Urinary Antibiotics and Dietary Determinants in Adults in Xinjiang, West China
Abstract
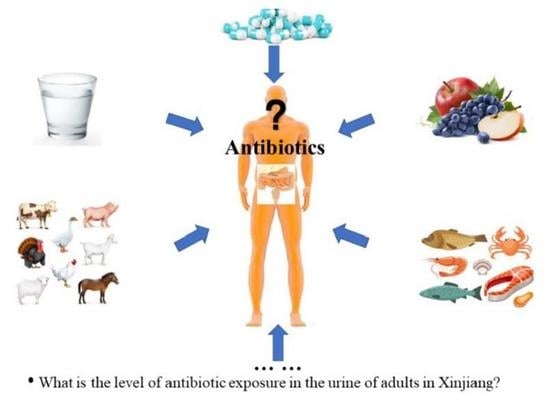
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Questionnaire and Medical Information Collection
2.3. Urine Collection and Analysis
2.4. Dietary Characteristics
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Browne, A.J.; Chipeta, M.G.; Haines-Woodhouse, G.; Kumaran, E.P.A.; Hamadani, B.H.K.; Zaraa, S.; Henry, N.J.; Deshpande, A.; Reiner, R.C.; Day, N.P.J.; et al. Global antibiotic consumption and usage in humans, 2000–18: A spatial modelling study. Lancet Planet. Health 2021, 5, e893–e904. [Google Scholar] [CrossRef]
- Huang, F.; An, Z.; Moran, M.J.; Liu, F. Recognition of typical antibiotic residues in environmental media related to groundwater in China (2009–2019). J. Hazard. Mater. 2020, 399, 122813. [Google Scholar] [CrossRef] [PubMed]
- Schar, D.; Klein, E.Y.; Laxminarayan, R.; Gilbert, M.; Van Boeckel, T.P. Global trends in antimicrobial use in aquaculture. Sci. Rep. 2020, 10, 21878. [Google Scholar] [CrossRef] [PubMed]
- Van Boeckel, T.P.; Brower, C.; Gilbert, M.; Grenfell, B.T.; Levin, S.A.; Robinson, T.P.; Teillant, A.; Laxminarayan, R. Global trends in antimicrobial use in food animals. Proc. Natl. Acad. Sci. USA 2015, 112, 5649–5654. [Google Scholar] [CrossRef] [Green Version]
- Wang, H.; Ren, L.; Yu, X.; Hu, J.; Chen, Y.; He, G.; Jiang, Q. Antibiotic residues in meat, milk and aquatic products in Shanghai and human exposure assessment. Food Control 2017, 80, 217–225. [Google Scholar] [CrossRef]
- Wang, H.; Yang, J.; Yu, X.; Zhao, G.; Zhao, Q.; Wang, N.; Jiang, Y.; Jiang, F.; He, G.; Chen, Y.; et al. Exposure of adults to antibiotics in a Shanghai Suburban Area and health risk assessment: A biomonitoring-based study. Environ. Sci. Technol. 2018, 52, 13942–13950. [Google Scholar] [CrossRef]
- Zeng, X.; Zhang, L.; Chen, Q.; Yu, K.; Zhao, S.; Zhang, L.; Zhang, J.; Zhang, W.; Huang, L. Maternal antibiotic concentrations in pregnant women in Shanghai and their determinants: A biomonitoring-based prospective study. Environ. Int. 2020, 138, 105638. [Google Scholar] [CrossRef]
- Zhou, Y.J.; Zhu, F.; Zheng, D.Y.; Gao, M.M.; Guo, B.F.; Zhang, N.; Meng, Y.; Wu, G.L.; Zhou, Y.L.; Huo, X. Detection of antibiotics in the urine of children and pregnant women in Jiangsu, China. Environ. Res. 2021, 196, 110945. [Google Scholar] [CrossRef]
- Luo, T.; Tian, T.; Liu, L.; Zhang, Z.; Sun, Q.; Sun, G.; Dai, J.; Yan, H. Cohort profile: The Xinjiang Multiethnic Cohort (XMC) study. BMJ Open 2022, 12, e048242. [Google Scholar]
- Xu, J.; Sangthong, R.; McNeil, E.; Tang, R.; Chongsuvivatwong, V. Antibiotic use in chicken farms in northwestern China. Antimicrob. Resist. Infect. Control 2020, 9, 10. [Google Scholar] [CrossRef] [Green Version]
- Zainab, S.M.; Junaid, M.; Xu, N.; Malik, R.N. Antibiotics and antibiotic resistant genes (ARGs) in groundwater: A global review on dissemination, sources, interactions, environmental and human health risks. Water Res. 2020, 187, 116455. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Tang, C.; Wang, Y.; Han, M.; Jiang, F.; Jiang, L.; Wu, J.; Fu, C.; Chen, Y.; Jiang, Q. Urinary antibiotic level of school children in Shanghai, East China, 2017-2020. Environ. Pollut. 2021, 291, 118167. [Google Scholar] [CrossRef] [PubMed]
- Fu, W.; Pei, H.; Shivappa, N.; Hebert, J.R.; Luo, T.; Tian, T.; Alimu, D.; Zhang, Z.; Dai, J. Association between dietary inflammatory index and type 2 diabetes mellitus in Xinjiang Uyghur autonomous region, China. PeerJ. 2021, 9, e11159. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Ho, K.W.K.; Ying, G.G.; Deng, W.J. Veterinary antibiotics in food, drinking water, and the urine of preschool children in Hong Kong. Environ. Int. 2017, 108, 246–252. [Google Scholar] [CrossRef]
- Liu, Y.; Wang, S.; Pan, J.; Zhu, F.; Wu, M.; Xu, G. Antibiotics in urine of the general population: Exposure, health risk assessment, and food factors. J. Environ. Sci. Health B 2021, 57, 1–12. [Google Scholar] [CrossRef]
- Taghizadeh-Behbahani, M.; Shamsipur, M.; Hemmateenejad, B. Detection and discrimination of antibiotics in food samples using a microfluidic paper-based optical tongue. Talanta 2022, 241, 123242. [Google Scholar] [CrossRef]
- Wang, H.; Tang, C.; Yang, J.; Wang, N.; Jiang, F.; Xia, Q.; He, G.; Chen, Y.; Jiang, Q. Predictors of urinary antibiotics in children of Shanghai and health risk assessment. Environ. Int. 2018, 121, 507–514. [Google Scholar] [CrossRef]
- Cui, Q.; Xia, Y.; Liu, Y.; Sun, Y.; Ye, K.; Li, W.; Wu, Q.; Chang, Q.; Zhao, Y. Validity and reproducibility of a FFQ for assessing dietary intake among residents of northeast China: Northeast cohort study of China. Br. J. Nutr. 2022, 1, 1–14. [Google Scholar] [CrossRef]
- McCullough, M.L.; Wang, Y.; Hartman, T.J.; Hodge, R.A.; Flanders, W.D.; Stevens, V.L.; Sampson, L.; Mitchell, D.C.; Patel, A.V. The Cancer Prevention Study-3 FFQ Is a Reliable and Valid Measure of Nutrient Intakes among Racial/Ethnic Subgroups, Compared with 24-Hour Recalls and Biomarkers. J. Nutr. 2021, 151, 636–648. [Google Scholar] [CrossRef]
- Zhu, A.; Chen, H.; Shen, J.; Wang, X.; Li, Z.; Zhao, A.; Shi, X.; Yan, L.; Zeng, Y.; Yuan, C.; et al. Interaction between plant-based dietary pattern and air pollution on cognitive function: A prospective cohort analysis of Chinese older adults. Lancet Reg. Health West. Pac. 2022, 20, 100372. [Google Scholar] [CrossRef]
- Sotos-Prieto, M.; Struijk, E.A.; Fung, T.T.; Rodríguez-Artalejo, F.; Willett, W.C.; Hu, F.B.; Lopez-Garcia, E. Association between the quality of plant-based diets and risk of frailty. J. Cachexia Sarcopenia Muscle 2022, 30, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Aljuraiban, G.S.; Gibson, R.; Al-Freeh, L.; Al-Musharaf, S.; Shivappa, N.; Hebert, J.R.; Oude Griep, L.M.; Chan, Q. Associations among plant-based dietary indexes, the dietary inflammatory index, and inflammatory potential in female college students in Saudi Arabia: A cross-sectional study. J. Acad. Nutr. Diet. 2022, 122, 771–785.e8. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Wang, B.; Zhao, Q.; Zhao, Y.; Fu, C.; Feng, X.; Wang, N.; Su, M.; Tang, C.; Jiang, F.; et al. Antibiotic body burden of Chinese school children: A multisite biomonitoring-based study. Environ. Sci. Technol. 2015, 49, 5070–5079. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Liu, K.; Zhang, J.; Liu, X.; Yang, L.; Wei, R.; Wang, S.; Zhang, D.; Xie, S.; Tao, F. Antibiotic body burden of elderly Chinese population and health risk assessment: A human biomonitoring-based study. Environ. Pollut. 2020, 256, 113311. [Google Scholar] [CrossRef]
- Ji, K.; Kho, Y.; Park, C.; Paek, D.; Ryu, P.; Paek, D.; Kim, M.; Kim, P.; Choi, K. Influence of water and food consumption on inadvertent antibiotics intake among general population. Environ. Res. 2010, 110, 641–649. [Google Scholar] [CrossRef]
- Liu, S.; Zhao, G.; Zhao, H.; Zhai, G.; Chen, J.; Zhao, H. Antibiotics in a general population: Relations with gender, body mass index (BMI) and age and their human health risks. Sci. Total Environ. 2017, 599–600, 298–304. [Google Scholar] [CrossRef]
- Wang, H.; Wang, N.; Wang, B.; Fang, H.; Fu, C.; Tang, C.; Jiang, F.; Zhou, Y.; He, G.; Zhao, Q.; et al. Antibiotics detected in urines and adipogenesis in school children. Environ. Int. 2016, 89–90, 204–211. [Google Scholar] [CrossRef]
- Han, Q.F.; Song, C.; Sun, X.; Zhao, S.; Wang, S.G. Spatiotemporal distribution, source apportionment and combined pollution of antibiotics in natural waters adjacent to mariculture areas in the Laizhou Bay, Bohai Sea. Chemosphere 2021, 279, 130381. [Google Scholar] [CrossRef]
- Li, D.; Yang, H.; Gong, Y.; Zhao, Y.; Qiu, L.; Sun, N.; Yin, X. Development and nationwide application of an antibiotic knowledge scale. Prev. Med. 2020, 141, 106262. [Google Scholar] [CrossRef]
- Ngaruka, G.B.; Neema, B.B.; Mitima, T.K.; Kishabongo, A.S.; Kashongwe, O.B. Animal source food eating habits of outpatients with antimi crobial resistance in Bukavu, D.R. Congo. Antimicrob. Resist. Infect. Control. 2021, 10, 124. [Google Scholar] [CrossRef]
- Heianza, Y.; Zheng, Y.; Ma, W.; Rimm, E.B.; Albert, C.M.; Hu, F.B.; Rexrode, K.M.; Manson, J.E.; Qi, L. Duration and life-stage of antibiotic use and risk of cardiovascular events in women. Eur. Heart J. 2019, 40, 3838–3845. [Google Scholar] [CrossRef] [PubMed]
- Al-Taie, A.; Hussein, A.N.; Albasry, Z. A Cross-Sectional Study of Patients’ Practices, Knowledge and Attitudes of Antibiotics among Iraqi Population. J. Infect Dev. Ctries. 2021, 15, 1845–1853. [Google Scholar] [CrossRef] [PubMed]
- Limbu, S.M.; Zhou, L.; Sun, S.X.; Zhang, M.L.; Du, Z.Y. Chronic exposure to low environmental concentrations and legal aquaculture doses of antibiotics cause systemic adverse effects in Nile tilapia and provoke differential human health risk. Environ. Int. 2018, 115, 205–219. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Wen, J.; Wu, M.; Li, J.Y.; Wang, Q.; Yin, J. In situ application of the diffusive gradients in thin film technique in aquaculture ponds for monitoring antibiotics, hormones, and herbicides. Environ. Sci. Pollut. Res. Int. 2022, 29, 21480–21490. [Google Scholar] [CrossRef] [PubMed]
- Guo, L.; Wu, X.; Liu, L.; Kuang, H.; Xu, C. Gold Immunochromatographic Assay for Rapid On-Site Detection of Lincosamide Residues in Milk, Egg, Beef, and Honey Samples. Biotechnol. J. 2020, 15, e1900174. [Google Scholar] [CrossRef]
- Peng, Z.; Hu, Z.; Li, Z.; Zhang, X.; Jia, C.; Li, T.; Dai, M.; Tan, C.; Xu, Z.; Wu, B.; et al. Antimicrobial resistance and population genomics of multidrug-resistant Escherichia coli in pig farms in mainland China. Nat. Commun. 2022, 13, 1116. [Google Scholar] [CrossRef]
- Patyra, E.; Kwiatek, K. HPLC-DAD analysis of florfenicol and thiamphenicol in medicated feedingstuffs. Food Addit. Contam. Part A Chem. Anal. Control Expo. Risk Assess. 2019, 36, 1184–1190. [Google Scholar] [CrossRef]
- Chen, Y.; Hu, C.; Deng, D.; Li, Y.; Luo, L. Factors affecting sorption behaviors of tetracycline to soils: Importance of soil organic carbon, pH and Cd contamination. Ecotoxicol. Environ. Saf. 2020, 197, 110572. [Google Scholar] [CrossRef] [PubMed]
- Cao, J.; Wang, Y.; Wang, G.; Ren, P.; Wu, Y.; He, Q. Effects of Typical Antimicrobials on Growth Performance, Morphology and Antimicro- bial Residues of Mung Bean Sprouts. Antibiotics 2022, 11, 807. [Google Scholar] [CrossRef]
- Zhang, X.H.; Tao, H.; Wang, Y.J.; Ma, Z.Y.; Zhou, Z.Y. Pollution Characteristics and Risk Assessment of Tetracycline Antibiotics in Farmland Soil in Yinchuan. Huan Jing Ke Xue 2021, 42, 4933–4941. [Google Scholar]
- Dekker, D.; Eibach, D.; Boahen, K.G.; Akenten, C.W.; Pfeifer, Y.; Zautner, A.E.; Mertens, E.; Krumkamp, R.; Jaeger, A.; Flieger, A.; et al. Fluoroquinolone-Resistant Salmonella enterica, Campylobacter spp., and Arcobacter butzleri from Local and Imported Poultry Meat in Kumasi, Ghana. Foodborne Pathog. Dis. 2019, 16, 352–358. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Payandeh, N.; Shahinfar, H.; Amini, M.; Jafari, A.; Safabakhsh, M.; Imani, H.; Shab-Bidar, S. The lack of association between plant-based dietary pattern and breast cancer: A hospital-based case-control study. Clin. Nutr. Res. 2021, 10, 115–126. [Google Scholar] [CrossRef] [PubMed]
- Makowska, N.; Bresa, K.; Koczura, R.; Philips, A.; Nowis, K.; Mokracka, J. Urban wastewater as a conduit for pathogenic Gram-positive bacteria and genes encoding resistance to β-lactams and glycopeptides. Sci. Total Environ. 2021, 765, 144176. [Google Scholar] [CrossRef] [PubMed]

| Antibiotic | Usage | N(%) a | Concentration (ng/mL) | |||||
|---|---|---|---|---|---|---|---|---|
| Percentiles | Maximum | |||||||
| 65th | 75th | 85th | 95th | 99th | ||||
| All antibiotics b | 435(49.8) | 0.5 | 1.8 | 8 | 220 | 21,000 | 80,000 | |
| HAs | 107(12.3) | — | — | — | 3.1 | 470 | 19,000 | |
| VAs | 90(10.3) | — | — | — | 2.2 | 95 | 36,000 | |
| PVAs | 354(40.5) | 0.3 | 0.8 | 3.8 | 51 | 12,000 | 80,000 | |
| Tetracyclines c | 128(14.7) | — | — | — | 17 | 6900 | 45,000 | |
| Chlortetracycline | VA | 5(0.6) | — | — | — | — | — | 120 |
| Tetracycline | PVA | 96(11) | — | — | — | 9 | 390 | 44,000 |
| Doxycycline | PVA | 6(0.7) | — | — | — | — | — | 11,000 |
| Oxytetracycline | VA | 54(6.2) | — | — | — | 1.5 | 72 | 36,000 |
| Fluoroquinolones c | 263(30.1) | — | 0.3 | 0.8 | 7.7 | 550 | 24,000 | |
| Enrofloxacin | VA | 12(1.4) | — | — | — | — | 0.2 | 9.4 |
| Norfloxacin | PVA | 92(10.7) | — | — | — | 1 | 51 | 24,000 |
| Ciprofloxacin | PVA | 53(6.1) | — | — | — | 0.6 | 6.9 | 930 |
| Ofloxacin | PVA | 168(19.2) | — | — | 0.2 | 1.6 | 34 | 2900 |
| Macrolides c | 61(7) | — | — | — | 2.1 | 470 | 19,000 | |
| Azithromycin | HA | 33(3.8) | — | — | — | — | 100 | 650 |
| Clarithromycin | HA | 4(0.5) | — | — | — | — | — | 4600 |
| Roxithromycin | HA | 29(3.3) | — | — | — | — | 82 | 19,000 |
| Sulfonamides c | 78(8.9) | — | — | — | 0.3 | 2.8 | 80,000 | |
| Sulfamethazine | PVA | 20(2.3) | — | — | — | — | 0.3 | 12 |
| Sulfadiazine | PVA | 1(0.1) | — | — | — | — | — | 11 |
| Sulfamethoxazole | PVA | 18(2.1) | — | — | — | — | 1.3 | 78,000 |
| Trimethoprim | PVA | 58(6.6) | — | — | — | 0.1 | 2.1 | 2000 |
| Phenicols c | 83(9.5) | — | — | — | 0.1 | 1.8 | 62 | |
| Chloramphenicol | HA | 51(5.8) | — | — | — | 0.04 | 0.7 | 60 |
| Florfenicol | VA | 33(3.8) | — | — | — | — | 0.6 | 62 |
| Thiamphenicol | PVA | 5(0.6) | — | — | — | — | — | 11 |
| Variable | Overall a,b | Antibiotic Concentration (ng/mL) c,d | Has a,b | Vas a,b | PVAs a,b |
|---|---|---|---|---|---|
| Sex | |||||
| Male | 210(49.2) | 250 | 54(12.6) | 45(10.5) | 170(39.8) |
| Female | 225(50.4) | 87 | 53(11.9) | 45(10.1) | 184(41.3) |
| Age (years) *^‡ | |||||
| 35–45 | 107(45.3) | 290 | 39(16.5) | 20(8.5) | 79(33.5) |
| 46–55 | 138(45.0) | 40 | 30(9.8) | 32(10.4) | 114(37.1) |
| 56–65 | 133(58.3) | 480 | 25(11.0) | 26(11.4) | 115(50.4) |
| 66–75 | 57(55.9) | 910 | 13(12.7) | 12(11.8) | 46(45.1) |
| Categories of BMI | |||||
| Normal weight | 235(52.2) | 290 | 53(11.8) | 51(11.3) | 189(42.0) |
| Obesity | 200(47.3) | 110 | 54(12.8) | 39(9.2) | 165(39.0) |
| Education *^‡ | |||||
| <Primary | 126(57.0) | 250 | 29(13.1) | 25(11.3) | 105(47.5) |
| Primary | 199(51.7) | 380 | 57(14.8) | 36(9.4) | 158(41.0) |
| Secondary | 87(41.8) | 66 | 16(7.7) | 24(11.5) | 72(34.6) |
| ≥High school | 23(39.0) | 180 | 5(8.5) | 5(8.5) | 19(32.2) |
| Monthly expenditure per capita (RMB) | |||||
| ≤240 | 117(53.7) | 500 | 27(12.4) | 22(10.1) | 95(43.6) |
| 240–333.33 | 82(49.7) | 180 | 17(10.3) | 20(12.1) | 70(42.4) |
| >333.33 | 230(48.0) | 150 | 61(12.7) | 46(9.6) | 186(38.8) |
| Variable | Overall a,b | Antibiotic Concentration (ng/mL) c,d | Has a,b | Vas a,b | PVAs a,b |
|---|---|---|---|---|---|
| Source of drinking water | |||||
| Tap water | 308(48.8) | 100 | 71(11.3) | 65(10.3) | 249(39.5) |
| Well and river water | 125(53.0) | 320 | 35(14.8) | 25(10.6) | 103(43.6) |
| Eggs and products † | |||||
| ≤1–3 times/month | 206(49.5) | 290 | 50(12.0) | 34(8.2) | 171(41.1) |
| ≥1–3 times/week | 221(50.3) | 93 | 54(12.3) | 54(12.3) | 176(40.1) |
| Cow and Goat Milk | |||||
| ≤1–3 times/month | 269(51.0) | 230 | 70(13.3) | 54(10.2) | 216(41.0) |
| ≥1–3 times/week | 153(48.1) | 120 | 32(10.1) | 33(10.4) | 129(40.6) |
| Pork *^ | |||||
| Not eaten | 367(50.8) | 240 | 91(12.6) | 72(10.0) | 299(41.4) |
| Occasionally eaten | 44(40.4) | 30 | 7(6.4) | 12(11.0) | 36(33.0) |
| Beef ‡ | |||||
| Not eat | 117(50.0) | 420 | 26(11.1) | 33(14.1) | 88(37.6) |
| Occasionally eaten | 233(48.3) | 110 | 67(13.9) | 41(8.5) | 190(39.4) |
| Eaten every day | 73(55.7) | 580 | 11(8.4) | 13(9.9) | 65(50.4) |
| Mutton | |||||
| Not eat | 84(50.3) | 620 | 21(12.6) | 20(12.0) | 72(43.1) |
| Occasionally eaten | 170(48.2) | 80 | 41(11.6) | 34(9.6) | 136(38.5) |
| Eaten every day | 170(51.7) | 280 | 42(12.8) | 34(10.3) | 137(41.6) |
| Seafood | |||||
| Not eaten | 254(50.6) | 490 | 65(12.9) | 51(10.2) | 206(41.0) |
| Occasionally eaten | 161(48.6) | 74 | 35(10.6) | 36(10.9) | 133(40.2) |
| Vegetables | |||||
| Not every day | 10(40.0) | 180 | 4(16.0) | 2(8.0) | 6(24.0) |
| Every day | 415(50.1) | 220 | 101(12.2) | 86(10.4) | 339(40.9) |
| Fruits ‡ | |||||
| Not every day | 313(50.8) | 180 | 75(12.2) | 57(9.3) | 262(42.5) |
| Every day | 115(47.5) | 270 | 31(12.8) | 31(12.8) | 85(35.1) |
| PDI *^ | |||||
| Q1 | 125(50.2) | 90 | 34(13.7) | 20(8.0) | 98(39.4) |
| Q2 | 98(49.5) | 2500 | 23(11.6) | 24(12.1) | 80(40.4) |
| Q3 | 143(56.3) | 290 | 37(14.6) | 29(11.4) | 118(46.5) |
| Q4 | 65(40.6) | 63 | 12(7.5) | 16(10.0) | 54(33.8) |
| uPDI | |||||
| Q1 | 134(48.6) | 470 | 35(12.7) | 30(10.9) | 104(37.7) |
| Q2 | 113(48.5) | 80 | 29(12.4) | 26(11.2) | 92(39.5) |
| Q3 | 88(52.4) | 450 | 22(13.1) | 19(11.3) | 71(42.3) |
| Q4 | 96(52.2) | 740 | 20(10.9) | 14(7.6) | 83(45.1) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chu, L.; Wang, H.; Su, D.; Zhang, H.; Yimingniyazi, B.; Aili, D.; Luo, T.; Zhang, Z.; Dai, J.; Jiang, Q. Urinary Antibiotics and Dietary Determinants in Adults in Xinjiang, West China. Nutrients 2022, 14, 4748. https://doi.org/10.3390/nu14224748
Chu L, Wang H, Su D, Zhang H, Yimingniyazi B, Aili D, Luo T, Zhang Z, Dai J, Jiang Q. Urinary Antibiotics and Dietary Determinants in Adults in Xinjiang, West China. Nutrients. 2022; 14(22):4748. https://doi.org/10.3390/nu14224748
Chicago/Turabian StyleChu, Lei, Hexing Wang, Deqi Su, Huanwen Zhang, Bahegu Yimingniyazi, Dilihumaer Aili, Tao Luo, Zewen Zhang, Jianghong Dai, and Qingwu Jiang. 2022. "Urinary Antibiotics and Dietary Determinants in Adults in Xinjiang, West China" Nutrients 14, no. 22: 4748. https://doi.org/10.3390/nu14224748