Use of the Baby-Led Weaning (BLW) Method in Complementary Feeding of the Infant—A Cross-Sectional Study of Mothers Using and Not Using the BLW Method
Abstract
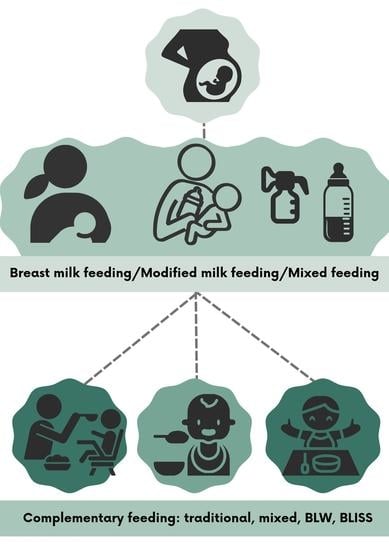
:1. Introduction
1.1. Strengths of BLW
1.2. Weaknesses of BLW
2. Materials and Methods
2.1. Study Group
Rationale for Selecting the Group
2.2. Inclusion and Exclusion Criteria
2.3. Research Tool
2.4. Statistical Analysis
3. Results
3.1. Characteristics of the Study Group
3.2. Use and Knowledge of BLW by the Surveyed Group of Mothers
3.3. Disadvantages of BLW and Their Importance among the Surveyed Group
4. Discussion
5. Conclusions
6. Study Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rapley, G.; Murkett, T. Bobas Lubi Wybór; Mamania: Warszawa, Poland, 2011. [Google Scholar]
- Utami, A.F.; Wanda, D.; Hayati, H.; Fowler, C. “Becoming an independent feeder”: Infant’s transition in solid food introduction through baby-led weaning. BMC Proc. 2020, 14, 18. [Google Scholar] [CrossRef] [PubMed]
- Jackowska, M. Baby-led weaning—Co wiadomo o tym podejściu do żywienia niemowląt? Przegląd literatury. Pol. J. Nutr. 2016, 4, 65–72. [Google Scholar]
- Erickson, L.W.; Taylor, R.W.; Haszard, J.J.; Fleming, E.A.; Daniels, L.; Morison, B.J.; Leong, C.; Fangupo, L.J.; Wheeler, B.J.; Taylor, B.J.; et al. Impact of a Modified Version of Baby-Led Weaning on Infant Food and Nutrient Intakes: The BLISS Randomized Controlled Trial. Nutrients 2018, 10, 740. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fewtrell, M.; Bronsky, J.; Campoy, C.; Domellöf, M.; Embleton, N.; Mis, N.F.; Hojsak, I.; Hulst, J.M.; Indrio, F.; Lapillonne, A.; et al. Complementary Feeding: A Position Paper by the European Society for Paediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN) Committee on Nutrition. J. Pediatr. Gastroenterol. Nutr. 2017, 64, 119–132. [Google Scholar] [CrossRef] [PubMed]
- Brown, A.; Lee, M. A descriptive study investigating the use and nature of baby-led weaning in a UK sample of mothers. Matern. Child Nutr. 2010, 7, 34–47. [Google Scholar] [CrossRef] [Green Version]
- Szajewska, H.; Socha, P.; Horvath, A. Zasady żywienia zdrowych niemowląt. Stanowisko Polskiego Towarzystwa Gastroenterologii, Hepatologii i Żywienia Dzieci. Stand. Med. 2021, T. 18, 805–822. [Google Scholar] [CrossRef]
- Brown, A.; Lee, M. Maternal Control of Child Feeding During the Weaning Period: Differences Between Mothers Following a Baby-led or Standard Weaning Approach. Matern. Child Health J. 2010, 15, 1265–1271. [Google Scholar] [CrossRef]
- Cameron, S.L.; Taylor, R.W.; Heath, A.-L.M. Development and pilot testing of Baby-Led Introduction to SolidS—A version of Baby-Led Weaning modified to address concerns about iron deficiency, growth faltering and choking. BMC Pediatr. 2015, 15, 99. [Google Scholar] [CrossRef] [Green Version]
- Brown, A. Differences in eating behaviour, well-being and personality between mothers following baby-led vs. traditional weaning styles. Matern. Child Nutr. 2015, 12, 826–837. [Google Scholar] [CrossRef]
- Brown, A.; Lee, M. An exploration of experiences of mothers following a baby-led weaning style: Developmental readiness for complementary foods. Matern. Child Nutr. 2011, 9, 233–243. [Google Scholar] [CrossRef] [Green Version]
- Rapley, G. Spoon-Feeding or Self-Feeding? The Infant’s First Experience of Solid Food. Ph.D. Thesis, Canterbury Christ Church University, Canterbury, UK, 2015. [Google Scholar]
- Brown, A.; Lee, M. Maternal child-feeding style during the weaning period: Association with infant weight and maternal eating style. Eat. Behav. 2011, 12, 108–111. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rowan, H.; Harris, C. Baby-led weaning and the family diet. A pilot study. Appetite 2012, 58, 1046–1049. [Google Scholar] [CrossRef] [PubMed]
- D’Auria, E.; Bergamini, M.; Staiano, A.; Banderali, G.; Pendezza, E.; Penagini, F.; Zuccotti, G.V.; Peroni, D.G.; Italian Society of Pediatrics. Baby-led weaning: What a systematic review of the literature adds on. Ital. J. Pediatr. 2018, 44, 49. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Toporowska-Kowalska, E.; Funkowicz, M. Kształtowanie preferencji smakowych we wczesnym okresie życia. Stand. Med. Pediatr. 2015, 12, 689–697. [Google Scholar]
- Harrison, M.; Brodribb, W.; Hepworth, J. A gualitative systematic review of maternal infant feeding practices in transitioning from milk feeds to family foods. Matern. Child Nutr. 2017, 13, e12360. [Google Scholar] [CrossRef] [PubMed]
- Cameron, S.L.; Heath, A.L.; Taylor, R.W. How Feasible Is Baby-Led Weaning as an Approach to Infant Feeding? A Review of the Evidence. Nutrients 2012, 4, 1575–1609. [Google Scholar] [CrossRef] [Green Version]
- Schwarzenberg, S.J.; Georgieff, M.K.; Daniels, S.; Corkins, M.; Golden, N.H.; Kim, J.H.; Lindsey, C.W.; Magge, S.N.; Committee on Nutrition. Advocacy for Improving Nutrition in the First 1000 Days to Support Childhood Development and Adult Health. Pediatrics 2018, 141, e20173716. [Google Scholar] [CrossRef] [Green Version]
- Baidal, J.A.W.; Locks, L.M.; Cheng, E.R.; Blake-Lamb, T.L.; Perkins, M.E.; Taveras, E.M. Risk Factors for Childhood Obesity in the First 1000 Days. Am. J. Prev. Med. 2016, 50, 761–779. [Google Scholar] [CrossRef]
- Coulthard, H.; Harris, G.; Emmett, P. Delayed introduction of lumpy foods to children during the complementary feeding period affects child’s food acceptance and feeding at 7 years of age. Matern. Child Nutr. 2009, 5, 75–85. [Google Scholar] [CrossRef]
- Nicklaus, S. Children’s acceptance of new foods at weaning. Role of practices of weaning and of food sensory properties. Appetite 2011, 57, 812–815. [Google Scholar] [CrossRef]
- Schwartz, C.; Scholtens, P.A.; Lalanne, A.; Weenen, H.; Nicklaus, S. Development of healthy eating habits early in life. Review of recent evidence and selected guidelines. Appetite 2011, 57, 796–807. [Google Scholar] [CrossRef] [PubMed]
- Committee on Injury, Violence, and Poison Prevention. Prevention of Choking Among Children. Pediatrics 2010, 125, 601–607. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fangupo, L.J.; Heath, A.L.M.; Williams, S.M.; Erickson Williams, L.W.; Morison, B.J.; Fleming, E.A.; Taylor, B.J.; Wheeler, B.J.; Taylor, R.W. A Baby-Led Approach to Eating Solids and Risk of Choking. Pediatrics 2016, 138, e20160772. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morison, B.J.; Taylor, R.W.; Haszard, J.J.; Schramm, C.J.; Williams Erickson, L.; Fangupo, L.J.; Fleming, E.A.; Luciano, A. Heath AL How different are baby-led weaning and conventional complementary feeding? A cross-sectional study of infants aged 6–8 months. BMJ Open 2016, 6, e010665. [Google Scholar] [CrossRef] [Green Version]
- OBWIESZCZENIE MARSZAŁKA SEJMU RZECZYPOSPOLITEJ POLSKIEJ z dnia 18 czerwca 2020 r. w Sprawie Ogłoszenia Jednolitego Tekstu Ustawy—Kodeks Pracy Warszawa, dnia 30 lipca 2020 r. Poz. 1320. Available online: https://www.pip.gov.pl/pl/f/v/224803/D2020000132001.pdf (accessed on 1 May 2022).
- Ministerstwo Rodziny i Polityki Społecznej. Urlopy dla Rodziców w 2019. Najnowsze dane. Available online: https://www.gov.pl/web/rodzina/urlopy-dla-rodzicow-w-2019-najnowsze-dane (accessed on 1 May 2022).
- Zakład Ubezpieczeń Społecznych. Ojcowie na Zasiłku Macierzyńskim. 23.06.2021 r. Available online: https://www.zus.pl/o-zus/aktualnosci/-/publisher/aktualnosc/0/ojcowie-na-zasilku-macierzynskim/4070408 (accessed on 1 May 2022).
- Zhang, S.; Li, T.; Xie, J.; Zhang, D.; Pi, C.; Zhou, L.; Yang, W. Gold standard for nutrition: A review of human milk oligosaccharide and its effects on infant gut microbiota. Microb. Cell Fact. 2021, 20, 108. [Google Scholar] [CrossRef]
- Walker, A. Breast Milk as the Gold Standard for Protective Nutrients. J. Pediatr. 2010, 156, S3–S7. [Google Scholar] [CrossRef]
- Zagórecka, E.; Motkowski, R.; Stolarczyk, A.; Socha, P.; Piotrowska-Jastrzębska, J.; Socha, J. Karmienie naturalne w żywieniu niemowląt z wybranych miast Polski Centralnej i Wschodniej. Pediatr. Polska 2007, 82, 538–549. [Google Scholar] [CrossRef]
- Ukasik, R.; Berek, A. Wiedza rodziców na temat żywienia dzieci w pierwszym roku życia. Probl. Pielęg. 2018, 26, 24–30. [Google Scholar]
- Fidler-Witoń, E.; Mikołajczak, K.; Waberska, M.; Miśkiewicz-Chotnicka, A.; Walkowiak, J. Żywienie niemowląt a aktualne rekomendacje. Now. Lek. 2010, 79, 356–361. [Google Scholar]
- Mikiel-Kostyra, K.; Mazur, J. Uwarunkowanie żywienia noworodków w szpitalnej opiece poporodowej. Część II: Czynniki warunkujące wyłączne karmienie piersią. Ginekol. Pol. 2000, 71, 604–610. [Google Scholar]
- Stolarczyk, A.; Zagórecka, E. Wartość odżywcza i sposób żywienia niemowląt w 6 i 12 miesiącu życia w Polsce. Pediatr. Wsp Gastroenterol. Hepatol. Zyw. Dziecka 2006, 8, 111–115. [Google Scholar]
- Gawęda, A.; Woś, H. Karmienie naturalne oraz czynniki warunkujące jego długość u dzieci z terenu Górnego Śląska. Nowa Pediatr. 2007, 1, 5–10. [Google Scholar]
- Official Journal Of The Republic Of Poland. Regulation Of The Council Of Ministers of March 30, 2021 in the National Health Program for the years 2021–2025; Official Journal Of The Republic Of Poland: Warsaw, Poland, 2021. [Google Scholar]
- Królak-Olejnik, B.; Szczygieł, A.; Asztabska, K. Dlaczego wskaźniki karmienia piersią w Polsce są aż tak niskie? Co i jak należałoby poprawić? Cz.1 Forum Pediatrii Prakt. 2018, 21, 56–61. [Google Scholar]
- Królak-Olejnik, B.; Błasiak, I.; Szczygieł, A. Promotion of breastfeeding in Poland: The current situation. J. Int. Med. Res. 2017, 45, 1976–1984. [Google Scholar] [CrossRef] [PubMed]
- Official Journal Of The Republic Of Poland. Ordinance of the Minister of Health of 16 August 2018 on the Organizational Standard of Perinatal Care; Official Journal Of The Republic Of Poland: Warsaw, Poland, 2018. [Google Scholar]
- Martí-Solsona, E.; González-Chordá, V.M.; Andreu-Pejo, L.; Cervera-Gasch, Á.; Valero-Chillerón, M.J.; Mena-Tudela, D. Parents’ Perception of the Complementary Baby-Led Weaning Feeding Method: A Validation Study. Nurs. Rep. 2020, 10, 115–123. [Google Scholar] [CrossRef] [PubMed]
- Rowan, H.; Lee, M.; Brown, A. Estimated energy and nutrient intake for infants following baby-led and traditional weaning approaches. J. Hum. Nutr. Diet. 2021, 35, 325–336. [Google Scholar] [CrossRef]
- Pearce, J.; Langley-Evans, S.C. Comparison of food and nutrient intake in infants aged 6–12 months, following baby-led or traditional weaning: A cross-sectional study. J. Hum. Nutr. Diet. 2021, 35, 310–324. [Google Scholar] [CrossRef]
- Quintiliano-Scarpelli, D.; Lehmann, N.; Castillo, B.; Blanco, E. Infant Feeding and Information Sources in Chilean Families Who Reported Baby-Led Weaning as a Complementary Feeding Method. Nutrients 2021, 13, 2707. [Google Scholar] [CrossRef]
- Neves, F.S.; Romano, B.M.; Campos, A.A.L.; Pavam, C.A.; Oliveira, R.M.S.; Cândido, A.P.C.; Netto, M.P. Brazilian health professionals’ perception about the Baby-Led Weaning (BLW) method for complementary feeding: An exploratory study. Rev. Paul. Pediatr. 2022, 40, e2020321. [Google Scholar] [CrossRef]
- Arias-Ramos, N.; Andina-Díaz, E.; Granado-Soto, M.; Rodríguez, R.; Liébana-Presa, C. Baby-led weaning: Health professionals ‘knowledge and attitudes and parents’ experiences from Spain. A mixed methods approach. Health Soc. Care Community 2022, 30, e1352–e1363. [Google Scholar] [CrossRef]
- Moore, A.P.; Milligan, P.; Goff, L.M. An online survey of knowledge of the weaning guidelines, advice from health visitors and other factors that influence weaning timing in UK mothers. Matern. Child Nutr. 2012, 10, 410–421. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Complementary Feeding of Young Children in Developing Countries: A Review of Current Scientific Knowledge; WHO: Geneva, Switzerland, 1998; Volume 98.1.
- Sociedade Brasileira de Pediatria. Guia Prático de Atualização: A Alimentação Complementar e o Método BLW (Baby Led Weaning); Sociedade Brasileira de Pediatria: Rio de Janeiro, Brasil, 2017. [Google Scholar]
- Daniels, L.; Heath, A.-L.M.; Williams, S.M.; Cameron, S.L.; Fleming, E.A.; Taylor, B.J.; Wheeler, B.J.; Gibson, R.S.; Taylor, R.W. Baby-Led Introduction to SolidS (BLISS) study: A randomised controlled trial of a baby-led approach to complementary feeding. BMC Pediatr. 2015, 15, 179. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Townsend, E.; Pitchford, N.J. Baby knows best? The impact of weaning style on food preferences and body mass index in early childhood in a case–controlled sample. BMJ Open 2012, 2, e000298. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cameron, S.L.; Taylor, R.W.; Heath, A.-L.M. Parent-led or baby-led? Associations between complementary feeding practices and health-related behaviours in a survey of New Zealand families. BMJ Open 2013, 3, e003946. [Google Scholar] [CrossRef] [Green Version]
- Brown, A. No difference in self-reported frequency of choking between infants introduced to solid foods using a baby-led weaning or traditional spoon-feeding approach. J. Hum. Nutr. Diet. 2017, 31, 496–504. [Google Scholar] [CrossRef]
- D’Andrea, E.; Jenkins, K.; Mathews, M.; Roebothan, B. Baby-led Weaning: A Preliminary Investigation. Can. J. Diet. Pract. Res. 2016, 77, 72–77. [Google Scholar] [CrossRef]
| n | % | |
|---|---|---|
| Age of mothers: | ||
| Under 19 years | 6 | 1.9% |
| 19–30 years | 169 | 52.8% |
| Over 30 years | 145 | 45.3% |
| Place of residence: | ||
| City | 253 | 79.1% |
| Village | 67 | 21.9% |
| Education: | ||
| Higher | 265 | 82.8% |
| Medium | 50 | 15.6% |
| Vocational | 3 | 0.9% |
| Basic | 2 | 0.6% |
| Professional activity: | ||
| Maternity/parental leave leave/sick | 214 | 66.9% |
| Leave/unemployment | ||
| White-collar work/studying | 94 | 29.4% |
| Physical labor | 12 | 4.7% |
| Childbearing: | ||
| 1 child in the family | 222 | 69.4% |
| 2 children in the family | 89 | 27.8% |
| 3 and more children in the family | 9 | 2.8% |
| Age of child: | ||
| 0–4 months | 19 | 5.9% |
| 5–6 months | 28 | 8.7% |
| 7–12 months | 114 | 35.6% |
| 12–24 months | 112 | 35.0% |
| 24–36 months | 47 | 14.7% |
| n | % | |
|---|---|---|
| Using BLW with your baby | ||
| Yes | 240 | 75.0% |
| No | 80 | 25.0% |
| Reasons for not using the BLW method | ||
| (n = 80; 25%): | ||
| The child does not cooperate | 30 | 37.5% |
| The child was not ready to start expanding the diet | 20 | 25.0% |
| The BLW method is inappropriate for expanding a young child’s diet | 15 | 18.75% |
| Lack of time to use BLW | 7 | 8.75% |
| Use of BLW not recommended by mum/grandma/friends/others | 5 | 6.25% |
| Mothers were concerned about the risk of their baby choking | 3 | 3.75% |
| Giving up Breastfeeding While Using BLW | ||||||
|---|---|---|---|---|---|---|
| Yes, It Is Necessary | It Is Not Necessary | Total | ||||
| n | % | n | % | n | % | |
| Uses BLW | 2 | 0.8% | 238 | 99.2% | 240 | 100% |
| Do not use BLW | 0 | 0.0% | 80 | 100% | 80 | 100% |
| Total | 2 | 0.6% | 318 | 99.4% | 320 | 100% |
| Starting to Expand the Diet | ||||||||
|---|---|---|---|---|---|---|---|---|
| 4 Months–6 Months | 6 Months | Above 6 Months of Age | Total | |||||
| n | % | n | % | n | % | n | % | |
| Uses BLW | 7 | 2.9% | 51 | 21.3% | 182 | 75.8% | 240 | 100% |
| Do not use BLW | 4 | 5.0% | 13 | 16.3% | 63 | 75.8% | 80 | 100% |
| Total | 11 | 3.4% | 64 | 20.0% | 245 | 76.6% | 320 | 100% |
| The Deciding Factor in Starting to Expand the BLW Diet | Uses BLW | Do Not Use BLW | Total | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Completed 4 months of age | 6 | 2.5% | 8 | 10.0% | 14 | 4.4% |
| Completed 6 months of age | 194 | 80.8% | 53 | 66.3% | 247 | 77.2% |
| Stable seating in chair/on lap | 205 | 85.4% | 65 | 81.3% | 270 | 84.4% |
| Sitting alone | 78 | 32.5% | 20 | 25.0% | 98 | 30.6% |
| Frequent awakenings during the night | 1 | 0.4% | 1 | 1.3% | 2 | 0.6% |
| Doctor’s opinion | 23 | 9.6% | 21 | 26.3% | 44 | 13.8% |
| Environment | 0 | 0.0% | 1 | 1.3% | 1 | 0.3% |
| Opinion of mother/grandmother/family | 3 | 1.3% | 2 | 2.5% | 5 | 1.6% |
| Total | 240 | 100% | 80 | 100% | 320 | 100% |
| The Most Significant Disadvantage | Significant Flaw | Neither a Disadvantage nor an Advantage | In My Opinion, This Is Not a Disadvantage | |||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| Risk of choking | 88 | 36.7% | 73 | 30.4% | 45 | 18.8% | 34 | 14.2% |
| Risk of nutritional deficiencies | 7 | 2.9% | 84 | 35.0% | 75 | 31.3% | 74 | 30.8% |
| Unfavorable reactions from professionals/environment | 3 | 1.3% | 14 | 5.8% | 75 | 21.3% | 148 | 61.7% |
| Mess when learning to eat on your own | 25 | 10.4% | 57 | 23.8% | 51 | 21.3% | 107 | 44.9% |
| Problematic determination of the portion eaten by the child | 8 | 3.3% | 57 | 23.8% | 58 | 24.2% | 117 | 48.8% |
| The child decides how much and whether to eat a meal | 6 | 2.5% | 15 | 6.3% | 40 | 16.7% | 179 | 74.6% |
| The child associates meals with a form of play | 6 | 2.5% | 15 | 6.3% | 75 | 21.3% | 144 | 60.0% |
| Need to devote more time | 7 | 2.9% | 35 | 14.6% | 65 | 27.1% | 133 | 55.4% |
| The Most Significant Disadvantage | Significant Flaw | Neither a Disadvantage nor an Advantage | In My Opinion, This Is Not a Disadvantage | |||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| Risk of choking | 45 | 56.3% | 23 | 28.8% | 7 | 8.8% | 5 | 6.3% |
| Risk of nutritional deficiencies | 6 | 7.5% | 35 | 43.8% | 21 | 26.3% | 18 | 22.5% |
| Unfavorable reactions from professionals/environment | 0 | 0.0% | 9 | 11.3% | 30 | 37.5% | 41 | 51.3% |
| Mess when learning to eat on your own | 7 | 8.8% | 22 | 27.5% | 19 | 23.8% | 32 | 40.0% |
| Problematic determination of the portion eaten by the child | 6 | 7.5% | 41 | 51.3% | 18 | 22.5% | 15 | 18.8% |
| The child decides how much and whether to eat a meal | 0 | 0.0% | 22 | 27.5% | 17 | 21.3% | 41 | 51.3% |
| The child associates meals with a form of play | 8 | 10.0% | 21 | 26.3% | 24 | 30.0% | 27 | 33.8% |
| Need to devote more time | 9 | 11.3% | 24 | 30.0% | 25 | 31.3% | 22 | 27.5% |
| The Most Important Aim of Expanding Your Diet with BLW | Uses BLW | Do Not Use BLW | Total | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Weaning from milk | 6 | 2.5% | 1 | 1.3% | 7 | 2.2% |
| Learning to eat on your own | 222 | 92.5% | 78 | 97.5% | 300 | 93.8% |
| Making everyday life easier | 33 | 13.8% | 14 | 17.5% | 47 | 14.7% |
| Improving the ability to chew, bite and swallow food | 220 | 91.7% | 63 | 78.8% | 283 | 88.4% |
| To inspire confidence in the child | 20 | 8.3% | 4 | 5.0% | 24 | 7.5% |
| Self-regulation of a child’s appetite | 168 | 70.0% | 55 | 68.8% | 223 | 69.7% |
| Total | 240 | 100% | 80 | 100% | 320 | 100% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Białek-Dratwa, A.; Soczewka, M.; Grajek, M.; Szczepańska, E.; Kowalski, O. Use of the Baby-Led Weaning (BLW) Method in Complementary Feeding of the Infant—A Cross-Sectional Study of Mothers Using and Not Using the BLW Method. Nutrients 2022, 14, 2372. https://doi.org/10.3390/nu14122372
Białek-Dratwa A, Soczewka M, Grajek M, Szczepańska E, Kowalski O. Use of the Baby-Led Weaning (BLW) Method in Complementary Feeding of the Infant—A Cross-Sectional Study of Mothers Using and Not Using the BLW Method. Nutrients. 2022; 14(12):2372. https://doi.org/10.3390/nu14122372
Chicago/Turabian StyleBiałek-Dratwa, Agnieszka, Monika Soczewka, Mateusz Grajek, Elżbieta Szczepańska, and Oskar Kowalski. 2022. "Use of the Baby-Led Weaning (BLW) Method in Complementary Feeding of the Infant—A Cross-Sectional Study of Mothers Using and Not Using the BLW Method" Nutrients 14, no. 12: 2372. https://doi.org/10.3390/nu14122372