West Nile or Usutu Virus? A Three-Year Follow-Up of Humoral and Cellular Response in a Group of Asymptomatic Blood Donors
Abstract
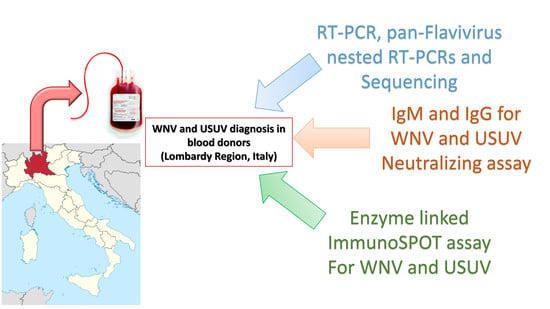
:1. Introduction
2. Materials and Methods
2.1. Blood Donors
2.2. Molecular Assays
2.3. Serological Assays
2.4. Enzyme-Linked Immunospot Assays
2.5. Ethics Statement
2.6. Statistical Analysis
3. Results
3.1. True Positive WNV and USUV Infections
3.2. Serological Patterns of WNV and USUV Infections in Blood Donors
3.3. T-Cell Responses against WNV and USUV
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Hayes, E.B.; Sejvac, J.J.; Zaki, S.R.; Lanciotti, R.S.; Bode, A.V.; Campbell, G.L. Virology, pathology, and clinical manifestation of West Nile virus disease. Emerg. Infect. Dis. 2005, 11, 1174–1179. [Google Scholar] [CrossRef]
- Autorino, G.L.; Battisti, A.; Deubel, V.; Ferrari, G.; Forletta, R.; Giovannini, A.; Lelli, R.; Murri, S.; Scicluna, M.T. West Nile virus epidemic in horses, Tuscany region, Italy. Emerg. Infect. Dis. 2002, 8, 1372–1378. [Google Scholar] [CrossRef]
- Blitvich, B.J. Transmission dynamics and changing epidemiology of West Nile virus. Anim. Health. Res. Rev. 2008, 9, 71–86. [Google Scholar] [CrossRef] [PubMed]
- Healy, J.M.; Reisen, W.K.; Kramer, V.L.; Fischer, M.; Lindsey, N.P.; Nasci, R.S.; Macedo, P.A.; White, G.; Takahashi, R.; Khang, L.; et al. Comparison of the efficiency and cost of West Nile virus surveillance methods in California. Vector Borne Zoonotic Dis. 2015, 15, 147–155. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rizzo, C.; Salcuni, P.; Nicoletti, L.; Ciufolini, M.G.; Russo, F.; Masala, R.; Frongia, O.; Finarelli, A.C.; Gramegna, M.; Gallo, L.; et al. Epidemiological surveillance of West Nile neuroinvasive diseases in Italy, 2008 to 2011. Euro Surveill. 2012, 17, 20172. [Google Scholar] [PubMed]
- Calzolari, M.; Bonilauri, P.; Bellini, R.; Caimi, M.; Defilippo, F.; Maioli, G.; Albieri, A.; Medici, A.; Veronesi, R.; Pilani, R.; et al. Arboviral survey of mosquitoes in two northern Italian regions in 2007 and 2008. Vector Borne Zoonotic Dis. 2010, 10, 875–884. [Google Scholar] [CrossRef] [PubMed]
- Weissenböck, H.; Bakonyi, T.; Rossi, G.; Mani, P.; Nowotny, N. Usutu virus, Italy, 1996. Emerg. Infect. Dis. 2013, 274–277. [Google Scholar] [CrossRef]
- Weissenböck, H.; Kolodziejek, J.; Url, A.; Lussy, H.; Rebel-Bauder, B.; Nowotny, N. Emergence of Usutu virus, an African mosquito-borne flavivirus of the Japanese encephalitis virus group, central Europe. Emerg. Infect. Dis. 2002, 8, 652–656. [Google Scholar] [CrossRef]
- Cavrini, F.; Gaibani, P.; Longo, G.; Pierro, A.M.; Rossini, G.; Bonilauri, P.; Gerunda, G.E.; Di Benedetto, F.; Pasetto, A.; Girardis, M.; et al. Usutu virus infection in a patient who underwent orthotropic liver transplantation, Italy, August–September 2009. Euro Surveill. 2009, 14, 19448. [Google Scholar]
- Pecorari, M.; Longo, G.; Gennari, W.; Grottola, A.; Sabbatini, A.; Tagliazucchi, S.; Savini, G.; Monaco, F.; Simone, M.; Lelli, R.; et al. First human case of Usutu virus neuroinvasive infection, Italy, August–September 2009. Euro Surveill. 2009, 14, 19446. [Google Scholar]
- Calzolari, M.; Bonilauri, P.; Bellini, R.; Albieri, A.; Defilippo, F.; Maioli, G.; Galletti, G.; Gelati, A.; Barbieri, I.; Tamba, M.; et al. Evidence of simultaneous circulation of West Nile and Usutu viruses in mosquitoes samples in Emilia-Romagna region (Italy) in 2009. PLoS ONE 2010, 5, e14324. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pradier, S.; Lecollinet, S.; Leblond, A. West Nile virus epidemiology and factors triggering change in its distribution in Europe. Rev. Sci. Tech. 2012, 31, 829–844. [Google Scholar] [CrossRef] [PubMed]
- Oliphant, T.; Nybakken, G.E.; Engle, M.; Xu, Q.; Nelson, C.A.; Sukupolvi-Petty, S.; Marri, A.; Lachmi, B.E.; Olshevsky, U.; Fremont, D.H.; et al. Antibody recognition and neutralization determinants on domains I and II of West Nile Virus envelope protein. J. Virol. 2006, 80, 12149–12159. [Google Scholar] [CrossRef] [Green Version]
- Nikolay, B.; Fall, G.; Boye, C.S.; Sall, A.A.; Skern, T. Validation of a structural comparison of the antigenic characteristics of Usutu virus and West Nile virus envelope proteins. Virus. Res. 2014, 189, 87–91. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Seco, M.P.; Rosario, D.; Domingo, C.; Hernández, L.; Valdés, K.; Guzmán, M.G.; Tenorio, A. Generic RT-nested-PCR for detection of flaviviruses using degenerated primers and internal control followed by sequencing for specific identification. J. Virol. Methods 2005, 126, 101–109. [Google Scholar] [CrossRef]
- Gaibani, P.; Pierro, A.; Lunghi, G.; Farina, C.; Toschi, V.; Matinato, C.; Orlandi, A.; Zoccoli, A.; Almini, D.; Landini, M.P.; et al. Seroprevalence of West Nile virus antibodies in blood donors living in the metropolitan area of Milan, Italy, 2009-2011. New Microbiol. 2013, 36, 81–83. [Google Scholar]
- Pierro, A.; Gaibani, P.; Manisera, C.; Rossini, G.; Finarelli, A.C.; Ghinelli, F.; Macini, P.; Landini, M.P.; Sambri, V. Persistence of anti-West Nile virus-specific antibodies among asymptomatic blood donors in northeastern Italy. Vector Borne Zoonotic Dis. 2013, 13, 892–893. [Google Scholar] [CrossRef]
- Cadar, D.; Maier, P.; Müller, S.; Kress, J.; Chudy, M.; Bialonski, A.; Schlaphof, A.; Jansen, S.; Jöst, H.; Tannich, E.; et al. Blood donor screening for West Nile virus (WNV) revealed acute Usutu virus (USUV) infection, Germany, September 2016. Euro Surveill. 2017, 22, 30452. [Google Scholar] [CrossRef]
- Engle, M.J.; Diamond, M.S. Antibody prophylaxis and therapy against West Nile virus infection in wild-type and immunodeficient mice. J. Virol. 2003, 77, 12941–12949. [Google Scholar] [CrossRef] [Green Version]
- Stewart, B.S.; Demarest, V.L.; Wong, S.J.; Green, S.; Bernard, K.A. Persistence of virus-specific immune responses in the central nervous system of mice after West Nile virus infection. BMC Immunol. 2011, 12, 6. [Google Scholar] [CrossRef] [Green Version]
- Linke, S.; Ellerbrok, H.; Niedrig, M.; Nitsche, A.; Pauli, G. Detection of West Nile virus lineages 1 and 2 by real-time PCR. J. Virol. Methods. 2007, 146, 355–358. [Google Scholar] [CrossRef] [PubMed]
- Scaramozzino, N.; Crance, J.M.; Jouan, A.; DeBriel, D.A.; Stoll, F.; Garin, D. Comparison of Flavivirus universal primer pairs and development of a rapid, highly sensitive heminested reverse transcription-PCR assay for detection of Flavivirus targeted to a conserved region of the NS5 gene sequence. J. Clin. Microbiol. 2001, 39, 1922–1927. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Calarota, S.A.; Chiesa, A.; Zelini, P.; Comolli, G.; Minoli, L.; Baldanti, F. Detection of Epstein-Barr virus-specific memory CD4+ T cells using a peptide-based cultured enzyme-linked immunospot assay. Immunology 2013, 139, 533–544. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.G.; Liu, X.; Kaufhold, R.M.; Clair, J.; Caulfield, M.J. Development and Validation of a Gamma Interferon ELISPOT Assay for Quantitation of Cellular Immune Responses to Varicella-Zoster Virus. Clin. Diagn. Lab. Immunol. 2001, 8, 871–879. [Google Scholar] [CrossRef] [Green Version]
- Pierro, A.; Gaibani, P.; Manisera, C.; Dirani, G.; Rossini, G.; Cavrini, F.; Ghinelli, F.; Ghinelli, P.; Finarelli, A.C.; Mattivi, A.; et al. Seroprevalence of West Nile virus-specific antibodies in a cohort of blood donors in northeastern Italy. Vector Borne Zoonotic Dis. 2011, 11, 1605–1607. [Google Scholar] [CrossRef]
- Pierro, A.; Gaibani, P.; Spadafora, C.; Ruggeri, D.; Randi, V.; Parenti, S.; Finarelli, A.C.; Rossini, G.; Landini, M.P.; Sambri, V. Detection of specific antibodies against West Nile and Usutu viruses in healthy blood donors in northern Italy, 2010–2011. Clin. Microbiol. Infect. 2013, 19, E451–E453. [Google Scholar] [CrossRef] [Green Version]
- Grottola, A.; Marcacci, M.; Tagliazucchi, S.; Gennari, W.; Di Gennaro, A.; Orsini, M.; Monaco, F.; Marchegiano, P.; Marini, V.; Meacci, M.; et al. Usutu virus infections in humans: A retrospective analysis in the municipality of Modena, Italy. Clin. Microbiol. Infect. 2017, 23, 33–37. [Google Scholar] [CrossRef] [Green Version]
- Percivalle, E.; Sassera, D.; Rovida, F.; Isernia, P.; Fabbi, M.; Baldanti, F.; Marone, P. Usutu Virus Antibodies in Blood Donors and Healthy Forestry Workers in the Lombardy Region, Northern Italy. Vector Borne Zoonotic Dis. 2017, 17, 658–661. [Google Scholar] [CrossRef]
- Aberle, S.W.; Kolodziejek, J.; Jungbauer, C.; Stiasny, K.; Aberle, J.H.; Zoufaly, A.; Hourfar, M.K.; Weidner, L.; Nowotny, N. Increase in human West Nile and Usutu virus infections, Austria, 2018. Euro Surveill. 2018, 23, 1800545. [Google Scholar] [CrossRef] [Green Version]
- Zaaijer, H.L.; Slot, E.; Molier, M.; Reusken, C.B.E.M.; Koppelman, M.H.G.M. Usutu virus infection in Dutch blood donors. Transfusion 2019, 59, 2931–2937. [Google Scholar] [CrossRef]
- Bakonyi, T.; Jungbauer, C.; Aberle, S.W.; Kolodziejek, J.; Dimmel, K.; Stiasny, K.; Allerberger, F.; Nowotny, N. Usutu virus infections among blood donors, Austria, July and August 2017-Raising awareness for diagnostic challenges. Euro Surveill. 2017, 22. [Google Scholar] [CrossRef] [PubMed]
- Domanović, D.; Gossner, C.M.; Lieshout-Krikke, R.; Mayr, W.; Baroti-Toth, K.; Dobrota, A.M.; Escoval, M.A.; Henseler, O.; Jungbauer, C.; Liumbruno, G.; et al. Nile and Usutu Virus Infections and Challenges to Blood Safety in the European Union. Emerg. Infect. Dis. 2019, 25, 1050–1057. [Google Scholar] [PubMed]
- Calisher, C.H.; Karabatsos, N.; Dalrymple, J.M.; Shope, R.E.; Porterfield, J.S.; Westaway, E.G.; Brandt, W.E. Antigenic relationships between flaviviruses as determined by cross-neutralization tests with polyclonal antisera. J. Gen. Virol. 1989, 70, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Chanama, S.; Anantapreecha, S.; A-nuegoonpipat, A.; Sa-gnasang, A.; Kurane, I.; Sawanpanyalert, P. Analysis of specific IgM responses in secondary dengue virus infections: Levels and positive rates in comparison with primary infections. J. Clin. Virol. 2004, 31, 185–189. [Google Scholar] [CrossRef]
- Diamond, M.S.; Sitati, E.M.; Friend, L.D.; Higgs, S.; Shrestha, B.; Engle, M. A critical role for induced IgM in the protection against West Nile virus infection. J. Exp. Med. 2003, 198, 1853–1862. [Google Scholar] [CrossRef]
- Pacenti, M.; Sinigaglia, A.; Martello, T.; De Rui, M.E.; Franchin, E.; Pagni, S.; Peta, E.; Riccetti, S.; Milani, A.; Montarsi, F.; et al. Clinical and virological findings in patients with Usutu virus infection, northern Italy, 2018. Euro Surveill. 2019, 24. [Google Scholar] [CrossRef]
- Barzon, L.; Percivalle, E.; Pacenti, M.; Rovida, F.; Zavattoni, M.; Del Bravo, P.; Cattelan, A.M.; Palù, G.; Baldanti, F. Virus and antibody dynamics in travelers with acute Zika virus infection. Clin. Infect. Dis. 2018, 66, 1173–1180. [Google Scholar] [CrossRef]


| Year | WNV Confirmed Cases | WNV RT-PCR/PAN pos | WNV SER pos | USUV Confirmed Cases | USUV PAN pos | USUV SER pos | USUV ELISpot n = 9 | Unknown (n) | Total no. of Blood Donors/Year |
|---|---|---|---|---|---|---|---|---|---|
| 2016 | 9 | 3 | 6 | 5 | 0 | 5 | 0 | 0 | 14 (25.9%) |
| 2017 | 2 | 2 | 0 | 11 | 6 | 5 | 1 | 2 | 15 (27.8%) |
| 2018 | 14 | 7 | 7 | 9 | 0 | 9 | 0 | 2 | 25 (46.3%) |
| total | 25 (46.2%) | 12 (11.8%) | 13 (24.0%) | 25 (46.2%) | 6 (11.1%) | 19 (35.1%) | 1 (11.1%) | 4 (7.4%) | 54 |
| Serological Patterns | True Positive WNV WNV IgM+, IgG+, NT+ | True Positive USUV USUV IgM+, IgG+, NT+ | p-Value (Fisher’s Exact Test) |
|---|---|---|---|
| USUV IgM-, IgG-, NT- | 15 | 0 | <0.0001 * |
| USUV IgM+, IgG+, NT+ | 6 | 0 | 0.0223 * |
| USUV IgM-, IgG+, NT+ | 4 | 0 | 0.1099 |
| WNV IgM-, IgG-, NT- | 0 | 7 | 0.0096 * |
| WNV IgM+, IgG+, NT+ | 0 | 8 | 0.0040 * |
| WNV IgM-, IgG+, NT+ | 0 | 10 | 0.0006 * |
| Total | 25 | 25 |
| Blood Donor | WNV ELISpot Net Spots/Million PBMC | USUV ELISpot Net Spots/Million PBMC | Molecular Test | WNV NT Abs | USUV NT Abs | True Positive for WNV/USUV |
|---|---|---|---|---|---|---|
| 1 | 80 | 135 | USUV | <10 | 40 | USUV |
| 2 | 8 | 655 | N | 10 | 10 | USUV |
| 3 | 63 | 105 | N | 10 | 40 | USUV |
| 4 | 18 | 610 | USUV | 20 | 20 | USUV |
| 5 | 15 | 30 | N | <10 | 80 | USUV |
| 6 | 128 | 5 | WNV | 160 | <10 | WNV |
| 7 | 20 | 10 | WNV | 80 | 20 | WNV |
| 8 | 35 | 10 | N | 80 | <10 | WNV |
| 9 | 10 | 0 | WNV | 40 | <10 | WNV |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Percivalle, E.; Cassaniti, I.; Sarasini, A.; Rovida, F.; Adzasehoun, K.M.G.; Colombini, I.; Isernia, P.; Cuppari, I.; Baldanti, F. West Nile or Usutu Virus? A Three-Year Follow-Up of Humoral and Cellular Response in a Group of Asymptomatic Blood Donors. Viruses 2020, 12, 157. https://doi.org/10.3390/v12020157
Percivalle E, Cassaniti I, Sarasini A, Rovida F, Adzasehoun KMG, Colombini I, Isernia P, Cuppari I, Baldanti F. West Nile or Usutu Virus? A Three-Year Follow-Up of Humoral and Cellular Response in a Group of Asymptomatic Blood Donors. Viruses. 2020; 12(2):157. https://doi.org/10.3390/v12020157
Chicago/Turabian StylePercivalle, Elena, Irene Cassaniti, Antonella Sarasini, Francesca Rovida, Kodjo Messan Guy Adzasehoun, Ilaria Colombini, Paola Isernia, Irene Cuppari, and Fausto Baldanti. 2020. "West Nile or Usutu Virus? A Three-Year Follow-Up of Humoral and Cellular Response in a Group of Asymptomatic Blood Donors" Viruses 12, no. 2: 157. https://doi.org/10.3390/v12020157