Iron Deficiency in Cystic Fibrosis: A Cross-Sectional Single-Centre Study in a Referral Adult Centre
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
- -
- New or increased cough, sputum production or chest congestion.
- -
- Decreased exercise tolerance, increased dyspnoea.
- -
- Increased fatigue, decreased appetite.
- -
- Increase respiratory rate or dyspnoea at rest.
- -
- Change in sputum appearance.
- -
- Fever.
2.2. Data Collection
2.3. Anaemia and Micronutrient Deficiency Definitions
- (i)
- The international recommended biological definition of ID [11] was used as our primary endpoint: ferritin ≤20 (women) or 30 (men) μg/L, or ≤100 μg/L in the case of systemic inflammation (CRP ≥ 10 mg/L) or TSAT ≤ 16%.
- (ii)
2.4. Statistics
2.5. Ethics
3. Results
3.1. Baseline Characteristics
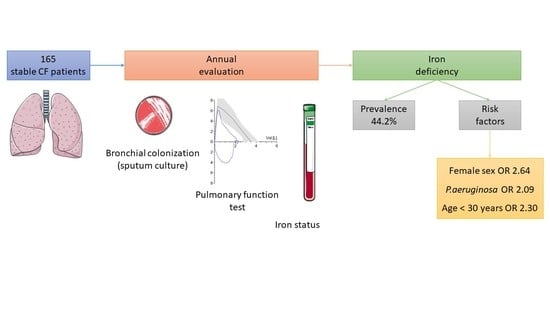
3.2. Iron Deficiency Prevalence
3.3. Iron Deficiency Risk Factors
3.3.1. Univariate Analysis
3.3.2. Multivariate Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- GBD. 2017 Disease and Injury Incidence and Prevalence Collaborators Global, Regional, and National Incidence, Prevalence, and Years Lived with Disability for 354 Diseases and Injuries for 195 Countries and Territories, 1990-2017: A Systematic Analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1789–1858. [Google Scholar] [CrossRef] [Green Version]
- Fischer, R.; Simmerlein, R.; Huber, R.M.; Schiffl, H.; Lang, S.M. Lung Disease Severity, Chronic Inflammation, Iron Deficiency, and Erythropoietin Response in Adults with Cystic Fibrosis. Pediatric Pulmonol. 2007, 42, 1193–1197. [Google Scholar] [CrossRef] [PubMed]
- Staudinger, B.J.; Muller, J.F.; Halldórsson, S.; Boles, B.; Angermeyer, A.; Nguyen, D.; Rosen, H.; Baldursson, Ó.; Gottfreðsson, M.; Guðmundsson, G.H.; et al. Conditions Associated with the Cystic Fibrosis Defect Promote Chronic Pseudomonas Aeruginosa Infection. Am. J. Respir. Crit. Care Med. 2014, 189, 812–824. [Google Scholar] [CrossRef] [Green Version]
- Smith, D.J.; Lamont, I.L.; Anderson, G.J.; Reid, D.W. Targeting Iron Uptake to Control Pseudomonas Aeruginosa Infections in Cystic Fibrosis. Eur. Respir. J. 2013, 42, 1723–1736. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Keevil, B.; Rowlands, D.; Burton, I.; Webb, A.K. Assessment of Iron Status in Cystic Fibrosis Patients. Ann. Clin. Biochem. 2000, 37 Pt 5, 662–665. [Google Scholar] [CrossRef]
- Reid, D.W.; Withers, N.J.; Francis, L.; Wilson, J.W.; Kotsimbos, T.C. Iron Deficiency in Cystic Fibrosis: Relationship to Lung Disease Severity and Chronic Pseudomonas Aeruginosa Infection. Chest 2002, 121, 48–54. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Uijterschout, L.; Nuijsink, M.; Hendriks, D.; Vos, R.; Brus, F. Iron Deficiency Occurs Frequently in Children with Cystic Fibrosis. Pediatric Pulmonol. 2014, 49, 458–462. [Google Scholar] [CrossRef]
- von Drygalski, A.; Biller, J. Anemia in Cystic Fibrosis: Incidence, Mechanisms, and Association with Pulmonary Function and Vitamin Deficiency. Nutr. Clin. Pract. 2008, 23, 557–563. [Google Scholar] [CrossRef] [Green Version]
- Smith, D.J.; Anderson, G.J.; Lamont, I.L.; Masel, P.; Bell, S.C.; Reid, D.W. Accurate Assessment of Systemic Iron Status in Cystic Fibrosis Will Avoid the Hazards of Inappropriate Iron Supplementation. J. Cyst. Fibros. 2013, 12, 303–304. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gettle, L.S.; Harden, A.; Bridges, M.; Albon, D. Prevalence and Risk Factors for Iron Deficiency in Adults With Cystic Fibrosis. Nutr. Clin. Pract. 2020, 35, 1101–1109. [Google Scholar] [CrossRef] [PubMed]
- Camaschella, C. Iron Deficiency. Blood 2019, 133, 30–39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nemeth, E.; Ganz, T. Hepcidin-Ferroportin Interaction Controls Systemic Iron Homeostasis. Int. J. Mol. Sci. 2021, 22, 6493. [Google Scholar] [CrossRef] [PubMed]
- Fuchs, H.J.; Borowitz, D.S.; Christiansen, D.H.; Morris, E.M.; Nash, M.L.; Ramsey, B.W.; Rosenstein, B.J.; Smith, A.L.; Wohl, M.E. Effect of Aerosolized Recombinant Human DNase on Exacerbations of Respiratory Symptoms and on Pulmonary Function in Patients with Cystic Fibrosis. The Pulmozyme Study Group. N. Engl. J. Med. 1994, 331, 637–642. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Haemoglobin Concentrations for the Diagnosis of Anaemia and Assessment of Severity; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Ehrhardt, P.; Miller, M.G.; Littlewood, J.M. Iron Deficiency in Cystic Fibrosis. Arch. Dis. Child. 1987, 62, 185–187. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khalid, S.; McGrowder, D.; Kemp, M.; Johnson, P. The Use of Soluble Transferin Receptor to Assess Iron Deficiency in Adults with Cystic Fibrosis. Clin. Chim. Acta 2007, 378, 194–200. [Google Scholar] [CrossRef]
- Favrat, B.; Balck, K.; Breymann, C.; Hedenus, M.; Keller, T.; Mezzacasa, A.; Gasche, C. Evaluation of a Single Dose of Ferric Carboxymaltose in Fatigued, Iron-Deficient Women—PREFER a Randomized, Placebo-Controlled Study. PLoS ONE 2014, 9, e94217. [Google Scholar] [CrossRef] [Green Version]
- Holick, M.F. Vitamin D Deficiency. N. Engl. J. Med. 2007, 357, 266–281. [Google Scholar] [CrossRef]
- Raederstorff, D.; Wyss, A.; Calder, P.C.; Weber, P.; Eggersdorfer, M. Vitamin E Function and Requirements in Relation to PUFA. Br. J. Nutr. 2015, 114, 1113–1122. [Google Scholar] [CrossRef] [Green Version]
- Carazo, A.; Macáková, K.; Matoušová, K.; Krčmová, L.K.; Protti, M.; Mladěnka, P. Vitamin A Update: Forms, Sources, Kinetics, Detection, Function, Deficiency, Therapeutic Use and Toxicity. Nutrients 2021, 13, 1703. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. STROBE Initiative The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. Ann. Intern. Med. 2007, 147, 573–577. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wish, J.B. Assessing Iron Status: Beyond Serum Ferritin and Transferrin Saturation. Clin. J. Am. Soc. Nephrol. 2006, 1 (Suppl. 1), S4–S8. [Google Scholar] [CrossRef]
- Dignass, A.; Farrag, K.; Stein, J. Limitations of Serum Ferritin in Diagnosing Iron Deficiency in Inflammatory Conditions. Int. J. Chronic. Dis. 2018, 2018, 9394060. [Google Scholar] [CrossRef] [Green Version]
- Kałużna-Czyż, M.; Grzybowska-Chlebowczyk, U.; Woś, H.; Więcek, S. Serum Hepcidin Level as a Marker of Iron Status in Children with Cystic Fibrosis. Mediat. Inflamm. 2018, 2018, 3040346. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yadav, K.; Singh, M.; Angurana, S.K.; Attri, S.V.; Sharma, G.; Tageja, M.; Bhalla, A.K. Evaluation of Micronutrient Profile of North Indian Children with Cystic Fibrosis: A Case–Control Study. Pediatr. Res. 2014, 75, 762–766. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gifford, A.H.; Moulton, L.A.; Dorman, D.B.; Olbina, G.; Westerman, M.; Parker, H.W.; Stanton, B.A.; O’Toole, G.A. Iron Homeostasis during Cystic Fibrosis Pulmonary Exacerbation. Clin. Transl. Sci. 2012, 5, 368–373. [Google Scholar] [CrossRef]
- Gifford, A.H.; Miller, S.D.; Jackson, B.P.; Hampton, T.H.; O’Toole, G.A.; Stanton, B.A.; Parker, H.W. Iron and CF-Related Anemia: Expanding Clinical and Biochemical Relationships. Pediatr. Pulmonol. 2011, 46, 160–165. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jaffé, A.; Buchdahl, R.; Bush, A.; Balfour-Lynn, I.M. Are Annual Blood Tests in Preschool Cystic Fibrosis Patients Worthwhile? Arch. Dis. Child. 2002, 87, 518–520. [Google Scholar] [CrossRef]
- Pond, M.N.; Morton, A.M.; Conway, S.P. Functional Iron Deficiency in Adults with Cystic Fibrosis. Respir. Med. 1996, 90, 409–413. [Google Scholar] [CrossRef] [Green Version]
- Zempsky, W.T.; Rosenstein, B.J.; Carroll, J.A.; Oski, F.A. Effect of Pancreatic Enzyme Supplements on Iron Absorption. Am. J. Dis. Child. 1989, 143, 969–972. [Google Scholar] [CrossRef]
- Ater, J.L.; Herbst, J.J.; Landaw, S.A.; O’Brien, R.T. Relative Anemia and Iron Deficiency in Cystic Fibrosis. Pediatrics 1983, 71, 810–814. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention (CDC) Iron Deficiency--United States, 1999-2000. MMWR Morb. Mortal. Wkly. Rep. 2002, 51, 897–899.
- Gillan, J.L.; Davidson, D.J.; Gray, R.D. Targeting Cystic Fibrosis Inflammation in the Age of CFTR Modulators: Focus on Macrophages. Eur. Respir. J. 2021, 57, 2003502. [Google Scholar] [CrossRef]
- Gifford, A.H.; Heltshe, S.L.; Goss, C.H. CFTR Modulator Use Is Associated with Higher Hemoglobin Levels in Individuals with Cystic Fibrosis. Ann. Am. Thorac. Soc. 2019, 16, 331–340. [Google Scholar] [CrossRef]
- Garlow, G.M.; Gettle, L.S.; Felicetti, N.J.; Polineni, D.; Gifford, A.H. Perspectives on Anemia and Iron Deficiency from the Cystic Fibrosis Care Community. Pediatr. Pulmonol. 2019, 54, 939–940. [Google Scholar] [CrossRef]
- Hoo, Z.H.; Wildman, M.J. Intravenous Iron among Cystic Fibrosis Patients. J. Cyst. Fibros. 2012, 11, 560–562. [Google Scholar] [CrossRef] [Green Version]
- Gifford, A.H.; Alexandru, D.M.; Li, Z.; Dorman, D.B.; Moulton, L.A.; Price, K.E.; Hampton, T.H.; Sogin, M.L.; Zuckerman, J.B.; Parker, H.W.; et al. Iron Supplementation Does Not Worsen Respiratory Health or Alter the Sputum Microbiome in Cystic Fibrosis. J. Cyst. Fibros. 2014, 13, 311–318. [Google Scholar] [CrossRef] [Green Version]
- Sharma, R.; Stanek, J.R.; Koch, T.L.; Grooms, L.; O’Brien, S.H. Intravenous Iron Therapy in Non-Anemic Iron-Deficient Menstruating Adolescent Females with Fatigue. Am. J. Hematol. 2016, 91, 973–977. [Google Scholar] [CrossRef] [PubMed]
- Jankowska, E.A.; Kirwan, B.-A.; Kosiborod, M.; Butler, J.; Anker, S.D.; McDonagh, T.; Dorobantu, M.; Drozdz, J.; Filippatos, G.; Keren, A.; et al. The Effect of Intravenous Ferric Carboxymaltose on Health-Related Quality of Life in Iron-Deficient Patients with Acute Heart Failure: The Results of the AFFIRM-AHF Study. Eur. Heart J. 2021, ehab234. [Google Scholar] [CrossRef] [PubMed]
- Turck, D.; Braegger, C.P.; Colombo, C.; Declercq, D.; Morton, A.; Pancheva, R.; Robberecht, E.; Stern, M.; Strandvik, B.; Wolfe, S.; et al. ESPEN-ESPGHAN-ECFS Guidelines on Nutrition Care for Infants, Children, and Adults with Cystic Fibrosis. Clin. Nutr. 2016, 35, 557–577. [Google Scholar] [CrossRef] [Green Version]



| Men (n = 87) | Women (n = 78) | p | |
|---|---|---|---|
| Age (years) | 30.2 ± 7.7 | 32.1 ± 10.1 | 0.37 |
| Genotype | |||
| p.PheF508del heterozygote (n, %) | 32 (36.8%) | 29 (37.2%) | 0.59 |
| p.PheF508del homozygote (n, %) | 45 (51.7%) | 36 (46.1%) | |
| other genotypes (n, %) | 10 (11.5%) | 13 (16.7%) | |
| BMI (kg·m−2) | 21.4 ± 2.5 | 20.3 ± 2.1 | 0.005 |
| Diabetes (n, %) | 8 (9.2%) | 19 (24.4%) | 0.009 |
| CF-related liver disease (n, %) | 6 (6.9%) | 11 (14.1%) | 0.12 |
| P. aeruginosa colonization (n, %) | 54/85 (63.5%) | 46/76 (60.5%) | 0.69 |
| Anaemia (n, %) | 2/80 (2.5%) | 7/67 (10.4%) | 0.08 |
| Ferritin (μg/L) | 87.4 ± 69.2 | 49.7 ± 64.8 | <0.001 |
| TSAT (%) | 22.8 ± 8.8 | 17.5 ± 6.1 | <0.001 |
| CRP (mg/L) | 5.8 ± 8.2 | 8 ± 14.3 | 0.78 |
| FEV1 (n, %) | n = 86 | n = 76 | |
| >79% | 50 (58.1%) | 32 (42.1%) | 0.05 |
| 50–79% | 17 (19.8%) | 27 (35.5%) | |
| 30–49% | 19 (22.1%) | 16 (21.1%) | |
| <30% | 0 | 1 (1.3%) |
| No-ID (n = 92) | ID (n = 73) | p | |
|---|---|---|---|
| Age (year) | 32.5 ± 9.1 | 29.4 ± 8.5 | 0.02 |
| Female gender (%) | 38% | 58.9% | 0.008 |
| BMI (kg/m2) | 21.3 ± 2.5 | 20.5 ± 2.2 | 0.05 |
| P. aeruginosa (%) | 55.1% | 70.8% | 0.04 |
| Diabetes mellitus (n) | 11 | 16 | 0.08 |
| CF-related liver disease (n) | 9 | 8 | 0.80 |
| Antiacid drugs/PPI (%) | 25% | 38.4% | 0.06 |
| CFTR corrector drugs (%) | 32.6% | 37% | 0.60 |
| FEV1 | |||
| <30% | 0 | 1 | 0.07 |
| 30–49% | 16 | 19 | |
| 50–79% | 35 | 33 | |
| ≥80% | 39 | 19 |
| n | Patients | ID Biological Definition | ID Prevalence | Exacerbation | |
|---|---|---|---|---|---|
| Gettle, 2020 [10] | 67 | A | ferritin < 12 μg/L and/or TSAT < 16% | 41.8% | PEx+ |
| Kałużna-Czyż, 2018 [24] | 46 | P | ferritin < 12 μg/L (<5 yo) ferritin < 15 μg/L (>5 yo) | 39% | PEx+ and PEx− |
| Yadav, 2014 [25] | 27 | P | SI < 4 μmol/L | 48.1% | PEx+ and PEx− |
| Gifford, 2012 [26] | 12 | A | SI < 12 μmol/L | 83% | PEx+ |
| Gifford, 2011 [27] | 39 | A | SI < 12 μmol/L | 76.9% | PEx+ and PEx− |
| von Drygalski, 2008 [8] | 26 | A + P | SI ≤ 40 μg/dL or TSAT ≤ 20% or ferritin ≤ 35 μg/L | 61% * 87.5% # | NA |
| Khalid, 2007 [16] | 127 | A | ferritin < 12 μg/L (women) and 20 μg/L (men) or SI < 12 μmol/L or TSAT ≤ 15% or sTfR < 1.74 mg/L | 18.9% (ferritin) 42.5% (TSAT)15% (sTfR) | PEx+ and PEx− |
| Reid, 2002 [6] | 30 | A | SI < 12 μmol/L or TSAT < 16% | 74% | PEx− |
| Jaffe, 2002 [28] | 144 | P | NA | 58% | NA |
| Keevil, 2000 [5] | 70 | A | ferritin < 12 μg/L (women) ferritin < 20 μg/L (men) SI < 12 μmol/L TSAT < 16% sTfR < 1.74 mg/L | 11% (ferritin) 69% (TSAT) 29% (sTfR) | NA |
| Pond, 1996 [29] | 71 | A | TSAT < 16% | 62% | NA |
| Zempsky, 1989 [30] | 13 | A | ferritin ≤ 25 μg/L | 38.4% | PEx− |
| Ehrhardt, 1987 [15] | 127 | A + P | ferritin < 12 μg/L | 32.3% | PEx+ and PEx− |
| Ater, 1983 [31] | 39 | A + P | ferritin < 12 μg/L SI < 40 μg/dL TSAT < 16% | 33% (ferritin) 25% (SI) 28% (TSAT) | PEx+ and Pex− |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lobbes, H.; Durupt, S.; Mainbourg, S.; Pereira, B.; Nove-Josserand, R.; Durieu, I.; Reynaud, Q. Iron Deficiency in Cystic Fibrosis: A Cross-Sectional Single-Centre Study in a Referral Adult Centre. Nutrients 2022, 14, 673. https://doi.org/10.3390/nu14030673
Lobbes H, Durupt S, Mainbourg S, Pereira B, Nove-Josserand R, Durieu I, Reynaud Q. Iron Deficiency in Cystic Fibrosis: A Cross-Sectional Single-Centre Study in a Referral Adult Centre. Nutrients. 2022; 14(3):673. https://doi.org/10.3390/nu14030673
Chicago/Turabian StyleLobbes, Hervé, Stéphane Durupt, Sabine Mainbourg, Bruno Pereira, Raphaele Nove-Josserand, Isabelle Durieu, and Quitterie Reynaud. 2022. "Iron Deficiency in Cystic Fibrosis: A Cross-Sectional Single-Centre Study in a Referral Adult Centre" Nutrients 14, no. 3: 673. https://doi.org/10.3390/nu14030673