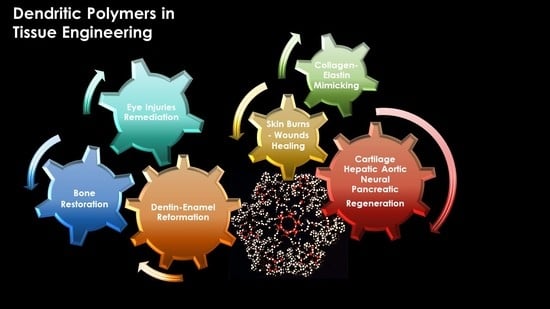
Dendritic Polymers in Tissue Engineering: Contributions of PAMAM, PPI PEG and PEI to Injury Restoration and Bioactive Scaffold Evolution
Abstract
:1. Introduction
2. Peptide Functionalized Dendritic Polymers Mimicking Collagen and Elastin
2.1. Collagen
2.2. Elastin
3. Dendritic Polymers Mediating to Cell Adhesion, Proliferation, and Differentiation
3.1. Scaffolds from Collagen and Beyond

3.2. Hydrogel Matrices
3.3. Dendritic Glues for Cell Aggregation
4. Bone Restoration
4.1. Hydroxy Apatite Nucleation and Functionalization


4.2. Osseointegration
4.2.1. Adhesion and Proliferation of Osteoblasts and Other Cells Related to Bone Development

4.2.2. Cell Differentiation


4.3. Bone Formation
5. Applications of Dendritic Polymers in Dentistry
5.1. Interactions with Odontoblasts and Dental Pulp Cells
5.2. Dentin Reconstitution




5.3. Enamel


6. Treatment of Eye Related Conditions
6.1. Remediation of Cornea Incisions and Injuries

6.2. Corneal Tissue (re)Creation
7. Skin
7.1. Wound Treatment by Hydrogels
7.2. Dendritic Polymers as Cell Nanocarriers to the Skin
7.3. Scaffolds for Skin Tissue Regeneration
8. Articular Cartilage Tissue Reparation
9. Hepatic Aortic Neural and Pancreatic Tissue Engineering


| Dendritic Polymer | Modification | Substrate | Function | Ref. |
|---|---|---|---|---|
| PAMAM G4 | Bovine collagen type I | Poly(lactide-co-glycolide) Microspheres | Chondrocytes Proliferation- Articular Cartilage Tissue Regeneration | [288] |
| PEG core methacrylated poly(glycerol succinic acid) | PEG core photo–cross-linking | Hydrogel | Chondrocytes Proliferation- Cartilage Tissue Regeneration | [284] |
| PEG core poly(glycerol succinic acid), poly(glycerol beta-alanine) | Methacrylate ester photo–cross-linking | - | Osteochondral defects repair | [285] |
| G4 Dendrigraft polylysines | - | Poly(glycolic acid) fibrous scaffolds | Hippocampal neurons (nerve cells) | [290] |
| G4 PAMAM | PEG | Kartogenin | Chondrogenic differentiation of mesenchymal stem cells | [286] |
| Thiol-terminated dendron | Maleimide end-capped PEG crosslinker | Hydrogel sealant | Hepatic and aortic trauma | [291] |
| G4 PAMAM | Filter paper functionalized with glutaraldehyde | Liver HepG2 cells | [294] | |
| G5 PAMAM | Neuroligin-2-derived peptide | Pancreatic β-cells’ proliferation | [292] | |
| Hyperbranched polyester | Polypyrrole end groups polycaprolactone | Nanofiber Scaffold | HepG2 cells Liver | [289] |
| Poly ε-lysine dendrimers | Ile-lys-val-ala-val | Pre-crosslinked collagen | Rat Schwann cells proliferation, human dermal fibroblasts inhibition, selective neural cell response | [293] |
| PAMAM | Methacrylic anhydride | Gelatin methacrylate hydrogel | Cartilage defect repair, in vivo cartilage defect repair | [287] |
10. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Caminade, A.M.; Turrin, C.O.; Laurent, R.; Ouali, A.; Delavaux-Nicot, B. (Eds.) Dendrimers: Towards Catalytic, Material, and Biomedical Uses; John Wiley & Sons: Hoboken, NJ, USA, 2011. [Google Scholar]
- Buhleier, E.; Wehner, W.; Vögtle, F. “Cascade”- and “Nonskid-Chain-like” Syntheses of Molecular Cavity Topologies. Synthesis 1978, 1978, 155–158. [Google Scholar] [CrossRef]
- De Gennes, P.G.; Hervet, H. Statistics of «starburst» polymers. J. Phys. Lett. 1983, 44, 351–360. [Google Scholar] [CrossRef]
- Tomalia, D.A.; Frechet, J.M.J. Discovery of dendrimers and dendritic polymers: A brief historical perspective. J. Polym. Sci. Part A Polym. Chem. 2002, 40, 2719–2728. [Google Scholar] [CrossRef]
- Newkome, G.R.; Moorefield, C.N.; Vögtle, F. Dendritic Molecules: Concepts, Syntheses, Perspectives; John Wiley & Sons: Hoboken, NJ, USA, 2008. [Google Scholar]
- Voit, B.I. Dendritic polymers: From aesthetic macromolecules to commercially interesting materials. Acta Polym. 1995, 46, 87–99. [Google Scholar] [CrossRef]
- Vögtle, F. Functional dendrimers. Prog. Polym. Sci. 2000, 25, 987–1041. [Google Scholar] [CrossRef]
- Ardoin, N.; Astruc, D. Molecular trees: From syntheses towards applications. Bull. Société Chim. Fr. 1995, 9, 875–909. [Google Scholar]
- Bosman, A.W.; Janssen, H.M.; Meijer, E.W. About Dendrimers: Structure, Physical Properties, and Applications. Chem. Rev. 1999, 99, 1665–1688. [Google Scholar] [CrossRef]
- Dvornic, P.R.; Tomalia, D.A. November. Starburst® dendrimers: A conceptual approach to nanoscopic chemistry and architecture. Macromol. Symp. 1994, 88, 123–148. [Google Scholar] [CrossRef]
- Tully, D.C.; Fréchet, J.M.J. Dendrimers at surfaces and interfaces: Chemistry and applications. Chem. Commun. 2001, 1229–1239. [Google Scholar] [CrossRef]
- Zeng, F.; Zimmerman, S.C. Dendrimers in Supramolecular Chemistry: From Molecular Recognition to Self-Assembly. Chem. Rev. 1997, 97, 1681–1712. [Google Scholar] [CrossRef]
- Kaur, D.; Jain, K.; Mehra, N.K.; Kesharwani, P.; Jain, N.K. A review on comparative study of PPI and PAMAM dendrimers. J. Nanopart. Res. 2016, 18, 146. [Google Scholar] [CrossRef]
- Jikei, M.; Kakimoto, M.-A. Hyperbranched polymers: A promising new class of materials. Prog. Polym. Sci. 2001, 26, 1233–1285. [Google Scholar] [CrossRef]
- Kim, Y.H. Hyperbranched polymers 10 years after. J. Polym. Sci. Part A Polym. Chem. 1998, 36, 1685–1698. [Google Scholar] [CrossRef]
- Malmström, E.; Hult, A. Hyperbranched Polymers. J. Macromol. Sci. Part C Polym. Rev. 1997, 37, 555–579. [Google Scholar] [CrossRef]
- Sunder, A.; Heinemann, J.; Frey, H. Controlling the growth of polymer trees: Concepts and perspectives for hyper-branched polymers. Chem. Eur. J. 2000, 6, 2499–2506. [Google Scholar] [CrossRef]
- Voit, B.I. Hyperbranched polymers: A chance and a challenge. Comptes Rendus Chim. 2003, 6, 821–832. [Google Scholar] [CrossRef]
- Yates, C.; Hayes, W. Synthesis and applications of hyperbranched polymers. Eur. Polym. J. 2004, 40, 1257–1281. [Google Scholar] [CrossRef]
- Zheng, Y.; Li, S.; Weng, Z.; Gao, C. Hyperbranched polymers: Advances from synthesis to applications. Chem. Soc. Rev. 2015, 44, 4091–4130. [Google Scholar] [CrossRef]
- Belgaonkar, M.S.; Kandasubramanian, B. Hyperbranched Polymer-based Nanocomposites: Synthesis, Progress, and Applications. Eur. Polym. J. 2021, 147, 110301. [Google Scholar] [CrossRef]
- Grayson, S.M.; Fréchet, J.M.J. Convergent Dendrons and Dendrimers: From Synthesis to Applications. Chem. Rev. 2001, 101, 3819–3868. [Google Scholar] [CrossRef]
- Rosen, B.M.; Wilson, C.J.; Wilson, D.A.; Peterca, M.; Imam, M.R.; Percec, V. Dendron-Mediated Self-Assembly, Disassembly, and Self-Organization of Complex Systems. Chem. Rev. 2009, 109, 6275–6540. [Google Scholar] [CrossRef] [PubMed]
- Teertstra, S.J.; Gauthier, M. Dendrigraft polymers: Macromolecular engineering on a mesoscopic scale. Prog. Polym. Sci. 2004, 29, 277–327. [Google Scholar] [CrossRef]
- Okrugin, B.; Ilyash, M.; Markelov, D.; Neelov, I. Lysine Dendrigraft Nanocontainers. Influence of Topology on Their Size and Internal Structure. Pharmaceutics 2018, 10, 129. [Google Scholar] [CrossRef]
- Afang, Z. Synthesis, characterization and applications of dendronized polymers. Prog. Chem. 2005, 17, 157–171. [Google Scholar] [CrossRef]
- Chen, Y.; Xiong, X. Tailoring dendronized polymers. Chem. Commun. 2010, 46, 5049–5060. [Google Scholar] [CrossRef] [PubMed]
- Frauenrath, H. Dendronized polymers—Building a new bridge from molecules to nanoscopic objects. Prog. Polym. Sci. 2005, 30, 325–384. [Google Scholar] [CrossRef]
- Schlüter, A.D.; Rabe, J.P. Dendronized polymers: Synthesis, characterization, assembly at interfaces, and manipulation. Angew. Chem. Int. Ed. 2000, 39, 864–883. [Google Scholar] [CrossRef]
- Liu, X.; Lin, W.; Astruc, D.; Gu, H. Syntheses and applications of dendronized polymers. Prog. Polym. Sci. 2019, 96, 43–105. [Google Scholar] [CrossRef]
- Douloudi, M.; Nikoli, E.; Katsika, T.; Vardavoulias, M.; Arkas, M. Dendritic Polymers as Promising Additives for the Manufacturing of Hybrid Organoceramic Nanocomposites with Ameliorated Properties Suitable for an Extensive Diversity of Applications. Nanomaterials 2020, 11, 19. [Google Scholar] [CrossRef]
- Arkas, M.; Kitsou, I.; Gkouma, A.; Papageorgiou, M. The role of hydrogen bonds in the mesomorphic behaviour of supramolecular assemblies organized in dendritic architectures. Liq. Cryst. Rev. 2019, 7, 60–105. [Google Scholar] [CrossRef]
- Astruc, D.; Boisselier, E.; Ornelas, C. Dendrimers Designed for Functions: From Physical, Photophysical, and Supramolecular Properties to Applications in Sensing, Catalysis, Molecular Electronics, Photonics, and Nanomedicine. Chem. Rev. 2010, 110, 1857–1959. [Google Scholar] [CrossRef]
- Astruc, D.; Chardac, F. Dendritic Catalysts and Dendrimers in Catalysis. Chem. Rev. 2001, 101, 2991–3024. [Google Scholar] [CrossRef]
- Wang, D.; Astruc, D. Dendritic catalysis—Basic concepts and recent trends. Coord. Chem. Rev. 2013, 257, 2317–2334. [Google Scholar] [CrossRef]
- Arkas, M.; Anastopoulos, I.; Giannakoudakis, D.A.; Pashalidis, I.; Katsika, T.; Nikoli, E.; Panagiotopoulos, R.; Fotopoulou, A.; Vardavoulias, M.; Douloudi, M. Catalytic Neutralization of Water Pollutants Mediated by Dendritic Polymers. Nanomaterials 2022, 12, 445. [Google Scholar] [CrossRef]
- Arkas, M.; Douloudi, M.; Nikoli, E.; Karountzou, G.; Kitsou, I.; Kavetsou, E.; Korres, D.; Vouyiouka, S.; Tsetsekou, A.; Giannakopoulos, K.; et al. Investigation of two bioinspired reaction mechanisms for the optimization of nano catalysts generated from hyperbranched polymer matrices. React. Funct. Polym. 2022, 174, 105238. [Google Scholar] [CrossRef]
- Kitsou, I.; Arkas, M.; Tsetsekou, A. Synthesis and characterization of ceria-coated silica nanospheres: Their application in heterogeneous catalysis of organic pollutants. SN Appl. Sci. 2019, 1, 1557. [Google Scholar] [CrossRef]
- Marcos, M.; Martín-Rapún, R.; Omenat, A.; Serrano, J.L. Highly congested liquid crystal structures: Dendrimers, dendrons, dendronized and hyperbranched polymers. Chem. Soc. Rev. 2007, 36, 1889–1901. [Google Scholar] [CrossRef] [PubMed]
- Saez, I.M.; Goodby, J.W. Supermolecular liquid crystals. J. Mater. Chem. 2005, 15, 26–40. [Google Scholar] [CrossRef]
- Percec, V. Bioinspired supramolecular liquid crystals. Philos. Trans. R. Soc. A Math. Phys. Eng. Sci. 2006, 364, 2709–2719. [Google Scholar] [CrossRef]
- Tsiourvas, D.; Arkas, M. Columnar and smectic self-assembly deriving from non ionic amphiphilic hyperbranched polyethylene imine polymers and induced by hydrogen bonding and segregation into polar and non polar parts. Polymer 2013, 54, 1114–1122. [Google Scholar] [CrossRef]
- Savage, N.; Diallo, M.S. Nanomaterials and Water Purification: Opportunities and Challenges. J. Nanopart. Res. 2005, 7, 331–342. [Google Scholar] [CrossRef]
- Arkas, M.; Tsiourvas, D.; Paleos, C.M. Functional Dendritic Polymers for the Development of Hybrid Materials for Water Purification. Macromol. Mater. Eng. 2010, 295, 883–898. [Google Scholar] [CrossRef]
- Tsetsekou, A.; Arkas, M.; Kritikaki, A.; Simonetis, S.; Tsiourvas, D. Optimization of hybrid hyperbranched polymer/ceramic filters for the efficient absorption of polyaromatic hydrocarbons from water. J. Membr. Sci. 2007, 311, 128–135. [Google Scholar] [CrossRef]
- Arkas, M.; Eleades, L.; Paleos, C.M.; Tsiourvas, D. Alkylated hyperbranched polymers as molecular nanosponges for the purification of water from polycyclic aromatic hydrocarbons. J. Appl. Polym. Sci. 2005, 97, 2299–2305. [Google Scholar] [CrossRef]
- Adronov, A.; Fréchet, J.M.J. Light-harvesting dendrimers. Chem. Commun. 2000, 1701–1710. [Google Scholar] [CrossRef]
- Nantalaksakul, A.; Reddy, D.R.; Bardeen, C.J.; Thayumanavan, S. Light Harvesting Dendrimers. Photosynth. Res. 2006, 87, 133–150. [Google Scholar] [CrossRef]
- Akbari, S.; Kozłowski, R.M. A review of application of amine-terminated dendritic materials in textile engineering. J. Text. Inst. 2019, 110, 460–467. [Google Scholar] [CrossRef]
- Atav, R. Dendritic molecules and their use in water repellency treatments of textile materials. In Water-Proof and Water Repellent Textiles and Clothing; Woodhead Publishing: Sawston, UK, 2018; pp. 191–214. [Google Scholar] [CrossRef]
- Arkas, M.; Kythreoti, G.; Favvas, E.P.; Giannakopoulos, K.; Mouti, N.; Arvanitopoulou, M.; Athanasiou, A.; Douloudi, M.; Nikoli, E.; Vardavoulias, M.; et al. Hydrophilic Antimicrobial Coatings for Medical Leathers from Silica-Dendritic Polymer-Silver Nanoparticle Composite Xerogels. Textiles 2022, 2, 464–485. [Google Scholar] [CrossRef]
- Wei, Q.; Achazi, K.; Liebe, H.; Schulz, A.; Noeske, P.-L.M.; Grunwald, I.; Haag, R. Mussel-Inspired Dendritic Polymers as Universal Multifunctional Coatings. Angew. Chem. Int. Ed. 2014, 53, 11650–11655. [Google Scholar] [CrossRef]
- Gurunathan, T.; Mohanty, S.; Nayak, S.K. Hyperbranched Polymers for Coating Applications: A Review. Polym. Technol. Eng. 2016, 55, 92–117. [Google Scholar] [CrossRef]
- Zhang, X.; Chen, T.-H.; Chen, F.-F.; Wu, H.; Yu, C.-Y.; Liu, L.-F.; Gao, C.-J. Structure adjustment for enhancing the water permeability and separation selectivity of the thin film composite nanofiltration membrane based on a dendritic hyperbranched polymer. J. Membr. Sci. 2021, 618, 118455. [Google Scholar] [CrossRef]
- Haag, R.; Sunder, A.; Hebel, A.; Roller, S. Dendritic Aliphatic Polyethers as High-Loading Soluble Supports for Carbonyl Compounds and Parallel Membrane Separation Techniques. J. Comb. Chem. 2002, 4, 112–119. [Google Scholar] [CrossRef]
- Jayaraman, G.; Li, Y.-F.; Moore, J.; Cramer, S.M. Ion-exchange displacement chromatography of proteins Dendritic polymers as novel displacers. J. Chromatogr. A 1995, 702, 143–155. [Google Scholar] [CrossRef]
- Sakai, K.; Teng, T.C.; Katada, A.; Harada, T.; Yoshida, K.; Yamanaka, K.; Asami, Y.; Sakata, M.; Hirayama, C.; Kunitake, M. Designable Size Exclusion Chromatography Columns Based on Dendritic Polymer-Modified Porous Silica Particles. Chem. Mater. 2003, 15, 4091–4097. [Google Scholar] [CrossRef]
- Cai, J.; Cao, X.-L.; Zhao, Y.; Zhou, F.-Y.; Cui, Z.; Wang, Y.; Sun, S.-P. The establishment of high-performance anti-fouling nanofiltration membranes via cooperation of annular supramolecular Cucurbit[6]uril and dendritic polyamidoamine. J. Membr. Sci. 2020, 600, 117863. [Google Scholar] [CrossRef]
- Li, X.; Cai, T.; Chung, T.-S. Anti-Fouling Behavior of Hyperbranched Polyglycerol-Grafted Poly(ether sulfone) Hollow Fiber Membranes for Osmotic Power Generation. Environ. Sci. Technol. 2014, 48, 9898–9907. [Google Scholar] [CrossRef]
- Wang, Q.; Mynar, J.L.; Yoshida, M.; Lee, E.; Lee, M.; Okuro, K.; Kinbara, K.; Aida, T. High-water-content mouldable hydrogels by mixing clay and a dendritic molecular binder. Nature 2010, 463, 339–343. [Google Scholar] [CrossRef] [PubMed]
- Ghobril, C.; Rodriguez, E.K.; Nazarian, A.; Grinstaff, M.W. Recent Advances in Dendritic Macromonomers for Hydrogel Formation and Their Medical Applications. Biomacromolecules 2016, 17, 1235–1252. [Google Scholar] [CrossRef]
- Seiler, M. Hyperbranched polymers: Phase behavior and new applications in the field of chemical engineering. Fluid Phase Equilibria 2006, 241, 155–174. [Google Scholar] [CrossRef]
- Domańska, U.; Żołek-Tryznowska, Z.; Pobudkowska, A. Separation of Hexane/Ethanol Mixtures. LLE of Ternary Systems (Ionic Liquid or Hyperbranched Polymer + Ethanol + Hexane) at T = 298.15 K. J. Chem. Eng. Data 2009, 54, 972–976. [Google Scholar] [CrossRef]
- Froehling, P.E. Dendrimers and dyes—A review. Dye. Pigment. 2001, 48, 187–195. [Google Scholar] [CrossRef]
- Xu, S.; Luo, Y.; Haag, R. Water-Soluble pH-Responsive Dendritic Core-Shell Nanocarriers for Polar Dyes Based on Poly(ethylene imine). Macromol. Biosci. 2007, 7, 968–974. [Google Scholar] [CrossRef]
- Martinho, N.; Florindo, H.; Silva, L.; Brocchini, S.; Zloh, M.; Barata, T. Molecular Modeling to Study Dendrimers for Biomedical Applications. Molecules 2014, 19, 20424–20467. [Google Scholar] [CrossRef] [PubMed]
- Esfand, R.; Tomalia, D.A. Poly(amidoamine) (PAMAM) dendrimers: From biomimicry to drug delivery and biomedical applications. Drug Discov. Today 2001, 6, 427–436. [Google Scholar] [CrossRef]
- Hecht, S.; Fréchet, J.M. Dendritic encapsulation of function: Applying nature’s site isolation principle from biomimetics to materials science. Angew. Chem. Int. Ed. 2001, 40, 74–91. [Google Scholar] [CrossRef]
- Liang, C.; Fréchet, J.M. Applying key concepts from nature: Transition state stabilization, pre-concentration and cooperativity effects in dendritic biomimetics. Prog. Polym. Sci. 2005, 30, 385–402. [Google Scholar] [CrossRef]
- Tsiourvas, D.; Tsetsekou, A.; Papavasiliou, A.; Arkas, M.; Boukos, N. A novel hybrid sol–gel method for the synthesis of highly porous silica employing hyperbranched poly(ethyleneimine) as a reactive template. Microporous Mesoporous Mater. 2013, 175, 59–66. [Google Scholar] [CrossRef]
- Arkas, M.; Tsiourvas, D. Organic/inorganic hybrid nanospheres based on hyperbranched poly(ethylene imine) encapsulated into silica for the sorption of toxic metal ions and polycyclic aromatic hydrocarbons from water. J. Hazard. Mater. 2009, 170, 35–42. [Google Scholar] [CrossRef]
- Svenson, S.; Tomalia, D.A. Dendrimers in biomedical applications—Reflections on the field. Adv. Drug Deliv. Rev. 2012, 64, 102–115. [Google Scholar] [CrossRef]
- Fan, Y.; Sun, W.; Shi, X. Design and Biomedical Applications of Poly(amidoamine)-Dendrimer-Based Hybrid Nanoarchitectures. Small Methods 2017, 1, 1700224. [Google Scholar] [CrossRef]
- Mintzer, M.A.; Grinstaff, M.W. Biomedical applications of dendrimers: A tutorial. Chem. Soc. Rev. 2011, 40, 173–190. [Google Scholar] [CrossRef]
- Wu, L.-P.; Ficker, M.; Christensen, J.B.; Trohopoulos, P.N.; Moghimi, S.M. Dendrimers in Medicine: Therapeutic Concepts and Pharmaceutical Challenges. Bioconjug. Chem. 2015, 26, 1198–1211. [Google Scholar] [CrossRef] [PubMed]
- Chis, A.A.; Dobrea, C.; Morgovan, C.; Arseniu, A.M.; Rus, L.L.; Butuca, A.; Juncan, A.M.; Totan, M.; Vonica-Tincu, A.L.; Cormos, G.; et al. Applications and Limitations of Dendrimers in Biomedicine. Molecules 2020, 25, 3982. [Google Scholar] [CrossRef]
- Araújo, R.V.D.; Santos, S.D.S.; Igne Ferreira, E.; Giarolla, J. New Advances in General Biomedical Applications of PAMAM Dendrimers. Molecules 2018, 23, 2849. [Google Scholar] [CrossRef]
- Saadati, A.; Hasanzadeh, M.; Seidi, F. Biomedical application of hyperbranched polymers: Recent Advances and challenges. TrAC Trends Anal. Chem. 2021, 142, 116308. [Google Scholar] [CrossRef]
- Oliveira, J.M.; Salgado, A.; Sousa, N.; Mano, J.; Reis, R.L. Dendrimers and derivatives as a potential therapeutic tool in regenerative medicine strategies—A review. Prog. Polym. Sci. 2010, 35, 1163–1194. [Google Scholar] [CrossRef]
- Calabretta, M.K.; Kumar, A.; McDermott, A.M.; Cai, C. Antibacterial Activities of Poly(amidoamine) Dendrimers Terminated with Amino and Poly(ethylene glycol) Groups. Biomacromolecules 2007, 8, 1807–1811. [Google Scholar] [CrossRef]
- Stach, M.; Siriwardena, T.N.; Köhler, T.; van Delden, C.; Darbre, P.-D.D.T.; Reymond, J.-L. Combining Topology and Sequence Design for the Discovery of Potent Antimicrobial Peptide Dendrimers against Multidrug-Resistant Pseudomonas aeruginosa. Angew. Chem. 2014, 126, 13041–13045. [Google Scholar] [CrossRef]
- Pérez-Anes, A.; Spataro, G.; Coppel, Y.; Moog, C.; Blanzat, M.; Turrin, C.-O.; Caminade, A.-M.; Rico-Lattes, I.; Majoral, J.-P. Phosphonate terminated PPH dendrimers: Influence of pendant alkyl chains on the in vitro anti-HIV-1 properties. Org. Biomol. Chem. 2009, 7, 3491–3498. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.-K.; Liang, P.-H.; Astronomo, R.D.; Hsu, T.-L.; Hsieh, S.-L.; Burton, D.R.; Wong, C.-H. Targeting the carbohydrates on HIV-1: Interaction of oligomannose dendrons with human monoclonal antibody 2G12 and DC-SIGN. Proc. Natl. Acad. Sci. USA 2008, 105, 3690–3695. [Google Scholar] [CrossRef] [Green Version]
- Meyers, S.R.; Juhn, F.S.; Griset, A.P.; Luman, N.R.; Grinstaff, M.W. Anionic Amphiphilic Dendrimers as Antibacterial Agents. J. Am. Chem. Soc. 2008, 130, 14444–14445. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.Z.; Beck-Tan, N.C.; Dhurjati, P.; van Dyk, T.K.; LaRossa, R.A.; Cooper, S.L. Quaternary Ammonium Functionalized Poly(propylene imine) Dendrimers as Effective Antimicrobials: Structure–Activity Studies. Biomacromolecules 2000, 1, 473–480. [Google Scholar] [CrossRef] [PubMed]
- Arkas, M.; Kithreoti, G.; Boukos, N.; Kitsou, I.; Petrakli, F.; Panagiotaki, K. Two completely different biomimetic reactions mediated by the same matrix producing inorganic/organic/inorganic hybrid nanoparticles. Nano-Struct. Nano-Objects 2018, 14, 138–148. [Google Scholar] [CrossRef]
- Pourjavadi, A.; Hosseini, S.H.; Alizadeh, M.; Bennett, C. Magnetic pH-responsive nanocarrier with long spacer length and high colloidal stability for controlled delivery of doxorubicin. Colloids Surf. B Biointerfaces 2014, 116, 49–54. [Google Scholar] [CrossRef]
- Yetisgin, A.A.; Cetinel, S.; Zuvin, M.; Kosar, A.; Kutlu, O. Therapeutic Nanoparticles and Their Targeted Delivery Applications. Molecules 2020, 25, 2193. [Google Scholar] [CrossRef]
- Le, N.T.T.; Nguyen, T.N.Q.; Cao, V.D.; Hoang, D.T.; Ngo, V.C.; Hoang Thi, T.T. Recent Progress and Advances of Multi-Stimuli-Responsive Dendrimers in Drug Delivery for Cancer Treatment. Pharmaceutics 2019, 11, 591. [Google Scholar] [CrossRef]
- Paleos, C.M.; Tsiourvas, D.; Sideratou, Z.; Tziveleka, L.-A. Drug delivery using multifunctional dendrimers and hyperbranched polymers. Expert Opin. Drug Deliv. 2010, 7, 1387–1398. [Google Scholar] [CrossRef]
- Chauhan, A.S. Dendrimers for Drug Delivery. Molecules 2018, 23, 938. [Google Scholar] [CrossRef]
- Kavand, A.; Anton, N.; Vandamme, T.; Serra, C.A.; Chan-Seng, D. Synthesis and functionalization of hyperbranched polymers for targeted drug delivery. J. Control. Release 2020, 321, 285–311. [Google Scholar] [CrossRef]
- Dias, A.P.; da Silva Santos, S.; da Silva, J.V.; Parise-Filho, R.; Ferreira, E.I.; El Seoud, O.; Giarolla, J. Dendrimers in the context of nanomedicine. Int. J. Pharm. 2020, 573, 118814. [Google Scholar] [CrossRef]
- Li, X.; Naeem, A.; Xiao, S.; Hu, L.; Zhang, J.; Zheng, Q. Safety Challenges and Application Strategies for the Use of Dendrimers in Medicine. Pharmaceutics 2022, 14, 1292. [Google Scholar] [CrossRef]
- Shi, X.; Wang, S.H.; Van Antwerp, M.E.; Chen, X.; Baker, J.J.R. Targeting and detecting cancer cells using spontaneously formed multifunctional dendrimer-stabilized gold nanoparticles. Analyst 2009, 134, 1373–1379. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Sun, J.; Zhu, H.; Wu, H.; Zhang, H.; Gu, Z.; Luo, K. Recent advances in development of dendritic polymer-based nano-medicines for cancer diagnosis. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2021, 13, e1670. [Google Scholar] [CrossRef] [PubMed]
- Shukla, R.; Singh, A.; Pardhi, V.; Sunil Dubey, P.K. Dendrimer (polyamidoamine, polypropylene imine, poly-L-lysine, carbosilane dendrimers, triazine dendrimers) as promising tool for anticancer therapeutics. In Polymeric Nanoparticles as a Promising Tool for Anti-Cancer Therapeutics; Wolff, A.G., Ed.; Elsevier Ltd.: Amsterdam, The Netherlands, 2019; pp. 233–255. ISBN 9780128169636. [Google Scholar]
- Wang, B.-Y.; Liao, M.-L.; Hong, G.-C.; Chang, W.-W.; Chu, C.-C. Near-Infrared-Triggered Photodynamic Therapy toward Breast Cancer Cells Using Dendrimer-Functionalized Upconversion Nanoparticles. Nanomaterials 2017, 7, 269. [Google Scholar] [CrossRef]
- Haensler, J.; Szoka, F.C., Jr. Polyamidoamine cascade polymers mediate efficient transfection of cells in culture. Bioconjug. Chem. 1993, 4, 372–379. [Google Scholar] [CrossRef]
- Kabanov, V.A.; Sergeyev, V.G.; Pyshkina, O.A.; Zinchenko, A.A.; Zezin, A.B.; Joosten, J.G.H.; Brackman, J.; Yoshikawa, K. Interpolyelectrolyte Complexes Formed by DNA and Astramol Poly(propylene imine) Dendrimers. Macromolecules 2000, 33, 9587–9593. [Google Scholar] [CrossRef]
- Patil, M.L.; Zhang, M.; Taratula, O.; Garbuzenko, O.B.; He, H.; Minko, T. Internally Cationic Polyamidoamine PAMAM-OH Dendrimers for siRNA Delivery: Effect of the Degree of Quaternization and Cancer Targeting. Biomacromolecules 2009, 10, 258–266. [Google Scholar] [CrossRef]
- German, N.; Popov, A.; Ramanavicius, A.; Ramanaviciene, A. Development and Practical Application of Glucose Biosensor Based on Dendritic Gold Nanostructures Modified by Conducting Polymers. Biosensors 2022, 12, 641. [Google Scholar] [CrossRef]
- Jiménez, A.; Armada, M.P.G.; Losada, J.; Villena, C.; Alonso, B.; Casado, C.M. Amperometric biosensors for NADH based on hyperbranched dendritic ferrocene polymers and Pt nanoparticles. Sens. Actuators B Chem. 2014, 190, 111–119. [Google Scholar] [CrossRef]
- Wiener, E.; Brechbiel, M.W.; Brothers, H.; Magin, R.L.; Gansow, O.A.; Tomalia, D.A.; Lauterbur, P.C. Dendrimer-based metal chelates: A new class of magnetic resonance imaging contrast agents. Magn. Reson. Med. 1994, 31, 1–8. [Google Scholar] [CrossRef]
- Nwe, K.; Bryant, J.L.H.; Brechbiel, M.W. Poly(amidoamine) Dendrimer Based MRI Contrast Agents Exhibiting Enhanced Relaxivities Derived via Metal Preligation Techniques. Bioconjug. Chem. 2010, 21, 1014–1017. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; Mou, Q.; Wang, D.; Zhu, X.; Yan, D. Dendritic Polymers for Theranostics. Theranostics 2016, 6, 930–947. [Google Scholar] [CrossRef] [PubMed]
- Korake, S.; Shaikh, A.; Salve, R.; Gajbhiye, K.; Gajbhiye, V.; Pawar, A. Biodegradable dendritic Boltorn™ nanoconstructs: A promising avenue for cancer theranostics. Int. J. Pharm. 2020, 594, 120177. [Google Scholar] [CrossRef] [PubMed]
- Dhanikula, R.S.; Argaw, A.; Bouchard, J.-F.; Hildgen, P. Methotrexate Loaded Polyether-Copolyester Dendrimers for the Treatment of Gliomas: Enhanced Efficacy and Intratumoral Transport Capability. Mol. Pharm. 2008, 5, 105–116. [Google Scholar] [CrossRef]
- Klajnert, B.; Cangiotti, M.; Calici, S.; Majoral, J.P.; Caminade, A.M.; Cladera, J.; Bryszewska, M.; Ottaviani, M.F. EPR Study of the Interactions between Dendrimers and Peptides Involved in Alzheimer’s and Prion Diseases. Macromol. Biosci. 2007, 7, 1065–1074. [Google Scholar] [CrossRef]
- Fruchon, S.; Poupot, M.; Martinet, L.; Turrin, C.-O.; Majoral, J.-P.; Fournié, J.-J.; Caminade, A.-M.; Poupot, R. Anti-inflammatory and immunosuppressive activation of human monocytes by a bioactive dendrimer. J. Leukoc. Biol. 2009, 85, 553–562. [Google Scholar] [CrossRef]
- Chandrasekar, D.; Sistla, R.; Ahmad, F.J.; Khar, R.K.; Diwan, P.V. Folate coupled poly(ethyleneglycol) conjugates of anionic poly(amidoamine) dendrimer for inflammatory tissue specific drug delivery. J. Biomed. Mater. Res. Part A 2007, 82A, 92–103. [Google Scholar] [CrossRef]
- Thomas, J.; Yadav, S.; Satija, J.; Agnihotri, S. Functional dendritic coatings for biomedical implants. In Emerging Trends in Nanomedicine; Springer: Singapore, 2021; pp. 173–201. [Google Scholar] [CrossRef]
- Jensen, L.K.; Jensen, H.E.; Blirup-Plum, S.A.; Bue, M.; Hanberg, P.; Kvich, L.; Aalbæk, B.; López, Y.; Soto, S.M.; Douloudi, M.; et al. Coating of bone implants with silica, hyperbranched polyethyleneimine, and gentamicin prevents development of osteomyelitis in a porcine model. Materialia 2022, 24, 101473. [Google Scholar] [CrossRef]
- Smith, D.M.; Simon, J.K.; Baker, J.R., Jr. Applications of nanotechnology for immunology. Nat. Rev. Immunol. 2013, 13, 592–605. [Google Scholar] [CrossRef] [PubMed]
- Grinstaff, M.W. Biodendrimers: New Polymeric Biomaterials for Tissue Engineering. Chem.—Eur. J. 2002, 8, 2838–2846. [Google Scholar] [CrossRef]
- Joshi, N.; Grinstaff, M. Applications of dendrimers in tissue engineering. Curr. Top. Med. Chem. 2008, 8, 1225–1236. [Google Scholar] [CrossRef]
- Oliveira, I.M.; Carvalho, M.R.; Reis, R.L.; Oliveira, J.M. Dendrimers in tissue engineering. In Dendrimer-Based Nanotherapeutics; Academic Press: Cambridge, MA, USA, 2021; pp. 327–336. [Google Scholar] [CrossRef]
- Shaikh, A.; Kesharwani, P.; Gajbhiye, V. Dendrimer as a momentous tool in tissue engineering and regenerative medicine. J. Control. Release 2022, 346, 328–354. [Google Scholar] [CrossRef]
- Kinberger, G.A.; Cai, W.; Goodman, M. Collagen Mimetic Dendrimers. J. Am. Chem. Soc. 2002, 124, 15162–15163. [Google Scholar] [CrossRef] [PubMed]
- Kinberger, G.A.; Taulane, J.P.; Goodman, M. The design, synthesis, and characterization of a PAMAM-based triple helical collagen mimetic dendrimer. Tetrahedron 2006, 62, 5280–5286. [Google Scholar] [CrossRef]
- Kojima, C.; Tsumura, S.; Harada, A.; Kono, K. A Collagen-Mimic Dendrimer Capable of Controlled Release. J. Am. Chem. Soc. 2009, 131, 6052–6053. [Google Scholar] [CrossRef]
- Suehiro, T.; Tada, T.; Waku, T.; Tanaka, N.; Hongo, C.; Yamamoto, S.; Nakahira, A.; Kojima, C. Temperature-dependent higher order structures of the (Pro-Pro-Gly)10-modified dendrimer. Biopolymers 2011, 95, 270–277. [Google Scholar] [CrossRef]
- Kojima, C.; Suehiro, T.; Tada, T.; Sakamoto, Y.; Waku, T.; Tanaka, N. Preparation of heat-induced artificial collagen gels based on collagen-mimetic dendrimers. Soft Matter 2011, 7, 8991–8997. [Google Scholar] [CrossRef]
- Duan, X.; Sheardown, H. Crosslinking of collagen with dendrimers. J. Biomed. Mater. Res. Part A 2005, 75A, 510–518. [Google Scholar] [CrossRef] [PubMed]
- Kojima, C.; Irie, K. Synthesis of temperature-dependent elastin-like peptide-modified dendrimer for drug delivery. Pept. Sci. 2013, 100, 714–721. [Google Scholar] [CrossRef]
- Kojima, C.; Irie, K.; Tada, T.; Tanaka, N. Temperature-sensitive elastin-mimetic dendrimers: Effect of peptide length and dendrimer generation to temperature sensitivity. Biopolymers 2014, 101, 603–612. [Google Scholar] [CrossRef]
- Fukushima, D.; Sk, U.H.; Sakamoto, Y.; Nakase, I.; Kojima, C. Dual stimuli-sensitive dendrimers: Photothermogenic gold nanoparticle-loaded thermo-responsive elastin-mimetic dendrimers. Colloids Surf. B Biointerfaces 2015, 132, 155–160. [Google Scholar] [CrossRef] [PubMed]
- Gorain, B.; Tekade, M.; Kesharwani, P.; Iyer, A.K.; Kalia, K.; Tekade, R.K. The use of nanoscaffolds and dendrimers in tissue engineering. Drug Discov. Today 2017, 22, 652–664. [Google Scholar] [CrossRef] [PubMed]
- Chan, J.C.Y.; Burugapalli, K.; Naik, H.; Kelly, J.L.; Pandit, A. Amine Functionalization of Cholecyst-Derived Extracellular Matrix with Generation 1 PAMAM Dendrimer. Biomacromolecules 2008, 9, 528–536. [Google Scholar] [CrossRef] [PubMed]
- Zhong, S.; Yung, L.Y.L. Enhanced biological stability of collagen with incorporation of PAMAM dendrimer. J. Biomed. Mater. Res. Part A 2009, 91A, 114–122. [Google Scholar] [CrossRef]
- Lee, A.S.; Inayathullah, M.; Lijkwan, M.A.; Zhao, X.; Sun, W.; Park, S.; Hong, W.X.; Parekh, M.B.; Malkovskiy, A.V.; Lau, E.; et al. Prolonged survival of transplanted stem cells after ischaemic injury via the slow release of pro-survival peptides from a collagen matrix. Nat. Biomed. Eng. 2018, 2, 104–113. [Google Scholar] [CrossRef]
- Princz, M.; Sheardown, H. Modified Dendrimer Cross-Linked Collagen-Based Matrices. J. Biomater. Sci. Polym. Ed. 2012, 23, 2207–2222. [Google Scholar] [CrossRef]
- Walsh, D.; Heise, A.; O’Brien, F.J.; Cryan, S.-A. An efficient, non-viral dendritic vector for gene delivery in tissue engineering. Gene Ther. 2017, 24, 681–691. [Google Scholar] [CrossRef] [PubMed]
- Pourabadeh, A.; Mirjalili, M.; Shahvazian, M. Modification of silk fibroin nanofibers scaffold by PAMAM dendrimer for cell culture. J. Exp. Nanosci. 2020, 15, 297–306. [Google Scholar] [CrossRef]
- Paolini, A.; Leoni, L.; Giannicchi, I.; Abbaszadeh, Z.; D’Oria, V.; Mura, F.; Cort, A.D.; Masotti, A. MicroRNAs delivery into human cells grown on 3D-printed PLA scaffolds coated with a novel fluorescent PAMAM dendrimer for biomedical applications. Sci. Rep. 2018, 8, 13888. [Google Scholar] [CrossRef]
- Goodarzi, K.; Shariatzadeh, F.J.; Solouk, A.; Akbari, S.; Mirzadeh, H. Injectable drug loaded gelatin based scaffolds as minimally invasive approach for drug delivery system: CNC/PAMAM nanoparticles. Eur. Polym. J. 2020, 139, 109992. [Google Scholar] [CrossRef]
- Grinstaff, M.W. Dendritic macromers for hydrogel formation: Tailored materials for ophthalmic, orthopedic, and biotech applications. J. Polym. Sci. Part A Polym. Chem. 2008, 46, 383–400. [Google Scholar] [CrossRef]
- Grinstaff, M.W. Designing hydrogel adhesives for corneal wound repair. Biomaterials 2007, 28, 5205–5214. [Google Scholar] [CrossRef] [PubMed]
- Kaga, S.; Arslan, M.; Sanyal, R.; Sanyal, A. Dendrimers and Dendrons as Versatile Building Blocks for the Fabrication of Functional Hydrogels. Molecules 2016, 21, 497. [Google Scholar] [CrossRef] [PubMed]
- Desai, P.N.; Yuan, Q.; Yang, H. Synthesis and Characterization of Photocurable Polyamidoamine Dendrimer Hydrogels as a Versatile Platform for Tissue Engineering and Drug Delivery. Biomacromolecules 2010, 11, 666–673. [Google Scholar] [CrossRef]
- Zhang, H.; Patel, A.; Gaharwar, A.K.; Mihaila, S.M.; Iviglia, G.; Mukundan, S.; Bae, H.; Yang, H.; Khademhosseini, A. Hyperbranched Polyester Hydrogels with Controlled Drug Release and Cell Adhesion Properties. Biomacromolecules 2013, 14, 1299–1310. [Google Scholar] [CrossRef]
- Wu, C.; Strehmel, C.; Achazi, K.; Chiappisi, L.; Dernedde, J.; Lensen, M.C.; Gradzielski, M.; Ansorge-Schumacher, M.B.; Haag, R. Enzymatically Cross-Linked Hyperbranched Polyglycerol Hydrogels as Scaffolds for Living Cells. Biomacromolecules 2014, 15, 3881–3890. [Google Scholar] [CrossRef]
- Roumani, S.; Jeanneau, C.; Giraud, T.; Cotten, A.; Laucournet, M.; Sohier, J.; Pithioux, M.; About, I. Osteogenic Potential of a Polyethylene Glycol Hydrogel Functionalized with Poly-Lysine Dendrigrafts (DGL) for Bone Regeneration. Materials 2023, 16, 862. [Google Scholar] [CrossRef]
- Mo, X.; Li, Q.; Lui, L.W.Y.; Zheng, B.; Kang, C.H.; Nugraha, B.; Yue, Z.; Jia, R.R.; Fu, H.X.; Choudhury, D.; et al. Rapid construction of mechanically- confined multi- cellular structures using dendrimeric intercellular linker. Biomaterials 2010, 31, 7455–7467. [Google Scholar] [CrossRef]
- Zhao, D.; Ong, S.-M.; Yue, Z.; Jiang, Z.; Toh, Y.-C.; Khan, M.; Shi, J.; Tan, C.-H.; Chen, J.P.; Yu, H. Dendrimer hydrazides as multivalent transient inter-cellular linkers. Biomaterials 2008, 29, 3693–3702. [Google Scholar] [CrossRef]
- Jiang, L.-Y.; Lv, B.; Luo, Y. The effects of an RGD-PAMAM dendrimer conjugate in 3D spheroid culture on cell proliferation, expression and aggregation. Biomaterials 2013, 34, 2665–2673. [Google Scholar] [CrossRef]
- Tang, N.; Chen, Z.; Lian, F.; Wang, X.; Chen, Y. Arginine–glycine–aspartic acid–polyethylene glycol–polyamidoamine dendrimer conjugate improves liver-cell aggregation and function in 3-D spheroid culture. Int. J. Nanomed. 2016, 11, 4247–4259. [Google Scholar] [CrossRef] [PubMed]
- Khew, S.T.; Yang, Q.J.; Tong, Y.W. Enzymatically crosslinked collagen-mimetic dendrimers that promote integrin-targeted cell adhesion. Biomaterials 2008, 29, 3034–3045. [Google Scholar] [CrossRef] [PubMed]
- Wegst, U.G.; Bai, H.; Saiz, E.; Tomsia, A.P.; Ritchie, R.O. Bioinspired structural materials. Nat. Mater. 2015, 14, 23–36. [Google Scholar] [CrossRef]
- Dey, A.; Bomans, P.; Muller, F.; Will, J.; Frederik, P.; De With, G.; Sommerdijk, N. The role of prenucleation clusters in surface-induced calcium phosphate crystallization. Nat. Mater. 2010, 9, 1010–1014. [Google Scholar] [CrossRef] [PubMed]
- Mahamid, J.; Sharir, A.; Addadi, L.; Weiner, S. Amorphous calcium phosphate is a major component of the forming fin bones of zebrafish: Indications for an amorphous precursor phase. Proc. Natl. Acad. Sci. USA 2008, 105, 12748–12753. [Google Scholar] [CrossRef] [PubMed]
- Mahamid, J.; Aichmayer, B.; Shimoni, E.; Ziblat, R.; Li, C.; Siegel, S.; Paris, O.; Fratzl, P.; Weiner, S.; Addadi, L. Mapping amorphous calcium phosphate transformation into crystalline mineral from the cell to the bone in zebrafish fin rays. Proc. Natl. Acad. Sci. USA 2010, 107, 6316–6321. [Google Scholar] [CrossRef] [PubMed]
- Beniash, E.; Metzler, R.A.; Lam, R.S.; Gilbert, P. Transient amorphous calcium phosphate in forming enamel. J. Struct. Biol. 2009, 166, 133–143. [Google Scholar] [CrossRef] [PubMed]
- Khopade, A.; Khopade, S.; Jain, N. Development of hemoglobin aquasomes from spherical hydroxyapatite cores precipitated in the presence of half-generation poly(amidoamine) dendrimer. Int. J. Pharm. 2002, 241, 145–154. [Google Scholar] [CrossRef] [PubMed]
- Donners, J.; Nolte, R.; Sommerdijk, N. Dendrimer-Based Hydroxyapatite Composites with Remarkable Materials Properties. Adv. Mater. 2003, 15, 313–316. [Google Scholar] [CrossRef]
- Murugan, E.; Arumugam, S. New dendrimer functionalized multi-walled carbon nanotube hybrids for bone tissue engineering. RSC Adv. 2014, 4, 35428–35441. [Google Scholar] [CrossRef]
- Vasile, E.; Serafim, A.; Petre, D.; Giol, D.; Dubruel, P.; Iovu, H.; Stancu, I.C. Direct Synthesis and Morphological Characterization of Gold-Dendrimer Nanocomposites Prepared Using PAMAM Succinamic Acid Dendrimers: Preliminary Study of the Calcification Potential. Sci. World J. 2014, 2014, 103462. [Google Scholar] [CrossRef] [PubMed]
- Hentrich, D.; Taabache, S.; Brezesinski, G.; Lange, N.; Unger, W.; Kübel, C.; Bertin, A.; Taubert, A. A Dendritic Amphiphile for Efficient Control of Biomimetic Calcium Phosphate Mineralization. Macromol. Biosci. 2017, 17, 1600524. [Google Scholar] [CrossRef]
- Zhang, F.; Zhou, Z.-H.; Yang, S.-P.; Mao, L.-H.; Chen, H.-M.; Yu, X.-B. Hydrothermal synthesis of hydroxyapatite nanorods in the presence of anionic starburst dendrimer. Mater. Lett. 2005, 59, 1422–1425. [Google Scholar] [CrossRef]
- Zhou, Z.-H.; Zhou, P.-L.; Yang, S.-P.; Yu, X.-B.; Yang, L.-Z. Controllable synthesis of hydroxyapatite nanocrystals via a dendrimer-assisted hydrothermal process. Mater. Res. Bull. 2007, 42, 1611–1618. [Google Scholar] [CrossRef]
- Yan, S.-J.; Zhou, Z.-H.; Zhang, F.; Yang, S.-P.; Yang, L.-Z.; Yu, X.-B. Effect of anionic PAMAM with amido groups starburst dendrimers on the crystallization of Ca10(PO4)6(OH)2 by hydrothermal method. Mater. Chem. Phys. 2006, 99, 164–169. [Google Scholar] [CrossRef]
- Tsiourvas, D.; Tsetsekou, A.; Kammenou, M.-I.; Boukos, N. Controlling the Formation of Hydroxyapatite Nanorods with Dendrimers. J. Am. Ceram. Soc. 2011, 94, 2023–2029. [Google Scholar] [CrossRef]
- Tsiourvas, D.; Sapalidis, A.; Papadopoulos, T. Hydroxyapatite/chitosan-based porous three-dimensional scaffolds with complex geometries. Mater. Today Commun. 2016, 7, 59–66. [Google Scholar] [CrossRef]
- Pistone, A.; Iannazzo, D.; Celesti, C.; Scolaro, C.; Giofré, S.V.; Romeo, R.; Visco, A. Chitosan/PAMAM/Hydroxyapatite Engineered Drug Release Hydrogels with Tunable Rheological Properties. Polymers 2020, 12, 754. [Google Scholar] [CrossRef] [Green Version]
- Shkilnyy, A.; Friedrich, A.; Tiersch, B.; Schöne, S.; Fechner, M.; Koetz, J.; Schläpfer, C.-W.; Taubert, A. Poly(ethylene imine)-Controlled Calcium Phosphate Mineralization. Langmuir 2008, 24, 2102–2109. [Google Scholar] [CrossRef]
- Tsiourvas, D.; Tsetsekou, A.; Arkas, M.; Diplas, S.; Mastrogianni, E. Covalent attachment of a bioactive hyperbranched polymeric layer to titanium surface for the biomimetic growth of calcium phosphates. J. Mater. Sci. Mater. Med. 2010, 22, 85–96. [Google Scholar] [CrossRef]
- Charitidis, C.A.; Skarmoutsou, A.; Tsetsekou, A.; Brasinika, D.; Tsiourvas, D. Nanomechanical properties of hydroxyapatite (HAP) with DAB dendrimers (poly-propylene imine) coatings onto titanium surfaces. Mater. Sci. Eng. B 2013, 178, 391–399. [Google Scholar] [CrossRef]
- Liu, Y.; Luo, D.; Wang, T. Hierarchical Structures of Bone and Bioinspired Bone Tissue Engineering. Small 2016, 12, 4611–4632. [Google Scholar] [CrossRef]
- Xie, L.; Wang, L.; Jia, X.; Kuang, G.; Yang, S.; Feng, H. Effects of glutamic acid shelled PAMAM dendrimers on the crystallization of calcium phosphate in diffusion systems. Polym. Bull. 2011, 66, 119–132. [Google Scholar] [CrossRef]
- Xin, J.; Chen, T.; Lin, Z.; Dong, P.; Tan, H.; Li, J. Phosphorylated dendronized poly(amido amine)s as protein analogues for directing hydroxylapatite biomineralization. Chem. Commun. 2014, 50, 6491–6493. [Google Scholar] [CrossRef] [PubMed]
- Paleos, C.; Arkas, M.; Seghrouchni, R.; Skoulios, A. Smectic Mesophases from Quaternary Amphiphilic Ammonium Salts Functionalized with Interacting Endgroups. Mol. Cryst. Liq. Cryst. 1995, 268, 179–182. [Google Scholar] [CrossRef]
- Pramanik, N.; Imae, T. Fabrication and Characterization of Dendrimer-Functionalized Mesoporous Hydroxyapatite. Langmuir 2012, 28, 14018–14027. [Google Scholar] [CrossRef]
- Huysal, M.; Şenel, M. Dendrimer functional hydroxyapatite nanoparticles generated by functionalization with siloxane-cored PAMAM dendrons. J. Colloid Interface Sci. 2017, 500, 105–112. [Google Scholar] [CrossRef]
- Wang, L.; Erasquin, U.J.; Zhao, M.; Ren, L.; Zhang, M.Y.; Cheng, G.J.; Wang, Y.; Cai, C. Stability, antimicrobial activity, and cytotoxicity of poly (amidoamine) dendrimers on titanium substrates. ACS Appl. Mater. Interfaces 2011, 3, 2885–2894. [Google Scholar] [CrossRef]
- Boduch-Lee, K.A.; Chapman, T.; Petricca, S.E.; Marra, K.G.; Kumta, P. Design and Synthesis of Hydroxyapatite Composites Containing an mPEG–Dendritic Poly(l-lysine) Star Polycaprolactone. Macromolecules 2004, 37, 8959–8966. [Google Scholar] [CrossRef]
- Staehlke, S.; Lehnfeld, J.; Schneider, A.; Nebe, J.B.; Müller, R. Terminal chemical functions of polyamidoamine dendrimer surfaces and its impact on bone cell growth. Mater. Sci. Eng. C 2019, 101, 190–203. [Google Scholar] [CrossRef]
- Vida, Y.; Collado, D.; Najera, F.; Claros, S.; Becerra, J.; Andrades, J.A.; Perez-Inestrosa, E. Dendrimer surface orientation of the RGD peptide affects mesenchymal stem cell adhesion. RSC Adv. 2016, 6, 49839–49844. [Google Scholar] [CrossRef]
- Molina, N.; González, A.; Monopoli, D.; Mentado, B.; Becerra, J.; Santos-Ruiz, L.; Vida, Y.; Perez-Inestrosa, E. Dendritic Scaffold onto Titanium Implants. A Versatile Strategy Increasing Biocompatibility. Polymers 2020, 12, 770. [Google Scholar] [CrossRef] [PubMed]
- De Jong, E.R.; Deloch, N.; Knoll, W.; Turrin, C.-O.; Majoral, J.-P.; Caminade, A.-M.; Köper, I. Synthesis and characterization of bifunctional dendrimers: Preliminary use for the coating of gold surfaces and the proliferation of human osteoblasts (HOB). N. J. Chem. 2015, 39, 7194–7205. [Google Scholar] [CrossRef]
- Bi, X.; Luckanagul, J.A.; Allen, A.; Ramaboli, M.; Campbell, E.; West, D.; Maturavongsadit, P.; Brummett, K.; Wang, Q. Synthesis of PAMAM dendrimer-based fast cross-linking hydrogel for biofabrication. J. Biomater. Sci. Polym. Ed. 2015, 26, 669–682. [Google Scholar] [CrossRef] [PubMed]
- Patil, S.S.; Nune, K.C.; Misra, R. Alginate/poly(amidoamine) injectable hybrid hydrogel for cell delivery. J. Biomater. Appl. 2018, 33, 295–314. [Google Scholar] [CrossRef]
- Jaymand, M.; Sarvari, R.; Abbaszadeh, P.; Massoumi, B.; Eskandani, M.; Beygi-Khosrowshahi, Y. Development of novel electrically conductive scaffold based on hyperbranched polyester and polythiophene for tissue engineering applications. J. Biomed. Mater. Res. Part A 2016, 104, 2673–2684. [Google Scholar] [CrossRef]
- Arumugam, S.; Ramamoorthy, P.; Chakkarapani, L.D. Biodegradable dendrimer functionalized carbon nanotube-hybrids for biomedical applications. J. Polym. Res. 2019, 26, 182. [Google Scholar] [CrossRef]
- Santos, J.L.; Oramas, E.; Pêgo, A.P.; Granja, P.L.; Tomás, H. Osteogenic differentiation of mesenchymal stem cells using PAMAM dendrimers as gene delivery vectors. J. Control. Release 2009, 134, 141–148. [Google Scholar] [CrossRef]
- Bae, Y.; Lee, S.; Green, E.S.; Park, J.H.; Ko, K.S.; Han, J.; Choi, J.S. Characterization of basic amino acids-conjugated PAMAM dendrimers as gene carriers for human adipose-derived mesenchymal stem cells. Int. J. Pharm. 2016, 501, 75–86. [Google Scholar] [CrossRef]
- Maturavongsadit, P.; Bi, X.; Gado, T.A.; Nie, Y.-Z.; Wang, Q. Adhesive peptides conjugated PAMAM dendrimer as a coating polymeric material enhancing cell responses. Chin. Chem. Lett. 2016, 27, 1473–1478. [Google Scholar] [CrossRef]
- Oliveira, J.M.; Kotobuki, N.; Marques, A.P.; Pirraco, R.P.; Benesch, J.; Hirose, M.; Costa, S.A.; Mano, J.F.; Ohgushi, H.; Reis, R.L. Surface Engineered Carboxymethylchitosan/Poly(amidoamine) Dendrimer Nanoparticles for Intracellular Targeting. Adv. Funct. Mater. 2008, 18, 1840–1853. [Google Scholar] [CrossRef]
- Oliveira, J.M.; Sousa, R.; Kotobuki, N.; Tadokoro, M.; Hirose, M.; Mano, J.F.; Reis, R.L.; Ohgushi, H. The osteogenic differentiation of rat bone marrow stromal cells cultured with dexamethasone-loaded carboxymethylchitosan/poly(amidoamine) dendrimer nanoparticles. Biomaterials 2009, 30, 804–813. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, J.; Kotobuki, N.; Tadokoro, M.; Hirose, M.; Mano, J.; Reis, R.; Ohgushi, H. Ex vivo culturing of stromal cells with dexamethasone-loaded carboxymethylchitosan/poly(amidoamine) dendrimer nanoparticles promotes ectopic bone formation. Bone 2010, 46, 1424–1435. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, J.M.; Sousa, R.A.; Malafaya, P.B.; Silva, S.S.; Kotobuki, N.; Hirose, M.; Ohgushi, H.; Mano, J.F.; Reis, R.L. In vivo study of dendronlike nanoparticles for stem cells “tune-up”: From nano to tissues. Nanomed. Nanotechnol. Biol. Med. 2011, 7, 914–924. [Google Scholar] [CrossRef]
- Meikle, S.T.; Bianchi, G.; Olivier, G.; Santin, M. Osteoconductive phosphoserine-modified poly(ε-lysine) dendrons: Synthesis, titanium oxide surface functionalization and response of osteoblast-like cell lines. J. R. Soc. Interface 2013, 10, 20120765. [Google Scholar] [CrossRef]
- Galli, C.; Piemontese, M.; Meikle, S.T.; Santin, M.; Macaluso, G.M.; Passeri, G. Biomimetic coating with phosphoserine-tethered poly(epsilon-lysine) dendrons on titanium surfaces enhances Wnt and osteoblastic differentiation. Clin. Oral Implant. Res. 2014, 25, e133–e139. [Google Scholar] [CrossRef]
- Raucci, M.G.; Alvarez-Perez, M.A.; Meikle, S.; Ambrosio, L.; Santin, M. Poly(Epsilon-Lysine) Dendrons Tethered with Phosphoserine Increase Mesenchymal Stem Cell Differentiation Potential of Calcium Phosphate Gels. Tissue Eng. Part A 2014, 20, 474–485. [Google Scholar] [CrossRef]
- Wang, Y.; Zhao, Q.; Zhang, H.; Yang, S.; Jia, X. A Novel Poly(amido amine)-Dendrimer-Based Hydrogel as a Mimic for the Extracellular Matrix. Adv. Mater. 2014, 26, 4163–4167. [Google Scholar] [CrossRef]
- Bi, X.; Maturavongsadit, P.; Tan, Y.; Watts, M.; Bi, E.; Kegley, Z.; Morton, S.; Lu, L.; Wang, Q.; Liang, A. Polyamidoamine dendrimer-PEG hydrogel and its mechanical property on differentiation of mesenchymal stem cells. Bio-Med. Mater. Eng. 2019, 30, 111–123. [Google Scholar] [CrossRef]
- Gao, C.; Zhang, Y.; Xie, J.; Wang, X.; Cao, L.; Chen, G.; Mao, H.; Bi, X.; Gu, Z.; Yang, J. VE-cadherin functionalized injectable PAMAM/HA hydrogel promotes endothelial differentiation of hMSCs and vascularization. Appl. Mater. Today 2020, 20, 100690. [Google Scholar] [CrossRef]
- Murugan, E.; Akshata, C.; Yogaraj, V.; Sudhandiran, G.; Babu, D. Synthesis, characterization and in vitro evaluation of dendrimer-MWCNT reinforced SrHAP composite for bone tissue engineering. Ceram. Int. 2022, 48, 16000–16009. [Google Scholar] [CrossRef]
- Chatzipetros, E.; Christopoulos, P.; Donta, C.; Tosios, K.; Tsiambas, E.; Tsiourvas, D.; Kalogirou, E.; Tsiklakis, K. Application of nano-hydroxyapatite/chitosan scaffolds on rat calvarial critical-sized defects: A pilot study. Med. Oral Patol. Oral Cir. Bucal 2018, 23, e625–e632. [Google Scholar] [CrossRef]
- Chatzipetros, E.; Damaskos, S.; Tosios, K.I.; Christopoulos, P.; Donta, C.; Kalogirou, E.-M.; Yfanti, Z.; Tsiourvas, D.; Papavasiliou, A.; Tsiklakis, K. The effect of nano-hydroxyapatite/chitosan scaffolds on rat calvarial defects for bone regeneration. Int. J. Implant. Dent. 2021, 7, 40. [Google Scholar] [CrossRef] [PubMed]
- Stübinger, S.; Nuss, K.; Bürki, A.; Mosch, I.; le Sidler, M.; Meikle, S.T.; von Rechenberg, B.; Santin, M. Osseointegration of titanium implants functionalised with phosphoserine-tethered poly(epsilon-lysine) dendrons: A comparative study with traditional surface treatments in sheep. J. Mater. Sci. Mater. Med. 2015, 26, 87. [Google Scholar] [CrossRef]
- Bengazi, F.; Lang, N.P.; Canciani, E.; Viganò, P.; Velez, J.U.; Botticelli, D. Osseointegration of implants with dendrimers surface characteristics installed conventionally or with Piezosurgery®. A comparative study in the dog. Clin. Oral Implant. Res. 2014, 25, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Yuan, B.; Raucci, M.G.; Fan, Y.; Zhu, X.; Yang, X.; Zhang, X.; Santin, M.; Ambrosio, L. Injectable strontium-doped hydroxyapatite integrated with phosphoserine-tethered poly(epsilon-lysine) dendrons for osteoporotic bone defect repair. J. Mater. Chem. B 2018, 6, 7974–7984. [Google Scholar] [CrossRef]
- Yang, L.; Chen, S.; Shang, T.; Zhao, R.; Yuan, B.; Zhu, X.; Raucci, M.G.; Yang, X.; Zhang, X.; Santin, M.; et al. Complexation of Injectable Biphasic Calcium Phosphate with Phosphoserine-Presenting Dendrons with Enhanced Osteoregenerative Properties. ACS Appl. Mater. Interfaces 2020, 12, 37873–37884. [Google Scholar] [CrossRef]
- Wang, Y.; Zhao, Q.; Luo, Y.; Xu, Z.; Zhang, H.; Yang, S.; Wei, Y.; Jia, X. A high stiffness bio-inspired hydrogel from the combination of a poly(amido amine) dendrimer with DOPA. Chem. Commun. 2015, 51, 16786–16789. [Google Scholar] [CrossRef]
- Palmer, L.C.; Newcomb, C.J.; Kaltz, S.R.; Spoerke, E.D.; Stupp, S.I. Biomimetic Systems for Hydroxyapatite Mineralization Inspired by Bone and Enamel. Chem. Rev. 2008, 108, 4754–4783. [Google Scholar] [CrossRef]
- Hill, E.; Shukla, R.; Park, S.S.; Baker, J.R., Jr. Synthetic PAMAM–RGD Conjugates Target and Bind To Odontoblast-like MDPC 23 cells and the Predentin in Tooth Organ Cultures. Bioconjug. Chem. 2007, 18, 1756–1762. [Google Scholar] [CrossRef]
- Kim, J.K.; Shukla, R.; Casagrande, L.; Sedgley, C.; Nör, J.E.; Baker, J.R., Jr.; Hill, E.E. Differentiating dental pulp cells via RGD-dendrimer conjugates. J. Dent. Res. 2010, 89, 1433–1438. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Gao, Y.; Zhu, X.; Zhang, Y.; Xu, H.; Wang, T.; Zhang, G. Phosphorylated PAMAM dendrimers: An analog of dentin non-collagenous proteins, enhancing the osteo/odontogenic differentiation of dental pulp stem cells. Clin. Oral Investig. 2022, 26, 1737–1751. [Google Scholar] [CrossRef] [PubMed]
- Bapat, R.A.; Dharmadhikari, S.; Chaubal, T.V.; Amin, M.C.I.M.; Bapat, P.; Gorain, B.; Choudhury, H.; Vincent, C.; Kesharwani, P. The potential of dendrimer in delivery of therapeutics for dentistry. Heliyon 2019, 5, e02544. [Google Scholar] [CrossRef]
- Li, J.; Yang, J.; Li, J.; Chen, L.; Liang, K.; Wu, W.; Chen, X.; Li, J. Bioinspired intrafibrillar mineralization of human dentine by PAMAM dendrimer. Biomaterials 2013, 34, 6738–6747. [Google Scholar] [CrossRef] [PubMed]
- Xie, F.; Wei, X.; Li, Q.; Zhou, T. In vivo analyses of the effects of polyamidoamine dendrimer on dentin biomineralization and dentinal tubules occlusion. Dent. Mater. J. 2016, 35, 104–111. [Google Scholar] [CrossRef] [PubMed]
- Liang, K.; Yuan, H.; Li, J.; Yang, J.; Zhou, X.; He, L.; Cheng, L.; Gao, Y.; Xu, X.; Zhou, X.; et al. Remineralization of Demineralized Dentin Induced by Amine-Terminated PAMAM Dendrimer. Macromol. Mater. Eng. 2015, 300, 107–117. [Google Scholar] [CrossRef]
- Wang, T.; Yang, S.; Wang, L.; Feng, H. Use of Poly (Amidoamine) Dendrimer for Dentinal Tubule Occlusion: A Preliminary Study. PLoS ONE 2015, 10, e0124735. [Google Scholar] [CrossRef]
- Khater, A.A.A.E.-A.; Niazy, M.A.; Gad, N.A.E.-A. The Effect of Poly Amido Amine Dendrimer, Gluteraldehyde and Their Combination on the Micro Hardness and Micromorphology of Demineralized Dentin. Al-Azhar Dent. J. Girls 2018, 5, 341–347. [Google Scholar] [CrossRef] [Green Version]
- Jia, R.; Lu, Y.; Yang, C.-W.; Luo, X.; Han, Y. Effect of generation 4.0 polyamidoamine dendrimer on the mineralization of demineralized dentinal tubules in vitro. Arch. Oral Biol. 2014, 59, 1085–1093. [Google Scholar] [CrossRef]
- Gao, Y.; Liang, K.; Li, J.; Yuan, H.; Liu, H.; Duan, X.; Li, J. Effect and Stability of Poly(Amido Amine)-Induced Biomineralization on Dentinal Tubule Occlusion. Materials 2017, 10, 384. [Google Scholar] [CrossRef]
- Liang, K.; Gao, Y.; Li, J.; Liao, Y.; Xiao, S.; Lv, H.; He, L.; Cheng, L.; Zhou, X.; Li, J. Effective dentinal tubule occlusion induced by polyhydroxy-terminated PAMAM dendrimer in vitro. RSC Adv. 2014, 4, 43496–43503. [Google Scholar] [CrossRef]
- Tao, S.; Fan, M.; Xu, H.H.K.; Li, J.; He, L.; Zhou, X.; Liang, K.; Li, J. The remineralization effectiveness of PAMAM dendrimer with different terminal groups on demineralized dentin in vitro. RSC Adv. 2017, 7, 54947–54955. [Google Scholar] [CrossRef]
- Liang, K.; Gao, Y.; Li, J.; Liao, Y.; Xiao, S.; Zhou, X.; Li, J. Biomimetic mineralization of collagen fibrils induced by amine-terminated PAMAM dendrimers—PAMAM dendrimers for remineralization. J. Biomater. Sci. Polym. Ed. 2015, 26, 963–974. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Huang, J.; Qin, H.; Long, J.; Lin, X.; Xie, F. Remineralization of human dentin type I collagen fibrils induced by carboxylated polyamidoamine dendrimer/amorphous calcium phosphate nanocomposite: An in vitro study. J. Biomater. Sci. Polym. Ed. 2022, 33, 668–686. [Google Scholar] [CrossRef]
- Xie, F.; Li, Q.; Wei, X.; Zhou, T. [Effect of Ca(OH)2 pre-treated on remineralization of the demineralized dentin induced by polyamidoamine dendrime]. Chin. J. Stomatol. 2015, 50, 244–247. [Google Scholar]
- Liang, K.; Wang, S.; Tao, S.; Xiao, S.; Zhou, H.; Cheng, L.; Zhou, X.; Weir, M.D.; Oates, T.W.; Li, J.; et al. Dental remineralization via poly(amido amine) and restorative materials containing calcium phosphate nanoparticles. Int. J. Oral Sci. 2019, 11, 15. [Google Scholar] [CrossRef]
- Liang, K.; Weir, M.D.; Xie, X.; Wang, L.; Reynolds, M.A.; Li, J.; Xu, H.H. Dentin remineralization in acid challenge environment via PAMAM and calcium phosphate composite. Dent. Mater. 2016, 32, 1429–1440. [Google Scholar] [CrossRef]
- Liang, K.; Gao, Y.; Xiao, S.; Tay, F.R.; Weir, M.D.; Zhou, X.; Oates, T.W.; Zhou, C.; Li, J.; Xu, H.H. Poly(amido amine) and rechargeable adhesive containing calcium phosphate nanoparticles for long-term dentin remineralization. J. Dent. 2019, 85, 47–56. [Google Scholar] [CrossRef]
- Liang, K.; Xiao, S.; Weir, M.D.; Bao, C.; Liu, H.; Cheng, L.; Zhou, X.; Li, J.; Xu, H.H.K. Poly (amido amine) dendrimer and dental adhesive with calcium phosphate nanoparticles remineralized dentin in lactic acid. J. Biomed. Mater. Res. Part B Appl. Biomater. 2018, 106, 2414–2424. [Google Scholar] [CrossRef]
- Liang, K.; Weir, M.D.; Reynolds, M.A.; Zhou, X.; Li, J.; Xu, H.H. Poly (amido amine) and nano-calcium phosphate bonding agent to remineralize tooth dentin in cyclic artificial saliva/lactic acid. Mater. Sci. Eng. C 2017, 72, 7–17. [Google Scholar] [CrossRef]
- Liang, K.; Zhou, H.; Weir, M.D.; Bao, C.; Reynolds, M.A.; Zhou, X.; Li, J.; Xu, H.H. Poly(amido amine) and calcium phosphate nanocomposite remineralization of dentin in acidic solution without calcium phosphate ions. Dent. Mater. 2017, 33, 818–829. [Google Scholar] [CrossRef] [PubMed]
- Liang, K.; Xiao, S.; Wu, J.; Li, J.; Weir, M.D.; Cheng, L.; Reynolds, M.A.; Zhou, X.; Xu, H.H. Long-term dentin remineralization by poly(amido amine) and rechargeable calcium phosphate nanocomposite after fluid challenges. Dent. Mater. 2018, 34, 607–618. [Google Scholar] [CrossRef] [PubMed]
- Liang, K.; Gao, Y.; Tao, S.; Weir, M.D.; Zhou, C.; Li, J.; Xu, H.H.K. Dentin remineralization in acidic solution without initial calcium phosphate ions via poly(amido amine) and calcium phosphate nanocomposites after fluid challenges. Clin. Oral Investig. 2022, 26, 1517–1530. [Google Scholar] [CrossRef]
- Xiao, S.; Liang, K.; Weir, M.D.; Cheng, L.; Liu, H.; Zhou, X.; Ding, Y.; Xu, H.H.K. Combining Bioactive Multifunctional Dental Composite with PAMAM for Root Dentin Remineralization. Materials 2017, 10, 89. [Google Scholar] [CrossRef] [PubMed]
- Chuang, S.-F.; Chen, Y.-H.; Ma, P.; Ritchie, H.H. Phosphophoryn and Dentin Sialoprotein Effects on Dental Pulp Cell Migration, Proliferation, and Differentiation. Dent. J. 2018, 6, 70. [Google Scholar] [CrossRef] [PubMed]
- Wen, Y.; Wang, J.; Luo, J.; Yang, J. Remineralization of dentine tubules induced by phosphate-terminated PAMAM dendrimers. Heliyon 2020, 6, e05886. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.; Yang, S.; Wang, L.; Feng, H. Use of multifunctional phosphorylated PAMAM dendrimers for dentin biomimetic remineralization and dentinal tubule occlusion. RSC Adv. 2015, 5, 11136–11144. [Google Scholar] [CrossRef]
- Zhang, H.; Yang, J.; Liang, K.; Li, J.; He, L.; Yang, X.; Peng, S.; Chen, X.; Ding, C.; Li, J. Effective dentin restorative material based on phosphate-terminated dendrimer as artificial protein. Colloids Surf. B Biointerfaces 2015, 128, 304–314. [Google Scholar] [CrossRef] [PubMed]
- Qin, H.; Long, J.; Zhou, J.; Wu, L.; Xie, F. Use of phosphorylated PAMAM and carboxyled PAMAM to induce dentin biomimetic remineralization and dentinal tubule occlusion. Dent. Mater. J. 2021, 40, 800–807. [Google Scholar] [CrossRef]
- Xie, F.; Long, J.; Yang, J.; Qin, H.; Lin, X.; Chen, W. Effect of a new modified polyamidoamine dendrimer biomimetic system on the mineralization of type I collagen fibrils: An in vitro study. J. Biomater. Sci. Polym. Ed. 2022, 33, 212–228. [Google Scholar] [CrossRef]
- Lin, X.; Xie, F.; Ma, X.; Hao, Y.; Qin, H.; Long, J. Fabrication and characterization of dendrimer-functionalized nano-hydroxyapatite and its application in dentin tubule occlusion. J. Biomater. Sci. Polym. Ed. 2017, 28, 846–863. [Google Scholar] [CrossRef] [PubMed]
- Bae, J.; Son, W.-S.; Yoo, K.-H.; Yoon, S.-Y.; Bae, M.-K.; Lee, D.J.; Ko, C.-C.; Choi, Y.-K.; Kim, Y.-I. Effects of Poly(Amidoamine) Dendrimer-Coated Mesoporous Bioactive Glass Nanoparticles on Dentin Remineralization. Nanomaterials 2019, 9, 591. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Yang, J.; Lin, Z.; Li, J.; Liang, K.; Yuan, H.; Li, S.; Li, J. Triclosan-loaded poly(amido amine) dendrimer for simultaneous treatment and remineralization of human dentine. Colloids Surf. B Biointerfaces 2014, 115, 237–243. [Google Scholar] [CrossRef]
- Zhu, B.; Li, X.; Xu, X.; Li, J.; Ding, C.; Zhao, C.; Li, J. One-step phosphorylated poly(amide-amine) dendrimer loaded with apigenin for simultaneous remineralization and antibacterial of dentine. Colloids Surf. B Biointerfaces 2018, 172, 760–768. [Google Scholar] [CrossRef] [PubMed]
- Cai, X.; Wang, X. Chlorhexidine-loaded poly (amido amine) dendrimer and a dental adhesive containing amorphous calcium phosphate nanofillers for enhancing bonding durability. Dent. Mater. 2022, 38, 824–834. [Google Scholar] [CrossRef]
- Chen, L.; Chen, W.; Yu, Y.; Yang, J.; Jiang, Q.; Wu, W.; Yang, D. Effect of chlorhexidine-loaded poly(amido amine) dendrimer on matrix metalloproteinase activities and remineralization in etched human dentin in vitro. J. Mech. Behav. Biomed. Mater. 2021, 121, 104625. [Google Scholar] [CrossRef]
- EL Wafa, M.R.A.; Niazy, M.A.; Hagar, E.A.A.; Abu-Seida, A.M. Biological Pulp Response of Pulpine, Polyamidoamine Dendrimer and Their Combination in Dogs and their Remineralizing Effect on Carious Affected Human Dentin: A Randomized Clinical Trial. Al-Azhar Dent. J. Girls 2021, 8, 591–600. [Google Scholar] [CrossRef]
- Jaymand, M.; Lotfi, M.; Lotfi, R. Functional dendritic compounds: Potential prospective candidates for dental restorative materials and in situ re-mineralization of human tooth enamel. RSC Adv. 2016, 6, 43127–43146. [Google Scholar] [CrossRef]
- Chen, L.; Liang, K.; Li, J.; Wu, D.; Zhou, X.; Li, J. Regeneration of biomimetic hydroxyapatite on etched human enamel by anionic PAMAM template in vitro. Arch. Oral Biol. 2013, 58, 975–980. [Google Scholar] [CrossRef]
- Chen, L.; Yuan, H.; Tang, B.; Liang, K.; Li, J. Biomimetic Remineralization of Human Enamel in the Presence of Polyamidoamine Dendrimers in vitro. Caries Res. 2015, 49, 282–290. [Google Scholar] [CrossRef]
- Fan, M.; Zhang, M.; Xu, H.H.; Tao, S.; Yu, Z.; Yang, J.; Yuan, H.; Zhou, X.; Liang, K.; Li, J. Remineralization effectiveness of the PAMAM dendrimer with different terminal groups on artificial initial enamel caries in vitro. Dent. Mater. 2020, 36, 210–220. [Google Scholar] [CrossRef]
- Jia, L.; Tao, S.; Yang, J.; Liang, K.; Yu, Z.; Gao, Y.; Fan, M.; Zhang, M.; He, L.; Li, J. Adhesion of Streptococcus mutans on remineralized enamel surface induced by poly(amido amine) dendrimers. Colloids Surf. B Biointerfaces 2021, 197, 111409. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.; Yang, J.; Li, J.; Liang, K.; He, L.; Lin, Z.; Chen, X.; Ren, X.; Li, J. Modulated regeneration of acid-etched human tooth enamel by a functionalized dendrimer that is an analog of amelogenin. Acta Biomater. 2014, 10, 4437–4446. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; He, H.; Wang, L.; Jia, X.; Feng, H. Oriented crystallization of hydroxyapatite by the biomimetic amelogenin nanospheres from self-assemblies of amphiphilic dendrons. Chem. Commun. 2011, 47, 10100–10102. [Google Scholar] [CrossRef]
- Yang, J.; Cao, S.; Li, J.; Xin, J.; Chen, X.; Wu, W.; Xu, F.; Li, J. Staged self-assembly of PAMAM dendrimers into macroscopic aggregates with a microribbon structure similar to that of amelogenin. Soft Matter 2013, 9, 7553–7559. [Google Scholar] [CrossRef]
- Wu, D.; Yang, J.; Li, J.; Chen, L.; Tang, B.; Chen, X.; Wu, W.; Li, J. Hydroxyapatite-anchored dendrimer for in situ remineralization of human tooth enamel. Biomaterials 2013, 34, 5036–5047. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Liang, K.; Weir, M.D.; Gao, J.; Imazato, S.; Tay, F.; Lynch, C.D.; Oates, T.W.; Li, J.; Xu, H.H. Enamel remineralization via poly(amido amine) and adhesive resin containing calcium phosphate nanoparticles. J. Dent. 2020, 92, 103262. [Google Scholar] [CrossRef] [PubMed]
- Tao, S.; Yang, X.; Liao, L.; Yang, J.; Liang, K.; Zeng, S.; Zhou, J.; Zhang, M.; Li, J. A novel anticaries agent, honokiol-loaded poly(amido amine) dendrimer, for simultaneous long-term antibacterial treatment and remineralization of demineralized enamel. Dent. Mater. 2021, 37, 1337–1349. [Google Scholar] [CrossRef]
- Carnahan, M.A.; Middleton, C.; Kim, J.; Kim, T.; Grinstaff, M.W. Hybrid Dendritic–Linear Polyester–Ethers for in Situ Photopolymerization. J. Am. Chem. Soc. 2002, 124, 5291–5293. [Google Scholar] [CrossRef] [PubMed]
- Velazquez, A.J.; Carnahan, M.A.; Kristinsson, J.; Stinnett, S.; Grinstaff, M.W.; Kim, T. New Dendritic Adhesives for Sutureless Ophthalmic Surgical Procedures. Arch. Ophthalmol. 2004, 122, 867–870. [Google Scholar] [CrossRef]
- Degoricija, L.; Johnson, C.S.; Wathier, M.; Kim, T.; Grinstaff, M.W. Photo Cross-linkable Biodendrimers as Ophthalmic Adhesives for Central Lacerations and Penetrating Keratoplasties. Investig. Opthalmology Vis. Sci. 2007, 48, 2037–2042. [Google Scholar] [CrossRef] [PubMed]
- Berdahl, J.P.; Johnson, C.S.; Proia, A.D.; Grinstaff, M.W.; Kim, T. Comparison of Sutures and Dendritic Polymer Adhesives for Corneal Laceration Repair in an In Vivo Chicken Model. JAMA Ophthalmol 2009, 127, 442. [Google Scholar] [CrossRef] [PubMed]
- Wathier, M.; Jung, P.J.; Carnahan, M.A.; Kim, T.; Grinstaff, M.W. Dendritic Macromers as in Situ Polymerizing Biomaterials for Securing Cataract Incisions. J. Am. Chem. Soc. 2004, 126, 12744–12745. [Google Scholar] [CrossRef]
- Wathier, M.; Johnson, C.S.; Kim, T.; Grinstaff, M.W. Hydrogels Formed by Multiple Peptide Ligation Reactions to Fasten Corneal Transplants. Bioconjug. Chem. 2006, 17, 873–876. [Google Scholar] [CrossRef]
- Johnson, C.S.; Wathier, M.; Grinstaff, M.; Kim, T. In Vitro Sealing of Clear Corneal Cataract Incisions With a Novel Biodendrimer Adhesive. Arch. Ophthalmol. 2009, 127, 430–434. [Google Scholar] [CrossRef] [PubMed]
- Oelker, A.M.; Berlin, J.A.; Wathier, M.; Grinstaff, M.W. Synthesis and Characterization of Dendron Cross-Linked PEG Hydrogels as Corneal Adhesives. Biomacromolecules 2011, 12, 1658–1665. [Google Scholar] [CrossRef]
- Kang, P.C.; Carnahan, M.A.; Wathier, M.; Grinstaff, M.W.; Kim, T. Novel tissue adhesives to secure laser in situ keratomileusis flaps. J. Cataract. Refract. Surg. 2005, 31, 1208–1212. [Google Scholar] [CrossRef]
- Oelker, A.M.; Grinstaff, M.W. Synthesis, Characterization, and In Vitro Evaluation of a Hydrogel-Based Corneal Onlay. IEEE Trans. Nanobiosci. 2011, 11, 37–45. [Google Scholar] [CrossRef]
- Duan, X.; Sheardown, H. Dendrimer crosslinked collagen as a corneal tissue engineering scaffold: Mechanical properties and corneal epithelial cell interactions. Biomaterials 2006, 27, 4608–4617. [Google Scholar] [CrossRef]
- Princz, M.A.; Sheardown, H. Heparin-modified dendrimer cross-linked collagen matrices for the delivery of basic fibroblast growth factor (FGF-2). J. Biomater. Sci. Polym. Ed. 2008, 19, 1201–1218. [Google Scholar] [CrossRef]
- Princz, M.; Sheardown, H. Heparin-modified dendrimer crosslinked collagen matrices for the delivery of heparin-binding epidermal growth factor. J. Biomed. Mater. Res. Part A 2012, 100A, 1929–1937. [Google Scholar] [CrossRef] [PubMed]
- Duan, X.; McLaughlin, C.; Griffith, M.; Sheardown, H. Biofunctionalization of collagen for improved biological response: Scaffolds for corneal tissue engineering. Biomaterials 2007, 28, 78–88. [Google Scholar] [CrossRef] [PubMed]
- Khalili, M.; Zarebkohan, A.; Dianat-Moghadam, H.; Panahi, M.; Andre, H.; Alizadeh, E. Corneal endothelial cell sheet bioengineering from neural crest cell-derived adipose stem cells on novel thermo-responsive elastin-mimetic dendrimers decorated with RGD. Chem. Eng. J. 2022, 429, 132523. [Google Scholar] [CrossRef]
- Carrancá, M.; Griveau, L.; Remoué, N.; Lorion, C.; Weiss, P.; Orea, V.; Sigaudo-Roussel, D.; Faye, C.; Ferri-Angulo, D.; Debret, R.; et al. Versatile lysine dendrigrafts and polyethylene glycol hydrogels with inherent biological properties: In vitro cell behavior modulation and in vivo biocompatibility. J. Biomed. Mater. Res. Part A 2020, 109, 926–937. [Google Scholar] [CrossRef]
- Ghobril, C.; Charoen, K.; Rodriguez, E.K.; Nazarian, A.; Grinstaff, M. A Dendritic Thioester Hydrogel Based on Thiol-Thioester Exchange as a Dissolvable Sealant System for Wound Closure. Angew. Chem. Int. Ed. 2013, 52, 14070–14074. [Google Scholar] [CrossRef]
- Zhang, Y.; Li, X.; Bai, G.; Wei, W.; Liu, X. Hyperbranched polymer with dynamic thiol–aldehyde crosslinking and its application as a self-healable bioadhesive. J. Mater. Chem. B 2021, 9, 5818–5828. [Google Scholar] [CrossRef]
- Granskog, V.; Andrén, O.C.J.; Cai, Y.; González-Granillo, M.; Felländer-Tsai, L.; von Holst, H.; Haldosen, L.-A.; Malkoch, M. Linear Dendritic Block Copolymers as Promising Biomaterials for the Manufacturing of Soft Tissue Adhesive Patches Using Visible Light Initiated Thiol-Ene Coupling Chemistry. Adv. Funct. Mater. 2015, 25, 6596–6605. [Google Scholar] [CrossRef]
- Konieczynska, M.D.; Villa-Camacho, J.C.; Ghobril, C.; Perez-Viloria, M.; Tevis, K.M.; Blessing, W.A.; Nazarian, A.; Rodriguez, E.K.; Grinstaff, M.W. On-Demand Dissolution of a Dendritic Hydrogel-based Dressing for Second-Degree Burn Wounds through Thiol-Thioester Exchange Reaction. Angew. Chem. Int. Ed. 2016, 55, 9984–9987. [Google Scholar] [CrossRef]
- Villa-Camacho, J.C.; Ghobril, C.; Anez-Bustillos, L.; Grinstaff, M.W.; Rodríguez, E.K.; Nazarian, A. The efficacy of a lysine-based dendritic hydrogel does not differ from those of commercially available tissue sealants and adhesives: An ex vivo study. BMC Musculoskelet. Disord. 2015, 16, 116. [Google Scholar] [CrossRef] [Green Version]
- Abdel-Sayed, P.; Kaeppeli, A.; Siriwardena, T.; Darbre, T.; Perron, K.; Jafari, P.; Reymond, J.-L.; Pioletti, D.P.; Applegate, L.A. Anti-Microbial Dendrimers against Multidrug-Resistant P. aeruginosa Enhance the Angiogenic Effect of Biological Burn-wound Bandages. Sci. Rep. 2016, 6, 22020. [Google Scholar] [CrossRef]
- Liu, Z.-J.; Daftarian, P.; Kovalski, L.; Wang, B.; Tian, R.; Castilla, D.M.; Dikici, E.; Perez, V.L.; Deo, S.; Daunert, S.; et al. Directing and Potentiating Stem Cell-Mediated Angiogenesis and Tissue Repair by Cell Surface E-Selectin Coating. PLoS ONE 2016, 11, e0154053. [Google Scholar] [CrossRef]
- Maji, S.; Agarwal, T.; Maiti, T.K. PAMAM (generation 4) incorporated gelatin 3D matrix as an improved dermal substitute for skin tissue engineering. Colloids Surf. B Biointerfaces 2017, 155, 128–134. [Google Scholar] [CrossRef]
- Ganjalinia, A.; Akbari, S.; Solouk, A. Tuning poly (L-lactic acid) scaffolds with poly(amidoamine) and poly(propylene imine) dendrimers: Surface chemistry, biodegradation and biocompatibility. J. Macromol. Sci. Part A 2021, 58, 433–447. [Google Scholar] [CrossRef]
- Vedhanayagam, M.; Kumar, A.S.; Nair, B.U.; Sreeram, K.J. Dendrimer-Functionalized Metal Oxide Nanoparticle-Mediated Self-Assembled Collagen Scaffold for Skin Regenerative Application: Function of Metal in Metal Oxides. Appl. Biochem. Biotechnol. 2022, 194, 266–290. [Google Scholar] [CrossRef] [PubMed]
- Vedhanayagam, M.; Nair, B.U.; Sreeram, K.J. Collagen-ZnO Scaffolds for Wound Healing Applications: Role of Dendrimer Functionalization and Nanoparticle Morphology. ACS Appl. Bio Mater. 2018, 1, 1942–1958. [Google Scholar] [CrossRef] [PubMed]
- Vedhanayagam, M.; Nair, B.U.; Sreeram, K.J. Dimension effect: Dendrimer functionalized carbon based nanomaterial mediated collagen scaffold for wound healing application. Materialia 2019, 7, 100354. [Google Scholar] [CrossRef]
- Luman, N.R.; Kim, T.; Grinstaff, M.W. Dendritic polymers composed of glycerol and succinic acid: Synthetic methodologies and medical applications. Pure Appl. Chem. 2004, 76, 1375–1385. [Google Scholar] [CrossRef]
- Söntjens, S.H.M.; Nettles, D.L.; Carnahan, M.A.; Setton, L.A.; Grinstaff, M.W. Biodendrimer-Based Hydrogel Scaffolds for Cartilage Tissue Repair. Biomacromolecules 2006, 7, 310–316. [Google Scholar] [CrossRef]
- Degoricija, L.; Bansal, P.N.; Söntjens, S.; Joshi, N.; Takahashi, M.; Snyder, B.; Grinstaff, M. Hydrogels for Osteochondral Repair Based on Photocrosslinkable Carbamate Dendrimers. Biomacromolecules 2008, 9, 2863–2872. [Google Scholar] [CrossRef] [Green Version]
- Hu, Q.; Ding, B.; Yan, X.; Peng, L.; Duan, J.; Yang, S.; Cheng, L.; Chen, D. Polyethylene glycol modified PAMAM dendrimer delivery of kartogenin to induce chondrogenic differentiation of mesenchymal stem cells. Nanomed. Nanotechnol. Biol. Med. 2017, 13, 2189–2198. [Google Scholar] [CrossRef]
- Liu, F.; Wang, X.; Li, Y.; Ren, M.; He, P.; Wang, L.; Xu, J.; Yang, S.; Ji, P. Dendrimer-modified gelatin methacrylate hydrogels carrying adipose-derived stromal/stem cells promote cartilage regeneration. Stem Cell Res. Ther. 2022, 13, 26. [Google Scholar] [CrossRef] [PubMed]
- Thissen, H.; Chang, K.-Y.; Tebb, T.A.; Tsai, W.-B.; Glattauer, V.; Ramshaw, J.A.M.; Werkmeister, J.A. Synthetic biodegradable microparticles for articular cartilage tissue engineering. J. Biomed. Mater. Res. Part A 2006, 77A, 590–598. [Google Scholar] [CrossRef] [PubMed]
- Hatamzadeh, M.; Sarvari, R.; Massoumi, B.; Agbolaghi, S.; Samadian, F. Liver tissue engineering via hyperbranched polypyrrole scaffolds. Int. J. Polym. Mater. Polym. Biomater. 2020, 69, 1112–1122. [Google Scholar] [CrossRef]
- Kojima, C.; Fusaoka-Nishioka, E.; Imai, T.; Nakahira, A.; Onodera, H. Dendrigraft polylysine coated-poly(glycolic acid) fibrous scaffolds for hippocampal neurons. J. Biomed. Mater. Res. Part A 2016, 104, 2744–2750. [Google Scholar] [CrossRef] [PubMed]
- Konieczynska, M.D.; Villa-Camacho, J.C.; Ghobril, C.; Perez-Viloria, M.; Blessing, W.A.; Nazarian, A.; Rodriguez, E.K.; Grinstaff, M.W. A hydrogel sealant for the treatment of severe hepatic and aortic trauma with a dissolution feature for post-emergent care. Mater. Horizons 2017, 4, 222–227. [Google Scholar] [CrossRef] [PubMed]
- Munder, A.; Moskovitz, Y.; Meir, A.; Kahremany, S.; Levy, L.; Kolitz-Domb, M.; Cohen, G.; Shtriker, E.; Viskind, O.; Lellouche, J.-P.; et al. Neuroligin-2-derived peptide-covered polyamidoamine-based (PAMAM) dendrimers enhance pancreatic β-cells’ proliferation and functions. MedChemComm 2019, 10, 280–293. [Google Scholar] [CrossRef]
- Kim, J.; Bax, D.; Murphy, R.; Best, S.; Cameron, R. Collagen Film Activation with Nanoscale IKVAV-Capped Dendrimers for Selective Neural Cell Response. Nanomaterials 2021, 11, 1157. [Google Scholar] [CrossRef]
- Agarwal, T.; Rustagi, A.; Das, J.; Maiti, T.K. PAMAM dendrimer grafted cellulose paper scaffolds as a novel in vitro 3D liver model for drug screening applications. Colloids Surf. B Biointerfaces 2018, 172, 346–354. [Google Scholar] [CrossRef]


























| Dendritic Polymer | Modification | Function | Reference |
|---|---|---|---|
| Trimesic acid core | Gly-Pro-Nleu and Gly-Nleu-Pro sequences as branches | Collagen Mimetic | [119] |
| G1-G3 PPI | - | Collagen Crosslinking | [124] |
| G0.5 PAMAM core | Gly-Pro-Nleu sequence as branches | Collagen Mimetic | [120] |
| G3.5 PAMAM | collagen model peptide, (Pro-Pro-Gly)5 | Collagen Mimetic | [121] |
| G4 PAMAM | (Pro-Pro-Gly)10 | Collagen Mimetic | [122] |
| G4 PAMAM | (Pro-Hyp-Gly)10 | Collagen Mimetic Hydrogel | [123] |
| G4 PAMAM | Ac-Val-Pro-Gly-Val-Gly | Elastin Mimetic | [125] |
| G3, G4, G5 PAMAM | Val-Pro-Gly-Val-Gly | Elastin Mimetic | [126] |
| G4 PAMAM | Val-Pro-Gly-Val-Gly Au Nps | Elastin Mimetic | [127] |
| Dendritic Polymer | Modification | Substrate | Cell Type | Ref. |
|---|---|---|---|---|
| G1 PAMAM | - | Collagen (cholecyst) | Murine 3T3 fibroblasts | [129] |
| G2 PAMAM | - | Collagen | Human conjunctival fibroblasts | [130] |
| G2 PPI | - | Bovine type-I collagen, human collagen (HC), and human extracellular matrix (hECM) | 3T3 fibroblast cell | [132] |
| dPAMAM transfection reagent | plasmid DNA | collagen-chondroitin sulfate scaffold | Mesenchymal stem cells | [113] |
| G1 PAMAM | pro-survival peptide analogs | Collagen | Stem cells | [131] |
| G5 PAMAM | Rhodamine | poly-lactide (PLA), miRNA mimics (premir-503) | HeLa Cells | [135] |
| G2 PAMAM | betamethasone sodium phosphate | Gelatin methacrylate | L929 cell line, anti-inflammatory | [136] |
| G2 PAMAM | Silk fibroin nanofibers | Fibroblasts cell line L929 | [134] | |
| G2 PAMAM | collagen-mimetic peptides, cell-binding sequence enzymatic cross-linking | Cell Aggregate | Hepatoma-liver | [148] |
| Dendrimer hydrazides | multi-cellular aggregates | Cell Aggregate | Human hepatoblastoma HepG2 cell line | [145] |
| G3 PAMAM | PEG acrylate photo–cross-linking | Hydrogel | RAW264.7 macrophages | [140] |
| G3 PPI hexadecaamine | Oleyl- polyethylene glycol | Cell Aggregate | C3A cells | [144] |
| Hyperbranched polyesters | Methacrylation photo–cross-linking | Hydrogel | NIH-3T3 fibroblasts | [141] |
| G4 PAMAM | RGD peptide | Cell Aggregate | NIH-3T3 fibroblasts | [146] |
| Hyperbranched PG | Phenol Groups Glucose | Hydrogel | Living Fibroblast cells | [142] |
| G3 PAMAM | Arg-Gly-Asp and PEG spacer | Cell Aggregate | Human hepatoblastoma HepG2 cell line | [147] |
| Dendritic Polymer | Modification | Substrate | Function | Ref. |
|---|---|---|---|---|
| 3.5, 4.5 PAMAM | - | - | Hydroxyapatite hemoglobin aquasomes | [154] |
| PPI | SDS | - | Hydroxyapatite nucleation | [155] |
| Dendritic Poly(L-lysine) Star Polycaprolactone | - | Hydroxyapatite | MG63 Cell Proliferation | [175] |
| G5.5 PAMAM | - | - | Hydroxyapatite nucleation | [159] |
| G1 to G4 PAMAM | - | Hydroxyapatite nucleation | [140] | |
| PAMAM | Carboxylic/polyhydroxy terminated | - | Hydroxyapatite nucleation | [139] |
| G1.5 PAMAM | Dexamethasone | Carboxymethyl chitosan | Human osteoblast-like cells/Rat bone marrow stromal cells proliferation | [187] |
| PEI 25000 | - | - | Calcium phosphate nucleation | [165] |
| G1.5 PAMAM | Dexamethasone carboxymethyl chitosan | Hydroxyapatite or starch–polycaprolactone scaffolds | Osteogenic differentiation rat Bone marrow stromal cells | [188] |
| G5, G6, G7 PAMAM | - | - | Mesenchymal stem cells osteogenic differentiation | [184] |
| G1.5 PAMAM | dexamethasone carboxymethyl chitosan | hydroxyapatite or starch–polycaprolactone scaffolds | Rat bone marrow stromal cells proliferation | [189] |
| G4 PPI | - | - | Hydroxyapatite nucleation | [162] |
| G5 PAMAM | PEG | Ti | human bone mesenchymal stem cells proliferation | [174] |
| PEI 25000 | Ti | Hydroxyapatite nucleation | [166] | |
| G2 PAMAM | Glutamic Acid | Gelatin Gel | Hydroxyapatite nucleation | [169] |
| G1.5 PAMAM | Carboxymethyl chitosan, dexamethasone | - | rat bone marrow stromal cells differentiation to osteoblasts | [190] |
| G4 PAMAM | Hydroxyapatite | Hydroxyapatite nucleation | [172] | |
| Poly(1-lysine) dendrons | Phosphoserine | Etched titanium oxide | Calcium phosphate nucleation MG63 and SAOS-2 osteoblast-like cells proliferation | [191] |
| G4 PPI | Ti | Hydroxyapatite nucleation | [167] | |
| G2, G3 PPI | MWCNTs | human osteosarcoma (MG-63) cell line | [156] | |
| G4 PAMAM | PEG, Arg-Gly-Asp-(D-Tyr)-cysteine (RGDyC) | poly(lactic acid)-b-poly(ethylene glycol)-b-poly(lactic acid) | Mouse bone marrow mesenchymal stem cells differentiation for bone formation | [194] |
| Dendronized PAMAM | tri-phosphate or bis-phosphonate peripheral groups | Hydroxyapatite nucleation | [170] | |
| Poly(Epsilon-Lysine) Hyperbranched Dendrons | Phosphoserine | Calcium Phosphate Gels | Mesenchymal stem cell differentiation for bone cell stimulation | [193] |
| G2, G4, G6 PAMAM-succinic acid 1,12-diaminododecane core | Gold Nanoparticles | - | Hydroxyapatite nucleation | [157] |
| Poly(epsilon-lysine) dendrons | Phosphoserine | Ti | Murine osteoblastic MC3T3 cells and primary bone marrow cells proliferation | [192] |
| Bifunctional dendrimers with cyclotriphosphazene core | Thioctic acid | Gold surfaces | Proliferation of human osteoblasts | [179] |
| G5 PAMAM | Arg-Gly-Asp, Hyaluronic acid | - | Bone marrow stem cells proliferation | [180] |
| Poly(Epsilon-Lysine) Hyperbranched Dendrons | phosphoserine | Titanium implants | Osseointegration | [200] |
| G4.0 PAMAM | Maleimide-PEG-succinimidyl carbonate ester, methoxy-PEG-succinimidyl carbonate ester | 3, 4-dihydroxy-L-phenylalanine DOPAD-terminated 8-armed PEG | Mouse bone marrow mesenchymal stem cells | [204] |
| G5 PAMAM | RGD, YIGSR, and IKVAV peptides | - | Bone marrow stem cells, pheochromocytoma (PC12) cells proliferation | [186] |
| Hyperbranched aliphatic polyester | Polythiophene, poly(ε-caprolactone) | - | Mouse osteoblast MC3T3-E1 proliferation | [182] |
| PEI 5000 | Hydroxyapatite | Chitosan | In vivo bone formation | [163] |
| G4 PAMAM | Amino acids | Luciferase reporter plasmid DNA | Human adipose-derived mesenchymal stem cells (AD-MSCs) osteogenic-chondrogenic differentiation | [185] |
| G1 PAMAM | Arg-Gly-Asp tripeptides | Polystyrene | Human bone mesenchymal stem cells | [177] |
| G1-G5 PAMAM Dendrons | Triethoxysillyl focal point | - | Hydroxyapatite nucleation | [173] |
| Dendritic Amphiphile | cholesterol | - | Calcium Phosphate Mineralization | [158] |
| PEI 5000 | Hydroxyapatite | Chitosan | In vivo bone formation | [198] |
| G1 PAMAM | Alginate | - | MC3T3-E1 pre-osteoblasts proliferation | [181] |
| G3 poly(epsilon-lysine) dendrons | Phosphoserine | Strontium-doped hydroxyapatite gel | Macrophage osteogenic differentiation, In vivo bone formation | [202] |
| G5 PAMAM | 8arm-PEG-SH | - | Rat bone marrow mesenchymal stem cells osteogenic differentiation | [195] |
| PAMAM G1/G2/G3 | carbon nanotubes (CNTs) | nanostructured hydroxyapatite | osteoblast-like MG 63 cell line | [183] |
| G5 PAMAM | CO2H- or CH3-NH2 groups | Silicon | MG-63 osteoblastic cells | [176] |
| G1.5, G2.5, G3.5 PAMAM | chitosan, ketoprofen | Hydroxyapatite | [164] | |
| Amide-based amino terminal dendrons | Arg-Gly-Asp | Ti | Human osteoblastic cells | [178] |
| G3 poly(epsilon-lysine) dendron | phosphoserine | Biphasic calcium phosphate | Biomineralization and stem cell osteogenic differentiation bone marrow stromal cells proliferation | [203] |
| PEI 5000 | Hydroxyapatite | Chitosan | In vivo bone formation | [199] |
| G3 PAMAM | Sr Hydroxyapatite, Curcumin | d-MWCNT | Human osteoblast-like MG-63 cells, proliferation, differentiation | [197] |
| G5 PAMAM | VE-cadherin | Thiolated hyaluronic acid | Human umbilical cord mesenchymal stem cells differentiation | [196] |
| Dendritic Polymer | Modification | Substrate | Function | Ref. |
|---|---|---|---|---|
| G5 PAMAM | Arg-Gly Asp | - | Dermal microvessel endothelial, human vascular endothelial, odontoblast-like MDPC-23 cells | [206] |
| G5 PAMAM | Fluorescein isothiocyanate Arg-Gly Asp | - | Dental pulp cells differentiation mouse odontoblast-like MDPC-23 cells | [207] |
| G3, G4 PAMAM-COOH | Carboxylic acid functionalization | Collagen fibrils | Dentin remineralization | [210] |
| G3.5 PAMAM | Alendronate | Demineralized enamel | Enamel remineralization | [252] |
| G4 PAMAM-COOH | Butanedioic anhydride | Ferric chloride solution | Aggregates with a microribbon structure | [251] |
| PAMAM G3 | Carboxylic acid functionalization | Demineralized enamel | Enamel remineralization | [245] |
| G1 PAMAM Dendron | Aspartic acid, hexadecyl chain at the focal point | Biomimetic amelogenin nanospheres | Hydroxyapatite orientation Enamel | [250] |
| G4 PAMAM | Dimethyl phosphate | Demineralized enamel | Enamel remineralization | [249] |
| G3 PAMAM-NH2 | Demineralized dentin | Dentin remineralization | [217] | |
| G4 PAMAM-COOH | Triclosan | Demineralized dentin | Dentin remineralization, anti-bacterial | [239] |
| G4 PAMAM | Demineralized dentinal tubules | Dentin remineralization | [215] | |
| G3 PAMAM-NH2 | Type-I collagen fibrils | Mineralization of collagen fibrils | [219] | |
| G2 G4-PAMAM-OH | Demineralized dentin | Dentin remineralization | [212] | |
| PAMAM-COOH | Ca(OH)2 | Demineralized dentin | Dentin remineralization | [221] |
| G4.5 PAMAM-COOH | Demineralized enamel | Enamel remineralization | [246] | |
| G2 PAMAM | Glutaraldehyde | Demineralized dentin | Dentin remineralization | [213] |
| G3 PAMAM | Phosphorylation polyacrylic acid | Demineralized dentin | Dentin remineralization | [233] |
| G4 PAMAM | Phosphorylation | Demineralized dentin | Dentin remineralization | [234] |
| G3 PAMAM | Amorphous calcium phosphate | Demineralized dentin | Dentin remineralization | [223] |
| G3.5 PAMAM | Demineralized dentin | In vivo Dentin remineralization | [211] | |
| PAMAM-COOH | Nano-hydroxyapatite | Demineralized dentin | Dentin remineralization | [237] |
| PAMAM-OH, PAMAM-COOH, PAMAM-NH2 | Demineralized dentin | Dentin remineralization | [218] | |
| G3 PAMAM | Nanoparticles of amorphous calcium phosphate (NACP) | Demineralized dentin | Dentin remineralization | [225] |
| G3-PAMAM-NH2 | Nanoparticles of amorphous calcium phosphate (NACP) | Demineralized dentin | Dentin remineralization in an acidic solution | [226] |
| PAMAM 3.5 | NACP resin | Demineralized dentin | Dentin remineralization | [227] |
| PAMAM | Demineralized dentin | Dentin remineralization | [216] | |
| G3 PAMAM | bioactive multifunctional composite | Demineralized dentin | Dentin remineralization | [230] |
| G3 PAMAM | Glutaraldehyde | Demineralized dentin | Dentin remineralization | [214] |
| G3 PAMAM-NH2 | Amorphous calcium phosphate nanoparticles | Ethoxylated bisphenol A, dimethacrylate pyromellitic glycerol dimethacrylate resin | Dentin remineralization | [228] |
| Phosphorylated G3, G4 PAMAM | Apigenin | Demineralized dentin | Dentin remineralization, anti-bacterial | [240] |
| G4 PAMAM | Mesoporous bioactive glass nanoparticles | Dentin remineralization | [238] | |
| G4 PAMAM | SN15 salivary statherin protein-inspired peptide NACP resin | Demineralized dentin | Enamel remineralization | [253] |
| PAMAM | Nanoparticles of amorphous calcium phosphate | Demineralized dentin | Dentin remineralization | [222] |
| G3 PAMAM-COOH | Nanoparticles of amorphous calcium phosphate | Demineralized dentin | Dentin remineralization | [224] |
| PAMAM-NH2, PAMAM-COOH, PAMAM-OH | Enamel | Enamel remineralization | [247] | |
| G5 PAMAM-NH2, PAMAM-COOH | Demineralized enamel | Enamel remineralization | [248] | |
| PAMAM-PO3H2 | Demineralized dentin and type I collagen matrix | Hydroxyapatite, Dentin remineralization | [232] | |
| G3 PAMAM | Pulpine | Demineralized dentin | Dentin remineralization, pulp tissue repair | [243] |
| PAMAM | Honokiol-loaded | Demineralized dentin | Enamel remineralization, anti-bacterial | [254] |
| G4 PAMAM-COOH | Chlorhexidine | Demineralized dentin | Dentin remineralization | [242] |
| G3 PAMAM-NH2 | Nanoparticles of amorphous calcium phosphate, pyromellitic glycerol dimethacrylate, ethoxylated bisphenol A dimethacrylate resin | Demineralized dentin | Dentin remineralization in an acidic solution after severe fluid challenges | [229] |
| G4 PAMAM- PO3H2 G4 PAMAM-COOH | Demineralized dentin | Dentin biomimetic remineralization and dentinal tubule occlusion | [235] | |
| G4 PAMAM-COOH | Amorphous calcium phosphate nanofillers, chlorhexidine | Demineralized dentin | Dentin remineralization, anti-bacterial | [241] |
| PAMAM- PO3H2 | Dental pulp stem cells | [208] | ||
| PAMAM- PO3H2 PAMAM-COOH | Collagen fibrils | Mineralization of type I collagen fibrils | [236] | |
| PAMAM–COOH | Nano-sized amorphous calcium phosphate | Collagen fibrils | Mineralization of dentin type I collagen fibrils | [220] |
| Dendritic Polymer | Modification | Substrate | Function | Ref. |
|---|---|---|---|---|
| PEG core methacrylated poly(glycerol succinic acid) | Cross-linking | - | Cornea wound healing | [255] |
| Lysine-based peptide dendrons | Poly(ethylene glycol dialdehyde) cross-linking | - | Cataract Surgeries | [259] |
| G1-PGLSAMA)2-PEG: polyethylene glycol, succinic acid glycerol, methacrylic acid | methacrylate ester photo–cross-linking | - | Cornea wound healing | [256] |
| G1-PGLSAMA)2-PEG: polyethylene glycol, succinic acid glycerol, methacrylic acid | methacrylate ester photo–cross-linking | - | Cornea wound healing | [257] |
| G1-PGLSA-MA)2-PEG3400) poly(ethylene glycol), succinic acid, glycerol, methacrylic acid, cysteine dendron | methacrylate ester photo–cross-linking, Self-Gelling | - | securing laser in situ keratomileuses (LASIK) flaps | [260] |
| Cysteine-terminated lysine dendron | PEG diester-aldehyde-pseudo proline peptide ligation | - | Corneal transplant | [251] |
| G2 PPI | Collagen | Human corneal epithelial cells proliferation | [265] | |
| G2 PPI | YIGSR cell adhesion peptide | Collagen | Human corneal epithelial cells proliferation | [268] |
| G2 PPI | Fibroblast growth factor, heparin | Collagen | Cornea wound healing | [266] |
| Lysine cysteine dendritic polymer | PEG-butyric dialdehyde | Hydrogel | Sealing of clear corneal cataract incisions | [261] |
| PEG core dendritic polyesters | Methacryliation | - | Corneal laceration repair | [258] |
| Lys3Cys4 dendritic cross-linker | Propionaldehyde, butyraldehyde, 2-oxoethyl succinate PEG | Cornea wound healing | [262] | |
| Poly(ethylene glycol) core succinic acid and glycerol branches | Cell adhesion ligand RGD | 2-hydroxyethyl methacrylate hydrogel type I collagen | Corneal fibroblasts, corneal epithelial cell proliferation | [264] |
| G2 PPI | Heparin-binding fibroblast growth factor, heparin | Collagen | Corneal wound healing-human corneal epithelial cells proliferation | [267] |
| G4 PAMAM | Val-Pro-Gly-Val-Gly | Human adipose-derived mesenchymal stem cells differentiation to Human Corneal Endothelial Cells | [269] |
| Dendritic Polymer | Modification | Substrate | Function | Ref. |
|---|---|---|---|---|
| Dendritic Thioester | PEG cross-linking | - | Wound closure | [271] |
| G3-G6 PG core hyperbranched 2,2-bis(hydroxymethyl) propionic acid | Tris [2-(3-mercapto propionyl oxy)ethyl] isocyanurate | Surgical mesh | Soft tissue adhesive patches | [273] |
| Pegylated lysine dendron | Poly(ethylene glycol disuccinimidyl valerate) | Hydrogel | Wound closure | [275] |
| Lysine-based dendron | Thioester with PEG cross-linker | - | Burn Wounds | [274] |
| G5 PAMAM | Acetylation and conjugation with protein | Stem cell | Wound closure | [277] |
| Peptide (arginine-lysine) polycationic dendrimers | - | Progenitor cell biological bandages | Human umbilical vein endothelial cells proliferation wound healing, antibacterial | [276] |
| G4 PAMAM | - | Gelatin scaffolds | Keratinocytes, fibroblasts proliferation dermal skin tissue engineering | [278] |
| G1 PAMAM silylated dendron | Collagen | ZnO nanoparticles | Human Epidermal Keratinocytes Wound healing | [281] |
| G3 PAMAM | Triethoxysillyl focal point | Graphene oxide, reduced graphene, carbon nanotube, and fullerene | Collagen wound closure | [282] |
| Poly(L-lysine) dendrigrafts | PEG | - | Human dermal fibroblasts proliferation | [270] |
| G3, G5 PAMAM, G2, G3, G5 PPI | - | Poly (L-lactic acid) scaffolds | Human dermal fibroblast cells, higher attachment, and homogeneous spread morphology | [279] |
| Hyperbranched polymer with thiol end groups | Benzaldehyde-terminated PEG (PEGCHO) | - | Wound Closure | [272] |
| G3 PAMAM | Triethoxysillyl focal point | ZnO, TiO2, Fe3O4, CeO2, and SiO2 | Collagen wound closure | [280] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arkas, M.; Vardavoulias, M.; Kythreoti, G.; Giannakoudakis, D.A. Dendritic Polymers in Tissue Engineering: Contributions of PAMAM, PPI PEG and PEI to Injury Restoration and Bioactive Scaffold Evolution. Pharmaceutics 2023, 15, 524. https://doi.org/10.3390/pharmaceutics15020524
Arkas M, Vardavoulias M, Kythreoti G, Giannakoudakis DA. Dendritic Polymers in Tissue Engineering: Contributions of PAMAM, PPI PEG and PEI to Injury Restoration and Bioactive Scaffold Evolution. Pharmaceutics. 2023; 15(2):524. https://doi.org/10.3390/pharmaceutics15020524
Chicago/Turabian StyleArkas, Michael, Michail Vardavoulias, Georgia Kythreoti, and Dimitrios A. Giannakoudakis. 2023. "Dendritic Polymers in Tissue Engineering: Contributions of PAMAM, PPI PEG and PEI to Injury Restoration and Bioactive Scaffold Evolution" Pharmaceutics 15, no. 2: 524. https://doi.org/10.3390/pharmaceutics15020524