L.; Neder, J.A.; Almeida, W.S.; Schor, N. Exercise capacity in polycystic kidney disease. Am. J. Kidney Dis. 2014, 64, 239–246. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Vea, A.; Bardaji, A.; Gutierrez, C.; García, C.; Peralta, C.; Marcas, L.; Oliver, J.A. Exercise blood pressure, cardiac structure, and diastolic function in young normotensive patients with polycystic kidney disease: A prehypertensive state. Am. J. Kidney Dis. 2004, 44, 216–223. [Google Scholar] [CrossRef]
- Orscelik, O.; Kocyigit, I.; Baran, O.; Kaya, C.; Dogdu, O.; Zengin, H.; Karadavut, S.; Gedikli, O.; Kut, E.; Duran, M.; et al. Impairment of heart rate recovery index in autosomal-dominant polycystic kidney disease patients without hypertension. Blood Press. 2012, 21, 300–305. [Google Scholar] [CrossRef]
- Provenzano, M.; Andreucci, M.; De Nicola, L.; Garofalo, C.; Battaglia, Y.; Borrelli, S.; Gagliardi, I.; Faga, T.; Michael, A.; Mastroroberto, P.; et al. The Role of Prognostic and Predictive Biomarkers for Assessing Cardiovascular Risk in Chronic Kidney Disease Patients. Biomed. Res. Int. 2020, 2020, 2314128. [Google Scholar] [CrossRef]

| CKD Stage | eGFR | Daily Amount of Protein |
|---|---|---|
| Stage 1 | ≥90 mL/min | 0.8 mg/kg/die |
| Stage 2 | 60–89 mL/min | |
| Stage 3a | 45–59 mL/min | |
| Stage 3b | 30–44 mL/min | 0.6 mg/kg/die |
| Sage 4 | 15–29 mL/min | 0.6 mg/kg/die or 0.4–0.3 mg/kg/die + ketoanalogues |
| Stage 5 | ≤14 mL/min |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Capelli, I.; Lerario, S.; Aiello, V.; Provenzano, M.; Di Costanzo, R.; Squadrani, A.; Vella, A.; Vicennati, V.; Poli, C.; La Manna, G.; et al. Diet and Physical Activity in Adult Dominant Polycystic Kidney Disease: A Review of the Literature. Nutrients 2023, 15, 2621. https://doi.org/10.3390/nu15112621
Capelli I, Lerario S, Aiello V, Provenzano M, Di Costanzo R, Squadrani A, Vella A, Vicennati V, Poli C, La Manna G, et al. Diet and Physical Activity in Adult Dominant Polycystic Kidney Disease: A Review of the Literature. Nutrients. 2023; 15(11):2621. https://doi.org/10.3390/nu15112621
Chicago/Turabian StyleCapelli, Irene, Sarah Lerario, Valeria Aiello, Michele Provenzano, Roberta Di Costanzo, Andrea Squadrani, Anna Vella, Valentina Vicennati, Carolina Poli, Gaetano La Manna, and et al. 2023. "Diet and Physical Activity in Adult Dominant Polycystic Kidney Disease: A Review of the Literature" Nutrients 15, no. 11: 2621. https://doi.org/10.3390/nu15112621