Injectable Hyaluronan-Based Thermoresponsive Hydrogels for Dermatological Applications
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
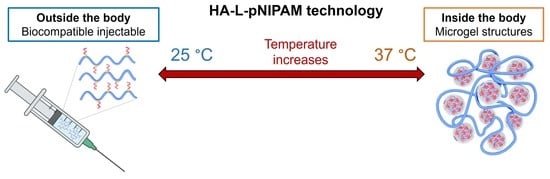
2.2. Synthesis of HA-L-pNIPAM Copolymers
2.3. Physical Characterization of HA-L-pNIPAM Hydrogels
2.3.1. Rheological Properties
2.3.2. Injectability
2.3.3. Accelerated Degradation Assays
2.4. Biological Evaluations of HA-L-pNIPAM Hydrogels
2.4.1. In Vitro Biocompatibility Evaluation Using a L929 Cell Line
2.4.2. Evaluation of Tissue Integration in Ex Vivo Porcine Skin Model
3. Results and Discussion
3.1. HA-L-pNIPAM Copolymer Synthesis
3.2. Physicochemical Characterization of HA-L-pNIPAM Hydrogels
3.2.1. Rheological Properties
3.2.2. Injectability
3.2.3. In Vitro Degradation
3.3. Biological Evaluation of HA-L-pNIPAM Hydrogels
3.3.1. In Vitro Biocompatibility on L929 Cell Line
3.3.2. Tissue Integration in the Ex Vivo Porcine Skin Model
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Zhao, P.; Zhao, W.; Zhang, K.; Lin, H.; Zhang, X. Polymeric injectable fillers for cosmetology: Current status, future trends, and regulatory perspectives. J. Appl. Polym. Sci. 2020, 137, 48515. [Google Scholar] [CrossRef] [Green Version]
- Akinbiyi, T.; Othman, S.; Familusi, O.; Calvert, C.; Card, E.B.; Percec, I. Better Results in Facial Rejuvenation with Fillers. Plast Reconstr. Surg. Glob. Open. 2020, 8, e2763. [Google Scholar] [CrossRef] [PubMed]
- Juhaščik, M.; Kováčik, A.; Huerta-Ángeles, G. Recent Advances of Hyaluronan for Skin Delivery: From Structure to Fabrication Strategies and Applications. Polymers 2022, 14, 4833. [Google Scholar] [CrossRef] [PubMed]
- Fallacara, A.; Durini, E.; Vertuani, S.; Manfredini, S. Hyaluronic Acid Fillers in Soft Tissue Regeneration. Facial Plast. Surg. 2017, 33, 87–96. [Google Scholar] [CrossRef] [PubMed]
- American Society of Plastic Surgeons. ASPS National Clearinghouse of Plastic Surgery Procedura. Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&ved=2ahUKEwjfp6vogrD_AhW_mlYBHYTLCvMQFnoECAkQAQ&url=https%3A%2F%2Fwww.plasticsurgery.org%2Fdocuments%2FNews%2FStatistics%2F2020%2Fplastic-surgery-statistics-full-report-2020.pdf&usg=AOvVaw3iGUn-TOl1_dRZIn0kGoFs (accessed on 1 June 2023).
- Stern, R.; Maibach, H.I. Hyaluronan in skin: Aspects of aging and its pharmacologic modulation. Clin. Dermatol. 2008, 26, 106–122. [Google Scholar] [CrossRef]
- Baumann, L. Skin ageing and its treatment. J. Pathol. 2007, 211, 241–251. [Google Scholar] [CrossRef]
- Weissmann, B.; Meyer, K. The Structure of Hyalobiuronic Acid and of Hyaluronic Acid from Umbilical Cord. J. Am. Chem. Soc. 1954, 76, 1753–1757. [Google Scholar] [CrossRef]
- Schanté, C.; Zuber, G.; Herlin, C.; Vandamme, T.F. Synthesis of N-alanyl-hyaluronamide with high degree of substitution for enhanced resistance to hyaluronidase-mediated digestion. Carbohydr. Polym. 2011, 86, 747–752. [Google Scholar] [CrossRef]
- Gupta, R.C.; Lall, R.; Srivastava, A.; Sinha, A. Hyaluronic Acid: Molecular Mechanisms and Therapeutic Trajectory. Front. Vet. Sci. 2019, 6, 192. [Google Scholar] [CrossRef] [Green Version]
- DelCarlo, M.; Loeser, R.F. Chondrocyte cell death mediated by reactive oxygen species-dependent activation of PKC-betaI. Am. J. Physiol.-Cell Physiol. 2006, 290, C802–C811. [Google Scholar] [CrossRef] [Green Version]
- Hawkins, C.L.; Davies, M.J. Direct detection and identification of radicals generated during the hydroxyl radical-induced degradation of hyaluronic acid and related materials. Free Radic. Biol. Med. 1996, 21, 275–290. [Google Scholar] [CrossRef]
- Fraser, J.R.E.; Laurent, T.C.; Laurent, U.B.G. Hyaluronan: Its nature, distribution, functions and turnover. J. Intern. Med. 1997, 242, 27–33. [Google Scholar] [CrossRef] [Green Version]
- Žádníková, P.; Šínová, R.; Pavlík, V.; Šimek, M.; Šafránková, B.; Hermannová, M.; Nešporová, K.; Velebný, V. The Degradation of Hyaluronan in the Skin. Biomolecules 2022, 12, 251. [Google Scholar] [CrossRef]
- Slevin, M.; Krupinski, J.; Kumar, S.; Gaffney, J. Angiogenic oligosaccharides of hyaluronan induce protein tyrosine kinase activity in endothelial cells and activate a cytoplasmic signal transduction pathway resulting in proliferation. Lab. Investig. 1998, 78, 987–1003. [Google Scholar]
- Hoarau, A.; Polette, M.; Coraux, C. Lung Hyaluronasome: Involvement of Low Molecular Weight Ha (Lmw-Ha) in Innate Immunity. Biomolecules 2022, 12, 658. [Google Scholar] [CrossRef]
- Lee, B.M.; Park, S.J.; Noh, I.; Kim, C.H. The effects of the molecular weights of hyaluronic acid on the immune responses. Biomater Res. 2021, 25, 27. [Google Scholar] [CrossRef]
- West, D.C.; Hampson, I.N.; Arnold, F.; Kumar, S. Angiogenesis induced by degradation products of hyaluronic acid. Science 1985, 228, 1324–1326. [Google Scholar] [CrossRef]
- Hu, L.; Nomura, S.; Sato, Y.; Takagi, K.; Ishii, T.; Honma, Y.; Watanabe, K.; Mizukami, Y.; Muto, J. Anti-inflammatory effects of differential molecular weight Hyaluronic acids on UVB-induced calprotectin-mediated keratinocyte inflammation. J. Dermatol. Sci. 2022, 107, 24–31. [Google Scholar] [CrossRef]
- Termeer, C.C.; Hennies, J.; Voith, U.; Ahrens, T.; Weiss, J.M.; Prehm, P.; Simon, J.C. Oligosaccharides of hyaluronan are potent activators of dendritic cells. J. Immunol. 2000, 165, 1863–1870. [Google Scholar] [CrossRef] [Green Version]
- Kim, J.; Kim, S.; Son, D.; Shin, M. Phenol-Hyaluronic Acid Conjugates: Correlation of Oxidative Crosslinking Pathway and Adhesiveness. Polymers 2021, 13, 3130. [Google Scholar] [CrossRef]
- Picotti, F.; Fabbian, M.; Gianni, R.; Sechi, A.; Stucchi, L.; Bosco, M. Hyaluronic acid lipoate: Synthesis and physicochemical properties. Carbohydr. Polym. 2013, 93, 273–278. [Google Scholar] [CrossRef] [PubMed]
- Shu, X.Z.; Liu, Y.; Palumbo, F.; Prestwich, G.D. Disulfide-crosslinked hyaluronan-gelatin hydrogel films: A covalent mimic of the extracellular matrix for in vitro cell growth. Biomaterials 2003, 24, 3825–3834. [Google Scholar] [CrossRef] [PubMed]
- Micheels, P.; Sarazin, D.; Tran, C.; Salomon, D. Effect of Different Crosslinking Technologies on Hyaluronic Acid Behavior: A Visual and Microscopic Study of Seven Hyaluronic Acid Gels. J. Drugs Dermatol. 2016, 15, 600–606. [Google Scholar] [PubMed]
- Fidalgo, J.; Deglesne, P.A.; Arroyo, R.; Sepúlveda, L.; Ranneva, E.; Deprez, P. Detection of a new reaction by-product in BDDE cross-linked autoclaved hyaluronic acid hydrogels by LC-MS analysis. Med. Devices Evid. Res. 2018, 11, 367–376. [Google Scholar] [CrossRef] [Green Version]
- Keizers, P.H.; Vanhee, C.; Elzen, E.M.V.D.; de Jong, W.H.; Venhuis, B.J.; Hodemaekers, H.M.; Schwillens, P.; Lensen, D.G. A high crosslinking grade of hyaluronic acid found in a dermal filler causing adverse effects. J. Pharm. Biomed. Anal. 2018, 159, 173–178. [Google Scholar] [CrossRef]
- Guarise, C.; Barbera, C.; Pavan, M.; Panfilo, S.; Beninatto, R.; Galesso, D. HA-based dermal filler: Downstream process comparison, impurity quantitation by validated HPLC-MS analysis, and in vivo residence time study. J. Appl. Biomater. Funct. Mater. 2019, 17, 2280800019867075. [Google Scholar] [CrossRef]
- Yeom, J.; Bhang, S.H.; Kim, B.-S.; Seo, M.S.; Hwang, E.J.; Cho, I.H.; Park, J.K.; Hahn, S.K. Effect of cross-linking reagents for hyaluronic acid hydrogel dermal fillers on tissue augmentation and regeneration. Bioconjug. Chem. 2010, 21, 240–247. [Google Scholar] [CrossRef]
- Shi, X.-H.; Zhou, X.; Zhang, Y.-M.; Lei, Z.-Y.; Liu, T.; Fan, D. Complications from Nasolabial Fold Injection of Calcium Hydroxylapatite for Facial Soft-Tissue Augmentation: A Systematic Review and Meta-Analysis. Aesthet. Surg. J. 2016, 36, 712–717. [Google Scholar] [CrossRef] [Green Version]
- Fino, P.; Toscani, M.; Grippaudo, F.R.; Giordan, N.; Scuderi, N. Randomized Double-Blind Controlled Study on the Safety and Efficacy of a Novel Injectable Cross-linked Hyaluronic Gel for the Correction of Moderate-to-Severe Nasolabial Wrinkles. Aesthet. Plast. Surg. 2019, 43, 470–479. [Google Scholar] [CrossRef]
- Stern, R.; Asari, A.A.; Sugahara, K.N. Hyaluronan fragments: An information-rich system. Eur. J. Cell Biol. 2006, 85, 699–715. [Google Scholar] [CrossRef]
- Enright, K.M.; Sampalis, J.; Nikolis, A. Evaluation of physician volumetric accuracy during hyaluronic acid gel injections: An observational, proof-of-concept study. J. Cosmet. Dermatol. 2020, 19, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Porcello, A.; Gonzalez-Fernandez, P.; Jeannerat, A.; Peneveyre, C.; Abdel-Sayed, P.; Scaletta, C.; Raffoul, W.; Hirt-Burri, N.; Applegate, L.A.; Allémann, E.; et al. Thermo-Responsive Hyaluronan-Based Hydrogels Combined with Allogeneic Cytotherapeutics for the Treatment of Osteoarthritis. Pharmaceutics 2023, 15, 1528. [Google Scholar] [CrossRef]
- Porcello, A.; Gonzalez-Fernandez, P.; Jordan, O.; Allémann, E. Nanoforming Hyaluronan-Based Thermoresponsive Hydrogels: Optimized and Tunable Functionality in Osteoarthritis Management. Pharmaceutics 2022, 14, 659. [Google Scholar] [CrossRef] [PubMed]
- Cooperstein, M.A.; Canavan, H.E. Assessment of cytotoxicity of (N-isopropyl acrylamide) and poly(N-isopropyl acrylamide)-coated surfaces. Biointerphases 2013, 8, 19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haq, M.A.; Su, Y.; Wang, D. Mechanical properties of PNIPAM based hydrogels: A review. Mater. Sci. Eng. C 2017, 70 Pt 1, 842–855. [Google Scholar] [CrossRef]
- Plunkett, K.N.; Zhu, X.; Moore, J.S.; Leckband, D.E. PNIPAM chain collapse depends on the molecular weight and grafting density. Langmuir 2006, 22, 4259–4266. [Google Scholar] [CrossRef]
- Sundaram, H.; Cassuto, D. Biophysical characteristics of hyaluronic acid soft-tissue fillers and their relevance to aesthetic applications. Plast. Reconstr. Surg. 2013, 132 (Suppl. 2), 5S–21S. [Google Scholar] [CrossRef]
- Crescenzi, V.; Francescangeli, A.; Taglienti, A.; Capitani, D.; Mannina, L. Synthesis and partial characterization of hydrogels obtained via glutaraldehyde crosslinking of acetylated chitosan and of hyaluronan derivatives. Biomacromolecules 2003, 4, 1045–1054. [Google Scholar] [CrossRef]
- Flynn, T.C.; Thompson, D.H.; Hyun, S.-H. Molecular Weight Analyses and Enzymatic Degradation Profiles of the Soft-Tissue Fillers Belotero Balance, Restylane, and Juvederm Ultra. Plast. Reconstr. Surg. 2013, 132, 22s–32s. [Google Scholar] [CrossRef]
- Molliard, S.G.; Bétemps, J.B.; Hadjab, B.; Topchian, D.; Micheels, P.; Salomon, D. Key rheological properties of hyaluronic acid fillers: From tissue integration to product degradation. Plast. Aesthetic Res. 2018, 5, 17. [Google Scholar] [CrossRef] [Green Version]
- Li, W.; Zhou, J.; Xu, Y. Study of the in vitro cytotoxicity testing of medical devices. Biomed. Rep. 2015, 3, 617–620. [Google Scholar] [CrossRef] [Green Version]
- Lebonvallet, N.; Jeanmaire, C.; Danoux, L.; Sibille, P.; Pauly, G.; Misery, L. The evolution and use of skin explants: Potential and limitations for dermatological research. Eur. J. Dermatol. 2010, 20, 671–684. [Google Scholar]
- Neil, J.E.; Brown, M.B.; Williams, A.C. Human skin explant model for the investigation of topical therapeutics. Sci. Rep. 2020, 10, 21192. [Google Scholar] [CrossRef]
- Tran, C.; Carraux, P.; Micheels, P.; Kaya, G.; Salomon, D. In vivo bio-integration of three hyaluronic acid fillers in human skin: A histological study. Dermatology 2014, 228, 47–54. [Google Scholar] [CrossRef]
- Dugaret, A.S.; Bertino, B.; Gauthier, B.; Gamboa, B.; Motte, M.; Rival, Y.; Piwnica, D.; Osman-Ponchet, H.; Bourdès, V.; Voegel, J.J. An innovative method to quantitate tissue integration of hyaluronic acid-based dermal fillers. Ski. Res. Technol. 2018, 24, 423–431. [Google Scholar] [CrossRef]
- Flynn, T.C.; Sarazin, D.; Bezzola, A.; Terrani, C.; Micheels, P. Comparative histology of intradermal implantation of mono and biphasic hyaluronic acid fillers. Dermatol. Surg. 2011, 37, 637–643. [Google Scholar] [CrossRef]
- Choi, M.-S.; Kwak, S.; Kim, J.; Park, M.-S.; Ko, S.M.; Kim, T.; Jeong, D.S.; Rhee, C.-H.; Yang, G.-H.; Son, W.-C.; et al. Comparative Analyses of Inflammatory Response and Tissue Integration of 14 Hyaluronic Acid-Based Fillers in Mini Pigs. Clin. Cosmet. Investig. Dermatol. 2021, 14, 765–778. [Google Scholar] [CrossRef]
- Santer, V.; Molliard, S.G.; Micheels, P.; del Río-Sancho, S.; Quinodoz, P.; Kalia, Y.N.; Salomon, D. Hyaluronic Acid After Subcutaneous Injection-An Objective Assessment. Dermatol. Surg. 2019, 45, 108–116. [Google Scholar] [CrossRef]






| Formulation | Copolymer | Formulation Concentration (mg/mL) | HA Content (mg/mL) |
|---|---|---|---|
| Candidate 1 | HA-L-pNIPAM0.10 | 20 | 15 |
| Candidate 2 | HA-L-pNIPAM0.25 | 20 | 8 |
| Candidate 3 | HA-L-pNIPAM0.50 + HA (1.5–1.75 MDa) | 20 | 9.5 |
| Formulation | HA Content (mg/mL) | Temperature (°C) | G′ | G″ | Tan δ = |
|---|---|---|---|---|---|
| Belotero Balance® | 22.5 | 37 | 53 | 33 | 0.62 |
| Belotero Volume® | 26.0 | 37 | 233 | 54 | 0.23 |
| Candidate 1 | 15.0 | 22 | 105.1 | 50.1 | 0.48 |
| 37 | 234.1 | 28.7 | 0.13 | ||
| Candidate 2 | 8.0 | 22 | 167.8 | 83.8 | 0.50 |
| 37 | 420.2 | 34.9 | 0.08 | ||
| Candidate 3 | 9.5 | 22 | 66.9 | 35.3 | 0.50 |
| 37 | 92.5 | 43.5 | 0.49 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gou, S.; Porcello, A.; Allémann, E.; Salomon, D.; Micheels, P.; Jordan, O.; Kalia, Y.N. Injectable Hyaluronan-Based Thermoresponsive Hydrogels for Dermatological Applications. Pharmaceutics 2023, 15, 1708. https://doi.org/10.3390/pharmaceutics15061708
Gou S, Porcello A, Allémann E, Salomon D, Micheels P, Jordan O, Kalia YN. Injectable Hyaluronan-Based Thermoresponsive Hydrogels for Dermatological Applications. Pharmaceutics. 2023; 15(6):1708. https://doi.org/10.3390/pharmaceutics15061708
Chicago/Turabian StyleGou, Si, Alexandre Porcello, Eric Allémann, Denis Salomon, Patrick Micheels, Olivier Jordan, and Yogeshvar N. Kalia. 2023. "Injectable Hyaluronan-Based Thermoresponsive Hydrogels for Dermatological Applications" Pharmaceutics 15, no. 6: 1708. https://doi.org/10.3390/pharmaceutics15061708