Prediction and Optimization of the Cost of Energy Resources in Greek Public Hospitals
Abstract
:1. Introduction
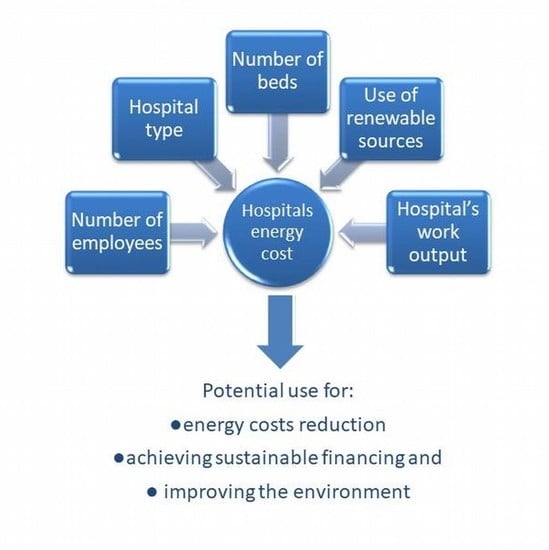
- Have a complete picture of the cost of energy resources, both in total and per health unit.
- Understand the factors that contribute to the energy cost so that they can plan targeted interventions.
- Compare the indicators of each hospital against the ones with the best performance and practices, thus detecting which ones have less efficient energetic behaviors and promoting the use of renewable energy sources.
- Be well-prepared regarding budgeting so that they can ensure the viability of their finances through sustainable development.
- Have positive outcomes, such as decreasing costs and improving sustainability or even profitability due to better energy efficiency.
- Measure, monitor, and improve the environmental footprint of the hospital, thus improving the environmental conditions of its area and potentially the health of the residents of the region in which it is located.
2. Materials and Methods
- A hospital’s type is the first characteristic that reflects major information about its size and the number and complexity of the medical units that operate in it. There are four types of hospitals in Greece: small hospital/health centers, general hospitals, university hospitals, and special hospitals.
- The number of beds was also included in our model because it indicates, to a large extent, the size of each hospital building and the type of services provided.
- One additional element that significantly affects operating costs is the area in which each hospital is located. This variable concerns the location of each hospital, in mainland or island Greece, which indicates short or long distances from production units and high or low transport costs.
- Τhe non/existence of special units such as intensive care, increased care, and artificial kidney units was included because of their possible special demands of energy sources.
- The amount of total annual operating costs was also recorded as a comparison measurement between hospitals and the identification of best practices.
- Τhe existence of a natural gas supply for the heating of the building facilities and water in each hospital is clearly more economical and more ecological than the use of petrol; for this reason, it was recorded separately.
- The number of employees, i.e., permanent and auxiliary staff members, was recorded.
- The total number of patients, both internal and external.
- The total number of laboratory tests, e.g., bio-pathological tests, endoscopic examinations, invasive diagnostic tests, and medical imaging tests.
- The total number of dialyses performed in the artificial kidney unit.
- The total number of surgeries.
3. Results
4. Discussion
- (a)
- The age of the buildings and electromechanical installations.
- (b)
- Access to renewable energy sources.
- (c)
- The educational needs of the hospitals stuff for sustainable behavior and sustainable management.
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- OECD. Healthcare Costs Unsustainable in Advanced Economies without Reform. Available online: http://www.oecd.org/health/healthcarecostsunsustainableinadvancedeconomieswithoutreform.htm (accessed on 15 June 2021).
- U.N. Transforming Our World: The 2030 Agenda for Sustainable Development. In Seventieth United Nations General Assembly. Available online: http://www.un.org/ga/search/view_doc.asp?symbol=A/RES/70/1&Lang=E (accessed on 15 June 2021).
- World Health Organization. WHO Calls for Urgent Action to Protect Health from Climate Change. Available online: www.who.int/globalchange/ (accessed on 15 June 2021).
- Ziebik, A.; Hoinka, K. Energy Systems of Complex Buildings; Springer: London, UK, 2013. [Google Scholar]
- Bawaneh, K.; Ghazi Nezami, F.; Rasheduzzaman, M.; Deken, B. Energy consumption analysis and characterization of healthcare facilities in the United States. Energies 2019, 19, 3775. [Google Scholar] [CrossRef] [Green Version]
- Ma, H.; Du, N.; Yu, S.; Lu, W.; Zhang, Z.; Deng, N.; Li, C. Analysis of typical public building energy consumption in northern China. Energy Build. 2017, 136, 139–150. [Google Scholar] [CrossRef]
- Jiang, C.; Xing, J.; Ling, J.; Qin, X. Energy consumption and carbon emissions of hospitals in Tianjin. Front. Energy 2012, 6, 427–435. [Google Scholar] [CrossRef]
- Morgenstern, P.; Li, M.; Raslan, R.; Ruyssevelt, P.; Wright, A. Benchmarking acute hospitals: Composite electricity targets based on departmental consumption intensities. Energy Build. 2016, 118, 277–290. [Google Scholar] [CrossRef]
- Christiansen, N.; Kaltschmitt, M.; Dzukowski, F. Electrical energy consumption and utilization time analysis of hospital departments and large scale medical equipment. Energy Build. 2016, 131, 172–183. [Google Scholar] [CrossRef]
- Christiansen, N.; Kaltschmitt, M.; Dzukowski, F.; Isensee, F. Electricity consumption of medical plug loads in hospital laboratories: Identification, evaluation, prediction and verification. Energy Build. 2015, 107, 392–406. [Google Scholar] [CrossRef]
- Zorita, A.L.; Fernández-Temprano, M.A.; García-Escudero, L.A.; Duque-Perez, O. A statistical modeling approach to detect anomalies in energetic efficiency of buildings. Energy Build. 2016, 110, 377–386. [Google Scholar] [CrossRef]
- Gaglia, A.G.; Balaras, C.A.; Mirasgedis, S.; Georgopoulou, E.; Sarafidis, Y.; Lalas, D.P. Empirical assessment of the Hellenic non-residential building stock, energy consumption, emissions and potential energy savings. Energy Convers. Manag. 2007, 48, 1160–1175. [Google Scholar] [CrossRef]
- Vourdoubas, J. Energy consumption and carbon emissions in Venizelio hospital in Crete, Greece: Can it be carbon neutral? J. Eng. Archit. 2018, 6, 19–27. [Google Scholar]
- González, A.G.; García-Sanz-Calcedo, J.; Salgado, D.R. A quantitative analysis of final energy consumption in hospitals in Spain. Sustain. Cities Soc. 2018, 36, 169–175. [Google Scholar] [CrossRef]
- García-Sanz-Calcedo, J.; Gómez-Chaparro, M.; Sanchez-Barroso, G. Electrical and thermal energy in private hospitals: Consumption indicators focused on healthcare activity. Sustain. Cities Soc. 2019, 47, 101482. [Google Scholar] [CrossRef]
- González González, A.; García-Sanz-Calcedo, J.; Rodríguez Salgadom, D. Evaluation of energy consumption in German hospitals: Benchmarking in the public sector. Energies 2018, 11, 2279. [Google Scholar] [CrossRef] [Green Version]
- Diggle, P.J.; Heagerty, P.J.; Liang, K.Y.; Zeger, S.L. Analysis of Longitudinal Data; Oxford University Press: Oxford, UK, 2002. [Google Scholar]
- Huber, P.J. The behavior of maximum likelihood estimates under nonstandard conditions. In Proceedings of the Fifth Berkeley Symposium on Mathematical Statistics and Probability, Los Angeles, CA, USA, 18–21 July 1965; University of California Press: Berkeley, CA, USA, 1967; Volume 1, pp. 221–233. [Google Scholar]
- White, H.L., Jr. A heteroskedasticity-consistent covariance matrix estimator and a direct test for heteroskedasticity. Econometrica 1980, 48, 817–838. [Google Scholar] [CrossRef]
- White, H.L., Jr. Maximum likelihood estimation of misspecified models. Econometrica 1982, 50, 1–25. [Google Scholar] [CrossRef]
- Liang, K.-Y.; Zeger, S.L. Longitudinal data analysis using generalized linear models. Biometrika 1986, 73, 13–22. [Google Scholar] [CrossRef]
- Laird, N.M.; Ware, J.H. Random-effects models for longitudinal data. Biometrika 1982, 38, 963–974. [Google Scholar] [CrossRef]
- Skrondal, A.; Rabe-Hesketh, S. Generalized Latent Variable Modeling: Multilevel, Longitudinal, and Structural Equation Models; Chapman & Hall/CRC: Boca Raton, FL, USA, 2004. [Google Scholar]
- Sepetis, A. Sustainable Finance in Sustainable Health Care System. Open J. Bus. Manag. 2020, 8, 262–281. [Google Scholar] [CrossRef] [Green Version]
- Sepetis, A. Sustainable Health Care Management in the Greek Health Care Sector. Open J. Soc. Sci. 2019, 7, 386. [Google Scholar] [CrossRef] [Green Version]







| Hospital Type | Area | |||
|---|---|---|---|---|
| Mainland | Island | |||
| Number of Hospitals | Number of Beds | Number of Hospitals | Number of Beds | |
| Small Hospitals/Health Centers | 9 | 388 | 10 | 477 |
| General Hospitals | 64 | 18,468 | 13 | 2518 |
| University Hospitals | 6 | 3973 | 2 | 1115 |
| Specialized Hospitals | 17 | 6460 | 0 | 0 |
| Hospital Type | Average Annual Cost of Energy Resources per Bed from Both Years 2018 and 2019 | ||||
|---|---|---|---|---|---|
| Obs | Mean | Std. Dev. | Min | Max | |
| Small Hospital/Heath Center | 38 | 2705.11 | 1778.74 | 712.20 | 8728.43 |
| General Hospital | 155 | 3073.69 | 1440.71 | 789.07 | 10,435.82 |
| University Hospital | 16 | 4049.81 | 1185.23 | 1779.09 | 6165.49 |
| Specialized Hospital | 33 | 2467.77 | 1379.45 | 956.87 | 7057.02 |
| Univariate Associations of the 23 Independent Variables in the Total Cost of Energy Resources | Linear Regression for Cost of Energy Resources Year 2018 | Linear Regression for Cost of Energy Resources Year 2019 | Linear Regression for Cost of Energy Resources Clustered per Hospital | Random Effect Regression (GLS) for Cost of Energy Resources |
|---|---|---|---|---|
| Number of Obs = 121 | Number of Obs = 121 | Number of Obs = 242 Number of Groups = 121 | Number of Obs = 242 Number of Groups = 121 | |
| Coef. (Std. Err.) | Coef. (Std. Err.) | Coef. (Std. Err.) | Coef. (Std. Err.) | |
| Number of Beds | 2583.323 (183.3146) | 2885.454 (185.8608) | 2735.491 (404.5028) | 2735.491 (130.6286) |
| Hospital Type | ||||
| Small Hospital/Health Center | − | − | − | − |
| General Hospital | 618,148.7 (138,856.2) | 698,553.4 (160,696.5) | 658,642 (75,678.37) | 658,642 (105,513.8) |
| University Hospital | 2,473,521 (228,460.8) | 2,494,973 (264,730.9) | 2,484,247 (358,166.6) | 2,484,247 (173,713.4) |
| Specialized Hospital | 622,670.6 (180,968) | 635,208.7 (213,128.6) | 628,601.6 (119,088.8) | 628,601.6 (138,697.5) |
| Area—Island | −186,407.6 (170,239.4) | −257,482.8 (184,100.5) | −221,945.2 (187,034.7) | −221,945.2 (124,977.8) |
| Total Internal Patients | 29.77748 (1.995884) | 29.24453 (2.318873) | 29.5028 (3.672652) | 29.5028 (1.53056) |
| Days of Stay | 9.627841 (0.6174054) | 9.806502 (0.706705) | 9.71513 (1.003908) | 9.71513 (0.4693699) |
| Total Number of Outpatients | 7.707917 (0.5921816) | 8.544256 (0.6152159) | 8.121719 (1.044999) | 8.121719 (0.427375) |
| Total Surgeries | 111.7947 (12.60767) | 130.2421 (13.89072) | 120.507 (21.77539) | 120.507 (9.361653) |
| Total Laboratory Tests | 0.4572315 (0.0269609) | 0.4933744 (0.0286535) | 0.4756304 (0.0481975) | 0.4756304 (0.0196695) |
| Medical Imaging Tests | 5.869697 (0.6399809) | 6.709507 (0.6620062) | 6.289428 (1.200686) | 6.289428 (0.4600281) |
| Average Days of Stay | −11,523.83 (20,782.18) | −5940.653 (23,832.93) | −9048.96 (11,783.63) | −9048.96 (15,697.78) |
| Average Bed Coverage | 719,374 (236,046.4) | 644,088.4 (243,526) | 677,010.9 (523,825.4) | 677,010.9 (169,197.2) |
| Patient Income Rate | 421,863.9 (178,211.9) | 314,378.6 (184,733.5) | 365,219.9 (296,320.8) | 365,219.9 (128,091.2) |
| Total Number of Employees | 1212.711 (66.04963) | 1,325.883 (62.22339) | 1271.508 (111.8295) | 1271.508 (45.33585) |
| Intensive Care Unit | 850,144.1 (115,520.8) | 879,509.4 (127,579.9) | 864,251.8 (109,305.8) | 864,251.8 (85,831.18) |
| Artificial Kidney Unit | 453,859.2 (141,255.3) | 537,861.2 (153,044.8) | 496,155.2 (116,690.6) | 496,155.2 (103,787.5) |
| Number of Dialysis | 57.45735 (12.96495) | 65.3004 (14.15578) | 61.34309 (11.70055) | 61.34309 (9.565,021) |
| Gas Yes/No | 335,470.1 (137,725.1) | 456,603.5 (147,253.1) | 396,036.8 (136,887.2) | 396,036.8 (100,556.3) |
| Average Low Temperature in Winter °C | 301.2561 (20,963.22) | 3182.975 (22,739.5) | 1742.116 (30,626.47) | 1742.116 (15,412.65) |
| Average High Temperature in Summer °C | 94,859.44 (38,050.85) | 109,922.1 (41,126.1) | 102,390.8 (35,712.58) | 102,390.8 (27,926.4) |
| Pearson’s Correlations | Beds | Internal Patients | Days of Stay | Total number of Outpatients | Number of Sessions in AKU | Total Surgeries | Laboratory Tests | Medical Imaging Tests | Total Number of Employees | Average Days of Stay | Average Bed Coverage | Patient Income Rate |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Beds | 1.0000 | |||||||||||
| Internal patients | 0.7996 | 1.0000 | ||||||||||
| Days of stay | 0.9074 | 0.8986 | 1.0000 | |||||||||
| Total number of outpatients | 0.7556 | 0.8532 | 0.7802 | 1.0000 | ||||||||
| Number of sessions in AKU | 0.3070 | 0.3887 | 0.3118 | 0.4960 | 1.0000 | |||||||
| Total number of surgeries | 0.7021 | 0.8045 | 0.7407 | 0.8612 | 0.4108 | 1.0000 | ||||||
| Laboratory tests | 0.7932 | 0.8772 | 0.8762 | 0.8316 | 0.3575 | 0.7731 | 1.0000 | |||||
| Medical imaging tests | 0.6295 | 0.7119 | 0.6807 | 0.7893 | 0.3832 | 0.7760 | 0.7221 | 1.0000 | ||||
| Total number of employees | 0.9236 | 0.8793 | 0.9214 | 0.8524 | 0.3511 | 0.8012 | 0.9166 | 0.7398 | 1.0000 | |||
| Average Days of Stay | 0.1921 | −0.181 | 0.1579 | −0.2137 | −0.2041 | −0.2142 | −0.1472 | −0.1768 | −0.0105 | 1.0000 | ||
| Average Bed Coverage | 0.2314 | 0.3616 | 0.4627 | 0.2637 | 0.1373 | 0.2779 | 0.2963 | 0.2395 | 0.3239 | 0.3480 | 1.0000 | |
| Patient Income Rate | 0.1118 | 0.4477 | 0.2426 | 0.3506 | 0.1751 | 0.4274 | 0.2735 | 0.2434 | 0.2290 | −0.4012 | 0.3699 | 1.0000 |
| Variables | Linear Regression for Cost of Energy Resources for Year 2018 | Linear Regression for Cost of Energy Resources for Year 2019 | Linear Regression for Cost of Energy Resources Clustered per Hospital | Random Effect Regression (GLS) for Cost of Energy Resources (Model 1) | |
|---|---|---|---|---|---|
| Number of Obs = 121 R² = 0.8737 | Number of Obs = 121 R² = 0.8823 | Number of Obs = 242 Number of Groups = 121 R² = 0.8706 | Number of Obs = 242 Number of Groups = 121 Wald chi² = 771.39 | ||
| Coef. (Std. Err.) | Coef. (Std. Err.) | Coef. (Std. Err.) | Coef. (Std. Err.) | ||
| Number of Beds | b₁ | 1737.639 (379.5269) | 1141.638 (407.442) | 1457.61 (427.0586) | 1457.61 (280.5435) |
| Total Internal Patients | b₂ | −7.148189 (4.642647) | −20.38138 (4.466779) | −14.39322 (4.973882) | −14.39322 (3.244414) |
| Total Surgeries | b₃ | −41.46583 (11.992) | −39.14559 (13.2354) | −40.00607 (11.5357) | −40.00607 (8.982373) |
| Medical Imaging Tests | b₄ | 0.6098211 (0.516857) | 1.371569 (0.549363) | 1.008296 (0.452521) | 1.008296 (0.3811336) |
| Total Number of Employees | b₅ | 748.5674 (175.9849) | 1162.502 (187.1926) | 977.9197 (159.9215) | 977.9197 (129.222) |
| Gas Yes/No | b₆ | 318,254.9 (107,887.6) | 318,874 (110,294.2) | 316,048.8 (100,715.5) | 316,048.8 (77,994.67) |
| Beds # Internal Patients | b₇ | 0.0304837 (0.006491) | 0.0354459 (0.0065366) | 0.0325848 (0.0064755) | 0.0325848 (0.0046534) |
| Gass # Beds Gass = Yes | b₈ | −2099.597 (289.5574) | −1669.537 (289.5997) | −1880.896 (409.1054) | −1880.896 (206.8234) |
| Constant | b₀ | −5651.184 (57,453.19) | −8279.186 (59,706.13) | −11,034.03 (40,728.71) | −11,034.0 (41,903.62) |
| Model | Obs | ll (Null) | ll (Model) | df | AIC | BIC |
|---|---|---|---|---|---|---|
| Model 1 | 242 | −3629.395 | −3381.432 | 11 | 6784.863 | 6823.242 |
| Model 2 | 242 | −3629.396 | −3402.71 | 8 | 6821.421 | 6849.332 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zaza, P.N.; Sepetis, A.; Bagos, P.G. Prediction and Optimization of the Cost of Energy Resources in Greek Public Hospitals. Energies 2022, 15, 381. https://doi.org/10.3390/en15010381
Zaza PN, Sepetis A, Bagos PG. Prediction and Optimization of the Cost of Energy Resources in Greek Public Hospitals. Energies. 2022; 15(1):381. https://doi.org/10.3390/en15010381
Chicago/Turabian StyleZaza, Paraskevi N., Anastasios Sepetis, and Pantelis G. Bagos. 2022. "Prediction and Optimization of the Cost of Energy Resources in Greek Public Hospitals" Energies 15, no. 1: 381. https://doi.org/10.3390/en15010381