Manipulations of Oral Medications in Paediatric Neurology and Oncology Care at a Swedish University Hospital: Health Professionals’ Attitudes and Sources of Information
Abstract
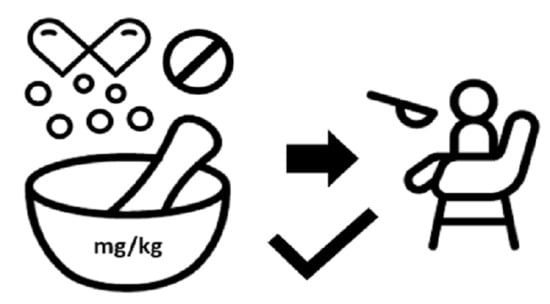
:1. Introduction
2. Materials and Methods
2.1. Prevalence of Manipulated Dosage Forms
- (1)
- Admission to ward A or to ward B.
- (2)
- Patients aged 18 months–18 years. This inclusion criterium was set to also include young children, based on the finding that children, even as young as one year, may accept a solid oral dosage form [11].
- (3)
- Patients who were administered oral medications.
2.2. Ward Observational Study
2.3. Survey Study
3. Results
3.1. Prevalence of Manipulated Dosage Forms
3.2. Ward Observational Study
3.3. Survey Study
3.3.1. Paediatricians’ Perspective
3.3.2. Nurses’ Perspective
4. Discussion
4.1. Prevalence of Manipulated Dosage Forms
4.2. Ward Observational Study
4.3. Survey Study
4.4. General Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Kearns, G.L.; Abdel-Rahman, S.M.; Alander, S.W.; Blowey, D.L.; Leeder, J.S.; Kauffman, R.E. Developmental Pharmacology—Drug Disposition, Action, and Therapy in Infants and Children. N. Engl. J. Med. 2003, 349, 1157–1167. [Google Scholar] [CrossRef]
- COM(2017)626—State of Paediatric Medicines in the EU—10 Years of the EU Paediatric Regulation—EU Monitor. Available online: https://www.eumonitor.eu/9353000/1/j9vvik7m1c3gyxp/vkishwm1efzz (accessed on 21 June 2021).
- Rei Bolislis, W.; Bejeuhr, G.; Benzaghou, F.; Corriol-Rohou, S.; Herrero-Martinez, E.; Hildebrand, H.; Hill-Venning, C.; Hoogland, H.; Johnson, C.; Joos, A.; et al. Optimizing Pediatric Medicine Developments in the European Union Through Pragmatic Approaches. Clin. Pharmacol. Ther. 2021, 110, cpt.2152. [Google Scholar] [CrossRef] [PubMed]
- Barker, C. Modric Manipulation of Drugs Required in Children—A Guide for Health Professionals. Available online: http://www.alderhey.nhs.uk/wp-content/uploads/MODRIC_Guideline_FULL-DOCUMENT.pdf (accessed on 5 September 2021).
- Bjerknes, K.; Bøyum, S.; Kristensen, S.; Brustugun, J.; Wang, S. Manipulating Tablets and Capsules given to Hospitalised Children in Norway Is Common Practice. Acta Paediatr. 2017, 106, 503–508. [Google Scholar] [CrossRef]
- van der Vossen, A.C.; Al-Hassany, L.; Buljac, S.; Brugma, J.-D.; Vulto, A.G.; Hanff, L.M. Manipulation of Oral Medication for Children by Parents and Nurses Occurs Frequently and Is Often Not Supported by Instructions. Acta Paediatr. 2019, 108, 1475–1481. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zahn, J.; Hoerning, A.; Trollmann, R.; Rascher, W.; Neubert, A. Manipulation of Medicinal Products for Oral Administration to Paediatric Patients at a German University Hospital: An Observational Study. Pharmaceutics 2020, 12, 583. [Google Scholar] [CrossRef]
- Nunn, A.; Richey, R.; Shah, U.; Barker, C.; Craig, J.; Peak, M.; Ford, J.; Turner, M. Estimating the Requirement for Manipulation of Medicines to Provide Accurate Doses for Children. Eur. J. Hosp. Pharm. 2013, 20, 3. [Google Scholar] [CrossRef]
- Richey, R.H.; Shah, U.U.; Peak, M.; Craig, J.V.; Ford, J.L.; Barker, C.E.; Nunn, A.J.; Turner, M.A. Manipulation of Drugs to Achieve the Required Dose Is Intrinsic to Paediatric Practice but Is Not Supported by Guidelines or Evidence. BMC Pediatr. 2013, 13, 81. [Google Scholar] [CrossRef] [Green Version]
- European Medicines Agency: EMA/CHMP/QWP/805880/2012—Guideline on Pharmaceutical Development of Medicines for Paediatric Use 2013. Available online: https://www.ema.europa.eu/en/documents/scientific-guideline/guidelinepharmaceutical-development-medicines-paediatric-use_en.pdf (accessed on 5 September 2021).
- van Riet-Nales, D.A.; de Neef, B.J.; Schobben, A.F.A.M.; Ferreira, J.A.; Egberts, T.C.G.; Rademaker, C.M.A. Acceptability of Different Oral Formulations in Infants and Preschool Children. Arch. Dis. Child. 2013, 98, 725–731. [Google Scholar] [CrossRef] [Green Version]
- Cambio COSMIC-Cambio COSMIC Health Care Information System. Cambio. Available online: https://www.cambiogroup.com/our-solutions/cambio-cosmic/ (accessed on 5 September 2021).
- WHOCC—Home. Available online: https://www.whocc.no/ (accessed on 5 September 2021).
- Kelley, K.; Clark, B.; Brown, V.; Sitzia, J. Good Practice in the Conduct and Reporting of Survey Research. Int. J. Qual. Health Care 2003, 15, 261–266. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Senaste Version av HSLF-FS 2017:37 Socialstyrelsens Föreskrifter Och Allmänna Råd om Ordination och Hantering av Läkemedel i Hälso- och Sjukvården—Konsoliderad. Available online: https://www.socialstyrelsen.se/regler-och-riktlinjer/foreskrifter-och-allmanna-rad/konsoliderade-foreskrifter/201737-om-ordination-och-hantering-av-lakemedel-i-halso--och-sjukvarden/ (accessed on 11 January 2021).
- FASS Vårdpersonal—Startsida. Available online: http://www.fass.se/LIF/startpage;jsessionid=_9roI_T-cN0Xs9LtLGH6Nc1diSXzXZb-Ur67WwvH0dIFpN2-kiEO!-2033438433?userType=0 (accessed on 5 April 2016).
- Sväljes Hela Apoteket AB. 2013. Available online: https://www.apoteket.se/globalassets/svaljes-hela_mars-2013.pdf (accessed on 5 April 2016).
- Läkemedelsverket Enteral Läkemedelsadministrering—Nytt Kunskapsstöd_webb.Pdf. Available online: https://lakemedelsverket.se/upload/halso-och-sjukvard/behandlingsrekommendationer/Enteral%20l%C3%A4kemedelsadministrering%20-%20nytt%20kunskapsst%C3%B6d_webb.pdf (accessed on 5 April 2016).
- White, R.; Bradnam, V. Handbook of Drug Administration via Enteral Feeding Tubes, 3rd ed.; Pharmaceutical Press: London, UK, 2015; ISBN 978-0-85711-162-3. [Google Scholar]
- ePed Best Practice. Available online: https://eped.se/best-practice/ (accessed on 17 June 2021).
- HighAlert2018-Acute-Final.Pdf. Available online: https://www.ismp.org/sites/default/files/attachments/2018-08/highAlert2018-Acute-Final.pdf (accessed on 9 June 2021).
- Nydert, P.; Kumlien, A.; Norman, M.; Lindemalm, S. Cross-Sectional Study Identifying High-Alert Substances in Medication Error Reporting among Swedish Paediatric Inpatients. Acta Paediatr. 2020, 109, 2810–2819. [Google Scholar] [CrossRef] [PubMed]
- Andersson, Å.; Lindemalm, S.; Eksborg, S. Dividing the Tablets for Children—Good or Bad? Pharm. Methods 2016, 7, 1. [Google Scholar] [CrossRef]
- Richey, R.H.; Hughes, C.; Craig, J.V.; Shah, U.U.; Ford, J.L.; Barker, C.E.; Peak, M.; Nunn, A.J.; Turner, M.A. A Systematic Review of the Use of Dosage Form Manipulation to Obtain Required Doses to Inform Use of Manipulation in Paediatric Practice. Int. J. Pharm. 2017, 518, 155–166. [Google Scholar] [CrossRef] [Green Version]
- Brustugun, J.; Notaker, N.; Paetz, L.H.; Tho, I.; Bjerknes, K. Adjusting the Dose in Paediatric Care: Dispersing Four Different Aspirin Tablets and Taking a Proportion. Eur. J. Hosp. Pharm. 2021, 28, 76–82. [Google Scholar] [CrossRef] [Green Version]
- The Committee of Ministers of the Council of Europe Resolution CM/Res(2016)2 on Good Reconstitution Practices in Health Care Establishments for Medicinal Products for Parenteral Use. Available online: https://www.edqm.eu/sites/default/files/resolution_cm_res_2016_2_good_reconstitution_practices_in_health_care_establishments_for_medicinal_products_for_parenteral_use_.pdf (accessed on 5 September 2021).
- Garnemark, C.; Lilja, L.; Kindblom, J. Drug treatment of hospitalized children can become more secure. Better decision support, better customized IT systems, and a better working environment needed. Lakartidningen 2016, 113, DU9C. [Google Scholar]
- Kimland, E.; Nydert, P.; Odlind, V.; Bottiger, Y.; Lindemalm, S. Paediatric Drug Use with Focus on Off-Label Prescriptions at Swedish Hospitals—A Nationwide Study. Acta Paediatr. 2012, 101, 772–778. [Google Scholar] [CrossRef] [Green Version]
- Teigen, A.; Wang, S.; Truong, B.T.; Bjerknes, K. Off-Label and Unlicensed Medicines to Hospitalised Children in Norway. J. Pharm. Pharmacol. 2017, 69, 432–438. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moustaka, Ε.; Constantinidis, T.C. Sources and Effects of Work-Related Stress in Nursing. Health Sci. J. 2010, 4, 7. [Google Scholar]
- Measuring the Four Dimensions of Digital Health|HIMSS Analytics—Asia Pacific. Available online: https://www.himssanalytics.org/asia-pacific/news/measuring-four-dimensions-digital-health (accessed on 17 June 2021).
- Maaskant, J.M.; Vermeulen, H.; Apampa, B.; Fernando, B.; Ghaleb, M.A.; Neubert, A.; Thayyil, S.; Soe, A. Interventions for Reducing Medication Errors in Children in Hospital. Cochrane Database Syst. Rev. 2015. [Google Scholar] [CrossRef] [PubMed]
- Naseralallah, L.M.; Hussain, T.A.; Jaam, M.; Pawluk, S.A. Impact of Pharmacist Interventions on Medication Errors in Hospitalized Pediatric Patients: A Systematic Review and Meta-Analysis. Int. J. Clin. Pharm. 2020, 42, 979–994. [Google Scholar] [CrossRef]
- Costello, J.L.; Torowicz, D.L.; Yeh, T.S. Effects of a Pharmacist-Led Pediatrics Medication Safety Team on Medication-Error Reporting. Am. J. Health-Syst. Pharm. 2007, 64, 1422–1426. [Google Scholar] [CrossRef]
- Preis, M.; Öblom, H. 3D-Printed Drugs for Children—Are We Ready Yet? AAPS PharmSciTech 2017, 18, 303–308. [Google Scholar] [CrossRef]
- Lind, J.; Kälvemark Sporrong, S.; Kaae, S.; Rantanen, J.; Genina, N. Social Aspects in Additive Manufacturing of Pharmaceutical Products. Expert Opin. Drug Deliv. 2017, 14, 927–936. [Google Scholar] [CrossRef] [PubMed]
- Araújo, M.; Sa-Barreto, L.; Gratieri, T.; Gelfuso, G.; Cunha-Filho, M. The Digital Pharmacies Era: How 3D Printing Technology Using Fused Deposition Modeling Can Become a Reality. Pharmaceutics 2019, 11, 128. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Öblom, H.; Zhang, J.; Pimparade, M.; Speer, I.; Preis, M.; Repka, M.; Sandler, N. 3D-Printed Isoniazid Tablets for the Treatment and Prevention of Tuberculosis—Personalized Dosing and Drug Release. AAPS PharmSciTech 2019, 20, 52. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Walsh, J.; Schaufelberger, D.; Iurian, S.; Klein, S.; Batchelor, H.; Turner, R.; Gizurarson, S.; Boltri, L.; Alessandrini, E.; Tuleu, C.; et al. Path towards Efficient Paediatric Formulation Development Based on Partnering with Clinical Pharmacologists and Clinicians, a C4c Expert Group White Paper. Br. J. Clin. Pharmacol. 2021. [Google Scholar] [CrossRef]
- Raijada, D.; Wac, K.; Greisen, E.; Rantanen, J.; Genina, N. Integration of Personalized Drug Delivery Systems into Digital Health. Adv. Drug Deliv. Rev. 2021, 176, 113857. [Google Scholar] [CrossRef]
- Reber, E.; Messerli, M.; Stanga, Z.; Mühlebach, S. Pharmaceutical Aspects of Artificial Nutrition. J. Clin. Med. 2019, 8, 2017. [Google Scholar] [CrossRef] [Green Version]


| Patient Characteristics | Ward A n (%) | Ward B n (%) |
|---|---|---|
| Included Day 1 Patients | 232 | 166 |
| Excluded (<1.5 years) | 10 (4%) | 15 (9%) |
| Excluded (No oral meds) | 21 (9%) | 22 (13%) |
| Qualified Day 1 Patients | 201 | 129 |
| Unique Patients | 49 | 30 |
| Female | 88 (43.8%) | 55 (42.6%) |
| Male | 113 (56.2%) | 74 (57.4%) |
| Toddlers (1.5–2 years) | 3 (1.5%) | 12 (9.3%) |
| Pre-School (2–5 years) | 46 (22.9%) | 60 (46.5%) |
| Schoolchildren (6–11 years) | 45 (22.4%) | 35 (27.1%) |
| Adolescents (12–18 years) | 107 (53.2%) | 22 (17.1%) |
| Age (years), median (min/max) | 12.9 (1.6–18.1) | 5.8 (1.4–17.2) |
| Weight (kg), median (min/max) | 38.8 (9.2–109) | 17 (6.7–105) |
| Enteral feeding tube present | 53 (26.4%) | 40 (31%) |
| Self administration 2 | 24 (11.9%) | 13 (10.1%) |
| Living in Region Uppsala | 70 (34.8%) | 70 (54.3%) |
| Medications Orders | Ward A n(%) | Ward B n(%) |
| Number of active orders (excluding PRN etcetera) | 1271 | 771 |
| Number of orders for oral delivery (% of active) | 791 (62%) | 488 (63%) |
| Administered oral doses | 895 | 463 |
| To Toddlers (1.5–2 years) | 2 (0.2%) | 23 (5%) |
| To Pre-School (2–5 years) | 11 (1.2%) | 98 (21.2%) |
| To Schoolchildren (6–11 years) | 65 (7.3%) | 204 (44.1%) |
| To Adolescents (12–18 years) | 817 (91.3%) | 138 (29.8%) |
| Manipulated | 117 (13.1%) | 94 (20.3%) |
| -due to inappropriate strength | 97 (10.8%) | 42 (9.1%) |
| -due to tube administration | 20 (2.2%) | 52 (11.2%) |
| for Toddlers (1.5–2 years) | 2 (100%) | 14 (60.9%) |
| for Pre-School (2–5 years) | 3 (27.3%) | 54 (55.1%) |
| for Schoolchildren (6–11 years) | 25 (38.5%) | 11 (5.4%) |
| for Adolescents (12–18 years) | 87 (10.6%) | 15 (10.9%) |
| ATC | Active | Dosage Form | Part | Product | SmPC Comment | Ward |
|---|---|---|---|---|---|---|
| A02BC05 | Esomeprazole | Sachet | 0.5 | Nexium 10 mg | Missing info | B |
| A06AD65 | Macrogol combination | Sachet | 0.5 | Movicol | Missing info | A/B |
| A12AA06 | Calcium | Effervescent | 0.5 | Calcium-Sandoz | Information regarding divisibility is missing | A |
| B02AA02 | Tranexamic acid | Effervescent | 0.5 | Cyklokapron 1 g | Information regarding divisibility is missing | A |
| C07AB02 | Metoprolol | MR * tablet | 0.5 | Metoprolol orion 50 mg | Information regarding divisibility is missing | A |
| C08CA02 | Felodipine | MR * tablet | 0.5 | Felodipin TEVA | Cannot be divided | B |
| C09AA02 | Enalapril | Tablet | 0.5 | Enalapril krka 5 mg | Supported. Can be split in two halves | A |
| H02AB06 | Prednisolone | Tablet | 0.5 | Prednisolon 10 mg | Supported. Can be split in two halves | A |
| H02AB09 | Hydrocortisone | Tablet | 0.25 + 0.75 | Hydrokortison 10 mg | Can only be split in half | A |
| H03AA01 | Levothyroxine | Tablet | 0.5 | Levaxin 25 µg | Should not be divided | A |
| J01DB05 | Cefadroxil | Tablet | 0.25 | Cefadroxil Sandoz 1 g | Information regarding divisibility is missing | A |
| J05AB01 | Aciclovir | Tablet | 0.5 | Aciclovir 200 mg | Missing info | A |
| L01BB02 | Mercaptopurine | Tablet | 0.75 | Puri-nethol 50 mg | Cannot be divided. Cannot be crushed. | A |
| L01BB03 | Tioguanine | Tablet | 0.5 | Lanvis 40 mg | Can be divided only to ease swallowing | A |
| L04AA10 | Sirolimus | Tablet | 0.5 | Rapamune 1 mg | Cannot be divided. Cannot be crushed. | A |
| M03BX01 | Baclofen | Tablet | 0.5 | Baklofen alternova 10 mg | Supported. Can be split in two halves | A |
| M03BX01 | Baclofen | Tablet | 0.25 | Baklofen 25 mg | Can only be split in half | B |
| M03BX01 | Baclofen | Tablet | 0.5 | Lioresal 10 mg | Information regarding divisibility is missing | B |
| N02AA01 | Morphine | Tablet | 0.5 | Morfin meda 10 mg | Can be divided only to ease swallowing | A |
| N02AA01 | Morphine | Tablet | 0.5 | Morfin Alternova 10 mg | Can be divided into two equal parts. | B |
| N02BE01 | Paracetamol | Tablet | 0.5 | Alvedon 500 mg | Supported. Can be split in two halves | A |
| N03AB02 | Phenytoin | Tablet | 0.75 + 0.5 | Fenantoin Meda 100 mg | Can be divided only to ease swallowing | B |
| N03AF02 | Oxcarbazepine | Tablet | 0.5 | Trileptal 600 mg | Can be divided only to ease swallowing | B |
| N03AG01 | Valproic acid | MR * capsule | 0.5 | Orfiril long 150 mg | Can be opened, but not possible to get accurate dose | B |
| N03AG04 | Vigabatrin | Sachet | 0.5 | Sabrilex 500 mg | Missing info | B |
| N03AX11 | Topiramate | Tablet | 0.5 | Topiramat 1A Farma | To be swallowed whole | B |
| N05BA09 | Clobazam | Tablet | 0.75 + 0.5 | Frisium Sanofi 10 mg | Information regarding divisibility is missing | B |
| N05CF01 | Zopiclone | Tablet | 0.5 | Imovane 5 mg | Information regarding divisibility is missing | A |
| N06AA09 | Amitriptyline | Tablet | 0.5 | Amitriptylin 10 mg | Swallowed whole with half a glass of water | A |
| N07BC02 | Methadone | Tablet | 0.5 | Metadon Abcur 5 mg | Supported. Can be split in two halves | A |
| Accuracy of Dose | When preparing ¼ of a tablet, the tablet is divided twice using tablet splitter and eye measurement, making the result inaccurate with uneven, crumbly parts. Another approach for preparing ¼ of a tablet was to dissolve the tablet in 10 mL of water and administer 2.5 mL to the patient. When questioned if the nurse reflected upon solubility when dissolving a tablet or a sachet in water and extracting a fraction of it, the nurse did not have a clear answer. There were scales in both ward medication rooms, but they were not used for purpose of, e.g., dividing sachet content due to lack of precision. |
| Cross Contamination | The splitting/crushing devices were seldom cleaned properly, largely due to the construction of the device. Crushing of tablets containing hazardous medications was performed in safety cabinets and afterwards handled in closed containers (e.g., oral/enteral syringes). |
| Disposing of unused medication | When only a part of a tablet or sachet was used, the rest was discarded because there were no appropriate stability data or suitable containers. |
| Ease of Administration | One of the nurses had noticed positive effects of using tablet coating devices (e.g., the Medcoat® product). Some children have a hard time swallowing tablets but may succeed if they are allowed to hold the tablet in the mouth for a while prior to swallowing, which is facilitated by the flavoured coating. Crushing of tablets is done for patients (both with and without enteral feeding tubes) in order to allow for easy swallowing. One nurse had noted an adverse effect when mixing medication with gruel, eventuating a dislike towards the gruel, which is unfortunate, since it is often an essential part of paediatric nutrition. |
| Experience/Attitude | Number | Never | Rarely | Occasionally | Often | Always | No Opinion |
|---|---|---|---|---|---|---|---|
| Does the health care provider ensure that the order can be compliant with the regulations 1? | n = 17 N (%) | 0 (0) | 2 (11.8) | 3 (17.6) | 9 (52.9) | 1 (5.9) | 2 (11.8) |
| How often do you order medications on paper because of an insufficient CPOE software? | n = 16 N (%) | 5 (31.3) | 9 (56.3) | 2 (12.5) | 0 (0) | 0 (0) | 0 (0) |
| Do you have the time to search for information regarding procedure/instructions for manipulation of a dosage form (off-label)? | n = 17 N (%) | 3 (17.6) | 9 (52.9) | 3 (17.6) | 2 (11.8) | 0 (0) | 0 (0) |
| Do you have the time to write thorough instructions for the procedure of the manipulation of a dosage form (off-label)? | n = 17 N (%) | 4 (23.5) | 5 (29.4) | 6 (35.3) | 2 (11.8) | 0 (0) | 0 (0) |
| Experience/Attitude | Number | Strongly Agree | Somewhat Agree | Neutral | Somewhat Disagree | Strongly Disagree | No Opinion |
| The available EHR/CPOE is sufficient for safe medication orders | n = 16 N (%) | 1 (6.3) | 6 (37.5) | 6 (37.5) | 2 (12.5) | 1 (6.3) | 0 (0) |
| Experience/Attitude | Number | Difficult | Intermediate Difficult | Neutral | Intermediate Easy | Easy | No Opinion |
| What is your perception of finding information in order to write a detailed medication order in regard to the procedure of manipulation of medication to children? | n = 17 N (%) | 4 (23.5) | 4 (23.5) | 5 (29.4) | 3 (17.6) | 0 (0) | 1 (5.9) |
| Experience/Attitude | Number | Yes, Based on: | No | Other | No Opinion | ||
| BW | BSA | BW0.75 | |||||
| When prescribing medications with unavailable dosing information to children, do you scale down from adult dosages to a corresponding dose suitable for children? If yes, with which scaling model? | n = 21 multiple choice N (%) | 8 (38.1) | 4 (19) | 1 (4.8) | 2 (9.5) | 6 (28.6) | 0 (0) |
| Experience/Attitude | Number | Never | Rarely | Occasionally | Often | Always | No Opinion |
|---|---|---|---|---|---|---|---|
| Do you feel safe/secure/comfortable with manipulation of medications? | n = 21 N (%) | 0 (0) | 0 (0) | 9 (42.9) | 12 (57.1) | 0 (0) | 0 (0) |
| Do you feel safe regarding working environment/health (for instance if a medication is hazardous)? | n = 21 N (%) | 0 (0) | 2 (9.5) | 10 (47.6) | 7 (33.3) | 2 (9.5) | 0 (0) |
| How often do you have to manipulate the dosage form of a medication for oral administration? | n = 21 N (%) | 0 (0) | 3 (14.3) | 8 (38.1) | 9 (42.9) | 1 (4.8) | 0 (0) |
| How often do you experience patients receiving complications from manipulated dosage forms? | n = 21 N (%) | 2 (9.5) | 12 (57.1) | 1 (4.8) | 0 (0) | 0 (0) | 6 (28.6) |
| If you have experienced complications, were there any serious consequences? | n = 13 N (%) | 9 (69.2) | 4 (30.8) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| How often are adverse effects from manipulations reported? | n = 18 N (%) | 2 (11.1) | 10 (55.6) | 3 (16.7) | 3 (16.7) | 0 (0) | 0 (0) |
| How often are clear instructions for execution of the manipulation of medications available in the paediatrician’s order? | n = 21 N (%) | 5 (23.8) | 8 (38.1) | 4 (19) | 3 (14.3) | 0 (0) | 1 (4.8) |
| How often do you consult with the prescribing paediatrician regarding the execution of a manipulation of a medication? | n = 21 N (%) | 0 (0) | 8 (38.1) | 9 (42.9) | 4 (19) | 0 (0) | 0 (0) |
| Do you have the time to search for information on the procedure for the manipulation? (e.g if it is possible to crush/divide a tablet/MR tablet/soft gelatine capsules)? | n = 21 N (%) | 1 (4.8) | 3 (14.3) | 7 (33.3) | 8 (38.1) | 2 (9.5) | 0 (0) |
| How often is it stressful to execute a manipulation of a medication? | n = 21 N (%) | 0 (0) | 4 (19) | 9 (42.9) | 8 (38.1) | 0 (0) | 0 (0) |
| Do you have time to execute manipulations of a dosage form? | n = 21 N (%) | 0 (0) | 1 (4.8) | 9 (42.9) | 9 (42.9) | 2 (9.5) | 0 (0) |
| Would it be valuable to receive ready-to-administer (RTA) medications from the pharmacy? | n = 21 N (%) | 0 (0) | 0 (0) | 1 (4.8) | 4 (19) | 15 (71.4) | 1 (4.8) |
| Do you get questions from the caregiver of the child (parent) regarding manipulating of dosage forms? | n = 21 N (%) | 9 (42.9) | 11 (52.4) | 0 (0) | 1 (4.8) | 0 (0) | 0 (0) |
| Are medications discarded (if only a fraction of a tablet was used) or solutions discarded due to short shelf life after being prepared? | n = 21 N (%) | 0 (0) | 1 (4.8) | 1 (4.8) | 4 (19) | 15 (71.4) | 0 (0) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kader, R.; Liminga, G.; Ljungman, G.; Paulsson, M. Manipulations of Oral Medications in Paediatric Neurology and Oncology Care at a Swedish University Hospital: Health Professionals’ Attitudes and Sources of Information. Pharmaceutics 2021, 13, 1676. https://doi.org/10.3390/pharmaceutics13101676
Kader R, Liminga G, Ljungman G, Paulsson M. Manipulations of Oral Medications in Paediatric Neurology and Oncology Care at a Swedish University Hospital: Health Professionals’ Attitudes and Sources of Information. Pharmaceutics. 2021; 13(10):1676. https://doi.org/10.3390/pharmaceutics13101676
Chicago/Turabian StyleKader, Rania, Gunnar Liminga, Gustaf Ljungman, and Mattias Paulsson. 2021. "Manipulations of Oral Medications in Paediatric Neurology and Oncology Care at a Swedish University Hospital: Health Professionals’ Attitudes and Sources of Information" Pharmaceutics 13, no. 10: 1676. https://doi.org/10.3390/pharmaceutics13101676