Potential Association of Osteoporosis and Not Osteoporotic Fractures in Patients with Gout: A Longitudinal Follow-Up Study
Abstract
:1. Introduction
2. Materials and Methods
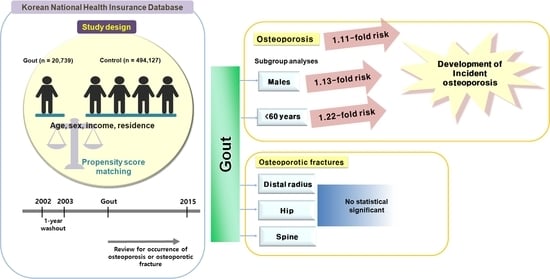
2.1. Study Design and Participant Selection
2.2. Definition of Gout (Independent Variable)
2.3. Definition of Osteoporosis and Osteoporotic Fractures (Dependent Variable)
2.4. Covariates
2.5. Statistical Analyses
3. Results
3.1. Baseline Characteristics
3.2. The Occurrence of Osteoporosis in the Gout and Control Groups
3.3. The Occurrence of Osteoporotic Fractures
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Richette, P.; Bardin, T. Gout. Lancet 2010, 375, 318–328. [Google Scholar] [CrossRef] [PubMed]
- Rai, S.K.; Burns, L.C.; De Vera, M.A.; Haji, A.; Giustini, D.; Choi, H.K. The economic burden of gout: A systematic review. Semin. Arthritis Rheum. 2015, 45, 75–80. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Pandya, B.J.; Choi, H.K. Prevalence of gout and hyperuricemia in the US general population: The National Health and Nutrition Examination Survey 2007–2008. Arthritis Rheum. 2011, 63, 3136–3141. [Google Scholar] [CrossRef]
- Kuo, C.F.; Grainge, M.J.; See, L.C.; Yu, K.H.; Luo, S.F.; Zhang, W.; Doherty, M. Epidemiology and management of gout in Taiwan: A nationwide population study. Arthritis Res. Ther. 2015, 17, 13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kuo, C.F.; Grainge, M.J.; Mallen, C.; Zhang, W.; Doherty, M. Rising burden of gout in the UK but continuing suboptimal management: A nationwide population study. Ann. Rheum. Dis. 2015, 74, 661–667. [Google Scholar] [CrossRef] [Green Version]
- Park, J.S.; Kang, M.; Song, J.-S.; Kim, H.S.; Lee, C.H. Trends of Gout Prevalence in South Korea Based on Medical Utilization: A National Health Insurance Service Database (2002∼2015). J. Rheum. Dis. 2020, 27, 174–181. [Google Scholar] [CrossRef]
- Kuo, C.F.; Grainge, M.J.; Zhang, W.; Doherty, M. Global epidemiology of gout: Prevalence, incidence and risk factors. Nat. Rev. Rheumatol. 2015, 11, 649–662. [Google Scholar] [CrossRef]
- Kim, S.C.; Liu, J.; Solomon, D.H. Risk of incident atrial fibrillation in gout: A cohort study. Ann. Rheum. Dis. 2016, 75, 1473–1478. [Google Scholar] [CrossRef] [Green Version]
- Borghi, C.; Agabiti-Rosei, E.; Johnson, R.J.; Kielstein, J.T.; Lurbe, E.; Mancia, G.; Redon, J.; Stack, A.G.; Tsioufis, K.P. Hyperuricaemia and gout in cardiovascular, metabolic and kidney disease. Eur. J. Int. Med. 2020, 80, 1–11. [Google Scholar] [CrossRef]
- Tzeng, H.E.; Lin, C.C.; Wang, I.K.; Huang, P.H.; Tsai, C.H. Gout increases risk of fracture: A nationwide population-based cohort study. Medicine 2016, 95, e4669. [Google Scholar] [CrossRef]
- Wang, Y.; Zhou, R.; Zhong, W.; Hu, C.; Lu, S.; Chai, Y. Association of gout with osteoporotic fractures. Int. Orthop. 2018, 42, 2041–2047. [Google Scholar] [CrossRef] [PubMed]
- Park, C.; Ha, Y.C.; Jang, S.; Jang, S.; Yoon, H.K.; Lee, Y.K. The incidence and residual lifetime risk of osteoporosis-related fractures in Korea. J. Bone Miner. Metab. 2011, 29, 744–751. [Google Scholar] [CrossRef] [PubMed]
- Ginaldi, L.; Di Benedetto, M.C.; De Martinis, M. Osteoporosis, inflammation and ageing. Immun. Ageing 2005, 2, 14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chhana, A.; Callon, K.E.; Pool, B.; Naot, D.; Watson, M.; Gamble, G.D.; McQueen, F.M.; Cornish, J.; Dalbeth, N. Monosodium urate monohydrate crystals inhibit osteoblast viability and function: Implications for development of bone erosion in gout. Ann. Rheum. Dis. 2011, 70, 1684–1691. [Google Scholar] [CrossRef] [PubMed]
- Yokose, K.; Sato, S.; Asano, T.; Yashiro, M.; Kobayashi, H.; Watanabe, H.; Suzuki, E.; Sato, C.; Kozuru, H.; Yatsuhashi, H.; et al. TNF-alpha potentiates uric acid-induced interleukin-1beta (IL-1beta) secretion in human neutrophils. Mod. Rheumatol. 2018, 28, 513–517. [Google Scholar] [CrossRef] [PubMed]
- Paik, J.M.; Kim, S.C.; Feskanich, D.; Choi, H.K.; Solomon, D.H.; Curhan, G.C. Gout and Risk of Fracture in Women: A Prospective Cohort Study. Arthritis Rheumatol. 2017, 69, 422–428. [Google Scholar] [CrossRef] [Green Version]
- Dennison, E.M.; Rubin, K.H.; Schwarz, P.; Harvey, N.C.; Bone, K.W.; Cooper, C.; Abrahamsen, B. Is allopurinol use associated with an excess risk of osteoporotic fracture? A National Prescription Registry study. Arch. Osteop. 2015, 10, 36. [Google Scholar] [CrossRef] [Green Version]
- Kim, S.C.; Paik, J.M.; Liu, J.; Curhan, G.C.; Solomon, D.H. Gout and the Risk of Non-vertebral Fracture. J. Bone Miner. Res. 2017, 32, 230–236. [Google Scholar] [CrossRef] [Green Version]
- Sultan, A.A.; Whittle, R.; Muller, S.; Roddy, E.; Mallen, C.D.; Bucknall, M.; Helliwell, T.; Hider, S.; Paskins, Z. Risk of fragility fracture among patients with gout and the effect of urate-lowering therapy. CMAJ 2018, 190, E581–E587. [Google Scholar] [CrossRef] [Green Version]
- Liu, F.; Dong, J.; Zhou, D.; Kang, Q.; Xiong, F. Gout is not associated with the risk of fracture: A meta-analysis. J. Orthop. Surg. Res. 2019, 14, 272. [Google Scholar] [CrossRef]
- Dogru, A.; Balkarli, A.; Karatay, C.C.; Cobankara, V.; Sahin, M. Bone mineral density and serum osteocalcin levels in patients with gout. Acta Clin. Belg. 2019, 74, 252–257. [Google Scholar] [CrossRef] [PubMed]
- Kok, V.C.; Horng, J.T.; Wang, M.N.; Chen, Z.Y.; Kuo, J.T.; Hung, G.D. Gout as a risk factor for osteoporosis: Epidemiologic evidence from a population-based longitudinal study involving 108,060 individuals. Osteop. Int. 2018, 29, 973–985. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.Y.; Min, C.; Oh, D.J.; Choi, H.G. Tobacco Smoking and Alcohol Consumption Are Related to Benign Parotid Tumor: A Nested Case-Control Study Using a National Health Screening Cohort. Clin. Exp. Otorhinolaryngol. 2019, 12, 412–419. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, J.W.; Kwak, S.G.; Lee, H.; Kim, S.K.; Choe, J.Y.; Park, S.H. Prevalence and incidence of gout in Korea: Data from the national health claims database 2007-2015. Rheumatol. Int. 2017, 37, 1499–1506. [Google Scholar] [CrossRef]
- Kim, S.Y.; Kim, H.J.; Min, C.; Choi, H.G. Association between benign paroxysmal positional vertigo and osteoporosis: Two nested case-control studies. Osteop. Int. 2020, 31, 2017–2024. [Google Scholar] [CrossRef]
- Kwon, M.J.; Kim, J.H.; Kim, J.H.; Cho, S.J.; Nam, E.S.; Choi, H.G. The Occurrence of Alzheimer’s Disease and Parkinson’s Disease in Individuals With Osteoporosis: A Longitudinal Follow-Up Study Using a National Health Screening Database in Korea. Front. Ageing Neurosci. 2021, 13, 786337. [Google Scholar] [CrossRef]
- Choi, H.G.; Kim, D.S.; Lee, B.; Youk, H.; Lee, J.W. High Risk of Hip and Spinal Fractures after Distal Radius Fracture: A Longitudinal Follow-Up Study Using a National Sample Cohort. Int. J. Environ. Res. Public Health 2021, 18, 7391. [Google Scholar] [CrossRef]
- Kim, S.Y.; Lee, J.K.; Lim, J.S.; Park, B.; Choi, H.G. Increased risk of dementia after distal radius, hip, and spine fractures. Medicine 2020, 99, e19048. [Google Scholar] [CrossRef]
- Lee, J.W.; Lee, Y.B.; Kwon, B.C.; Yoo, J.H.; Choi, H.G. Mortality and cause of death in distal radius fracture patients: A longitudinal follow-up study using a national sample cohort. Medicine 2019, 98, e18604. [Google Scholar] [CrossRef]
- Kim, S.Y.; Min, C.; Oh, D.J.; Choi, H.G. Bidirectional Association Between GERD and Asthma: Two Longitudinal Follow-Up Studies Using a National Sample Cohort. J. Allerg. Clin. Immunol. Pract. 2020, 8, 1005–1013.e1009. [Google Scholar] [CrossRef]
- Kim, S.Y.; Oh, D.J.; Park, B.; Choi, H.G. Bell’s palsy and obesity, alcohol consumption and smoking: A nested case-control study using a national health screening cohort. Sci. Rep. 2020, 10, 4248. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Quan, H.; Li, B.; Couris, C.M.; Fushimi, K.; Graham, P.; Hider, P.; Januel, J.M.; Sundararajan, V. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am. J. Epidemiol. 2011, 173, 676–682. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, D.; Dalton, J.E. A unified approach to measuring the effect size between two groups using SAS. In Proceedings of the SAS Global Forum Statistics Data Analysis, Cleveland, OH, USA, 22–25 April 2012. Paper 335-2012. [Google Scholar]
- Austin, P.C. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat. Med. 2009, 28, 3083–3107. [Google Scholar] [CrossRef] [Green Version]
- Ferrandez-Jimenez, M.; Calabuig, I.; Peral-Garrido, M.L.; Gomez-Garberi, M.; Andres, M. Risk of osteoporotic thoracic vertebral fractures in patients with gout. Reumatol. Clin. Eng. Ed. 2022, 18, 279–285. [Google Scholar] [CrossRef] [PubMed]
- Yao, Y.; Chu, X.; Ma, M.; Ye, J.; Wen, Y.; Li, P.; Cheng, B.; Cheng, S.; Zhang, L.; Liu, L.; et al. Evaluate the effects of serum urate level on bone mineral density: A genome-wide gene-environment interaction analysis in UK Biobank cohort. Endocrine 2021, 73, 702–711. [Google Scholar] [CrossRef] [PubMed]
- Chung, P.C.; Chan, T.C. Environmental and personal factors for osteoporosis or osteopenia from a large health check-up database: A retrospective cohort study in Taiwan. BMC Public Health 2022, 22, 1531. [Google Scholar] [CrossRef] [PubMed]
- Lin, K.M.; Lu, C.L.; Hung, K.C.; Wu, P.C.; Pan, C.F.; Wu, C.J.; Syu, R.S.; Chen, J.S.; Hsiao, P.J.; Lu, K.C. The Paradoxical Role of Uric Acid in Osteoporosis. Nutrients 2019, 11, 2111. [Google Scholar] [CrossRef] [Green Version]
- Manolagas, S.C.; Jilka, R.L. Bone marrow, cytokines, and bone remodeling. Emerging insights into the pathophysiology of osteoporosis. N. Engl. J. Med. 1995, 332, 305–311. [Google Scholar] [CrossRef]
- Siggelkow, H.; Eidner, T.; Lehmann, G.; Viereck, V.; Raddatz, D.; Munzel, U.; Hein, G.; Hufner, M. Cytokines, osteoprotegerin, and RANKL in vitro and histomorphometric indices of bone turnover in patients with different bone diseases. J. Bone Miner. Res. 2003, 18, 529–538. [Google Scholar] [CrossRef]
- Wei, S.; Kitaura, H.; Zhou, P.; Ross, F.P.; Teitelbaum, S.L. IL-1 mediates TNF-induced osteoclastogenesis. J. Clin. Investig. 2005, 115, 282–290. [Google Scholar] [CrossRef]
- Amaral, F.A.; Bastos, L.F.; Oliveira, T.H.; Dias, A.C.; Oliveira, V.L.; Tavares, L.D.; Costa, V.V.; Galvao, I.; Soriani, F.M.; Szymkowski, D.E.; et al. Transmembrane TNF-alpha is sufficient for articular inflammation and hypernociception in a mouse model of gout. Eur. J. Immunol. 2016, 46, 204–211. [Google Scholar] [CrossRef] [PubMed]
- Joosten, L.A.; Netea, M.G.; Mylona, E.; Koenders, M.I.; Malireddi, R.K.; Oosting, M.; Stienstra, R.; van de Veerdonk, F.L.; Stalenhoef, A.F.; Giamarellos-Bourboulis, E.J.; et al. Engagement of fatty acids with Toll-like receptor 2 drives interleukin-1beta production via the ASC/caspase 1 pathway in monosodium urate monohydrate crystal-induced gouty arthritis. Arthritis Rheum. 2010, 62, 3237–3248. [Google Scholar] [CrossRef] [PubMed]
- Pacifici, R.; Rifas, L.; McCracken, R.; Vered, I.; McMurtry, C.; Avioli, L.V.; Peck, W.A. Ovarian steroid treatment blocks a postmenopausal increase in blood monocyte interleukin 1 release. Proc. Natl. Acad. Sci. USA 1989, 86, 2398–2402. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zeng, J.; Li, K.; Gong, Y.; Xu, L.; Li, C.; Wang, L.; Zhang, Y.; Cheng, X. Association of pro-inflammatory cytokines with QCT-measured bone mineral density and its gender difference in a Chinese population-a pilot study. Endokrynol. Pol. 2019, 70, 248–254. [Google Scholar] [CrossRef]


| Characteristics | Total Participants | ||
|---|---|---|---|
| Gout (n = 16,305) | Control (n = 65,220) | Standardized Difference | |
| Age (years old, n, %) | 0.00 | ||
| 40–44 | 571 (3.5) | 2284 (3.5) | |
| 45–49 | 2008 (12.3) | 8032 (12.3) | |
| 50–54 | 3309 (20.3) | 13,236 (20.3) | |
| 55–59 | 3101 (19.0) | 12,404 (19.0) | |
| 60–64 | 2531 (15.5) | 10,124 (15.5) | |
| 65–69 | 2134 (13.1) | 8536 (13.1) | |
| 70–74 | 1488 (9.1) | 5952 (9.1) | |
| 75–79 | 823 (5.1) | 3292 (5.1) | |
| 80–84 | 277 (1.7) | 1108 (1.7) | |
| ≥85 | 63 (0.4) | 252 (0.4) | |
| Sex (n, %) | 0.00 | ||
| Male | 13,941 (85.5) | 55,764 (85.5) | |
| Female | 2364 (14.5) | 9456 (14.5) | |
| Income (n, %) | 0.00 | ||
| 1 (lowest) | 2175 (13.3) | 8700 (13.3) | |
| 2 | 1997 (12.3) | 7988 (12.3) | |
| 3 | 2500 (15.3) | 10,000 (15.3) | |
| 4 | 3430 (21.0) | 13,720 (21.0) | |
| 5 (highest) | 6203 (38.0) | 24,812 (38.0) | |
| Region of residence (n, %) | 0.00 | ||
| Urban | 7048 (43.2) | 28,192 (43.2) | |
| Rural | 9257 (56.8) | 37,028 (56.8) | |
| Total cholesterol level (mg/dL, mean, SD) | 200.2 (40.1) | 196.1 (37.1) | 0.11 |
| SBP (mmHg, mean, SD) | 130.2 (17.3) | 127.4 (16.4) | 0.17 |
| DBP (mmHg, mean, SD) | 81.1 (11.2) | 79.3 (10.7) | 0.16 |
| Fasting blood glucose level (mg/dL, mean, SD) | 101.6 (28.8) | 102.1 (30.9) | 0.02 |
| Obesity † (n, %) | 0.29 | ||
| Underweight | 193 (1.2) | 1510 (2.3) | |
| Normal | 3999 (24.5) | 22,726 (34.9) | |
| Overweight | 4507 (27.6) | 18,411 (28.2) | |
| Obese I | 6945 (42.6) | 21,068 (32.3) | |
| Obese II | 661 (4.1) | 1505 (2.3) | |
| Smoking status (n, %) | 0.08 | ||
| Nonsmoker | 8886 (54.5) | 34,681 (53.2) | |
| Past smoker | 3403 (20.9) | 12,280 (18.8) | |
| Current smoker | 4016 (24.6) | 18,259 (28.0) | |
| Alcohol consumption (n, %) | 0.11 | ||
| <1 time a week | 8108 (49.7) | 35,919 (55.1) | |
| ≥1 time a week | 8197 (50.3) | 29,301 (44.9) | |
| CCI score (score, n, %) | 0.13 | ||
| 0 | 10,359 (63.5) | 45,309 (69.5) | |
| 1 | 2425 (14.9) | 8563 (13.1) | |
| 2 | 1490 (9.1) | 4971 (7.6) | |
| ≥3 | 2031 (12.5) | 6377 (9.8) | |
| Osteoporosis (n, %) | 761 (4.7) | 2805 (4.3) | 0.02 |
| Distal radius fracture (n, %) | 277 (1.7) | 1052 (1.6) | 0.01 |
| Hip fracture (n, %) | 127 (0.8) | 500 (0.8) | 0.00 |
| Spine fracture (n, %) | 437 (2.7) | 1746 (2.7) | 0.00 |
| Characteristics | No. of Osteoporosis/ No. of Participants | Follow-Up Duration, Person-Years | Incidence Rate, Per 1000 Person-Years | Hazard Ratios for Osteoporosis | |||
|---|---|---|---|---|---|---|---|
| Crude † | p-Value | Adjusted ‡ | p-Value | ||||
| Total participants (n = 81,525) | |||||||
| Gout | 761/16,305 | 94,898 | 8.0 | 1.10 (1.01–1.19) | 0.022 | 1.11 (1.02–1.20) | 0.011 * |
| Control | 2805/65,220 | 382,132 | 7.3 | 1 | 1 | ||
| Age < 60 years old (n = 44,945) | |||||||
| Gout | 255/8989 | 60,212 | 4.2 | 1.21 (1.05–1.39) | 0.009 * | 1.22 (1.06–1.41) | 0.005 * |
| Control | 859/35,956 | 242,560 | 3.5 | 1 | 1 | ||
| Age ≥ 60 years old (n = 36,580) | |||||||
| Gout | 506/7316 | 34,686 | 14.6 | 1.05 (0.95–1.16) | 0.324 | 1.06 (0.96–1.17) | 0.250 |
| Control | 1946/29,264 | 139,572 | 13.9 | 1 | 1 | ||
| Males (n = 69,705) | |||||||
| Gout | 344/13,941 | 82,815 | 4.2 | 1.08 (0.96–1.22) | 0.189 | 1.13 (1.00–1.28) | 0.043 |
| Control | 1270/55,764 | 332,450 | 3.8 | 1 | 1 | ||
| Females (n = 11,820) | |||||||
| Gout | 417/2364 | 12,083 | 34.5 | 1.11 (1.00–1.24) | 0.058 | 1.11 (1.00–1.24) | 0.055 |
| Control | 1535/9456 | 49,682 | 30.9 | 1 | 1 | ||
| Characteristics | No. of Distal Radius Fracture/ No. of Participants | Follow-Up Duration, Person-Years | Incidence Rate, Per 1000 Person-Years | Hazard Ratios for Distal Radius Fracture | |||
|---|---|---|---|---|---|---|---|
| Crude † | p | Adjusted ‡ | p | ||||
| Total participants (n = 81,525) | |||||||
| Gout | 277/16,305 | 97,976 | 2.8 | 1.06 (0.93–1.21) | 0.401 | 1.06 (0.93–1.21) | 0.413 |
| Control | 1052/65,220 | 392,452 | 2.7 | 1 | 1 | ||
| Age < 60 years old (n = 44,945) | |||||||
| Gout | 142/8989 | 61,058 | 2.3 | 1.09 (0.91–1.31) | 0.367 | 1.08 (0.90–1.31) | 0.411 |
| Control | 525/35,956 | 245,087 | 2.1 | 1 | 1 | ||
| Age ≥ 60 years old (n = 36,580) | |||||||
| Gout | 135/7316 | 36,918 | 3.7 | 1.03 (0.85–1.24) | 0.774 | 1.03 (0.85–1.25) | 0.766 |
| Control | 527/29,264 | 147,365 | 3.6 | 1 | 1 | ||
| Males (n = 69,705) | |||||||
| Gout | 169/13,941 | 83,807 | 2.0 | 1.04 (0.88–1.23) | 0.666 | 1.06 (0.89–1.26) | 0.519 |
| Control | 652/55,764 | 335,341 | 1.9 | 1 | 1 | ||
| Females (n = 11,820) | |||||||
| Gout | 108/2364 | 14,169 | 7.6 | 1.09 (0.88–1.35) | 0.414 | 1.05 (0.85–1.31) | 0.645 |
| Control | 400/9,456 | 57,111 | 7.0 | 1 | 1 | ||
| Characteristics | No. of Hip Fracture/ No. of Participants | Follow-Up Duration, Person-Years | Incidence Rate, Per 1000 Person-Years | Hazard Ratios for Hip Fracture | |||
|---|---|---|---|---|---|---|---|
| Crude † | p | Adjusted ‡ | p | ||||
| Total participants (n = 81,525) | |||||||
| Gout | 127/16,305 | 98,689 | 1.3 | 1.02 (0.84–1.24) | 0.872 | 1.00 (0.82–1.22) | 0.997 |
| Control | 500/65,220 | 395,473 | 1.3 | 1 | 1 | ||
| Age < 60 years old (n = 44,945) | |||||||
| Gout | 31/8989 | 61,573 | 0.5 | 1.27 (0.85–1.90) | 0.245 | 1.23 (0.81–1.85) | 0.335 |
| Control | 98/35,956 | 247,060 | 0.4 | 1 | 1 | ||
| Age ≥ 60 years old (n = 36,580) | |||||||
| Gout | 96/7316 | 37,116 | 2.6 | 0.95 (0.76–1.19) | 0.679 | 0.94 (0.75–1.18) | 0.604 |
| Control | 402/29,264 | 148,413 | 2.7 | 1 | 1 | ||
| Males (n = 69,705) | |||||||
| Gout | 108/13,941 | 84,172 | 1.3 | 1.05 (0.85–1.30) | 0.641 | 1.09 (0.88–1.35) | 0.445 |
| Control | 410/55,764 | 336,974 | 1.2 | 1 | 1 | ||
| Females (n = 11,820) | |||||||
| Gout | 19/2364 | 14,517 | 1.3 | 0.85 (0.52–1.40) | 0.527 | 0.71 (0.42–1.19) | 0.191 |
| Control | 90/9456 | 58,499 | 1.5 | 1 | 1 | ||
| Characteristics | No. of Spine Fracture/ No. of Participants | Follow-Up Duration, Person-Years | Incidence Rate, Per 1000 Person-Years | Hazard Ratios for Spine Fracture | |||
|---|---|---|---|---|---|---|---|
| Crude † | p | Adjusted ‡ | p | ||||
| Total participants (n = 81,525) | |||||||
| Gout | 437/16,305 | 97,555 | 4.5 | 1.00 (0.90–1.12) | 0.943 | 0.98 (0.88–1.09) | 0.642 |
| Control | 1746/65,220 | 390,661 | 4.5 | 1 | 1 | ||
| Age < 60 years old (n = 44,945) | |||||||
| Gout | 132/8989 | 61,194 | 2.2 | 1.11 (0.92–1.35) | 0.287 | 1.06 (0.87–1.29) | 0.562 |
| Control | 479/35,956 | 245,546 | 2.0 | 1 | 1 | ||
| Age ≥ 60 years old (n = 36,580) | |||||||
| Gout | 305/7316 | 36,361 | 8.4 | 0.96 (0.85–1.09) | 0.567 | 0.94 (0.83–1.07) | 0.359 |
| Control | 1267/29,264 | 145,115 | 8.7 | 1 | 1 | ||
| Males (n = 69,705) | |||||||
| Gout | 330/13,941 | 83,344 | 4.0 | 1.02 (0.91–1.16) | 0.711 | 1.03 (0.91–1.16) | 0.679 |
| Control | 1286/55,764 | 333,657 | 3.9 | 1 | 1 | ||
| Females (n = 11,820) | |||||||
| Gout | 107/2364 | 14,211 | 7.5 | 0.95 (0.77–1.17) | 0.627 | 0.86 (0.69–1.06) | 0.160 |
| Control | 460/9456 | 57,004 | 8.1 | 1 | 1 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwon, M.J.; Park, J.Y.; Kim, S.G.; Kim, J.-K.; Lim, H.; Kim, J.-H.; Kim, J.H.; Cho, S.-J.; Nam, E.S.; Park, H.Y.; et al. Potential Association of Osteoporosis and Not Osteoporotic Fractures in Patients with Gout: A Longitudinal Follow-Up Study. Nutrients 2023, 15, 134. https://doi.org/10.3390/nu15010134
Kwon MJ, Park JY, Kim SG, Kim J-K, Lim H, Kim J-H, Kim JH, Cho S-J, Nam ES, Park HY, et al. Potential Association of Osteoporosis and Not Osteoporotic Fractures in Patients with Gout: A Longitudinal Follow-Up Study. Nutrients. 2023; 15(1):134. https://doi.org/10.3390/nu15010134
Chicago/Turabian StyleKwon, Mi Jung, Jae Yong Park, Sung Gyun Kim, Jwa-Kyung Kim, Hyun Lim, Joo-Hee Kim, Ji Hee Kim, Seong-Jin Cho, Eun Sook Nam, Ha Young Park, and et al. 2023. "Potential Association of Osteoporosis and Not Osteoporotic Fractures in Patients with Gout: A Longitudinal Follow-Up Study" Nutrients 15, no. 1: 134. https://doi.org/10.3390/nu15010134