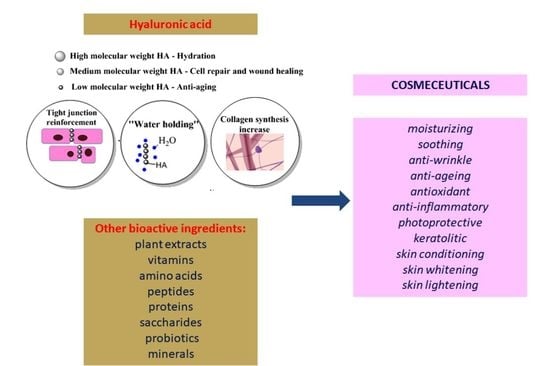
Advantages of Hyaluronic Acid and Its Combination with Other Bioactive Ingredients in Cosmeceuticals
Abstract
:1. Introduction
2. Applications of Hyaluronic Acid
3. Use of Hyaluronic Acid in Cosmetology
3.1. Hydratation Effect of HA in Cosmetic Formulations
3.2. Anti-Ageing Effect of HA in Cosmetic Formulations
4. Cosmetic Products with HA and Its Derivates Available on the Market
4.1. Bioactive Compounds in Cosmetics with HA and HA Derivates
4.2. Other Active Ingredients in Commercialy Available HA and HA Derivates Cosmetics
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AD | Atopic dermatitis |
| CIR | Cosmetic Ingredient Review |
| CS | Chondroitin sulphate |
| DEJ | Dermoepidermal junction |
| DOX | Docetaxel |
| Dx/HA | Dextranomer/hyaluronic acid copolymer |
| ECM | Extracellular matrix |
| FSFI | Female sexual function index |
| HA | Hyaluronic acid |
| HARE | Hyaluronan receptor for endocytosis |
| HMW-HA | High molecular weight hyaluronic acid |
| IOP | Intraocular pressure |
| KHA | Potassium hyaluronate |
| LMW-HA | Low molecular weight hyaluronic acid |
| LYVE1 | Lymphatic vessel endothelial hyaluronan receptor-1 |
| MMW-HA | Medium molecular weight hyaluronic acid |
| MSCs | Mesenchymal stronal cells |
| NaHA | Sodium hyaluronate |
| NP | Nanoparticles |
| OVD | Ophthalmic viscoelastic device |
| PLOD 3 | Procollagen-lysine, oxoglutarate 5-dioxygenase 3 |
| PTX | Paclitaxel |
| RHAMM | Receptor for hyaluronan-mediated motility |
| SC | Stratum corneum |
| SOD | Superoxide dismutase |
| TEWL | Transepidermal water loss |
| TLR | Toll-like receptor |
| TNF-α | Tumor necrosis factor-α |
| UTI | Urinary tract infection |
| VUR | Vesicoureteral reflux |
References
- Juhlin, L. Hyaluronan in skin. J. Intern. Med. 1997, 242, 61–66. [Google Scholar] [CrossRef]
- Ghersetich, I.; Lotti, T.; Campanile, G.; Grappone, C.; Dini, G. Hyaluronic acid in cutaneous intrinsec aging. Int. J. Dermatol. 1994, 33, 119–122. [Google Scholar] [CrossRef]
- Liao, Y.H.; Jones, S.A.; Forbes, B.; Martin, G.P.; Brown, M.B. Hyaluronan: Pharmaceutical characterization and drug delivery. Drug Deliv. J. Deliv. Target. Ther. Agents 2005, 12, 327–342. [Google Scholar] [CrossRef]
- Ibrahim, Z.A.; Gheida, S.F.; El Maghraby, G.M.; Farag, Z.E. Evaluation of the efficacy and safety of combinations of hydroquinone, glycolic acid, and hyaluronic acid in the treatment of melasma. J. Cosmet. Dermatol. 2015, 14, 113–123. [Google Scholar] [CrossRef]
- Turlier, V.; Rouquier, A.; Black, D.; Josse, G.; Auvergnat, A.; Briant, A.; Dahan, S.; Gassia, V.; Saint-Martory, C.; Zakaria, W.; et al. Assessment of the clinical efficacy of a hyaluronic acid-based deep wrinkle filler using new instrumental methods. J. Cosmet. Laser Ther. 2010, 12, 195–202. [Google Scholar] [CrossRef] [PubMed]
- Muntean, A.C.; Juncan, A.M.; Moisa, D.G.; Vonica, A.L.; Rus, L.L.; Morgovan, C.; Gligor, F.G.; Butuca, A.; Stanila, A. Primary packaging and stability evaluation of a serum used for the periorbital area of the sensitive eye. Mater. Plast. 2019, 56. [Google Scholar] [CrossRef]
- Price, R.D.; Berry, M.G.; Navsaria, H.A. Hyaluronic acid: The scientific and clinical evidence. J. Plast. Reconstr. Aesthetic Surg. 2007, 60, 1110–1119. [Google Scholar] [CrossRef]
- Robert, L. Hyaluronan, a truly “youthful” polysaccharide. Its medical applications. Pathol. Biol. 2015, 63, 32–34. [Google Scholar] [CrossRef]
- Andre, P. Hyaluronic acid and its use as a “rejuvenation” agent in cosmetic dermatology. Semin. Cutan. Med. Surg. 2004, 23, 218–222. [Google Scholar] [CrossRef] [PubMed]
- Witting, M.; Boreham, A.; Brodwolf, R.; Vávrová, K.; Alexiev, U.; Friess, W.; Hedtrich, S. Interactions of hyaluronic acid with the skin and implications for the dermal delivery of biomacromolecules. Mol. Pharm. 2015, 12, 1391–1401. [Google Scholar] [CrossRef] [PubMed]
- Brown, M.B.; Jones, S.A. Hyaluronic acid: A unique topical vehicle for the localized delivery of drugs to the skin. J. Eur. Acad. Dermatol. Venereol. 2005, 19, 308–318. [Google Scholar] [CrossRef] [PubMed]
- Voigt, J.; Driver, V.R. Hyaluronic acid and wound healing. Wound Repair Regen. 2012, 20, 317–331. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, E.L.; Roberts, J.L.; Moseley, R.; Griffiths, P.C.; Thomas, D.W. Evaluation of the physical and biological properties of hyaluronan and hyaluronan fragments. Int. J. Pharm. 2011, 420, 84–92. [Google Scholar] [CrossRef] [PubMed]
- Kakehi, K.; Kinoshita, M.; Yasueda, S.I. Hyaluronic acid: Separation and biological implications. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2003, 797, 347–355. [Google Scholar] [CrossRef]
- Girish, K.S.; Kemparaju, K. The magic glue hyaluronan and its eraser hyaluronidase: A biological overview. Life Sci. 2007, 80, 1921–1943. [Google Scholar] [CrossRef]
- Fallacara, A.; Baldini, E.; Manfredini, S.; Vertuani, S. Hyaluronic acid in the third millennium. Polymers 2018, 10, 701. [Google Scholar] [CrossRef] [Green Version]
- Salwowska, N.M.; Bebenek, K.A.; Żądło, D.A.; Wcisło-Dziadecka, D.L. Physiochemical properties and application of hyaluronic acid: A systematic review. J. Cosmet. Dermatol. 2016, 15, 520–526. [Google Scholar] [CrossRef]
- Altman, R.D.; Manjoo, A.; Fierlinger, A.; Niazi, F.; Nicholls, M. The mechanism of action for hyaluronic acid treatment in the osteoarthritic knee: A systematic review. BMC Musculoskelet. Disord. 2015, 16, 321. [Google Scholar] [CrossRef] [Green Version]
- Gupta, R.C.; Lall, R.; Srivastava, A.; Sinha, A. Hyaluronic Acid: Molecular Mechanisms and Therapeutic Trajectory. Front. Vet. Sci. 2019, 6, 1–24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Becker, L.C.; Bergfeld, W.F.; Belsito, D.V.; Klaassen, C.D.; Marks, J.G.; Shank, R.C.; Slaga, T.J.; Snyder, P.W.; Ingredient, C.; Expert, R.; et al. Final Report of the Safety Assessment of Hyaluronic Acid, Potassium Hyaluronate, and Sodium Hyaluronate. Int. J. Toxicol. 2009, 28, 5–67. [Google Scholar] [CrossRef]
- Scuri, M.; Abraham, W.M. Hyaluronan blocks human neutrophil elastase (HNE)-induced airway responses in sheep. Pulm. Pharmacol. Ther. 2003, 16, 335–340. [Google Scholar] [CrossRef]
- Rothe, H.; Fautz, R.; Gerber, E.; Neumann, L.; Rettinger, K.; Schuh, W.; Gronewold, C. Special aspects of cosmetic spray safety evaluations: Principles on inhalation risk assessment. Toxicol. Lett. 2011, 205, 97–104. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Global Hyaluronic Acid Products Market Size, Share, Trends and Growth Analysis Report—Segmented By Product Type, Application and Region—Industry Forecast (2020 to 2025). Available online: https://www.marketdataforecast.com/market-reports/hyaluronic-acid-products-market (accessed on 15 April 2020).
- Vasvani, S.; Kulkarni, P.; Rawtani, D. Hyaluronic acid: A review on its biology, aspects of drug delivery, route of administrations and a special emphasis on its approved marketed products and recent clinical studies. Int. J. Biol. Macromol. 2019, 151, 1012–1029. [Google Scholar] [CrossRef]
- Nien, H.K.; Yap, W.H.; Lai, C.; Lim, H.; Goh, B.H. Hyaluronic Acid-Mediated Drug Delivery System Targeting for In fl ammatory Skin Diseases: A Mini Review. Front. Pharmacol. 2020, 11, 1–8. [Google Scholar] [CrossRef]
- Bayer, I.S. Hyaluronic Acid and Controlled Release: A Review. Molecules 2020, 25, 2649. [Google Scholar] [CrossRef] [PubMed]
- Dubashynskaya, N.; Poshina, D.; Raik, S.; Urtti, A.; Skorik, Y.A. Polysaccharides in Ocular Drug Delivery. Pharmaceutics 2019, 12, 22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, G.; Huang, H. Application of hyaluronic acid as carriers in drug delivery. Drug Deliv. 2018, 25, 766–772. [Google Scholar] [CrossRef]
- Huang, G.; Huang, H. Hyaluronic acid-based biopharmaceutical delivery and tumor-targeted drug delivery system. J. Control. Release 2018, 278, 122–126. [Google Scholar] [CrossRef] [PubMed]
- Trombino, S.; Servidio, C.; Curcio, F.; Cassano, R. Strategies for Hyaluronic Acid-Based Hydrogel Design in Drug Delivery. Pharmaceutics 2019, 11, 407. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, S.Y.; Kang, M.S.; Jeong, W.Y.; Han, D.; Kim, K.S. Hyaluronic Acid-Based Theranostic Nanomedicines for Targeted Cancer Therapy. Cancers 2020, 12, 940. [Google Scholar] [CrossRef] [Green Version]
- Kim, J.H.; Moon, M.J.; Kim, D.Y.; Heo, Y.; Suk, H.H.; Jeong, Y.Y. Hyaluronic Acid-Based Nanomaterials for Cancer Therapy. Polymers 2018, 10, 1133. [Google Scholar] [CrossRef] [Green Version]
- Kim, S.; Moon, M.; Surendran, S.P.; Jeong, Y.Y. Biomedical Applications of Hyaluronic Acid-Based Nanomaterials in Hyperthermic Cancer Therapy. Pharmaceutics 2019, 11, 306. [Google Scholar] [CrossRef] [Green Version]
- Kim, K.; Choi, H.; Choi, E.S.; Park, M. Hyaluronic Acid-Coated Nanomedicine for Targeted Cancer Therapy. Pharmaceutics 2019, 11, 301. [Google Scholar] [CrossRef] [Green Version]
- Li, M.; Sun, J.; Zhang, W.; Zhao, Y.; Zhang, S.; Zhang, S.; Car, C. Drug delivery systems based on CD44-targeted glycosaminoglycans for cancer therapy. Carbohydr. Polym. 2021, 251, 117103. [Google Scholar] [CrossRef]
- Chis, A.A.; Dobrea, C.; Morgovan, C.; Arseniu, A.M.; Rus, L.L.; Butuca, A.; Juncan, A.M.; Totan, M.; Vonica-tincu, A.L.; Cormos, G.; et al. Applications and Limitations of Dendrimers in Biomedicine. Molecules 2020, 25, 3982. [Google Scholar] [CrossRef] [PubMed]
- Wickens, J.M.; Alsaab, H.O.; Kesharwani, P.; Bhise, K.; Amin, M.C.I.; Tekade, R.K.; Gupta, U.; Iyer, A.K. Recent advances in hyaluronic acid-decorated nanocarriers for targeted cancer therapy. Drug Discov. Today 2016, 22, 665–680. [Google Scholar] [CrossRef] [Green Version]
- Litwiniuk, M.; Krejner-Bienias, A.; Gauto, A.R.; Tomasz, G. Hyaluronic Acid in Inflammation and Tissue Regeneration. Wounds 2016, 28, 78–88. [Google Scholar] [PubMed]
- Schneider, H.P.; Landsman, A. Preclinical and Clinical Studies of Hyaluronic Acid in Wound Care: A Case Series and Literature Review. Wounds 2019, 31, 41–48. [Google Scholar] [PubMed]
- Graça, M.F.P.; Miguel, S.P.; Cabral, C.S.D.; Correia, I.J. Hyaluronic acid—Based wound dressings: A review. Carbohydr. Polym. 2020, 241, 116364. [Google Scholar] [CrossRef]
- Abatangelo, G.; Vindigni, V.; Avruscio, G.; Pandis, L.; Brun, P. Hyaluronic Acid: Redefining Its Role. Cells 2020, 9, 1743. [Google Scholar] [CrossRef]
- Ahmadian, E.; Dizaj, S.M.; Eftekhari, A.; Dalir, E.; Vahedi, P.; Hasanzadeh, A.; Samiei, M. The Potential Applications of Hyaluronic Acid Hydrogels in Biomedicine. Drug Res. 2020, 70, 6–11. [Google Scholar] [CrossRef] [PubMed]
- Sahana, T.G.; Rekha, P.D. Biopolymers: Applications in wound healing and skin tissue engineering. Mol. Biol. Rep. 2018, 45, 2857–2867. [Google Scholar] [CrossRef] [PubMed]
- Shaharudin, A.; Aziz, Z. Effectiveness of hyaluronic acid and its derivatives on chronic wounds: A systematic review. J. Wound Care 2016, 25, 585–592. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vigani, B.; Rossi, S.; Sandri, G.; Bonferoni, M.C.; Caramella, C.M.; Ferrari, F. Expert Opinion on Drug Delivery Hyaluronic acid and chitosan-based nanosystems: A new dressing generation for wound care wound care. Expert Opin. Drug Deliv. 2019, 16, 715–740. [Google Scholar] [CrossRef]
- Al-Khateeb, R.; Olszewska-Czyz, I. Heliyon Biological molecules in dental applications: Hyaluronic acid as a companion biomaterial for diverse dental applications. Heliyon 2020, 6, e03722. [Google Scholar] [CrossRef]
- Casale, M.; Moffa, A.; Vella, P.; Sabatino, L.; Capuano, F.; Salvinelli, B.; Lopez, M.A.; Carinci, F.; Salvinelli, F. Hyaluronic acid: Perspectives in dentistry. A systematic review. Int. J. Immunopathol. Pharmacol. 2016, 29, 572–582. [Google Scholar] [CrossRef]
- Vasilyev, A.V.; Kuznetsova, V.S.; Bukharova, T.B.; Grigoriev, T.E.; Zagoskin, Y.; Korolenkova, M.V.; Zorina, O.A.; Chvalun, S.N.; Goldshtein, D.V.; Kulakov, A.A. Development prospects of curable osteoplastic materials in dentistry and maxillofacial surgery. Heliyon 2020, 6, e04686. [Google Scholar] [CrossRef]
- Zhao, N.; Wang, X.; Qin, L.; Zhai, M.; Yuan, J.; Chen, J.; Li, D. Effect of hyaluronic acid in bone formation and its applications in dentistry. J. Biomed. Mater. Res. Part A 2016, 104, 1560–1569. [Google Scholar] [CrossRef]
- Carracedo, G.; Villa-Collar, C.; Martin-Gil, A.; Serramito, M.; Santamaria, L. Comparison Between Viscous Teardrops and Saline Solution to Fill Orthokeratology Contact Lenses Before Overnight Wear. Eye Contact Lens Sci. Clin. Pract. 2017, 44, S307–S311. [Google Scholar] [CrossRef]
- Lequeux, I.; Ducasse, E.; Jouenne, T.; Thebault, P. Addition of antimicrobial properties to hyaluronic acid by grafting of antimicrobial peptide. Eur. Polym. J. 2014, 51, 182–190. [Google Scholar] [CrossRef]
- Malvankar-Mehta, M.S.; Fu, A.; Subramanian, Y.; Hutnik, C. Impact of Ophthalmic Viscosurgical Devices in Cataract Surgery. J. Ophthalmol. 2020, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Vandermeer, G.; Chamy, Y.; Pisella, P.-J. Comparison of objective optical quality measured by double-pass aberrometry in patients with moderate dry eye: Normal saline vs. artificial tears: A pilot study. J. Fr. Ophtalmol. 2018, 41, e51–e57. [Google Scholar] [CrossRef]
- Zhang, Z.; Suner, S.S.; Blake, D.A.; Ramesh, A.S.; Sahiner, N. Antimicrobial activity and biocompatibility of slow-release hyaluronic acid- antibiotic conjugated particles. Int. J. Pharm. 2020, 576, 119024. [Google Scholar] [CrossRef]
- Baboolal, T.G.; Mastbergen, S.C.; Jones, E.; Calder, S.J.; Lafeber, F.P.J.G.; Mcgonagle, D. Synovial fluid hyaluronan mediates MSC attachment to cartilage, a potential novel mechanism contributing to cartilage repair in osteoarthritis using knee joint distraction. Ann. Rheum. Dis. 2015, 75, 908–915. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, C.; Cao, Z.; Li, W.; Liu, R.; Chen, Y.; Song, Y.; Liu, G.; Song, Z.; Liu, Z.; Lu, C.; et al. A review on the wide range applications of hyaluronic acid as a promising rejuvenating biomacromolecule in the treatments of bone related diseases. Int. J. Biol. Macromol. 2020, 165, 1264–1275. [Google Scholar] [CrossRef]
- Snetkov, P.; Zakharova, K.; Morozkina, S.; Olekhnovich, R.; Uspenskaya, M. Hyaluronic Acid: The Influence of Molecular Weight on Structural, Physical, Physico-Chemical, and Degradable Properties of Biopolymer. Polymers 2020, 12, 1800. [Google Scholar] [CrossRef] [PubMed]
- Kosiński, J.; Jarecki, J.; Przepiórka-Kosińska, J.; Ratajczak, M. Hyaluronic Acid in Orthopedics. Wiad Lek. 2020, LXXIII, 1878–1881. [Google Scholar] [CrossRef]
- Van de Merwe, J.P.; Nordling, J.; Bouchelouche, P.; Bouchelouche, K.; Cervigni, M.; Kurosch Daha, L.; Elneil, S.; Fall, M.; Hohlbrugger, G.; Irwin, P.; et al. Diagnostic Criteria, Classification, and Nomenclature for Painful Bladder Syndrome/Interstitial Cystitis: An ESSIC Proposal. Eur. Urol. 2008, 53, 60–67. [Google Scholar] [CrossRef]
- Arslan, B.; Gönültaş, S.; Gökmen, E.; Özman, O.; Asım Avci, M.; Özdemir, E. Outcomes of intravesical chondroitin-sulfate and combined hyaluronic-acid/chondroitin-sulfate therapy on female sexual function in bladder pain syndrome. Int. Urogynecol. J. 2019, 30, 1857–1862. [Google Scholar] [CrossRef]
- Pyo, J.-S.; Cho, W.J. Systematic Review and Meta-Analysis of Intravesical Hyaluronic Acid and Hyaluronic Acid/Chondroitin Sulfate Instillation for Interstitial Cystitis/Painful Bladder Syndrome. Cell. Physiol. Biochem. 2016, 39, 1618–1625. [Google Scholar] [CrossRef] [Green Version]
- Riedl, C.R.; Engelhardt, P.F.; Daha, K.L.; Morakis, N.; Pflüger, H. Hyaluronan treatment of interstitial cystitis/painful bladder syndrome. Int. Urogynecol. J. 2008, 19, 717–721. [Google Scholar] [CrossRef]
- Edwards, A.; Peters, C.A. Managing vesicoureteral reflux in children: Making sense of all the data. F1000Research 2019, 8, F1000. [Google Scholar] [CrossRef] [Green Version]
- Kim, S.W.; Lee, Y.S.; Han, S.W. Endoscopic injection therapy. Investig. Clin. Urol. 2017, 58, S38–S45. [Google Scholar] [CrossRef] [Green Version]
- Voynow, J.A.; Zheng, S.; Kummarapurugu, A.B. Glycosaminoglycans as Multifunctional Anti-Elastase and Anti-In fl ammatory Drugs in Cystic Fibrosis Lung Disease. Front. Pharmacol. 2020, 11, 1011. [Google Scholar] [CrossRef]
- Máiz Carro, L.; Martínez-García, M.A. Use of Hyaluronic Acid (HA) in Chronic Airway Diseases. Cells 2020, 9, 2210. [Google Scholar] [CrossRef]
- Fong, E.; Garcia, M.; Woods, C.M.; Ooi, E. Hyaluronic acid for post sinus surgery care: Systematic review and meta-analysis. J. Laryngol. Otol. 2017, 131, S2–S11. [Google Scholar] [CrossRef]
- Pignataro, L.; Marchisio, P.; Ibba, T.; Torretta, S. Topically administered hyaluronic acid in the upper airway: A narrative review. Immunopathol. Pharmacol. 2018, 32. [Google Scholar] [CrossRef]
- Abi Zeid Daou, C.; Bassim, M. Hyaluronic acid in otology: Its uses, advantages and drawbacks—A review. Am. J. Otolaryngol. 2020, 41, 102375. [Google Scholar] [CrossRef]
- Baumann, L. How to Use Oral and Topical Cosmeceuticals to Prevent and Treat Skin Aging. Facial Plast. Surg. Clin. N. Am. 2018, 26, 407–413. [Google Scholar] [CrossRef]
- Genovese, L.; Sibilla, S. Innovative Nutraceutical Approaches to Counteract the Signs of Aging. In Textbook of Aging Skin; Farage, M.A., Miller, K.W., Maibach, H.I., Eds.; Springer: Berlin/Heidelberg, Germany, 2017; pp. 1967–1991. ISBN 9783662473986. [Google Scholar]
- Janiš, R.; Pata, V.; Egner, P.; Pavlačková, J.; Zapletalová, A.; Kejlová, K. Comparison of metrological techniques for evaluation of the impact of a cosmetic product containing hyaluronic acid on the properties of skin surface. Biointerphases 2017, 12, 021006. [Google Scholar] [CrossRef]
- Papakonstantinou, E.; Roth, M.; Karakiulakis, G. Hyaluronic acid: A key molecule in skin aging. Dermatoendocrinology 2012, 4. [Google Scholar] [CrossRef] [Green Version]
- Nobile, V.; Buonocore, D.; Michelotti, A.; Marzatico, F. Anti-aging and filling efficacy of six types hyaluronic acid based dermo-cosmetic treatment: Double blind, randomized clinical trial of efficacy and safety. J. Cosmet. Dermatol. 2014, 13, 277–287. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sakulwech, S.; Lourith, N.; Ruktanonchai, U.; Kanlayavattanakul, M. Preparation and characterization of nanoparticles from quaternized cyclodextrin-grafted chitosan associated with hyaluronic acid for cosmetics. Asian J. Pharm. Sci. 2018, 13, 498–504. [Google Scholar] [CrossRef]
- Mondon, P.; Doridot, E.; Ringenbach, C.; Gracioso, O. Hyaluronic acid: History and future potential. Pers. Care 2015, 6, 27–30. [Google Scholar]
- Neuman, M.G.; Nanau, R.M.; Oruña-Sanchez, L.; Coto, G. Hyaluronic acid and wound healing. J. Pharm. Pharm. Sci. 2015, 18, 53–60. [Google Scholar] [CrossRef] [Green Version]
- Elsner, P.; Maibach, H.I. Cosmeceuticals: Drugs vs. Cosmetics, 1st ed.; Marcel Dekker: New York, NY, USA, 2000; Volume 23, ISBN 0824703057. [Google Scholar]
- Manuskiatti, W.; Maibach, H.I. Hyaluronic acid and skin: Wound healing and aging. Int. J. Dermatol. 1996, 35, 539–544. [Google Scholar] [CrossRef]
- Oh, J.H.; Kim, Y.K.; Jung, J.Y.; Shin, J.; Chung, J.H. Changes in glycosaminoglycans and related proteoglycans in intrinsically aged human skin in vivo. Exp. Dermatol. 2011, 20, 454–456. [Google Scholar] [CrossRef]
- Guaitolini, E.; Cavezzi, A.; Cocchi, S.; Roberto, C. Randomized, Placebo-controlled Study of a Nutraceutical Based on Hyaluronic Acid, L-carnosine, and Methylsulfonylmethane in Facial Skin Aesthetics and Well-being. J. Clin. Aesthet. Dermatol. 2021, 12, 40–45. [Google Scholar]
- Kawada, C.; Yoshida, T.; Yoshida, H.; Matsuoka, R.; Sakamoto, W.; Odanaka, W.; Sato, T.; Yamasaki, T.; Kanemitsu, T.; Masuda, Y.; et al. Ingested hyaluronan moisturizes dry skin. Nutr. J. 2014, 13, 70. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kawada, C.; Yoshida, T.; Yoshida, H.; Sakamoto, W.; Odanaka, W.; Sato, T.; Yamasaki, T.; Kanemitsu, T.; Masuda, Y.; Urushibata, O. Ingestion of hyaluronans (molecular weights 800 k and 300 k) improves dry skin conditions: A randomized, double blind, controlled study. J. Clin. Biochem. Nutr. 2015, 56, 66–73. [Google Scholar] [CrossRef] [Green Version]
- Baumann, L. Cosmetic Dermatology. Principles and Practice, 2nd ed.; McGraw-Hill: New York, NY, USA, 2009; ISBN 9780071641289. [Google Scholar]
- Gaffney, J.; Matou-Nasri, S.; Grau-Olivares, M.; Slevin, M. Therapeutic applications of hyaluronan. Mol. Biosyst. 2010, 6, 437–443. [Google Scholar] [CrossRef]
- Brown, T.J.; Alcorn, D.; Fraser, J.R.E. Absorption of Hyaluronan Applied to the Surface of Intact Skin. J. Investig. Dermatol. 1999, 113, 740–746. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schiraldi, C.; La Gatta, A.; De Rosa, M. Biotechnological Production and Application of Hyaluronan. In Biopolymers; Elnashar, M.M., Ed.; InTech Europe: Rijeka, Croatia, 2010; pp. 388–412. ISBN 9789533071091. [Google Scholar]
- Essendoubi, M.; Gobinet, C.; Reynaud, R.; Angiboust, J.F.; Manfait, M.; Piot, O. Human skin penetration of hyaluronic acid of different molecular weights as probed by Raman spectroscopy. Ski. Res. Technol. 2016, 22, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Bukhari, N.S.; Roswandi, N.L.; Waqas, M.; Habib, H.; Hussain, F.; Khan, S.; Sohail, M.; Ramli, N.A.; Thu, H.E.; Hussain, Z. Hyaluronic acid, a promising skin rejuvenating biomedicine: A review of recent updates and pre-clinical and clinical investigations on cosmetic and nutricosmetic effects. Int. J. Biol. Macromol. 2018, 120 Pt B, 1682–1695. [Google Scholar] [CrossRef]
- Morro, G.; Morvan, P.-Y.; Vallee, R. Epidermal hyaluronic acid: A new look at hydration. Pers. Care 2013, 11, 56–58. [Google Scholar]
- Tammi, R.; Säämämen, A.-M.; Maibach, H.I.; Tammi, M. Degradation of Newly Synthesized High Molecular Mass Hyaluronan in the Epidermal and Dermal Compartments of Human Skin in Organ Culture. J. Investig. Dermatol. 1991, 97, 126–130. [Google Scholar] [CrossRef] [Green Version]
- Rao, S.; Muia, F.; Bennett, S.; Lonza, J.V.G. Improving barrier function to address premature ageing. Pers. Care 2013, 9, 77–82. [Google Scholar]
- Pavicic, T.; Gauglitz, G.G.; Lersch, P.; Schwach-Abdellaoui, K.; Malle, B.; Korting, H.C.; Farwick, M. Efficacy of Cream-Based Novel Formulations of Hyaluronic Acid of Different Molecular Weights in Anti-Wrinkle Treatment. J. Drugs Dermatol. 2011, 10, 990–1000. [Google Scholar]
- Souto, E.B.; Fernandes, A.R.; Martins-Gomes, C.; Coutinho, T.E.; Durazzo, A.; Lucarini, M.; Souto, S.B.; Silva, A.M.; Santini, A. Nanomaterials for skin delivery of cosmeceuticals and pharmaceuticals. Appl. Sci. 2020, 10, 1594. [Google Scholar] [CrossRef] [Green Version]
- Dayan, N. Skin Aging Handbook. An Integrated Approach to Biochemistry and Product Development; Dayan, N., Ed.; William Andrew Inc.: New York, NY, USA, 2008; ISBN 9780815515845. [Google Scholar]
- Weindl, G.; Schaller, M.; Schäfer-Korting, M.; Korting, H.C. Hyaluronic Acid in the Treatment and Prevention of Skin Diseases: Molecular Biological, Pharmaceutical and Clinical Aspects. Skin Pharmacol. Physiol. 2004, 17, 207–213. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.H.; Oh, J.H.; Chung, J.H. Glycosaminoglycan and proteoglycan in skin aging. J. Dermatol. Sci. 2016, 83, 174–181. [Google Scholar] [CrossRef]
- Mourelle, M.; Gonzalez, J. Can a cosmetic have similar impact as dermal fillers? Pers. Care 2015, 11, 73–76. [Google Scholar]
- Fraser, J.R.E.; Laurent, T.C.; Laurent, U.B.G. Hyaluronan: Its nature, distribution, functions and turnover. J. Intern. Med. 1997, 242, 27–33. [Google Scholar] [CrossRef]
- Tzellos, T.G.; Klagas, I.; Vahtsevanos, K.; Triaridis, S.; Printza, A.; Kyrgidis, A.; Karakiulakis, G.; Zouboulis, C.C.; Papakonstantinou, E. Extrinsic ageing in the human skin is associated with alterations in the expression of hyaluronic acid and its metabolizing enzymes. Exp. Dermatol. 2009, 18, 1028–1035. [Google Scholar] [CrossRef]
- Olejnik, A.; Gościańska, J.; Nowak, I. Significance of hyaluronic acid in cosmetic industry and aesthetic medicine. Chemik 2012, 66, 129–135. [Google Scholar]
- Haeusler, H. Efficacy of Hyaluronic Acid Gel to Improve Skin Properties. SOFW J. 2015, 9, 16–18. [Google Scholar]
- Burgess, C.M. Soft Tissue Augmentation. In Cosmetic Dermatology; Burgess, C.M., Ed.; Springer: Berlin/Heidelberg, Germany, 2005; pp. 93–109. ISBN 3540230645. [Google Scholar]
- Cutting, K.F. Wound healing through synergy of hyaluronan and an iodine complex. J. Wound Care 2011, 20, 424–430. [Google Scholar] [CrossRef]
- Juncan, A.M. Visioline VL 650. The Images of Skin Texture before Product Application (D0) and after 28 Days (D28); Report No. 300924/19/JSHR Table 3; Courage+Khazaka Electronic GmbH: Köln, Germany, 2019. [Google Scholar]
- Reynaud, R.; Scandolera, A.; Dinant, C.; Lefèvre, F.; Bourgon, O. A new generation of oil-compatible hydrated HA. Pers. Care 2017, 9, 61–63. [Google Scholar]
- Tang, C.S.; Teo, C.-P.; Wei, K.K. Supply Chain Analysis: A Handbook on the Interaction of Information, System and Optimization; Springer Science+Business Media: New York, NY, USA, 2008; ISBN 9780387752396. [Google Scholar]
- Available online: https://www.fresh.com/us/skincare/categories/essences-serums/rose-deep-hydration-face-serum-H00003685.html (accessed on 20 May 2021).
- Available online: https://www.cultbeauty.co.uk/the-ordinary-buffet.html (accessed on 1 June 2021).
- Available online: https://www.cultbeauty.co.uk/the-ordinary-hyaluronic-acid-2-b5.html (accessed on 20 January 2021).
- Available online: https://www.apivita.com/en/intensive-care-eye-serum-10-22-01-615.html (accessed on 20 January 2021).
- Available online: https://www.farmec.eu/products/skin/hyaluronic-acid-ampoules-5-gerovital-h3-evolution-1119.html (accessed on 1 June 2021).
- Available online: https://infinitumcosmetics.ro/produs/deep-wrinkles-anti-aging-serum/ (accessed on 1 June 2021).
- Available online: https://www.skinsociety.me/collections/skin-care-anti-aging-day-night-care/products/mysterieux-mille-et-un-jours-anti-ageing-day-emulsion-combination-to-oily-skin-garancia (accessed on 15 May 2021).
- Available online: https://www.balanceme.com/gb/skincare/eye-creams/ (accessed on 1 June 2021).
- Available online: https://earthsciencebeauty.com/products/apricot-night-cream?_pos=1&_sid=7ac9e205a&_ss=r (accessed on 15 May 2021).
- Available online: http://www.cosmeticplant.com/skin-type/normal-skin/lift-up-anti-wrinkle-day-cream-with-hyaluronic-acid-liftonin-xpress-and-magnolia-extract-50-ml/ (accessed on 15 May 2021).
- Available online: https://infinitumcosmetics.ro/produs/cellular-regenerating-cream/ (accessed on 1 June 2021).
- Available online: https://www.gerocossen.ro/crema-antirid-de-zi-spf-10-hyaluron-anti-age-50-ml.html (accessed on 15 May 2021).
- Available online: https://infinitumcosmetics.ro/produs/golden-elixir-anti-ageing-cream/ (accessed on 1 June 2021).
- Available online: https://www.farmec.eu/products/skin/anti-wrinkle-cream-concentrated-with-hyaluronic-acid-3-684.html (accessed on 1 June 2021).
- Available online: https://www.arbonne.com/Pws/homeoffice/store/AMCA/product/RE9-Advanced-for-Men-Anti-Aging-Moisturizer-Broad-1094 Spectrum-SPF-15-CA-6513,8782.aspx (accessed on 15 May 2021).
- Available online: https://infinitumcosmetics.ro/produs/anti-aging-cleansing-emulsion/ (accessed on 15 May 2021).
- Available online: https://en.eauthermalejonzac.com/product/dermo-repair-cream-40-ml/ (accessed on 15 May 2021).
- Available online: https://www.everglowcosmetics.com/ (accessed on 1 June 2021).
- Available online: https://www.naturerepuliceurope.com/it/i-nostri-prodotti/ (accessed on 1 June 2021).
- Available online: https://www.dm.de/search?query=Alverde Handcreme&searchType=product (accessed on 15 May 2021).
- Available online: https://www.innisfree.com/hk/en/product/productView.do?prdSeq=16287 (accessed on 15 May 2021).
- Available online: https://www.innisfree.com/sg/en/product/productView.do?prdSeq=10837 (accessed on 15 May 2021).
- Available online: https://jjj-shop.com/etude-house-berry-aha-bright-peel-bubble-wash-review/ (accessed on 1 June 2021).
- Available online: https://www.illamasqua.com/liquid-lip-lure/11283816.html (accessed on 15 May 2021).
- Available online: https://www.clinique.com/product/1592/41442/makeup/sun-kissed-face-gelee-complexion-multitasker?size=1.0_fl_oz (accessed on 15 May 2021).
- Available online: https://www.paulandjoe-beaute.hk/ProductDetails.aspx?master_sku=APAAVN (accessed on 1 June 2021).
- Kato, A.; Koyama, J.; Shinzawa, K.; Imaeda, S.; Adachi, I.; Nash, R.J.; Fleet, G.W.J.; Shintani, M.; Takeuchi, C.; Ishikawa, F. Ginnalin B induces differentiation markers and modulates the proliferation/differentiation balance via the upregulation of NOTCH1 in human epidermal keratinocytes. Bioorg. Med. Chem. 2019, 27, 2172–2180. [Google Scholar] [CrossRef]
- Muhsinah, A.B.; Ma, H.; DaSilva, N.A.; Yuan, T.; Seeram, N.P. Bioactive Glucitol-Core Containing Gallotannins and other Phytochemicals from Silver Maple (Acer saccharinum) Leaves. Nat. Prod. Commun. 2017, 12, 83–84. [Google Scholar] [CrossRef] [Green Version]
- Liu, C.; Guo, H.; Dain, J.; Wan, Y.; Gao, X.-H.; Chen, H.-D.; Seeram, N.P.; Ma, H. Cytoprotective Effects of A Proprietary Red Maple Leaves Extract and Its Major Polyphenol, Ginnalin A, against Hydrogen Peroxide and Methylglyoxal Induced Oxidative Stress in Human Keratinocytes. Food Funct. 2020, 11, 5105–5114. [Google Scholar] [CrossRef] [PubMed]
- Ma, H.; Liu, W.; Frost, L.; Kirschenbaum, L.J.; Dain, J.A.; Seeram, N.P. Glucitol-core containing gallotannins inhibit the formation of advanced glycation end-products mediated by their antioxidant potential. Food Funct. 2016, 7, 2213–2222. [Google Scholar] [CrossRef] [PubMed]
- Santos, G.A.; Doty, M.S. IR Studies on Carrageenan of Ahnfeltia concinna, a Marine Red Alga. J. Pharm. Sci. 1975, 64, 704–1706. [Google Scholar] [CrossRef]
- Cheong, K.L.; Qiu, H.M.; Du, H.; Liu, Y.; Khan, B.M. Oligosaccharides Derived from Red Seaweed: Production, Properties, and Potential Health and Cosmetic Applications. Molecules 2018, 23, 2451. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cunha, L.; Grenha, A. Sulfated Seaweed Polysaccharides as Multifunctional Materials in Drug Delivery Applications. Mar. Drugs 2016, 14, 42. [Google Scholar] [CrossRef]
- Yun, E.J.; Lee, S.; Kim, J.H.; Kim, B.B.; Kim, H.T.; Lee, S.H.; Pelton, J.G.; Kang, N.J.; Choi, I.; Kim, K.H. Enzymatic production of 3, 6-anhydro-L-galactose from agarose and its purification and in vitro skin whitening and anti-inflammatory activities. Appl. Microbiol. Biotechnol. 2013, 97, 2961–2970. [Google Scholar] [CrossRef]
- Pimentel, F.B.; Alves, R.C.; Rodrigues, F.; Oliveira, M.B.P.P. Macroalgae-Derived Ingredients for Cosmetic Industry—An Update. Cosmetics 2018, 5, 2. [Google Scholar] [CrossRef] [Green Version]
- Verdy, C.; Branka, J.E.; Mekideche, N. Quantitative assessment of lactate and progerin production in normal human cutaneous cells during normal ageing: Effect of an Alaria esculenta extract. Int. J. Cosmet. Sci. 2011, 33, 462–466. [Google Scholar] [CrossRef]
- De la Moneda, A.; Carro, M.D.; Weisbjerg, M.R.; Roleda, M.Y.; Lind, V.; Novoa-Garrido, M.; Molina-Alcaide, E. Variability and Potential of Seaweeds as Ingredients of Ruminant Diets: An In Vitro Study. Animals 2019, 9, 851. [Google Scholar] [CrossRef] [Green Version]
- Rahnasto-Rilla, M.K.; McLoughlin, P.; Kulikowicz, T.; Doyle, M.; Bohr, V.A.; Lahtela-Kakkonen, M.; Ferrucci, L.; Hayes, M.; Moaddel, R. The Identification of a SIRT6 Activator from Brown Algae Fucus Distichus. Mar. Drugs 2017, 15, 190. [Google Scholar] [CrossRef] [Green Version]
- Couteau, C.; Coiffard, L. Seaweed Application in Cosmetics. In Seaweed in Health and Disease Prevention; Fleurence, J., Levine, I., Eds.; Elsevier, Inc.: London, UK, 2016; pp. 423–441. ISBN 9780128027936. [Google Scholar]
- Verdy, C.; Branka, J.; Mekideche, N. Melanosome transfer evaluation by quantitative measurement of Pmel 17 in human normal melanocyte-keratinocyte co-cultures: Effect of an Alaria esculenta extract. J. Cosmet. Sci. 2012, 63, 197–203. [Google Scholar]
- Rajauria, G. In-Vitro Antioxidant Properties of Lipophilic Antioxidant Compounds from 3 Brown Seaweed. Antioxidants 2019, 8, 596. [Google Scholar] [CrossRef] [Green Version]
- Heffernan, N.; Smyth, T.J.; Soler-Villa, A.; Fitzgerald, R.J.; Brunton, N.P. Phenolic content and antioxidant activity of fractions obtained from selected Irish macroalgae species (Laminaria digitata, Fucus serratus, Gracilaria gracilis and Codium fragile). J. Appl. Phycol. 2014, 27, 519–530. [Google Scholar] [CrossRef]
- Janssen Cosmetics. Ingredients Information Algae. Available online: https://www.janssen-cosmetics.com/Uploads/_UNTERGRUPPE/1590_Ocean_Treasure/1950_Ingredients_Information_Algae_Ritual.pdf (accessed on 18 March 2021).
- Guo, X.; Mei, N. Aloe vera: A review of toxicity and adverse clinical effects. J. Environ. Sci. Heal. Part C Environ. Carcinog. Ecotoxicol. Rev. 2016, 34, 77–96. [Google Scholar] [CrossRef] [PubMed]
- Cosmetic Ingredient Review Expert Panel. Final Report on the Safety Assessment of Aloe andongensis Extract, Aloe andongensis Leaf Juice, Aloe arborescens Leaf Extract, Aloe arborescens Leaf Juice, Aloe arborescens Leaf Protoplasts, Aloe barbadensis Flower Extract, Aloe barbadensis Leaf, Aloe Bar. Int. J. Toxicol. 2007, 26, 1–50. [Google Scholar] [CrossRef]
- Dal’Belo, S.E.; Rigo Gaspar, L.; Maia Campos, P.M.B.G. Moisturizing effect of cosmetic formulations containing Aloe vera extract in different concentrations assessed by skin bioengineering techniques. Skin Res. Technol. 2006, 12, 241–246. [Google Scholar] [CrossRef]
- Hamman, J.H. Composition and applications of Aloe vera leaf gel. Molecules 2008, 13, 1599–1616. [Google Scholar] [CrossRef] [Green Version]
- Herman, A. Comparison of Antimicrobial Activity of Essential Oils, Plant Extracts and Methylparaben in Cosmetic Emulsions: 2 Months Study. Indian J. Microbiol. 2014, 54, 361–364. [Google Scholar] [CrossRef] [Green Version]
- Miroddi, M.; Navarra, M.; Calapai, F.; Mancari, F.; Giofrè, S.V.; Gangemi, S.; Calapai, G. Review of clinical pharmacology of Aloe vera L. in the treatment of psoriasis. Phyther. Res. 2015, 29, 648–655. [Google Scholar] [CrossRef]
- Ganesan, P.; Choi, D.K. Current application of phytocompound-based nanocosmeceuticals for beauty and skin therapy. Int. J. Nanomed. 2016, 11, 1987–2007. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rigat, M.; Vallès, J.; D’Ambrosio, U.; Gras, A.; Iglésias, J.; Garnatje, T. Plants with topical uses in the Ripollès district (Pyrenees, Catalonia, Iberian Peninsula): Ethnobotanical survey and pharmacological validation in the literature. J. Ethnopharmacol. 2015, 164, 162–179. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Casetti, F.; Wölfle, U.; Gehring, W.; Schempp, C.M. Dermocosmetics for dry skin: A new role for botanical extracts. Skin Pharmacol. Physiol. 2011, 24, 289–293. [Google Scholar] [CrossRef]
- Beringhs, A.O.R.; Rosa, J.M.; Stulzer, H.K.; Budal, R.M.; Sonaglio, D. Green Clay and Aloe vera Peel-Off Facial Masks: Response Surface Methodology Applied to the Formulation Design. AAPS PharmSciTech. 2013, 14, 445–455. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krulj, J.; Brlek, T.; Pezo, L.; Brkljača, J.; Popović, S.; Zeković, Z.; Bodroža Solarov, M. Extraction methods of Amaranthus sp. grain oil isolation. J. Sci. Food Agric. 2016, 96, 3552–3558. [Google Scholar] [CrossRef]
- Huang, Z.R.; Lin, Y.K.; Fang, J.Y. Biological and Pharmacological Activities of Squalene and Related Compounds: Potential Uses in Cosmetic Dermatology. Molecules 2009, 14, 540–554. [Google Scholar] [CrossRef] [PubMed]
- Wołosik, K.; Knas, M.; Zalewska, A.; Niczyporuk, M.; Przystupa, A.W. The importance and perspective of plant-based squalene in cosmetology. J. Cosmet. Sci. 2013, 64, 59–65. [Google Scholar] [PubMed]
- De Vita, D.; Messore, A.; Toniolo, C.; Frezza, C.; Scipione, L.; Bertea, C.M.; Micera, M.; Di Sarno, V.; Madia, V.N.; Pindinello, I.; et al. Towards a new application of amaranth seed oil as an agent against Candida albicans. Nat. Prod. Res. 2019, 1–6. [Google Scholar] [CrossRef]
- Cho, Y.H.; Kim, J.H.; Park, S.M.; Lee, B.C.; Pyo, H.B.; Park, H.D. New cosmetic agents for skin whitening from Angelica dahurica. J. Cosmet. Sci. 2006, 57, 11–21. [Google Scholar]
- Kil, Y.; Pham, S.T.; Seo, K.E.; Jafari, M. Angelica keiskei, an emerging medicinal herb with various bioactive constituents and biological activities. Arch. Pharm. Res. 2017, 40, 655–675. [Google Scholar] [CrossRef] [PubMed]
- Son, H.-U.; Yoon, E.-K.; Cha, Y.-S.; Kim, M.-A.; Shin, Y.-K.; Kim, J.-M.; Choi, Y.-H.; Lee, S.-H. Comparison of the toxicity of aqueous and ethanol fractions of Angelica keiskei leaf using the eye irritancy test. Exp. Ther. Med. 2012, 4, 820–824. [Google Scholar] [CrossRef]
- Lee, S. Evaluation of acute skin irritation and phototoxicity by aqueous and ethanol fractions of Angelica keiskei. Exp. Ther. Med. 2012, 5, 45–50. [Google Scholar] [CrossRef]
- Paulsen, E. Contact sensitization from Compositae-containing herbal remedies and cosmetics. Contact Dermat. 2002, 47, 189–198. [Google Scholar] [CrossRef]
- Anonymous. Final Report on the Safety Assessment of Arnica Montana Extract and Arnica Montana. Int. J. Toxicol. 2001, 20, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Baumann, L.S. Less-known botanical cosmeceuticals. Dermatol. Ther. 2007, 20, 330–342. [Google Scholar] [CrossRef] [PubMed]
- Cizauskaite, U.; Bernatoniene, J. Innovative Natural ingredients-Based Multiple Emulsions: The Effect on Human Skin Moisture, Sebum Content, Pore Size and Pigmentation. Molecules 2018, 23, 1428. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vaseli-Hagh, N.; Deezagi, A.; Shahraki, M.K. Anti-aging effects of the proteins from artemia extract on human fibroblasts cell proliferation and collagen expression in induced aging conditions. Ann. Biotechnol. 2018, 3, 1015. [Google Scholar] [CrossRef]
- Macwan, C.; Patel, H.V.; Kalia, K. A comparative evaluation of in vitro antioxidant properties of bamboo Bambusa arundinacea leaves extracts. J. Cell Tissue Res. 2010, 10, 2413–2418. [Google Scholar]
- Arora, D.; Rani, A.; Sharma, A. A review on phytochemistry and ethnopharmacological aspects of genus Calendula. Pharmacogn. Rev. 2013, 7, 179–187. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jadoon, S.; Karim, S.; Asad, M.H.H.B.; Akram, M.R.; Kalsoom Khan, A.; Malik, A.; Chen, C.; Murtaza, G. Anti-Aging Potential of Phytoextract Loaded-Pharmaceutical Creams for Human Skin Cell Longetivity. Oxid. Med. Cell. Longev. 2015, 1–17. [Google Scholar] [CrossRef] [Green Version]
- Andresen, F.A. Final report on the safety assessment of Calendula officinalis extract and Calendula officinalis. Int. J. Toxicol. 2001, 20, 13–20. [Google Scholar] [CrossRef]
- Re, T.A.; Mooney, D.; Antignac, E.; Dufour, E.; Bark, I.; Srinivasan, V.; Nohynek, G. Application of the threshold of toxicological concern approach for the safety evaluation of calendula flower (Calendula officinalis) petals and extracts used in cosmetic and personal care products. Food Chem. Toxicol. 2009, 47, 1246–1254. [Google Scholar] [CrossRef] [PubMed]
- Lohani, A.; Mishra, A.K.; Verma, A. Cosmeceutical potential of geranium and calendula essential oil: Determination of antioxidant activity and in vitro sun protection factor. J. Cosmet. Dermatol. 2018, 18, 1–8. [Google Scholar] [CrossRef]
- Fonseca, Y.M.; Catini, C.D.; Vicentini, F.T.M.C.; Cardoso, J.C.; Cavalcanti De Albuquerque, R.L., Jr.; Vieira Fonseca, M.J. Efficacy of Marigold Extract-Loaded Formulations Against UV-induced Oxidative Stress. J. Pharm. Sci. 2011, 100, 2182–2193. [Google Scholar] [CrossRef]
- Akhtar, N.; Zaman, S.U.; Khan, B.A.; Amir, M.N.; Ebrahimzadeh, M.A. Calendula extract: Effects on mechanical parameters of human skin. Acta Pol. Pharm. Drug Res. 2011, 68, 693–701. [Google Scholar]
- Andersen, F.A.; Bergfeld, W.F.; Belsito, D.V.; Hill, R.A.; Klaassen, C.D.; Liebler, D.C.; Marks, J.G.; Shank, R.C.; Slaga, T.J.; Snyder, P.W. Final report of the cosmetic ingredient review expert panel amended safety assessment of Calendula officinalis-Derived cosmetic ingredients. Int. J. Toxicol. 2010, 29, 221S–243S. [Google Scholar] [CrossRef]
- Mahmood, T.; Akhtar, N. Combined Topical Application of Lotus and Green Tea Improves Facial Skin Surface Parameters. Rejuvenation Res. 2013, 16, 91–97. [Google Scholar] [CrossRef] [Green Version]
- Mahmood, T.; Akhtar, N.; Khan, B.A.; Khan, H.M.S.; Saeed, T. Outcomes of 3% green tea emulsion on skin sebum production in male volunteers. Bosn. J. Basic Med. Sci. 2010, 10, 260–264. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koch, W.; Zagórska, J.; Marzec, Z.; Kukula-Koch, W. Applications of tea (Camellia sinensis) and its Active Constituents in Cosmetics. Molecules 2019, 24, 4277. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hsu, S. Green tea and the skin. J. Am. Acad. Dermatol. 2005, 52, 1049–1059. [Google Scholar] [CrossRef] [PubMed]
- Gianeti, M.D.; Mercurio, D.G.; Maia Campos, P.M.B.G. The use of green tea extract in cosmetic formulations: Not only an antioxidant active ingredient. Dermatol. Ther. 2013, 26, 267–271. [Google Scholar] [CrossRef] [PubMed]
- Nobrega, A.T.; Wagemaker, T.A.L.; Maia Campos, P.M.B.G. Antioxidant activity of Matricaria chamomilla L. extract and clinical efficacy of cosmetic formulations containing this extract and its isolated compounds. J. Biomed. Biopharm. Res. 2013, 10, 249–261. [Google Scholar] [CrossRef]
- Srivastava, J.K.; Shankar, E.; Gupta, S. Chamomile: A herbal medicine of the past with a bright future (Review). Mol. Med. Rep. 2010, 3, 895–901. [Google Scholar] [CrossRef] [PubMed]
- Avonto, C.; Rua, D.; Lasonkar, P.B.; Chittiboyina, A.G.; Khan, I.A. Identification of a compound isolated from German chamomile (Matricaria chamomilla) with dermal sensitization potential. Toxicol. Appl. Pharmacol. 2017, 318, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Ratz-Łyko, A.; Arct, J.; Pytkowska, K. Moisturizing and Antiinflammatory Properties of Cosmetic Formulations Containing Centella asiatica Extract. Indian J. Pharm. Sci. 2016, 78, 27–33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bylka, W.; Znajdek-awiżeń, P.; Studzińska-sroka, E.; Brzezińska, M. Centella asiatica in cosmetology. Adv. Dermatology Allergol. 2013, 1, 46–49. [Google Scholar] [CrossRef]
- Lall, N.; Kishore, N.; Momtaz, S.; Hussein, A.; Naidoo, S.; Nqephe, M.; Crampton, B. Extract from Ceratonia siliqua Exhibits Depigmentation Properties. Phyther. Res. 2015, 29, 1729–1736. [Google Scholar] [CrossRef]
- Azab, A. CAROB (Ceratonia siliqua): Health, Medicine and Chemistry. Eur. Chem. Bull. 2017, 61, 456–469. [Google Scholar] [CrossRef] [Green Version]
- Krokou, A.; Stylianou, M.; Agapiou, A. Assessing the volatile profile of carob tree (Ceratonia siliqua L.). Environ. Sci. Pollut. Res. 2019. [Google Scholar] [CrossRef]
- Botto, J.-M.; Domloge, N.; Portolan, F. Cosmetic Use of a Carob Seed Extract as a Slimming Active Agent. European Patent No. EP2931231A2, 21 October 2015. [Google Scholar]
- Dosoky, N.S.; Setzer, W.N. Biological Activities and Safety of Citrus spp. Essential Oils. Int. J. Mol. Sci. 2018, 19, 1966. [Google Scholar] [CrossRef] [Green Version]
- Burnett, C.L.; Fiume, M.M.; Bergfeld, W.F.; Belsito, D.V.; Hill, R.A.; Klaassen, C.D.; Liebler, D.C.; Marks, J.G., Jr.; Shank, R.C.; Slaga, T.J.; et al. Safety Assessment of Citrus-Derived Peel Oils as Used in Cosmetics. Int. J. Toxicol. 2019, 38, 33S–59S. [Google Scholar] [CrossRef]
- Navarra, M.; Mannucci, C.; Delbò, M.; Calapai, G. Citrus bergamia essential oil: From basic research to clinical application. Front. Pharmacol. 2015, 6, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ravichandran, C.; Badgujar, P.C.; Gundev, P.; Upadhyay, A. Review of toxicological assessment of d-limonene, a food and cosmetics additive. Food Chem. Toxicol. 2018, 120, 668–680. [Google Scholar] [CrossRef] [PubMed]
- Sotiroudis, G.; Melliou, E.; Sotiroudis, T.G.; Chinou, I. Chemical Analysis, Antioxidant and Antimicrobial Activity of Three Greek Cucumber (Cucumis sativus) Cultivars. J. Food Biochem. 2009, 34, 61–78. [Google Scholar] [CrossRef]
- Fiume, M.M.; Bergfeld, W.F.; Belsito, D.V.; Hill, R.A.; Klaassen, C.D.; Liebler, D.C.; Marks, J.; Shank, R.C.; Slaga, T.J.; Snyder, P.W.; et al. Safety Assessment of Cucumis sativus (Cucumber)-Derived Ingredients as Used in Cosmetics. Int. J. Toxicol. 2014, 33, 47S–64S. [Google Scholar] [CrossRef]
- Kawahara, T.; Tsutsui, K.; Nakanishi, E.; Inoue, T.; Hamauzu, Y. Effect of the topical application of an ethanol extract of quince seeds on the development of atopic dermatitis-like symptoms in NC/Nga mice. Complement. Altern. Med. 2017, 17, 80. [Google Scholar] [CrossRef] [Green Version]
- Muzykiewicz, A.; Zielonka-brzezicka, J.; Klimowicz, A. Quince (Cydonia oblonga Mill.) as a useful source of antioxidants–antioxidant activity evaluation. Herba Pol. 2018, 64, 23–33. [Google Scholar] [CrossRef] [Green Version]
- Tamri, P.; Hemmati, A.; Boroujerdnia, G.M. Wound healing properties of quince seed mucilage: In vivo evaluation in rabbit full-thickness wound model. Int. J. Surg. 2014, 12, 843–847. [Google Scholar] [CrossRef] [Green Version]
- Monka, A.; Grygorieva, O.; Chlebo, P.; Brindza, J. Morphological and antioxidant characteristics of quince (Cydonia oblonga Mill.) and chinese quince fruit (Pseudocydonia sinensis Schneid.). Potravinarstvo 2014, 8, 333–340. [Google Scholar] [CrossRef]
- Aghmiuni, A.I.; Keshel, S.H.; Sefat, F.; Khiyavi, A.A. Quince seed mucilage-based scaffold as a smart biological substrate to mimic mechanobiological behavior of skin and promote fibroblasts proliferation and h-ASCs differentiation into keratinocytes. Int. J. Biol. Macromol. 2019, 142, 668–679. [Google Scholar] [CrossRef]
- Ghafourian, M.; Tamri, P.; Hemmati, A.A. Enhancement of Human Skin Fibroblasts Proliferation as a Result Treating With Quince Seed Mucilage. Jundishapur J. Nat. Pharm. Prod. 2015, 10, e18820. [Google Scholar] [CrossRef] [Green Version]
- Li, Y.; Huang, J.; Lu, J.; Ding, Y.; Jiang, L.; Hu, S.; Chen, J. The role and mechanism of Asian medicinal plants in treating skin pigmentary disorders. J. Ethnopharmacol. 2019, 112173. [Google Scholar] [CrossRef]
- Xu, P.; Su, S.; Tan, C.; Lai, R.; Min, Z. Effects of aqueous extracts of Ecliptae herba, Polygoni multiflori radix praeparata and Rehmanniae radix praeparata on melanogenesis and the migration of human melanocytes. J. Ethnopharmacol. 2016, 195, 89–95. [Google Scholar] [CrossRef]
- Chung, I.; Rajakumar, G.; Lee, J.; Kim, S. Ethnopharmacological uses, phytochemistry, biological activities, and biotechnological applications of Eclipta prostrata. Appl. Microbiol. Biotechnol. 2017, 101, 5247–5257. [Google Scholar] [CrossRef]
- Chan, C.; Huang, W.; Guo, H.; Wang, B.R. Potent Antioxidative and UVB Protective Effect of Water Extract of Eclipta prostrata L. Sci. World J. 2014, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Jahan, R.; Al-nahain, A.; Majumder, S.; Rahmatullah, M. Ethnopharmacological Significance of Eclipta alba (L.) Hassk. (Asteraceae). Int. Sch. Res. Not. 2014, 1–22. [Google Scholar] [CrossRef] [Green Version]
- Liu, Y.; Hwang, E.; Ngo, H.T.T.; Perumalsamy, H.; Kim, Y.J.; Li, L. Protective Effects of Euphrasia officinalis Extract against Ultraviolet B-Induced Photoaging in Normal Human Dermal Fibroblasts. Int. J. Mol. Sci. 2018, 19, 3327. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Petrichenko, V.M.; Sukhinina, T.V.; Babiyan, L.K.; Shramm, N.I. Chemical composition and antioxidant properties of biologically active compounds from Euphrasia brevipila. Pharm. Chem. J. 2006, 40, 312–316. [Google Scholar] [CrossRef]
- Bigagli, E.; Cinci, L.; D’Ambrosio, M.; Luceri, C. Pharmacological activities of an eye drop containing Matricaria chamomilla and Euphrasia officinalis extracts in UVB-induced oxidative stress and inflammation of human corneal cells. J. Photochem. Photobiol. B Biol. 2017, 173, 618–625. [Google Scholar] [CrossRef] [PubMed]
- Laekeman, G.; Houdart, M.; Vervisch, P. EMA Assessment Report on Euphrasia officinalis L. and Euphrasia rostkoviana Hayne, Herba. Available online: https://www.ema.europa.eu/en/documents/herbal-report/final-assessment-report-euphrasia-officinalis-l-euphrasia-rostkoviana-hayne-herba_en.pdf (accessed on 8 July 2020).
- Badgujar, S.B.; Patel, V.V.; Bandivdekar, A.H.; Mahajan, R.T. Traditional uses, phytochemistry and pharmacology of Ficus carica: A review. Pharm. Biol. 2014, 52, 1487–1503. [Google Scholar] [CrossRef] [Green Version]
- Khan, H.; Akhtar, N.; Ali, A. Effects of Cream Containing Ficus carica L. Fruit Extract on Skin Parameters: In vivo Evaluation. Indian J. Pharm. Sci. 2014, 76, 560–564. [Google Scholar]
- Abbasi, S.; Kamalinejad, M.; Babaie, D.; Shams, S.M.; Sadr, Z.; Gheysarif, M.; Askarig, V.R.; Rakhshandeh, H. Complementary Therapies in Medicine A new topical treatment of atopic dermatitis in pediatric patients based on Ficus carica L. (Fig): A randomized, placebo-controlled clinical trial. Complement. Ther. Med. 2017, 35, 85–91. [Google Scholar] [CrossRef]
- Azadbakht, M.; Monadi, T.; Esmaeili, Z.; Chabra, A.; Tavakoli, N. Formulation and evaluation of licorice shampoo in comparison with commercial shampoo. J. Pharm. Bioallied Sci. 2018, 10, 208–215. [Google Scholar] [CrossRef] [PubMed]
- Pastorino, G.; Cornara, L.; Rodrigues, F.; Oliveira, M.B.P.P. Liquorice (Glycyrrhiza glabra): A phytochemical and pharmacological review. Phyther. Res. 2018, 32, 2323–2339. [Google Scholar] [CrossRef] [PubMed]
- Schoelermann, A.M.; Weber, T.M.; Arrowitz, C.; Rizer, R.L.; Qian, K.; Babcock, M. Skin compatibility and ef fi cacy of a cosmetic skin care regimen with licochalcone A and 4-t-butylcyclohexanol in patients with rosacea subtype I. J. Eur. Acad. Dermatol. Venereol. 2016, 30, 21–27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Castangia, C.; Caddeo, M.; Manca, L.; Casu, L.; Latorre, A.C.; Díez-Sales, O.; Ruiz-Saurí, A.; Bacchetta, G.; Fadda, A.M.; Manconi, M. Delivery of liquorice extract by liposomes and hyalurosomes to protect the skin against oxidative stress injuries. Carbohydr. Polym. 2015, 134, 663. [Google Scholar] [CrossRef]
- Waqas, M.K.; Akhtar, N.; Mustafa, R.; Jamshaid, M.; Khan, H.M.S.; Murtaza, G. Review Dermatological and Cosmeceutical Benefits of Glycine Max (Soybean) and its Active Components. Acta Pol. Pharm. Drug Res. 2015, 72, 3–11. [Google Scholar]
- Lai, J.; Xin, C.; Zhao, Y.; Feng, B.; He, C.; Dong, Y.; Fang, Y.; Wei, S. Study of Active Ingredients in Black Soybean Sprouts and Their Safety in Cosmetic Use. Molecules 2012, 17, 11669–11679. [Google Scholar] [CrossRef]
- Bhattacharyya, T.K.; Bueller, H.; Hsia, Y.; Thomas, J.R. Dermal Histology in Mouse Skin Exposed to Cosmeceuticals. Facial Plast. Surg. 2017, 33, 545–550. [Google Scholar] [CrossRef]
- Jhan, J.; Chung, Y.; Chen, G.; Chang, C.; Lu, Y.; Hsu, C. Anthocyanin contents in the seed coat of black soya bean and their anti-human tyrosinase activity and antioxidative activity. Int. J. Cosmet. Sci. 2016, 38, 319–324. [Google Scholar] [CrossRef]
- Bazin, R.; Flament, F.; Colonna, A.; Harzic, L.; Bückle, R.; Piot, B.; Laize, F.; Kaaty, M.; König, K.; Fluhr, J.W. Clinical study on the effects of a cosmetic product on dermal extracellular matrix components using a high-resolution multiphoton tomograph. Skin Res. Technol. 2010, 16, 305–310. [Google Scholar] [CrossRef] [PubMed]
- Wallo, W.; Nebus, J.; Leyden, J.J. Efficacy of a soy moisturizer in photoaging: A double-blind, vehicle-controlled, 12-week study. J. Drugs Dermatol. 2007, 6, 917–922. [Google Scholar]
- Choi, S.; Jung, T.-D.; Cho, B.-Y.; Choi, S.-H.; Sim, W.-S.; Han, X.; Lee, S.J.; Kim, Y.-C.; Lee, O.-H. Anti-photoaging effect of fermented agricultural by-products on ultraviolet B-irradiated hairless mouse skin. Int. J. Mol. Med. 2019, 44, 559–568. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hooker, E. Final Report of the Amended Safety Assessment of PEG-5, -10, -16, -25, -30, and -40 Soy Sterol. Int. J. Toxicol. 2004, 23, 23–47. [Google Scholar] [CrossRef]
- Iijima, S.; Ito, M.; Makabe, K.; Murakami, Y.; Yokooji, T.; Matsuo, H. Case of anaphylactic reaction to soy following percutaneous sensitization by soy-based ingredients in cosmetic products. J. Dermatol. 2015, 42, 917–918. [Google Scholar] [CrossRef]
- Lutsenko, Y.; Bylka, W.; Matławska, I.; Darmohray, R. Hedera helix as a medicinal plant. Herba Pol. 2010, 56, 4–10. [Google Scholar]
- Facino, R.M.; Carini, M.; Stefani, R.; Aldini, G.; Saibene, L. Anti-Elastase and Anti-Hyaluronidase Activities of Saponins and Ruscus aculeatus: Factors Contributing to their Efficacy in the Sapogenins from Hedera helix, Aesculus hippocastanurn, and Treatment of Venous Insufficiency. Arch. Pharm. 1995, 328, 720–724. [Google Scholar] [CrossRef] [PubMed]
- Eberlin, S.; del Carmen Velazquez Pereda, M.; de Campos Dieamant, G.; Nogueira, C.; Werka, R.M.; de Souza, M.L. Effects of a Brazilian herbal compound as a cosmetic eyecare for periorbital hyperchromia (“dark circles”). J. Cosmet. Dermatol. 2009, 8, 127–135. [Google Scholar] [CrossRef]
- Mucaji, P.; Haladová, M.; Eisenreichová, E.; Sersen, F.; Ubik, K.; Granca, D. Constituents of Lilium candidum L. and their antioxidative activity. Ces. Slov. Farm. 2007, 56, 27–29. [Google Scholar]
- Golz-Berner, K.; Zastrow, L. Cosmetic Cleansing and Skin Care Preparation Containing Plant and Algae Extracts. U.S. Patent No. 6,221,372, 24 April 2001. [Google Scholar]
- Kanlayavattanakul, M.; Lourith, N. An update on cutaneous aging treatment using herbs: An update on cutaneous aging treatment using herbs. J. Cosmet. Laser Ther. 2015, 17, 343–352. [Google Scholar] [CrossRef]
- Active Concepts LLC. Safety Statement SilDerm® Conditioning (Cyclopentasiloxane & Dimethicone/Silsesquioxane Copolymer & Silk & Malva sylvestris (Mallow) Extract & Lilium candidum Bulb Extract & Lactobacillus/Eriodictyon Californicum Ferment Extract & Cymbidium grandiflorum F. Available online: https://activeconceptsllc.com/wp-content/uploads/2015/12/30341-SilDerm-Conditioning-Safety-Statement-v1.pdf (accessed on 20 March 2021).
- Bajpai, V.K.; Rahman, A.; Dung, N.T.; Huh, M.K.; Kang, S.C. In vitro Inhibition of Food Spoilage and Foodborne Pathogenic Bacteria by Essential Oil and Leaf Extracts of Magnolia liliflora Desr. J. Food Sci. 2008, 73, 314–320. [Google Scholar] [CrossRef]
- Bajpai, V.K.; Yoon, J.I.; Kang, S.C. Antioxidant and antidermatophytic activities of essential oil and extracts of Magnolia liliflora Desr. Food Chem. Toxicol. 2009, 47, 2606–2612. [Google Scholar] [CrossRef]
- Park, C.; Park, S.-Y.; Lee, S.; Kim, J.; Park, S. Analysis of Metabolites in White Flowers of Magnolia denudata Desr. and Violet Flowers of Magnolia liliiflora Desr. Molecules 2018, 23, 1558. [Google Scholar] [CrossRef] [Green Version]
- Martins, R.M.; de Alves Dias Assis, G.; De Siqueira Martins, S.; de Freitas, A.P.L.; Rochette, P.J.; Moulin, V.J.; Fonseca, M.J.V. Apple extract (Malus sp.) and rutin as photochemopreventive agents: Evaluation of UVB-induced alterations on skin biopsies and tissue-engineered skin. Rejuvenation Res. 2020, 23, 465–475. [Google Scholar] [CrossRef]
- Nešić, I.; Stojiljković, D.; Savić, S.; Tasić-Kostov, M.; Tadić, V. Stability, antioxidant activity, in vivo safety and efficacy of creams with standardized wild apple fruit extract: A comparison of conventional and biodegradable emulsifiers. Int. J. Cosmet. Sci. 2019, 41, 300–310. [Google Scholar] [CrossRef]
- Baldisserotto, A.; Malisardi, G.; Scalambra, E.; Andreotti, E.; Romagnoli, C.; Vicentini, C.B.; Manfredini, S.; Vertuani, S. Synthesis, Antioxidant and Antimicrobial Activity of a New Phloridzin Derivative for Dermo-Cosmetic Applications. Molecules 2012, 17, 13275–13289. [Google Scholar] [CrossRef] [Green Version]
- Moruś, M.; Baran, M.; Rost-Roszkowska, M.; Skotnicka-Graca, U. Plant Stem Cells as Innovation in Cosmetics. Acta Pol. Pharm. Drug Res. 2014, 71, 701–707. [Google Scholar]
- Shin, S.; Kum, H.; Ryu, D.; Kim, M.; Jung, E.; Park, D. Protective Effects of a New Phloretin Derivative against UVB-Induced Damage in Skin Cell Model and Human Volunteers. Int. J. Mol. Sci. 2014, 15, 18919–18940. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sampaio, G.G.; Leódido, G.; Machado Gonçalves, L.; Paschoa Benini, M.A. In vitro antimicrobial potential of infant mouthwashes against streptococcus mutans biofilm: A preliminary study. Indian J. Dent. Res. 2019, 30, 399–402. [Google Scholar] [CrossRef]
- Medellín-Luna, M.F. Castañeda-Delgado, J.E.; Martínez-Balderas, V.Y. Cervantes-Villagrana, A.R. Medicinal Plant Extracts and Their Use as Wound Closure Inducing Agents. J. Med. Food 2019, 22, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Braga, A.S.; Pires, J.G.; Magalhães, A.C. Effect of a mouthrinse containing Malva sylvestris on the viability and activity of microcosm biofilm and on enamel demineralization compared to known antimicrobials mouthrinses. Biofouling 2018, 34, 252–261. [Google Scholar] [CrossRef] [PubMed]
- Afshar, M.; Ravarian, B.; Zardast, M.; Adel, S.; Fard, M.H.; Valavi, M. Evaluation of cutaneous wound healing activity of Malva sylvestris aqueous extract in BALB/c mice. Iran. J. Basic Med. Sci. 2021, 18, 616–622. [Google Scholar]
- Nasiri, E.; Hosseinimehr, S.J.; Azadbakht, M.; Akbari, J.; Enayati-fard, R.; Azizi, S. Effect of Malva sylvestris cream on burn injury and wounds in rats. Avicenna J. Phytomed. 2021, 5, 341–354. [Google Scholar]
- Barros, L.; Carvalho, A.M.; Ferreira, I.C.F.R. Leaves, flowers, immature fruits and leafy flowered stems of Malva sylvestris: A comparative study of the nutraceutical potential and composition. Food Chem. Toxicol. 2010, 48, 1466–1472. [Google Scholar] [CrossRef]
- Pirbalouti, G.A.; Koohpyeh, A. Wound Healing Activity of Extracts of Malva sylvestris and Stachys lavandulifolia. Int. J. Biol. 2011, 3, 174–179. [Google Scholar] [CrossRef] [Green Version]
- Prudente, A.S.; Sponchiado, G.; Mendes, D.A.G.B.; Soley, B.S.; Cabrini, D.A.; Otuki, M.F. Pre-clinical efficacy assessment of Malva sylvestris on chronic skin inflammation. Biomed. Pharmacother. 2017, 93, 852–860. [Google Scholar] [CrossRef] [PubMed]
- Cudalbeanu, M.; Ghinea, I.O.; Furdui, B.; Dah-nouvlessounon, D.; Raclea, R.; Costache, T.; Cucolea, I.E.; Urlan, F.; Dinica, R.M. Exploring New Antioxidant and Mineral Compounds from Nymphaea alba Wild-Grown in Danube Delta Biosphere. Molecules 2018, 23, 1247. [Google Scholar] [CrossRef] [Green Version]
- Zhao, Y.; Fan, Y.-Y.; Yu, W.-G.; Wang, J.; Lu, W.; Song, X.-Q. Ultrasound-Enhanced Subcritical Fluid Extraction of Essential Oil from Nymphaea alba var and Its Antioxidant Activity. J. AOAC Int. 2019, 102, 1448–1454. [Google Scholar] [CrossRef]
- Bakr, R.O.; El-naa, M.M.; Zaghloul, S.S.; Omar, M.M. Profile of bioactive compounds in Nymphaea alba L. leaves growing in Egypt: Hepatoprotective, antioxidant and anti-inflammatory activity. BMC Complement. Altern. Med. 2017, 17, 52. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Laughlin, T.; Tan, Y.; Jarrold, B.; Chen, J.; Li, L.; Fang, B.; Zhao, W.; Tamura, M.; Matsubara, A.; Deng, G.; et al. Autophagy activators stimulate the removal of advanced glycation end products in human keratinocytes. J. Eur. Acad. Dermatol. Venereol. 2020, 34, 12–18. [Google Scholar] [CrossRef]
- Monrroy, M.; García, E.; Ríos, K.; García, J.R. Extraction and Physicochemical Characterization of Mucilage from Opuntia cochenillifera (L.) Miller. J. Chem. 2017, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Da Cruz Filho, I.J.; da Silva Barros, B.R.; de Souza Aguiar, L.M.; Navarro, C.D.C.; Ruas, J.S.; de Lorena, V.M.B.; de Moares Rocha, G.J.; Verecesi, A.E.; Moutinho Lagos de Melo, C.; Souto Maior, A.M. Lignins isolated from Prickly pear cladodes of the species Opuntia fícus-indica (Linnaeus) Miller and Opuntia cochenillifera (Linnaeus) Miller induces mice splenocytes activation, proliferation and cytokines production. Int. J. Biol. Macromol. 2019, 123, 1331–1339. [Google Scholar] [CrossRef]
- Stintzing, F.C.; Carle, R. Review Cactus stems (Opuntia spp.): A review on their chemistry, technology, and uses. Mol. Nutr. Food Res. 2005, 49, 175–194. [Google Scholar] [CrossRef]
- Aruwa, E.C.; Amoo, S.O.; Kudanga, T. Opuntia (Cactaceae) plant compounds, biological activities and prospects—A comprehensive review. Food Res. Int. 2018, 112, 328–344. [Google Scholar] [CrossRef] [PubMed]
- Kanlayavattanakul, M.; Lourith, N. Orchid Extracts and Cosmetic Benefits. In Orchids Phytochemistry, Biology and Horticulture; Mérillon, J.-M., Kodja, H., Eds.; Springer International Publishing: Cham, Switzerland, 2020; pp. 1–18. ISBN 9783030112578. [Google Scholar]
- Bose, B.; Choudhury, H.; Tandon, P.; Kumaria, S. Studies on secondary metabolite profiling, anti-inflammatory potential, in vitro photoprotective and skin-aging related enzyme inhibitory activities of Malaxis acuminata, a threatened orchid of nutraceutical importance. J. Photochem. Photobiol. B Biol. 2017, 173, 686–695. [Google Scholar] [CrossRef]
- Zhu, Y.; Pan, W.; Ku, C.F.; Zhang, H.; Tsang, S.W. Design, synthesis and evaluation of novel dihydrostilbene derivatives as potential anti-melanogenic skin-protecting agents. Eur. J. Med. Chem. 2018, 143, 1254–1260. [Google Scholar] [CrossRef]
- Hadi, H.; Razali, S.N.S.; Awadh, A.I. A Comprehensive Review of the Cosmeceutical Benefits of Vanda Species (Orchidaceae). Nat. Prod. Commun. 2015, 10, 1483–1488. [Google Scholar] [CrossRef] [Green Version]
- Tadokoro, T.; Bonte, F.; Archambault, J.C.; Cauchard, J.H.; Neveu, M.; Ozawa, K.; Noguchi, F.; Ikeda, A.; Nagamatsu, M.; Shinn, S. Whitening efficacy of plant extracts including orchid extracts on Japanese female skin with melasma and lentigo senilis. J. Dermatol. 2010, 37, 522–530. [Google Scholar] [CrossRef] [PubMed]
- MacAulay, J.C. Orchid allergy. Contact Dermat. 1987, 17, 112–113. [Google Scholar] [CrossRef] [PubMed]
- Mazzanti, G.; Braghiroli, L. Analgesic Antiinflammatory Action of Pfaffia paniculata (Martius) Kuntze. Phyther. Res. 1994, 8, 413–416. [Google Scholar] [CrossRef]
- Angelis, A.; Hubert, J.; Aligiannis, N.; Michalea, R.; Abedini, A.; Nuzillard, J.-M.; Gangloff, S.C.; Skaltsounis, A.-L.; Renault, J.-H. Bio-Guided Isolation of Methanol-Soluble by-Products and Investigation of Their Dermo-Cosmetic Properties. Molecules 2016, 21, 1586. [Google Scholar] [CrossRef] [Green Version]
- Hubert, J.; Angelis, A.; Aligiannis, N.; Rosalia, M.; Abedini, A.; Bakiri, A.; Reynaud, R.; Nuzillard, J.-M.; Gangloff, S.C.; Skaltsounis, A.-L.; et al. In Vitro Dermo-Cosmetic Evaluation of Bark Extracts from Common Temperate Trees. Planta Med. 2016, 82, 1351–1358. [Google Scholar] [CrossRef] [Green Version]
- Burčová, Z.; Kreps, F.; Greifová, M.; Jablonský, M.; Ház, A.; Schmidt, Š.; Šurina, I. Antibacterial and antifungal activity of phytosterols and methyl dehydroabietate of Norway spruce bark extracts. J. Biotechnol. 2018, 282, 18–24. [Google Scholar] [CrossRef]
- Sipponen, A.; Peltola, R.; Jokinen, J.J.; Laitinen, K.; Lohi, J.; Rautio, M.; Sipponen, P.; Lounatmaa, K. Effects of Norway Spruce (Picea abies) Resin on Cell Wall and Cell Membrane of Staphylococcus aureus. Ultrastruct. Pathol. 2009, 33, 128–135. [Google Scholar] [CrossRef]
- Jokinen, J.J.; Sipponen, A. Refined Spruce Resin to Treat Chronic Wounds: Rebirth of an Old Folkloristic Therapy. Adv. Wound Care 2016, 5, 198–207. [Google Scholar] [CrossRef] [Green Version]
- Marcati, A.; Ursu, V.A.; Laroche, C.; Soanen, N.; Marchal, L.; Jubeau, S.; Djelveh, G.; Michaud, P. Extraction and fractionation of polysaccharides and B-phycoerythrin from the microalga Porphyridium cruentum by membrane technology. Algal Res. 2014, 5, 258–263. [Google Scholar] [CrossRef]
- Arad, M.; Yaron, A. Natural pigments from red microalgae for use in foods and cosmetics. Trends Food Sci. Technol. 1992, 3, 92–97. [Google Scholar] [CrossRef]
- Servel, M.-O.; Claire, C.; Derrien, A.; Coiffard, L.; De Roeck-Holtzhauer, Y. Fatty acid composition of some Marine Microalge. Phytochemistry 1994, 36, 691–693. [Google Scholar] [CrossRef]
- Huang, J.J.; Xu, W.; Lin, S.; Cheung, P.C.-K. Phytochemical profiles of marine phytoplanktons: An evaluation of their in vitro antioxidant and anti-proliferative activities. Food Funct. 2016, 7, 5002–5017. [Google Scholar] [CrossRef]
- De Jesus Raposo, F.M.; de Morais, M.A.B.; de Morais, R.M.S.C. Marine Polysaccharides from Algae with Potential Biomedical Applications. Mar. Drugs 2015, 13, 2967–3028. [Google Scholar] [CrossRef] [PubMed]
- Mourelle, M.L.; Gómez, C.P.; Legido, J.L. The Potential Use of Marine Microalgae and Cyanobacteria in Cosmetics and Thalassotherapy. Cosmetics 2017, 4, 46. [Google Scholar] [CrossRef] [Green Version]
- Baby, A.R.; Maciel, C.P.M.; Kaneko, T.M.; Velasco, M.V.R. UV Spectrophotometric Determination of Bioflavonoids from a Semisolid Pharmaceutical Dosage Form Containing Trichilia catigua Adr. Juss and Ptychopetalum olacoides Bentham Standardized Extract: Analytical Method Validation and Statistical Procedures. J. AOAC Int. 2006, 89, 1532–1537. [Google Scholar] [CrossRef] [Green Version]
- Bogdan, C.; Iurian, S.; Tomuta, I.; Moldovan, M. Improvement of skin condition in striae distensae: Development, characterization and clinical efficacy of a cosmetic product containing Punica granatum seed oil and Croton lechleri resin extract. Drug Des. Devel. Ther. 2017, 11, 521–531. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fleck, A.; Cabral, P.F.G.; Vieira, F.F.M.; Pinheiro, D.A.; Pereira, C.R.; Santos, W.C.; Machado, T.B. Punica granatum L. Hydrogel for Wound Care Treatment: From Case Study to Phytomedicine Standardization. Molecules 2016, 21, 1059. [Google Scholar] [CrossRef] [Green Version]
- Prasad, D.; Kunnaiah, R. Punica granatum: A review on its potential role in treating periodontal disease. J. Indian Soc. Periodontol. 2014, 18, 428–432. [Google Scholar] [CrossRef]
- Javanmard, M.; Asadi-Gharneh, H.A.; Nikneshan, P. Characterization of biochemical traits of dog rose (Rosa canina L.) ecotypes in the central part of Iran. Nat. Prod. Res. 2018, 32, 1738–1743. [Google Scholar] [CrossRef] [PubMed]
- Ochando-Ibernón, G.; Schneller-Pavelescu, L.; Silvestre-Salvador, J.F. Allergic contact dermatitis caused by “Rosa mosqueta” oil. Contact Dermat. 2018, 79, 259–260. [Google Scholar] [CrossRef] [PubMed]
- Hwang, D.H.; Lee, D.Y.; Koh, P.O.; Yang, H.R.; Kang, C.; Kim, E. Rosa davurica pall. Improves Propionibacterium acnes-induced inflammatory responses in mouse ear edema model and suppresses pro-inflammatory chemokine production via MAPK and NF-κB pathways in HaCaT cells. Int. J. Mol. Sci. 2020, 21, 1717. [Google Scholar] [CrossRef] [Green Version]
- Olech, M.; Pietrzak, W.; Nowak, R. Characterization of Free and Bound Phenolic Acids and Flavonoid Aglycones in Rosa rugosa Thunb. Leaves and Achenes using LC-ESI-MS/MS-MRM Methods. Molecules 2020, 25, 1804. [Google Scholar] [CrossRef] [Green Version]
- Kılıç, S.; Okullu, S.Ö.; Kurt, Ö.; Sevinç, H.; Dündar, C.; Altınordu, F.; Türkoğlu, M. Efficacy of two plant extracts against acne vulgaris: Initial results of microbiological tests and cell culture studies. J. Cosmet. Dermatol. 2018, 10, 1061–1065. [Google Scholar] [CrossRef]
- Boskabady, M.H.; Shafei, M.N.; Saberi, Z.; Amini, S. Pharmacological effects of Rosa Damascena. Iran. J. Basic Med. Sci. 2011, 14, 295–307. [Google Scholar] [CrossRef]
- Basim, E.; Basim, H. Antibacterial activity of Rosa damascena essential oil. Fitoterapia 2003, 74, 394–396. [Google Scholar] [CrossRef]
- Baydar, N.G.; Baydar, H. Phenolic compounds, antiradical activity and antioxidant capacity of oil-bearing rose (Rosa damascena Mill.) extracts. Ind. Crops Prod. 2013, 41, 375–380. [Google Scholar] [CrossRef]
- Martínez, M.C.; Santiago, J.L.; Boso, S.; Gago, P.; Álvarez-Acero, I.; De Vega, M.E.; Martínez-Bartolomé, M.; Álvarez-Nogal, R.; Molíst, P.; Caser, M.; et al. Narcea—An unknown, ancient cultivated rose variety from northern Spain. Hortic. Res. 2020, 7, 1–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Palshetkar, A.; Pathare, N.; Jadhav, N.; Pawar, M.; Wadhwani, A.; Kulkarni, S.; Singh, K.K. In vitro anti-HIV activity of some Indian medicinal plant extracts. BMC Complement. Med. Ther. 2020, 20, 69. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Macedo, L.M.; Dos Santos, É.M.; Militão, L.; Tundisi, L.L.; Ataide, J.A.; Souto, E.B.; Mazzola, P.G. Rosemary (Rosmarinus officinalis L., syn Salvia rosmarinus Spenn.) and Its Topical Applications: A review. Plants 2020, 9, 651. [Google Scholar] [CrossRef]
- Nobile, V.; Michelotti, A.; Cestone, E.; Caturla, N.; Castillo, J.; Benavente-García, O.; Pérez-Sánchez, A.; Micol, V. Skin photoprotective and antiageing effects of a combination of rosemary (Rosmarinus officinalis) and grapefruit (Citrus paradisi) polyphenols. Food Nutr. Res. 2016, 60, 31871. [Google Scholar] [CrossRef] [Green Version]
- Miroddi, M.; Calapai, G.; Isola, S.; Minciullo, P.L.; Gangemi, S. Rosmarinus officinalis L. as cause of contact dermatitis. Allergol. Immunopathol. 2014, 42, 616–619. [Google Scholar] [CrossRef]
- Puupponen-Pimiä, R.; Nohynek, L.; Alakomi, H.-L.; Oksman-Caldentey, K.-M. Bioactive berry compounds—Novel tools against human pathogens. Appl. Microbiol. Biotechnol. 2004, 67, 8–18. [Google Scholar] [CrossRef] [PubMed]
- Hummer, K.E. Rubus Pharmacology: Antiquity to the Present. Hortic. Sci. 2010, 45, 1587–1591. [Google Scholar] [CrossRef] [Green Version]
- Final Report Plant-Derived Fatty Acid Oils as Used in Cosmetics. Available online: https://purelyprofessional.dk/wp-content/uploads/inci/persea-gratissima-oil.pdf (accessed on 15 May 2021).
- Singh, A.; Lal, U.R.; Mukhtar, H.M.; Singh, P.S.; Shah, G.; Dhawan, R.K. Phytochemical profile of sugarcane and its potential health aspects. Pharmacogn. Rev. 2015, 9, 45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alves, P.E.; Gomes, A.C.C.; Gomes, A.K.C.; Nigro, F.; Kuster, R.M.; de Freitas, Z.M.F.; Coutinho, C.S.C.; de S.B. Monteiro, M.S.; Pereira dos Santos, E.; Simas, N.K. Development and Characterization of Phytocosmetic Formulations with Saccharum officinarum. Rev. Bras. Farmacogn. 2020, 30, 406–415. [Google Scholar] [CrossRef]
- Ali, S.E.; El Gedaily, R.A.; Mocan, A.; Farag, M.A.; El-seedi, H.R. Sugarcane (Saccharum officinarum Linn.) Juice and Its Product Molasses via a Multiplex Metabolomics Approach. Molecules 2019, 24, 934. [Google Scholar] [CrossRef] [Green Version]
- Tundis, R.; Ursino, C.; Bonesi, M.; Loizzo, M.R.; Sicari, V.; Pellican, T.; Manfredi, I.L.; Figoli, A.; Cassano, A. Flower and Leaf Extracts of Sambucus nigra L.: Application of Membrane Processes to Obtain Fractions with Antioxidant and Antityrosinase Properties. Membranes 2019, 9, 127. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jarzycka, A.; Lewin, A.; Gancarz, R.; Wilk, K.A. Assessment of extracts of Helichrysum arenarium, Crataegus monogyna, Sambucus nigra in photoprotective UVA and UVB; photostability in cosmetic emulsions q. J. Photochem. Photobiol. B Biol. 2013, 128, 50–57. [Google Scholar] [CrossRef] [PubMed]
- Jarić, S.; Kostić, O.; Mataruga, Z.; Pavlović, D.; Pavlović, M.; Pavlović, P. Traditional wound-healing plants used in the Balkan region (Southeast Europe). J. Ethnopharmacol. 2017, 211, 311–328. [Google Scholar] [CrossRef] [PubMed]
- Örs, G.; İz Gülçe, S. Cytoprotective effect of a functional antipollutant blend through reducing B [a] P-induced intracellular oxidative stress and UVA exposure. Turk. J. Biol. 2018, 42, 453–462. [Google Scholar] [CrossRef]
- Lin, P.; Hwang, E.; Ngo, H.T.T.; Seo, S.A.; Yi, T.-H. Sambucus nigra L. ameliorates UVB-induced photoaging and inflammatory response in human skin keratinocytes. Cytotechnology 2019, 71, 1003–1017. [Google Scholar] [CrossRef]
- Mogoşanu, G.D.; Popescu, F.C.; Busuioc, C.J.; Pop, O.T.; Mogoantă, L.; Pârvănescu, H.; Rău, G.; Lascăr, I. Effects of a Topical Preparation Containing Sambuci Folium Extract in Experimental Model of Thermal Skin Burns on Rats. Farmacia 2014, 62, 693–703. [Google Scholar]
- Crisan, M.; David, L.; Moldovan, B.; Vulcu, A.; Dreve, S.; Perde-schrepler, M.; Tatomir, C.; Filip, G.; Bolfa, P. New nanomaterials for the improvement of psoriatic lesions. J. Mater. Chem. B 2013, 1, 3152. [Google Scholar] [CrossRef] [PubMed]
- Lall, N.; Chrysargyris, A.; Lambrechts, I.; Fibrich, B.; Van Staden, A.B.; Twilley, D.; de Canha, M.N.; Oosthuizen, C.B.; Bodiba, D.; Tzortzakis, N. Sideritis perfoliata (Subsp. Perfoliata) Nutritive Value and Its Potential Medicinal Properties. Antioxidants 2019, 8, 521. [Google Scholar] [CrossRef] [Green Version]
- Charami, M.-T.; Lazari, D.; Karioti, A.; Skaltsa, H.; Hadjipavlou-Litina, D. Souleles, C. Antioxidant and Antiinflammatory Activities of Sideritis perfoliata subsp. perfoliata (Lamiaceae). Phyther. Res. 2008, 22, 450–454. [Google Scholar] [CrossRef]
- Lytra, K.; Tomou, E.; Chrysargyris, A.; Drouza, C.; Skaltsa, H.; Tzortzakis, N. Traditionally Used Sideritis cypria Post.: Phytochemistry, Nutritional Content, Bioactive Compounds of Cultivated Populations. Front. Pharmacol. 2020, 11, 650. [Google Scholar] [CrossRef] [PubMed]
- Kirkan, B.; Locatelli, M.; Mocan, A.; Zengin, G.; Sarikurucu, C. Phenolic profile and bioactivities of Sideritis perfoliata L.: From the plant to its most active extract and its broad biological properties. Front. Pharmacol. 2020, 10, 1642. [Google Scholar] [CrossRef] [Green Version]
- Romanucci, V.; Di Fabio, G.; D’Alonzo, D.; Guaragna, A.; Scapagninib, G.; Zarrelli, A. Traditional uses, chemical composition and biological activities of Sideritis raeseri Boiss. & Heldr. J. Sci. Food Agric. 2016, 97, 373–383. [Google Scholar] [CrossRef]
- He, X.; Bai, Y.; Zhao, Z.; Wang, X.; Fang, J.; Huang, L.; Zeng, M.; Zhang, Q.; Zhang, Y.; Zheng, X. Local and traditional uses, phytochemistry, and pharmacology of Sophora japonica L.: A review. J. Ethnopharmacol. 2016, 187, 160–182. [Google Scholar] [CrossRef]
- Li, L.; Huang, T.; Lan, C.; Ding, H.; Yan, C.; Dou, Y. Protective effect of polysaccharide from Sophora japonica L. flower buds against UVB radiation in a human keratinocyte cell line (HaCaT cells). J. Photochem. Photobiol. B Biol. 2019, 191, 135–142. [Google Scholar] [CrossRef]
- Lo, Y.-H.; Lin, R.-D.; Lin, Y.-P.; Liu, Y.-L.; Lee, M.-H. Active constituents from Sophora japonica exhibiting cellular tyrosinase inhibition in human epidermal melanocytes. J. Ethnopharmacol. 2009, 124, 625–629. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.-H.; Lin, R.-D.; Hsu, F.-L.; Huang, Y.-H.; Chang, H.-C.; Huang, C.-Y.; Lee, M.-H. Cosmetic applications of selected traditional Chinese herbal medicines. J. Ethnopharmacol. 2006, 106, 353–359. [Google Scholar] [CrossRef]
- Sanguigno, L.; Minale, M.; Vannini, E.; Arato, G.; Riccio, R.; Casapullo, A.; Monti, M.C.; Riccio, R.; Formisano, S.; Di Rezo, G.; et al. Oligosaccharidic fractions derived from Triticum vulgare extract accelerate tissutal repairing processes in in vitro and in vivo models of skin lesions. J. Ethnopharmacol. 2015, 159, 198–208. [Google Scholar] [CrossRef] [Green Version]
- Tito, A.; Minale, M.; Riccio, S.; Grieco, F.; Colucci, M.G.; Apone, F. A Triticum vulgare Extract Exhibits Regenerating Activity During the Wound Healing Process. Clin. Cosmet. Investig. Dermatol. 2020, 13, 21–30. [Google Scholar] [CrossRef] [Green Version]
- D’Agostino, A.D.; Pirozzi, A.V.A.; Finamore, R.; Grieco, F.; Minale, M.; Schiraldi, C. Molecular Mechanisms at the Basis of Pharmaceutical Grade Triticum vulgare Extract Efficacy in Prompting Keratinocytes Healing. Molecules 2020, 25, 431. [Google Scholar] [CrossRef] [Green Version]
- Martini, P.; Mazzatenta, C.; Saponati, G. Efficacy and Tolerability of Fitostimoline in Two Different Forms (Soaked Gauzes and Cream) and Citrizan Gel in the Topical Treatment of Second-Degree Superficial Cutaneous Burns. Dermatol. Res. Pract. 2011, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Burnett, C.; Bergfeld, W.F.; Belsito, D.V.; Hill, R.A.; Klaassen, C.D.; Liebler, D.C.; Marks, J.G.; Shank, R.C.; Slaga, T.J.; Snyder, P.W.; et al. Safety Assessment of Hydrolyzed Wheat Protein and Hydrolyzed Wheat Gluten as Used in Cosmetics. Int. J. Toxicol. 2018, 37, 55S–66S. [Google Scholar] [CrossRef] [PubMed]
- Eom, S.Y.; Chung, C.B.; Kim, Y.S.; Kim, J.H.; Kim, K.S.; Kim, Y.H.; Park, S.H.; Hwang, Y.; Kim, K.H. Cosmeceutical properties of polysaccharides from the root bark of Ulmus davidiana var. japonica. J. Cosmet. Sci. 2006, 57, 355–367. [Google Scholar] [PubMed]
- Yang, H.H.; Son, J.-K.; Jung, B.; Zheng, M.; Kim, J.-R. Epifriedelanol from the Root Bark of Ulmus davidiana Inhibits Cellular Senescence in Human Primary Cells. Planta Med. 2011, 77, 441–449. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Choi, Y.-R.; Lee, Y.-K.; Chang, Y.H. Structural and rheological properties of pectic polysaccharide extracted from Ulmus davidiana esterified by succinic acid. Int. J. Biol. Macromol. 2018, 120, 245–254. [Google Scholar] [CrossRef]
- Svobodová, A.; Zdařilová, A.; Vostálová, J. Lonicera caerulea and Vaccinium myrtillus fruit polyphenols protect HaCaT keratinocytes against UVB-induced phototoxic stress and DNA damage. J. Dermatol. Sci. 2009, 56, 196–204. [Google Scholar] [CrossRef]
- Maramaldi, G.; Togni, S.; Di Pierro, F.; Biondi, M. A cosmeceutical formulation based on boswellic acids for the treatment of erythematous eczema and psoriasis. Clin. Cosmet. Investig. Dermatol. 2014, 7, 321–327. [Google Scholar] [CrossRef] [Green Version]
- Bucci, P.; Prieto, M.J.; Milla, L.; Calienni, M.N.; Martinez, L.; Rivarola, V.; Alonso, A.; Montanari, J. Skin penetration and UV-damage prevention by nanoberries. J. Cosmet. Dermatol. 2018, 17, 889–899. [Google Scholar] [CrossRef]
- Skarupova, D.; Vostalova, J.; Svobodova, A.R. Ultraviolet A protective potential of plant extracts and phytochemicals. Biomed. Pap. Med. Fac. Univ. Palacky. Olomouc. Czech. Repub. 2020, 164, 1–22. [Google Scholar] [CrossRef] [Green Version]
- Calò, R.; Marabini, L. Protective effect of Vaccinium myrtillus extract against UVA- and UVB-induced damage in a human keratinocyte cell line (HaCaT cells). J. Photochem. Photobiol. B Biol. 2014, 132, 27–35. [Google Scholar] [CrossRef]
- Widy-Tyszkiewicz, E. EMA Assessment Report on Vaccinium myrtillus L., Fructus. Available online: https://www.ema.europa.eu/en/documents/herbal-report/draft-assessment-report-vaccinium-myrtillus-l-fructus_en.pdf (accessed on 8 July 2020).
- Fiume, M.M.; Bergfeld, W.F.; Belsito, D.V.; Hill, R.A.; Klaassen, C.D.; Liebler, D.C.; Marks, J.G.; Shank, R.C.; Slaga, T.J.; Snyder, P.W.; et al. Safety Assessment of Vitis vinifera (Grape)-Derived Ingredients as Used in Cosmetics. Int. J. Toxicol. 2014, 33, 48S–83S. [Google Scholar] [CrossRef]
- Durazzo, A.; Lucarini, M.; Santini, A. Nutraceuticals in Human Health. Foods 2020, 9, 370. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dresch, R.R.; Dresch, M.T.K.; Biegelmeyer, R.; Argenta, D.F.; da Rocha, R.F.; Teixeira, H.F.; Moreira, J.C.F.; Henriques, A.T. Potential use of secondary products of the agri-food industry for topical formulations and comparative analysis of antioxidant activity of grape leaf polyphenols. Nat. Prod. Res. 2018, 32, 486–492. [Google Scholar] [CrossRef] [PubMed]
- Boo, Y.C. Human Skin Lightening Efficacy of Resveratrol and Its Analogs: From in Vitro Studies to Cosmetic Applications. Antioxidants 2019, 8, 332. [Google Scholar] [CrossRef] [Green Version]
- Minciullo, P.L.; Calapai, G.; Miroddi, M.; Mannucci, C.; Chinou, I.; Gangemi, S.; Schmidt, R.J. Contact dermatitis as an adverse reaction to some topically used European herbal medicinal products—Part 4: Solidago virgaurea–Vitis vinifera. Contact Dermat. 2017, 77, 67–87. [Google Scholar] [CrossRef] [PubMed]
- Enwere, N.J.; Hung, Y.-C. Some chemical and physical properties of bambara groundnut (Voundzeia subterrunea Thouars) seed and products. Int. J. Food Sci. Nutr. 1996, 47, 469–475. [Google Scholar] [CrossRef]
- Marcel, A.; Bienvenu, M.J. Chemical and phytochemical compositions of Voandzeia subterranea seeds. Pak. J. Biol. Sci. 2014, 17, 1083–1088. [Google Scholar] [CrossRef] [Green Version]
- Gilles Pauly, N. Cosmetic Composition containing an Extract from the seed of Bambara (Voandzeia subterranea) Nut. U.S. Patent No. 6,391,320, 21 May 2002. [Google Scholar]
- Roudsari, M.R.; Karimi, R.; Sohrabvandi, S.; Mortazavian, A.M. Health Effects of Probiotics on the Skin. Crit. Rev. Food Sci. Nutr. 2015, 55, 1219–1240. [Google Scholar] [CrossRef]
- Bustamante, M.; Oomah, B.D.; Oliveira, W.P.; Burgos-Díaz, C.; Rubilar, M.; Shene, C. Probiotics and prebiotics potential for the care of skin, female urogenital tract, and respiratory tract. Folia Microbiol. 2020, 65, 245–264. [Google Scholar] [CrossRef] [Green Version]
- Maguire, G. The role of microbiota, and probiotics and prebiotics in skin health. Arch. Dermatol. Res. 2017, 309, 411–421. [Google Scholar] [CrossRef]
- Al-Ghazzewi, F.H.; Tester, R.F. Impact of prebiotics and probiotics on skin health. Benef. Microbes. 2014, 5, 99–107. [Google Scholar] [CrossRef] [PubMed]
- Krutmann, J. Pre- and probiotics for human skin. J. Dermatol. Sci. 2009, 54, 1–5. [Google Scholar] [CrossRef]
- Knackstedt, R.; Knackstedt, T.; Gatherwright, J. The role of topical probiotics in skin conditions: A systematic review of animal and human studies and implications for future therapies. Exp. Dermatol. 2019, 29, 15–21. [Google Scholar] [CrossRef] [Green Version]
- Bindurani, S. Review: Probiotics in dermatology. J. Skin Sex. Transm. Dis. 2019, 1, 66–71. [Google Scholar] [CrossRef]
- Van der Hoeven, H. The skin microbiome, probiotics and skin care. Pers. Care 2017, 9, 25–27. [Google Scholar]
- Isolauri, E.; Arvola, T.; Sütas, Y.; Moilanen, E.; Salminen, S. Probiotics in the management of atopic eczema. Clin. Exp. Allergy 2000, 30, 1605–1610. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Caramia, G.; Atzei, A.; Fanos, V. Probiotics and the skin. Clin. Dermatol. 2008, 26, 4–11. [Google Scholar] [CrossRef] [PubMed]
- Mottin, V.H.M.; Suyenaga, E.S. An approach on the potential use of probiotics in the treatment of skin conditions: Acne and atopic dermatitis. Int. J. Dermatol. 2018, 57, 1425–1432. [Google Scholar] [CrossRef] [PubMed]
- Guéniche, A.; Bastien, P.; Ovigne, J.M.; Kermici, M.; Courchay, G.; Chevalier, V.; Breton, L.; Castiel-Higounenc, I. Bifidobacterium longum lysate, a new ingredient for reactive skin. Exp. Dermatol. 2010, 19, e1–e8. [Google Scholar] [CrossRef]
- Repair Complex CLR™ PF. Available online: https://www.ulprospector.com/documents/987102.pdf?bs=1382&b=90742&st=1&sl=92671889&crit=a2V5d29yZDpbQklGSURBIEZFUk1FTlQgTFlTQVRFXQ%3D%3D&k=BIFIDA%7CFERMENT%7CLYSATE&r=eu&ind=personalcare (accessed on 24 March 2021).
- Van der Hoeven, H.; Prade, H. Epidermal anti-ageing with a probiotic skin care approach. Pers. Care 2015, 9, 63–66. [Google Scholar]
- ProRenew Complex CLR™ NP. Available online: https://www.ulprospector.com/documents/1542305.pdf?bs=1382&b=736219&st=1&sl=92726643&crit=TGFjdG9jb2NjdXMgRmVybWVudCBMeXNhdGU%3D&r=eu&ind=personalcare (accessed on 24 March 2021).
- Mateu, M.; Davi, C.; Cañadas, E.; Soley, A.; Delgado, R. Sebum production and pore size finally under control. Pers. Care 2015, 4, 58–62. [Google Scholar]
- Lolou, V.; Panayiotidis, M.I. Functional Role of Probiotics and Prebiotics on Skin Health and Disease. Fermentation 2019, 5, 41. [Google Scholar] [CrossRef] [Green Version]
- Matmarine™ Biotech Ingredient G, Lipotec S.A.U. Available online: https://www.ulprospector.com/documents/1343813.pdf?bs=2316&b=525392&st=1&sl=92726092&crit=UHNldWRvYWx0ZXJvbW9uYXMgRmVybWVudCBFeHRyYWN0&r=eu&ind=personalcare (accessed on 24 March 2021).
- Ahsan, H. Immunopharmacology and immunopathology of peptides and proteins in personal products. J. Immunoass. Immunochem. 2019, 40, 439–447. [Google Scholar] [CrossRef]
- Burnett, C.L.; Heldreth, B.; Bergfeld, W.F.; Belsito, D.V.; Hill, R.A.; Klaassen, C.D.; Liebler, D.C.; Marks, J.G.J.; Shank, R.C.; Slaga, T.J.; et al. Safety Assessment of α-Amino Acids as Used in Cosmetics. Int. J. Toxicol. 2013, 32, 41S–64S. [Google Scholar] [CrossRef]
- Federici, A.; Federici, G.; Milani, M. An urea, arginine and carnosine based cream (Ureadin Rx Db ISDIN) shows greater efficacy in the treatment of severe xerosis of the feet in Type 2 diabetic patients in comparison with glycerol-based emollient cream. A randomized, assessor-blinded, controll. BMC Dermatol. 2012, 12, 16. [Google Scholar] [CrossRef] [Green Version]
- Marseglia, A.; Licari, A.; Agostinis, F.; Barcella, A.; Bonamonte, D.; Puviani, M.; Milani, M.; Marseglia, G.; Matteo, P.S. Local rhamnosoft, ceramides and L-isoleucine in atopic eczema: A randomized, placebo controlled trial. Pediatr. Allergy Immunol. Orig. 2014, 25, 271–275. [Google Scholar] [CrossRef] [Green Version]
- Lungu, C.; Considine, E.; Zahir, S.; Ponsati, B.; Arrastia, S.; Hallett, M. Pilot study of topical acetyl hexapeptide-8 in the treatment for blepharospasm in patients receiving botulinum toxin therapy. Eur. J. Neurol. 2013, 20, 515–518. [Google Scholar] [CrossRef] [Green Version]
- Lim, S.H.; Sun, Y.; Thiruvallur, T.M.; Rosa, V.; Kang, L. Enhanced Skin Permeation of Anti-wrinkle Peptides via Molecular Modification. Sci. Rep. 2018, 8, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kraeling, M.E.K.; Zhou, W.; Wang, P.; Ogunsola, O.A. In vitro skin penetration of acetyl hexapeptide-8 from a cosmetic formulation. Cutan. Ocul. Toxicol. 2014, 34, 46–52. [Google Scholar] [CrossRef]
- Campos, V.; Kalil, C.; Reinehr, C.; Canavaci, G.; Beltrao, F. Observational studies with confirmation of safety, tolerance and efficacy of a facial sterile solution for the skin rejuvenation containing hyaluronic acid, acetyl hexapeptide-8, carnitine and pyruvic acid in association to laser procedure. J. Am. Acad. Dermatol. 2017, 76, AB182. [Google Scholar] [CrossRef]
- Rull, M.; Davi, C.; Cañadas, E.; Cebrián, J.; Delgado, R. Reversing signs of ageing in mature skin. Pers. Care 2012, 9, 75–77. [Google Scholar]
- Park, J.; Jung, H.; Jang, B.; Song, H.; Han, I.; Oh, E. D-tyrosine adds an anti-melanogenic effect to cosmetic peptides. Sci. Rep. 2020, 10, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dragomirescu, A.O.; Andoni, M.; Ionescu, D.; Andrei, F. The Efficiency and Safety of Leuphasyl—A Botox-Like Peptide. Cosmetics 2014, 1, 75–81. [Google Scholar] [CrossRef] [Green Version]
- Dipeptide Diaminobutyroyl Benzylamide Diacetate. Available online: https://www.ulprospector.com/en/eu/PersonalCare/search?k=dipeptide+diaminobutyroyl benzylamide diacetate&st=1 (accessed on 24 March 2021).
- Hahn, H.J.; Jung, H.J.; Schrammek-Drusios, C.; Lee, S.N.; Kim, J.I.H.; Kwon, S.B.; An, I.-S.; An, S.; Ahn, K.J. Instrumental evaluation of anti-aging effects of cosmetic formulations containing palmitoyl peptides, Silybum marianum seed oil, vitamin E and other functional ingredients on aged human skin. Exp. Ther. Med. 2016, 12, 1171–1176. [Google Scholar] [CrossRef] [Green Version]
- Johnson, W., Jr.; Bergfeld, W.F.; Belsito, D.V.; Hill, R.A.; Klaassen, C.D.; Liebler, D.C.; James, M.G.; Shank, R.C.; Slaga, T.J.; Snyder, P.W.; et al. Safety Assessment of Tripeptide-1, Hexapeptide-12, Their Metal Salts and Fatty Acyl Derivatives, and Palmitoyl Tetrapeptide-7 as Used in Cosmetics. Int. J. Toxicol. 2018, 37, 90S–102S. [Google Scholar] [CrossRef]
- Gianeti, M.D.; Gaspar, L.R.; Bueno de Camarago Júnior, F.; Berardo Gonçalves Maia Campos, P.M. Benefits of Combinations of Vitamin A, C and E Derivatives in the Stability of Cosmetic Formulations. Molecules 2012, 17, 2219–2230. [Google Scholar] [CrossRef]
- Narda, M.; Brown, A.; Muscatelli-Groux, B.; Grimaud, J.A.; Granger, C. Epidermal and Dermal Hallmarks of Photoaging are Prevented by Treatment with Night Serum Containing Melatonin, Bakuchiol, and Ascorbyl Tetraisopalmitate: In Vitro and Ex Vivo Studies. Dermatol. Ther. 2020, 10, 191–202. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Assier, H.; Wolkenstein, P.; Grille, C.; Chosidow, O. Contact dermatitis caused by ascorbyl tetraisopalmitate in a cream used for the management of atopic dermatitis. Conta 2014, 71, 60–61. [Google Scholar] [CrossRef]
- Swinnen, I.; Goossens, A. Allergic contact dermatitis caused by ascorbyl tetraisopalmitate. Contact Dermat. 2011, 64, 241–242. [Google Scholar] [CrossRef] [PubMed]
- Wohlrab, J. Niacinamide—Mechanisms of Action and Its Topical Use in Dermatology. Skin Pharmacol. Physiol. 2014, 27, 311–315. [Google Scholar] [CrossRef] [PubMed]
- Panel, C.I.R.E. Final Report of the Safety Assessment of Niacinamide and Niacin. Int. J. Toxicol. 2014, 24, 1–31. [Google Scholar] [CrossRef]
- Pavlačková, J.; Egner, P.; Sedláček, T.; Mokrejš, P.; Sedlaříková, J.; Polášková, J. In vivo efficacy and properties of semisolid formulations containing panthenol. J. Cosmet. Dermatol. 2018, 18, 346–354. [Google Scholar] [CrossRef] [Green Version]
- Fernandes, R.A.; Santiago, L.; Gouveia, M.; Gonçalo, M. Allergic contact dermatitis caused by dexpanthenol—Probably a frequent allergen. Contact Dermat. 2018, 79, 276–280. [Google Scholar] [CrossRef]
- Miroux-Catarino, A.; Silva, L.; Amaro, C.; Viana, I. Allergic contact dermatitis caused dexpanthenol—But is that all? Contact Dermat. 2019, 81, 391–392. [Google Scholar] [CrossRef]
- Silva, S.; Ferreira, M.; Oliveira, A.S.; Magalhães, C.; Sousa, M.E.; Pinto, M.; Lobo Sousa, J.M.; Almeida, I.F. Evolution of the use of antioxidants in anti-ageing cosmetics. Int. J. Cosmet. Sci. 2019, 41, 378–386. [Google Scholar] [CrossRef] [PubMed]
- Mukherjee, S.; Date, A.; Patravale, V.; Korting, H.C.; Roeder, A.; Weindl, G. Retinoids in the treatment of skin aging: An overview of clinical efficacy and safety. Clin. Interv. Aging 2006, 1, 327–348. [Google Scholar] [CrossRef]
- Fiume, M.M.; Bergfeld, W.F.; Belsito, D.V.; Ronald, A.H.; Klaassen, C.D.; Liebler, D.C.; Marks, G.J.J.; Shank, R.C.; Slaga, T.J.; Snyder, P.W.; et al. Safety Assessment of Tocopherols and Tocotrienols as Used in Cosmetics. Int. J. Toxicol. 2018, 37, 61S–94S. [Google Scholar] [CrossRef] [Green Version]
- Ohtake, S.; Wang, Y.J. Trehalose: Current Use and Future Applications. J. Pharm. Sci. 2011, 100, 2020–2053. [Google Scholar] [CrossRef]
- Cai, X.; Seitl, I.; Mu, W.; Zhang, T.; Stressler, T.; Fischer, L.; Jiang, B. Biotechnical production of trehalose through the trehalose synthase pathway: Current status and future prospects. Appl. Microbiol. Biotechnol. 2018, 102, 2965–2976. [Google Scholar] [CrossRef]
- Cornara, L.; Biagi, M.; Xiao, J.; Burlando, B. Therapeutic Properties of Bioactive Compounds from Different Honeybee Products. Front. Pharmacol. 2017, 8. [Google Scholar] [CrossRef] [PubMed]
- Burlando, B.; Cornara, L. Honey in dermatology and skin care: A review. J. Cosmet. Dermatol. 2013, 12, 306–313. [Google Scholar] [CrossRef]
- Viuda-Martos, M.; Ruiz-Navajas, Y.; Fernández-López, J.; Pérez-Álvarez, J.A. Functional Properties of Honey, Propolis, and Royal Jelly. J. Food Sci. 2008, 73, 117–124. [Google Scholar] [CrossRef] [PubMed]
- Cole, N.; Sou, P.W.; Ngo, A.; Tsang, K.H.; Severino, J.A.J.; Arun, S.J.; Duke, C.C.; Reeve, V.E. Topical ‘Sydney’ Propolis Protects against UV-Radiation-Induced Inflammation, Lipid Peroxidation and Immune Suppression in Mouse Skin. Int. Arch. Allergy Immunol. 2010, 152, 87–97. [Google Scholar] [CrossRef]
- Duplan, H.; Questel, E.; Hernandez-Pigeon, H.; Galliano, M.F.; Caruana, A.; Ceruti, I.; Ambonati, M.; Mejean, C.; Damour, O.; Castex-Rizzi, N.; et al. Effects of Hydroxydecine® (10-hydroxy-2-decenoic acid) on skin barrier structure and function. Eur. J. Dermatol. 2011, 2, 906–915. [Google Scholar] [CrossRef]
- Park, H.M.; Hwang, E.; Lee, K.G.; Han, S.-M.; Cho, Y.; Kim, S.Y. Royal Jelly Protects Against Ultraviolet B–Induced Photoaging in Human Skin Fibroblasts via Enhancing Collagen Production. J. Med. Food 2011, 14, 899–906. [Google Scholar] [CrossRef] [Green Version]
- Rosmilah, M.; Shahnaz, M.; Patel, G.; Lock, J.; Rahman, D.; Masita, A.; Noormalin, A. Characterization of major allergens of royal jelly Apis mellifera. Trop. Biomed. 2009, 25, 243–251. [Google Scholar]
- Walgrave, S.E.; Warshaw, E.M.; Glesne, L.A. Allergic Contact Dermatitis from Propolis. Dermatitis 2005, 16, 209–215. [Google Scholar] [CrossRef] [PubMed]
- Nishinami, S.; Yoshizawa, S.; Arakawa, T.; Shiraki, K. Allantoin and hydantoin as new protein aggregation suppressors and their mechanisms of action. Int. J. Biol. Macromol. 2018, 114. [Google Scholar] [CrossRef]
- Becker, L.C.; Bergfeld, W.F.; Belsito, D.V.; Klaassen, C.D.; Marks, J.G.J.; Shank, R.C.; Slaga, T.J.; Snyder, P.W.; Andersen, F.A. Final Report of the Safety Assessment of Allantoin and Its Related Complexes. Int. J. Toxicol. 2010, 29, 84S–97S. [Google Scholar] [CrossRef]
- Angelova-Fischer, I.; Rippke, F.; Richter, D.; Filbry, A.; Arrowitz, C.; Weber, T.; Fischer, T.W.; Zillikens, D. Stand-alone Emollient Treatment Reduces Flares After Discontinuation of Topical Steroid Treatment in Atopic Dermatitis: A Double-blind, Randomized, Vehicle-controlled, Left-right Comparison Study. Acta Derm. Venereol. 2018, 98, 517–523. [Google Scholar] [CrossRef] [Green Version]
- Yilmaz, E.; Borchert, H.-H. Effect of lipid-containing, positively charged nanoemulsions on skin hydration, elasticity and erythema—An in vivo study. Int. J. Pharm. 2006, 307, 232–238. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.M.; Lee, B.-M. Safety and risk assessment of ceramide 3 in cosmetic products. Food Chem. Toxicol. 2015, 84, 8–17. [Google Scholar] [CrossRef]
- Cao, M.; Li, J.; Tang, J.; Chen, C.; Zhao, Y. Gold Nanomaterials in Consumer Cosmetics Nanoproducts: Analyses, Characterization, and Dermal Safety Assessment. Small 2016, 12, 5488–5496. [Google Scholar] [CrossRef]
- Cornier, J.; Keck, C.M.; Van de Voorde, M. Nanocosmetics. From Ideas to Products; Springer Nature Switzerland: Cham, Switzerland, 2019; ISBN 9783030165727. [Google Scholar]
- Pulit-Prociak, J.; Grabowska, A.; Majka, T.M. Safety of the application of nanosilver and nanogold in topical cosmetic preparations. Colloids Surf. B Biointerfaces 2019, 183. [Google Scholar] [CrossRef]
- Wee, Y.-J.; Kim, J.-N.; Ryu, H.-W. Biotechnological Production of Lactic Acid and Its Recent Applications. Food Technol. Biotechnol. 2006, 44, 163–172. [Google Scholar]
- Scherdin, U.; Presto, S.; Rippke, F.; Nielsen, J.; Strassner, M.; Imadojemun, A.; Gärtner, E.; Herpens, A.; Korting, H.C.; Bielfeldt, S. In vivo assessment of the efficacy of an innovative face care system in subjects with mild acne vulgaris. Int. J. Cosmet. Sci. 2004, 26, 221–229. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.; Goyal, S.; Ahmed, Q.R.; Gupta, N.; Singh, S. Effect of 82 % Lactic Acid in Treatment of Melasma. Int. Sch. Res. Not. 2014, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Fiume, Z. Final Report on the Safety Assessment of Lecithin and Hydrogenated Lecithin. Int. J. Toxicol. 2001, 20, 20–45. [Google Scholar] [CrossRef]
- Mala’Kîte™ Protective Mineral Complex. Available online: https://www.gattefosse.com/personal-care-actives/malakite (accessed on 25 March 2021).
- Lin, S.-Y.; Lin, T.-C. In Vitro Repairability for the Disordered Skin by Pyrrolidone-Carboxylate Sodium. Drug Dev. Ind. Pharm. 1994, 20, 665–676. [Google Scholar] [CrossRef]
- Fiume, M.M.; Bergfeld, W.F.; Belsito, D.V.; Hill, R.A.; Klaassen, C.D.; Liebler, D.C.; Marks, J.G., Jr.; Shank, R.C.; Slaga, T.J.; Snyder, P.W.; et al. Safety Assessment of PCA (2-Pyrrolidone-5-Carboxylic Acid) and Its Salts as Used in Cosmetics. Int. J. Toxicol. 2019, 38, 5S–11S. [Google Scholar] [CrossRef]
- Lods, L.M.; Dres, C.; Johnson, C.; Scholz, D.B.; Brooks, G.J. The future of enzymes in cosmetics. Int. J. Cosmet. Sci. 2000, 22, 85–94. [Google Scholar] [CrossRef]
- Ahmad Nasrollahi, S.; Ayatollahi, A.; Yazdanparast, T.; Samadi, A.; Hosseini, H.; Shamsipour, M.; Akhlaghi, A.A.; Yadangi, S.; Abels, C.; Firoozz, A. Comparison of linoleic acid-containing water- in-oil emulsion with urea-containing water-in-oil emulsion in the treatment of atopic dermatitis: A randomized clinical trial. Clin. Cosmet. Investig. Dermatol. 2018, 11, 21–28. [Google Scholar] [CrossRef] [Green Version]
- Yamarik, T.A.; Elmore, A.R. Final Report of the Safety Assessment of Urea. Int. J. Toxicol. 2005, 24, 1–56. [Google Scholar] [CrossRef]
- Bissonnette, R.; Maari, C.; Provost, N.; Bolduc, C.; Nigen, S.; Rougier, A.; Seite, S. A double-blind study of tolerance and efficacy of a new urea-containing moisturizer in patients with atopic dermatitis. J. Cosmet. Dermatol. 2010, 9, 16–21. [Google Scholar] [CrossRef] [PubMed]
- Celleno, L. Topical urea in skincare: A review. Dermatol. Ther. 2018, e12690. [Google Scholar] [CrossRef]






| Cosmetic Product Category/Proposed Use | Producer (Country of Origin)/Cosmetic Product Trade Name | HA Form | Other Active Ingredients Incorporated in the Cosmetic Formulation (INCI—International Nomenclature of Cosmetic Ingredients Denomination) | Cosmetic Claim | Market Segment | Reference |
|---|---|---|---|---|---|---|
| Skin care cosmetics | FRESH (USA) Deep Hydration Face Serum Serum | NaHA | Porphyridium Cruentum Extract, Pyrus Cydonia Seed Extract, Angelica Keiskei Extract, Voandzeia Subterra Nea Seed Extract, Cucumis Sativus (Cucumber) Fruit Extract, Tocopheryl Acetate | 24-h moisture | Premium Market | [108] |
| DECIEM (Canada) The ORDINARY “Buffet” Multi-Technology Peptide Serum Serum | NaHA | Lactococcus Ferment Lysate, Acetyl Hexapeptide-8, Pentapeptide-18, Palmitoyl Tripeptide-1, Palmitoyl Tetrapeptide-7, Palmitoyl Tripeptide-38, Dipeptide Diaminobutyroyl BenzylamideDiacetate, Acetylarginyltryptophyl Diphenylglycine, Allantoin, Glycine, Alanine, Serine, Valine, Isoleucine, Proline, Threonine, Histidine, Phenylalanin, Arginine, Aspartic, Acid, Trehalose, Fructose, Glucose, Maltose, Urea, Sodium PCA, PCA, Hydroxypropyl Cyclodextrin | anti-ageing | Premium Market | [109] | |
| DECIEM (Canada) THE ORDINARY Hyaluronic Acid 2% + B5 Serum | NaHA | Panthenol, Ahnfeltia Concinna Extract | moisturizing, anti-ageing | Premium Market | [110] | |
| APIVITA (Greece) 5-action Eye Serum Advanced eye care Serum | Hydrolyzed HA | Lilium Candidum Extract, PfaffiaPaniculata Extract, PtychopetalumOlacoides Extract, CopperLysinate/Prolinate, Propolis Extract, Mel Extract, Methylglucoside Phosphate, Euphrasia Officinalis Extract, Lecithin, Hydroxypropyl Cyclodextrin, Ascorbyl Tetraisopalmitate, Panthenol, SideritisPerfoliata Extract, Aloe Barbadensis Extract, SideritisScardica Extract, SideritisRaeseri Extract, Bisabolol | anti-ageing, moisturizing | Premium Market | [111] | |
| FARMEC (Romania) Hyaluronic Acid ampoules 5% Serum | NaHA | Superoxide Dismutase, Lecithin | anti-wrinkle, intensive moisturizing | Mass Market | [112] | |
| AVIVA COSMETICS (Romania) INFINITUM Deep Wrinkles Anti-Ageing Serum | Hydrolyzed HA | Aesculus Hippocastanum Extract | firming, anti-ageing | Premium Market | [113] | |
| GARANCIA (France) MYSTÉRIEUX MILLE ET UN JOURS Anti-Ageing Day Emulsion | Hydrolyzed HA | Alaria Esculenta Extract, Cyathea Cumingii Extract, Dipeptide Diaminobutyroyl Benzylamide Diacetate, Hydroxypropyl Cyclodextrin, Palmitoyl Tripeptide-38 | relax expression lines | Premium Market | [114] | |
| BALANCE ME (UK) Tinted Wonder Eye Cream Eye cream complexion perfection Day Cream | Hydrolyzed HA | Picea Abies Extract, Rubus Chamaemorus Seed Extract, Aloe Barbadensis Extract, Styrax Benzoin Extract, Rosmarinus Officinalis Extract, Vitis Vinifera Seed Extract, Tocopherol | soothing, anti-ageing | Mass Market | [115] | |
| EARTH SCIENCE (USA) Apricot Intensive night cream Night Cream | NaHA | Pyrus Malus Extract, Glycyrrhiza Glabra Extract, Glycine Soja Seed Extract, Tocopherol, Citrus Grandis Seed Extract, Calendula Officinalis Extract, Bambusa Arundinacea Extract, Sambucus Nigra Extract, Cucumis Sativus Extract, Arnica Montana Extract, Hedera Helix Extract, Lactic acid, Allantoin | reduces the appearance of fine lines and wrinkles | Mass Market | [116] | |
| COSMETIC PLANT (Romania) Lift Up—Hyaluronic Acid Day Anti-Ageing Cream Day Cream | Hydrolyzed HA | Porphyridium Cruentum Extract, Magnolia Liliflora Extract, Tocopherol | anti-ageing | Mass Market | [117] | |
| AVIVA COSMETICS (Romania) INFINITUM Cellular Regenerating Cream | Hydrolyzed HA | Aesculus Hippocastanum Extract, Tocopheryl Acetate | firming, regenerating, rejuvenating | Premium Market | [118] | |
| GEROCOSSEN (Romania) Hyaluron Anti-Age CreamSPF 10 Day Cream | NaHA | Lecithin, Tocopheryl acetate, Retinyl palmitate | anti-ageing | Mass Market | [119] | |
| AVIVA COSMETICS (Romania) INFINITUM Golden Elixir Anti-Ageing Cream SPF 15 Day Cream | Hydrolyzed HA | Aesculus Hippocastanum Extract, Gold (CI 777480), Ectoin | firming, anti-ageing, SPF 15 | Premium Market | [120] | |
| FARMEC (Romania) Anti-Wrinkle Cream Concentrated with Hyaluronic Acid 3% Day Cream | NaHA | Pseudoalteromonas Ferment Extract, Hydrolyzed Wheat Protein, Hydrolyzed Soy Protein, Tripeptide-10 Citrulline, Tripeptide-1, Lecithin, Artemia Salina Extract, Superoxide Dismutase | anti-wrinkle, line filling and smoothing, intense hydration | Mass Market | [121] | |
| ARBONNE RE9 (USA) Advanced For Men Anti-Aging Moisturizer Broad Spectrum Men Care | NaHA | Aloe Barbadensis Gel, Ceratonia Siliqua Extract, Laminaria Digitata Extract, Malachite Extract, Chamomilla Recutita Extract, Sophora Japonica Flower Extract, Tripleurospermum Maritimum Extract | moisturizing, SPF 15 | Premium Market | [122] | |
| AVIVA COSMETICS (Romania) INFINITUM Anti-Ageing Cleansing Emulsion | Hydrolyzed HA | Aesculus Hippocastanum Extract | firming, anti-ageing | Premium Market | [123] | |
| JONZAC (France) Bébé Bio Dermo-Repair Cream Baby Care | Hydrolyzed HA | Malva Sylvestris Extract, Tocopherol, Hydrogenated Lecithin | soothing, regenerating, protecting | Mass Market | [124] | |
| Body cosmetics | LES MERVEILLEUSES LADUREE (France) Sun Protection Body Cream Body Cream | NaHA | Rosa Centifolia Extract, Rosa Damascena Extract | hydrating, SPF 50 | Premium Market | [125] |
| NATURE REPUBLIC (South Korea) Ice Sun, Ice Puff Sun Sun/Sunbed Exposure | NaHA | Calendula Officinalis Extract | anti-wrinkle and skin bleftening, SPF 50 | Mass Market | [126] | |
| DM ALVERDE NATURKOSMETIK (Germany) Ivital + Hand cream | NaHA | Amaranthus Caudatus Extract, Triticum Aestivum Germ Extract, Punica Granatum Extract, Tocopherol | smoothes lines and wrinkles | Mass Market | [127] | |
| INNISFREE (South Korea) My Body Tangerine Blossom Body lotion | Hydrolyzed HA | Citrus Unshiu Peel Extract, Algae Extract, Eclipta Prostrata Extract, Orhid Extract, Camelia Sinensis Extract, Camelia Japonica Extract, Opuntia Coccinellifera Extract, Tocopherys Acetate | moisturizing | Mass Market | [128] | |
| INNISFREE (South Korea) Wine Peeling Jelly Scrub Peeling Scrub | NaHA | Vitis ViniferaExtract, Ulmus Davidiana Root Extract, Amaranthus Caudatus Extract, Centella Asiatica Extract, Ficus Carica Extract, Citrus Unshiu Extract, Orchis Extract, Camelia Sinensis Extract, Camelia Japonica Extract, Opuntia Coccinellifera Extract, Niacinamide, Allantoin, Ceramide 3 | moisturizing | Mass Market | [129] | |
| TUDE HOUSE (South Korea) Berry AHA! Bleft Peel Bubble Wash | Hydrolyzed HA | Algae Extract, Eclipta Prostrata Extract, Vaccinium Myrtillus Extract, Saccharum Officinarum Extract, Citrus Limonum Extract, Citrus Aurantium Dulcis Extract, Ulmus Davidiana Extract, Amaranthus Caudatus Extract, Acer Saccharinum Extract, Nymphaea Alba Extract, Bifida Ferment Lysate, Lecitin | bleftening | Mass Market | [130] | |
| Makeup cosmetics | ILLAMASQUA (UK) HYPNOTICA Lipe Lure Colour intense Liquid lipstick | NaHA | N | long-wearing, picture-perfect finish | Premium Market | [131] |
| CLINIQUE (USA) Sun-Kissed Face Gelee Complexion multitasker | NaHA | N | moisturizing | Premium Market | [132] | |
| PAUL& JOE (Japan) Pore SmoothingPrimer Face primer | Hydrolyzed HA | Calendula Officianlis Extract, Rosa Canina Fruit Extract, Tocopherol | moisturizing | Premium Market | [133] |
| Active Ingredient/Plant Species | Bioactive Components | Biological Role and Benefits for Skin | Toxicity of Topical Products |
|---|---|---|---|
| Acer saccharum | phenolic compounds (maplexins, ginnalins) [134,135] | increases the intracellular ceramide level stimulates the proliferation and differentiation of keratinocytes maintains thehomeostasis of the epidermis antioxidant capacity [134,136,137] | * N |
| Ahnfeltia concinna (red algae) | polysaccharides (carrageenan, agar), amino acids, minerals, vitamins, trace elements [138,139,140] | antioxidant capacity, anti-wrinkle, skin-whitening (suppresses the melanin production), skin moisturizing [139,140,141,142] | not toxic in topical applications possible irritation, sensitization, or photoreactions [142] |
| Alaria esculenta (brown algae) | polyphenols, diterpenoids, fatty acids, polysaccharides, fucosterol, fucoxhantin (e.g., retinoic acid), amino acids, minerals, vitamins, trace elements [143,144,145] | hyperpigmentation amelioration increases skin firmness and elasticity stimulates collagen and keratin synthesis, reducing the progerin production (increased in aged skin) of ‘aged’ fibroblasts skin-whitening, antioxidant capacity [142,143,146,147] anti-cellulite and antiedema activity [142,148,149,150] | possible local irritation, sensitization, or photoreactions [142] |
| Aloe sp. (Aloe barbadensis) | antraquinones, polysaccharides, phenolic compounds, organic acids [151,152,153,154] | antimicrobial activity [155,156] antioxidant capacity, anti-inflammatory, anti-pyrotic [156,157,158] improves skin moisture and water retention in the SC [153,156,157,159,160] | phototoxicity, eczema, contact dermatitis [151,152] |
| Amaranthus caudatus | amino-acids, proteins, amylopectin, minerals, vitamins (vitamin A, E, K), fibers, essential fatty acids, triterpenes (squalene) [161,162] | antioxidant capacity, moisturizing, skin hydration, suppressing the pigmentation [162,163,164] | * N |
| Angelica keiskei | coumarins, terpens, phenolic compounds [165,166,167,168] | antioxidant capacity, astringent, emollient, skin conditioning and protecting, skin whitening and lightening, sunlight protection [165] | * N |
| Arnica montana | fatty acids (palmitic, linoleic, myristic), essential oil, triterpenic alcohols, sugars, phytosterols, phenol acids, tannins, choline, inulin, flavonoids, carotenoids, coumarins, sesquiterpene lactones [169,170] | anti-inflammatory effect [158,171] reduces the ecchymosis and oedema [158] | contact dermatitis [169,172] rarely ocular irritation [170] |
| Artemia salina | diguanosine-tetraphosphate, D-myo-inosite-1,4,5-triphosphate, proteins, glucan [173] | stimulates skin regeneration, strengthens the immune system of the skin, sustains epidermal cell proliferation, anti-ageing (inhibiting the cells senescence, stimulating the collagen expression) and photo-protection effect [173] | * N |
| Bambusa arundinacea | flavonoids, phenolic compounds, chlorogenic acid, caffeic acid, ferulic acid, 8-C-glucosyl apigenin, luteolin derivatives [174] | antioxidant capacity, anti-ageing, photo-protection, skin pigmentation modulating effect, anti-allergic effect (inhibiting the production of IgE and lymphocytes) [174] | * N |
| Calendula officinalis | triterpenes, polyphenolic compounds, polysaccharides, vitamin C, tocopherols, quinones, carotenoids saponins, sterols [175,176,177,178] | anti-inflammatory effect [175,179] cell rejuvenation effect [179,180] skin smoothing and softening effect [179] prevents skin alteration and early ageing (improving the skin elasticity) [176,180,181] anti-irritant, anti-psoriatic and callus treating [158] stimulates the regeneration and epithelisation of wounded skin [175,179,180,181] antioxidant capacity [175,176,179,180] antimicrobial activity [155,179] | rare sensitization or allergic contact reactions [169,175,182] |
| Camelia sp. (C. sinensis, C. japonica) | polyphenols, catechins [176] | antioxidant capacity, reduces the sebum production, improves skin hydration, skin smoothing and softening, photoprotective, and anti-inflammatory effect [176,183,184,185,186,187] | contact dermatitis [172] |
| Chamomila recutita | polysaccharides, flavonoids (α-bisabolol, apigenin), sesquiterpene lactones [169,176] | anti-inflammatory effect, antioxidant capacity [188] repairs the SC, wound healing, anti-ageing activity skin smoothing and softening, also being used in the treatment of eczema [176,188,189] | skin sensitization, contact dermatitis [169,189,190] |
| Centella asiatica | saponins, flavonoids (quercetin, kaempferol, apigenil, naringenin, phenolic acids (chlorogenic acid), triterpenic steroids, amino acids, sugars [191,192] | antioxidant capacity, anti-inflammatory, anti-ageing effect stimulates the fibroblast proliferation, increasing the collagen synthesis increases the SC hydration and the epidermal barrier function anti-cellulite effect [191,192] | local allergic reactions, burning, eczemas, vesicles, pruritus [192] |
| Ceratonia siliqua | flavonoids, phytosterols, acids, esters, terpenoids, fenolic compounds [193,194,195] | anti-cellulite effect (increasing the aquaglyceroporines activity, stimulating lipolysis, reducing the localized fat overload), antioxidant capacity, depigmentation effect (anti-tyrosinase activity), skin lightening effect [193,194,196] | non-irritation potential [193] |
| Citrus sp. (C. aurantium dulcis, C. grandis, C. limon, C. unshiu peel) | bergapten, bergamotin, isopimpinellin, coumarins, psoralenes, angelical, volatile oil (limonene, linalool, linalyl acetate, terpineol, terpinene, terpinolene, ocimene, pinene etc.) [197,198,199] | antioxidant capacity, anti-inflammatory, antiseptic and anti-verrucous effect, used in acne treatment, wound healing properties, used as fragrance [158,197,198,199] | possible irritation, skin sensitization, hyperpigmentation, redness, oedema, photo-toxicity [197,198,199,200] |
| Cucumis sativus | flavonoids, saponins, sterols, carbohydrates, triterpenes, vitamins (C, B), fatty acid, proteins [201,202] | used in the treatment of periorbital edema, soothing emollient, anti-wrinkle, anti-ageing, anti-itching effects depigmentant and antioxidant capacity, anti-hyaluronidase and anti-elastase actions [201] | erythema after semi occlusive patch testing and conjunctival hyperemia/ocular irritation after a using of an eye lotion containing 1% C. sativus (cucumber) fruit extract [202] |
| Cydonia oblonga seed | cellulose, polysaccharides, polyphenols [203,204] | stimulates fibroblasts proliferation, wound, and burns healing maintains skin barrier function anti-inflammatory, anti-allergic and protective effects antioxidant capacity [203,204,205,206,207,208] | * N |
| Eclipta prostrata | flavonoids (luteolin, apigenin), wedelolactone, terpenoids, sterols, alkaloids, volatile oils [209,210,211,212,213] | depigmentant effect (anti-tyrosinase activity) hair revitalizing, dye in cosmetic products antioxidant and photoprotective capacity [209,210,211,212] | * N |
| Euphrasia officinalis | iridoids, flavonoids, polyphenols, saponins, alkaloids, tannins, etheric oils [214,215] | anti-inflammatory and astringent effect antioxidant capacity photo-protection, protective effect against photo-ageing, stimulates collagen synthesis [214,216,217] | * N |
| Ficus carica | phytosterols, anthocyanins, amino acids, atty acids, phenolic acids, flavonoids, volatile components [218,219] | antioxidant capacity, anti-warts and anti-verrucous activity used in the treatment of dry skin, eczema, acne anti-inflammatory, anti-ageing, anti-wrinkle and skin protection effects [158,218,219,220] | no side effects observed [220] |
| Glycyrrhiza glabra | saponins (glycyrrhizin), flavonoids (liquiritigenin, liquiritin), glycosides, isoflavons (glabridin, coumarins, stilbenoids) [221,222] | anti-inflammatory effect, antioxidant capacity, photo-protection effect reduces erythema and hyperpigmentation improves epidermal hydration and transepidermal water loss antibacterial and antifungal effect anti-dandruff effect [221,222,223,224] | eye sensitivity (burning, itch, redness), scalp pruritus (itch, dandruff) [221] |
| Glycine max | phenolic acids (ferulic, syringic, sinapic, flavonoids (isoflavons), soy proteins (β-conglycinin, glycinin), lipids, vitamin E [225,226,227] | anti-inflammatory effect, antioxidant capacity skin lightening and depigmentant protective effect against photo-ageing stimulates collagen and elastin synthesis, increasing the hyaluronic acid levels in aged skin skin regeneration effect, providing nutrients for cell renewal [225,226,227,228,229,230,231] | none allergic reactions to human skin toxicity evaluation [226,232] itching eczema after several months of exposure to a soy-based ingredients in cosmetic lotions [233] |
| Hedera helix | saponins (hederin, hederagenin, hederacosides, hederacolchisides etc.), flavonoids, anthocyanins, coumarins and phenolic acids, steroids, vitamins, volatile and fixed oils [234] | antiseptic, anti-elastase and anti-hyaluronidase effect indicated in cellulitis, cicatrisation, and wound healing [158,234,235] | contact dermatitis [234] |
| Lilium candidum | saponins, flavonoids, glycosides, nitrogenous compounds [236,237] | amelioration of skin redness, burn healing, hyperpigmentation, edema/skin inflammation anti-irritant, anti-inflammatory, antioxidant effect, and also emollient and sebostatic effect capacity of reducing ecchymosis, providing keratinocytes proliferation [158,236,238,239] | no irritations in vitro dermal or ocular irritation model [240] |
| Magnolia liliflora | terpenes, flavonoids, chlorogenic acid, rutin, quercetin, kaempferol, volatile oil (phenyethyl alcohol, levoxine, pinene, caryophyllene oxide, caryophyllene, bourbonene, farnesene, aerpineol, humulene) [241,242,243] | antioxidant capacity, anti-dermatophytes action, anti-inflammatory effect [241,242,243] | * N |
| Malus domestica/sylvestris | polyphenols (phloridizin, phloretin, quercetin, glycosides, rutin), acids (citric, malic, lactic, pyruvic, ascorbic etc.) [244,245,246] | confers cell protection, anti-ageing and photoprotective effect, antioxidant capacity increases moisture, reduces tyrosinase activity (depigmentation effect) [245,246,247,248] | absence of skin irritation of a cosmetic product containing 6% Malus sylvestris fruit extract under 24 h occlusive patch testing [245] |
| Malva sylvestris | mucilaginous polysaccharides, tannins, polyphenols, vitamin C, vitamin E, β-carotene, anthocyanidines, terpenes, naphthoquinones, flavonoids, fatty acids (e.g., α-linolenic acid) and minerals [158,249,250,251,252,253,254,255] | anti-pruritus, anti-psoriatic and antiseptic effect emollient, anti-inflammatory and antimicrobial capacity wound healing (stimulates the formation of free granulation tissue and reepithelization) [158,249,250,251,252,253,255] | low toxicity of Malva sylvestris hydro-alcoholic extract on topical application [256] |
| Nymphaea alba | polyphenols, flavonoids, essential oil, vitamin E, ellagitannins, sterols, fatty acids [257,258,259] | stimulates the autophagy (reduces the accumulation of advanced glycation end products which determine inflammatory response, destroys the protein structureand colors the skin in yellow or brown) antioxidant and photo-protection capacity reduces the hyperpigmentation [258,260] | * N |
| Opuntia cochenillifera | flavonoids, terpenes, cellulose, hemicellulose, lignins, pectines, malic acid, citric acid, ascorbic acid, oligosaccharides (fructose, glucose, sucrose, maltose etc.), amino-acids, fatty-acids [261,262,263,264] | antioxidant capacity, immunomodulation, hydration and cooling effects, wound healing [262,263] | * N |
| Orchid sp. | flavonoids, anthocyanins, fatty acids, organic acids, sterols, stilbenoids (resveratrol), amino-acids [265,266,267] | anti-inflammatory effect, antioxidant capacity, anti-tyrosinase activity, inhibits collagenase and elastase photo-protection, wound healing capacity cooling agent astringent, anti-ageing, emollient, skin moisturizing and whitening effect [265,266,268,269] | allergic contact dermatitis [270] |
| Pfaffia paniculata | saponins (pfaffosides), pfaffic acid, sterols, allantoin [236,271] | anti-inflammatory and anti-cellulite effect, antioxidant capacity, protective effect against photo-ageing [236,271] | * N |
| Picea abies | diterpene, stilbene glycosides (E-astringin, E-isorhapontin, flavonoids (catechin, taxifolin, taxifolin-3′-O-glucoside), lignin (pinoresinol) phenolic acid derivates, saccharose [272,273] | antioxidant capacity, antibacterial activity inhibits collagenase (anti-ageing activity), elastase (anti-ageing, anti-inflammatory and anti-psoriatic effect) and tyrosinase (whitening activity) wound healing and skin regeneration properties (cellular regeneration and epithelialization) [272,273,274,275,276] | possible allergic skin reactions (e.g., contact dermatitis) [276] |
| Porphyridium cruentum | exopolysaccharide, phycoerythrins, phycoerythrocyanins, phycocyanins, sterols, superoxide dismutase, polyunsaturated fatty acids [277,278,279] | antioxidant capacity, anti-inflammatory, anti-redness effect restores skin barrier permeability, photo-protection, regenerative and anti-wrinkles effect natural dye for cosmetics (creams, powders, lipsticks, make-up, eye shadows) [278,279,280,281,282] | * N |
| Ptychopetalum olacoides | fatty acids, saponins, flavonoids (rutin), sterols, aromatic oil, alkaloids, lupeol [236,283] | antioxidant capacity, anti-cellulite effect [236] | * N |
| Punica granatum | anthocyanins, ellagic acid, tannins [176] | improves viscoelasticity, anti-ageing effect, anti-inflammatory and antioxidant capacity antimicrobial activity [176,284,285] | no adverse effects [286] |
| Rosa sp. (R. damascena, R. canina, R. centifolia, R. davurica, R. mosqueta, R. rugosa) | carotenoids, sterols, anthocyanins, catechins, polyphenolic compounds (tocopherol), vitamin C, fatty acids (trans-retinoic acid, arachidonic acid, and unsaturated fatty acids, such as oleic, linoleic and linolenic acids) [287,288] | anti-inflammatory effect (suppressing proinflammatory cytokines) [289,290,291,292] antibacterial against skin bacteria (Propionibacterium acnes) [289,290,291,292,293] antioxidant capacity [290,292,294] antiproliferative and chemopreventive effects [290] fragrance in the perfumery industry [295] | well tolerate [296] no toxicity on human keratinocyte HaCaT cells [289] contact dermatitis to Rosa mosqueta oil applied for 3 days [288] |
| Rosmarinus officinalis | triterpes (rosmarinic acid, oleanolic acid, ursolic acid) [172,297] | antioxidant capacity, photoprotective effect, anti-aging, wound healing, anti-inflammatory, increases skin elasticity, wrinkles reducing effect [157,297,298] | eczema, contact dermatitis [172,299] |
| Rubus chamaemorus | ellagitannins, proanthocyanidins, fenolic acids, flavonoids, lignans, vitamin C, fatty acids (oleic, linoleic, linolenic etc.) [300] | antioxidant capacity antimicrobial effect (Staphylococcus aureus skin infections) reduces periorbital inflammations and ameliorates pruritus [300,301] | no irritation after an 48 h occlusive patch testin of a cosmetic product incorporating 2.5% Rubus chamaemorus Seed Oil (25 μL testing product quantity) [302] |
| Saccharum officinarum | fatty acids, fatty alcohols, acids, esters, aldehydes, ketones, sterols, terpoides, phenolic acids, flavonoids (flavones glycosides) [303,304,305] | antioxidant capacity, anti-tyrosinase activity photo-protection effect [304,305] | low toxicity after in vitro cytotoxicity assay [304] |
| Sambucus nigra | phenolic acids (caffeic, chlorogenic, ferulic, rosmarinic), flavonoids (quercetin, rutin, kaempferol), anthocyanins, tannins, triterpenes, organic acids [306,307,308] | antioxidant capacity, reduces tyrosinase activity antiseptic, anti-inflammatory, anti-psoriatic, photoprotective effects [306,307,308,309,310,311,312] | * N |
| Sideritis sp. (S. perfoliata, S. raeseri) | terpenes, phenolic compounds (flavonoids, phenylpropanid glycosides), tannins [313,314,315,316,317] | antioxidant capacity, anti-elastase, anti-melanin and anti-tyrosinase activity (anti-wrinkle and depigmentation effect) anti-inflammatory and antibacterial capacity photo-protection effect [313,314,316,317] | * N |
| Sophora japonica | flavonoids (rutin, quercetin etc.), tripterpenoids, alkaloids, saponins, polysaccharides [318,319,320] | antioxidant capacity, photo-protection, anti-melanin and anti-tyrosinase activity (skin-whitening) [318,319,320,321] | * N |
| Triticum aestivum | oligosaccharides [322] | stimulates hyaluronan synthase, fibronectin synthesys, restores the skin barrier integrity (wound healing: decubitus ulcers, skin lesions and burns), anti-inflammatory effect, antioxidant capacity [322,323,324,325] | possible hypersensitivity reactions [326] |
| Ulmus davidiana | saccharides (galactose, rhamnose, glucose), succinic acid, terpenoids (epifriedenalol), lignans, flavonoids (catechin) [327,328,329] | moisturizing, photoprotective, anti-ageing, anti-allergic and anti-inflammatory effect [327,328] | * N |
| Vaccinium myrtillus | anthocyanins (cyanidin, delphinidin, malvidin, peonidin, petunidin), flavonoids, phenolic acids [330] | antioxidant capacity, photoprotective and anti-inflammatory effect (anti-psoriatic, anti-erythematous), astringent properties, wound healing, restores and protects the skin barrier function [330,331,332,333,334,335] | * N |
| Vitis vinifera | polyphenols (resveratrol, anthocyanins), coumarn, carotenoids, flavonoids, tartaric acid, tannins, terpene alcohols [336,337,338] | anti-ageing effect, antioxidant capacity, anti-melanogenic activities, sunscreen protection [157,176,338,339] | allergic dermatitis [336,340] |
| Voandzeia subterranean | alkaloids, flavonoids, glycosides, saponins, steroids, triterpenoids, phenols, anthocyanins, carotenoids proteins, crude fiber, carbohydrates [341,342] | anti-wrinkle effects, photoprotective, anti-irritant, anti-pollution, hydrating effects, antioxidant capacity, anti-ageing activity, inhibits proteases, elastases, collagenases and catalase [343] | * N |
| Active Ingredient | Cosmetic Claim and Skin Benefits | Toxicity of Topical Products |
|---|---|---|
| Probiotics | prevention and improvement of skin conditions (e.g., external signs of ageing, acne, rosacea, yeast and bacterial infections, psoriasis, dermatitis) [344,345,346,347,348,349,350] | no side effects [344,350] |
| Bifida Ferment Lysate | improves the skin’s epidermal renewal process [351] diminishes clinical signs and symptoms of atopic eczema [352,353,354] regulates skin reactivity and dryness [355] | non-sensitizing [356] |
| Lactococcus Ferment Lysate | stimulates the skin’s self-renewal [357] significant improvement of atopic dermatitis (AD) [354] | non-irritant, no allergenic potential [358] |
| Pseudoalteromonas Ferment Extract | reduces skin shininess, pores, spots, and sebum [359,360] | non-sensitizing, non-irritating [361] |
| Amino acids, Peptides, Proteins | common ingredients in cosmetics, as they function as natural moisturizing factors which act as water-binding molecules stimulating collagen and elastin synthesis in skin and improving surface healing anti-ageing effect, increase hydration of the skin which helps to reduce wrinkles and improves the functions of the skin barrier [362] | safe in cosmetics [362] |
| Alanine | natural moisturizing factor which acts as a water binding molecule [362] | safe for cosmetic use no dermal irritation or sensitization [363] |
| Arginine | moisturizing effect increases skin hydration and alleviates the condition of skin dryness [364] | no dermal irritation or sensitization [363] |
| Isoleucine | an essential amino acid known for its ability to support tissue repair effective in the treatment of mild to moderate chronic lesion of atopic eczema of the face [365] | safe for cosmetic use [363] |
| Acetyl Hexapeptide-8 | cosmetic application for wrinkles, working by relaxing of superficial dermal muscles [366] decreases hyperkinetic facial lines or expression wrinkles, effective in reducing skin roughness [367] neurotransmitter inhibitor peptide, used in anti-wrinkle formulations applied to the periorbital area [368] | well tolerated, with lack of burning and discomfort to the patient safe for topical application [369] |
| Acetylarginyltryptophyl Diphenylglycine | enhances skin elasticity and tightness, increases type I collagen synthesis [370] | * N |
| Pentapeptide-18 | neurotransmitter-inhibiting peptide that decreases neuronal activity and catecholamine release, giving it Botox-like effects in reducing fine lines and wrinkles, and improving skin firmness [371] | safe for cosmetic use [372] |
| Dipeptide Diaminobutyroyl Benzylamide Diacetate | a small tripetide with anti-ageing and mattifying effect, stimulates PLOD 3 (procollagen-lysine, oxoglutarate 5-dioxygenase 3), enzyme which is known to be of importance for the intermolecular collagen crosslink stability, increasing the stability of collagen, especially in mature skin [373] | * N |
| Palmitoyl Tripeptide | improvement of facial wrinkles, elasticity, dermal density and skin tone [374] | safe in cosmetic products [375] |
| Vitamins | useful role in the treatment of skin ageing and protection of human skin against UV induced ageing [376] | |
| Ascorbyl Tetraisopalmitate | antioxidant and anti-inflammatory properties, increases skin hydration and smoothness [377] | contact dermatitis [378,379] |
| Niacinamide | antipruritic, antimicrobial, vasoactive, photoprotective, sebostatic capacity, lightening effect depending on its concentration [380] | safe for cosmetic use [381] |
| Panthenol | hydrating and softening potential, significantly accelerating epidermal regeneration [382] | allergic contact dermatitis [383,384] |
| Retinoids | antioxidant capacity, anti-wrinkle, depigmentation, anti-roughness, keratolytic effects, improve skin texture and laxity, protective effect against photo-ageing [385,386] | photosensitization, irritation, erythema, dermatitis, pruritus, burning sensation [386] |
| Tocopherol Tocotrienols | antioxidant capacity, anti-wrinkle effect, improving skin moisture [157,385,387] | erythema, oedema, local irritation [387] |
| Saccharides | ||
| Trehalose | moisture retaining agent in several cosmetic creams and lotions [388,389] | safe for use in cosmetic products [388] |
| Bee products (Honey, Propolis) | ||
| Honey Extract Propolis Extract | antimicrobial and immunomodulatory effect, antioxidant capacity, wound healing (stimulates angiogenesis, granulation, epithelialization, TNF-α (tumor necrosis factor-α) production, increasing collagen and fibroblasts synthesis), emollient, humectant, moisturizing, nourishing and protective effects against photo-ageing, restoration capacity of skin barrier function [390,391,392,393,394,395,396,397] | contact dermatitis, acute sensitization [391,396,397] |
| Other Chemical Compounds | ||
| Allantoin (5-ureidohydantoin) | anti-inflammatory effect and anti-irritation, wound healing and keratolytic properties, hydration effect, tissue regeneration and cell proliferation capacity [398,399] | no adverse effects [399] |
| Ceramide 3 | increases SC hydration, enhances the barrier function and reduces inflammation [400,401] | safe for use in cosmetic products [402] |
| Gold | anti-inflammatory and antioxidant effect, tissue regeneration capacity, restores skin elasticity, reduces signs of stress and ageing [403,404,405] | particles larger than 30 nm can be considered as safe but there is a need to comprehensively study the effects of gold nanoparticles on the basis of their size distribution for their safe application in cosmetics [404] |
| Lactic acid | primarily used as moisturizer and pH regulator in cosmetics, antimicrobial activity, skin lightening effect, keratolytic properties, possesses high water-binding capacity, antibacterial effect [406,407] peeling agent used in the amelioration of acne vulgaris and in the treatment of melasma [408] | good skin compatibility, showing only minor reactions [407] |
| Lecithin | antioxidant effect, dispersing agent for pigments [409] | safe as used in rinse-off products safe for use in leave-on products at concentrations of 15% insufficient data to determine the safety for use in cosmetic products where Lecithin or Hydrogenated Lecithin are likely to be inhaled [409] |
| Malachite Extract | a copper complex extracted from the malachite stone, being a powerful free radical scavenger, boosting cellular defenses, offering protection and detoxifying benefits [410] | * N |
| Sodium Pyrrolidone Carboxylate | skin moisturizing effect [411] | safe in cosmetics non-irritating in a reconstructed human epidermis model test using the EpiSkin model [412] |
| Superoxide Dismutase (SOD) | reduces UV-induced erythema, free radical scavenger, anti-irritant effect, anti-ageing capacity [413] | non-irritating and non-sensitizing [413] |
| Urea | humectant, decreases TEWL in normal skin and especially in xerotic skin disorders (AD patients) [414] moisturizing effect, desquamating actions (urea dissolves the intercellular cementing substance in the SC), antimicrobial action [415,416,417] | safe as used in cosmetic products [415]. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Juncan, A.M.; Moisă, D.G.; Santini, A.; Morgovan, C.; Rus, L.-L.; Vonica-Țincu, A.L.; Loghin, F. Advantages of Hyaluronic Acid and Its Combination with Other Bioactive Ingredients in Cosmeceuticals. Molecules 2021, 26, 4429. https://doi.org/10.3390/molecules26154429
Juncan AM, Moisă DG, Santini A, Morgovan C, Rus L-L, Vonica-Țincu AL, Loghin F. Advantages of Hyaluronic Acid and Its Combination with Other Bioactive Ingredients in Cosmeceuticals. Molecules. 2021; 26(15):4429. https://doi.org/10.3390/molecules26154429
Chicago/Turabian StyleJuncan, Anca Maria, Dana Georgiana Moisă, Antonello Santini, Claudiu Morgovan, Luca-Liviu Rus, Andreea Loredana Vonica-Țincu, and Felicia Loghin. 2021. "Advantages of Hyaluronic Acid and Its Combination with Other Bioactive Ingredients in Cosmeceuticals" Molecules 26, no. 15: 4429. https://doi.org/10.3390/molecules26154429