Journal Description
Diabetology
Diabetology
is an international, peer-reviewed, open access journal on diabetes research published quarterly online by MDPI.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- High Visibility: indexed within ESCI (Web of Science), Scopus, EBSCO, and other databases.
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 18 days after submission; acceptance to publication is undertaken in 6.8 days (median values for papers published in this journal in the second half of 2023).
- Recognition of Reviewers: APC discount vouchers, optional signed peer review, and reviewer names published annually in the journal.
Latest Articles
Do T2DM and Hyperglycaemia Affect the Expression Levels of the Regulating Enzymes of Cellular O-GlcNAcylation in Human Saphenous Vein Smooth Muscle Cells?
Diabetology 2024, 5(2), 162-177; https://doi.org/10.3390/diabetology5020013 (registering DOI) - 25 Apr 2024
Abstract
Protein O-GlcNAcylation, a dynamic and reversible glucose-dependent post-translational modification of serine and threonine residues on target proteins, has been proposed to promote vascular smooth muscle cell proliferation and migration events implicated in vein graft failure (VGF). Therefore, targeting the enzymes (glutamine fructose-6P
[...] Read more.
Protein O-GlcNAcylation, a dynamic and reversible glucose-dependent post-translational modification of serine and threonine residues on target proteins, has been proposed to promote vascular smooth muscle cell proliferation and migration events implicated in vein graft failure (VGF). Therefore, targeting the enzymes (glutamine fructose-6P amidotransferase (GFAT), O-GlcNAc transferase (OGT), and O-GlcNAcase (OGA)) that regulate cellular O-GlcNAcylation could offer therapeutic options to reduce neointimal hyperplasia and venous stenosis responsible for VGF. However, it is unclear how type 2 diabetes mellitus (T2DM) and hyperglycaemia affect the expression of these enzymes in human saphenous vein smooth muscle cells (HSVSMCs), a key cell type involved in the vascular dysfunction responsible for saphenous VGF. Therefore, our aim was to assess whether T2DM and hyperglycaemia affect GFAT, OGT, and OGA expression levels in HSVSMCs in vitro. Expression levels of GFAT, OGT, and OGA were determined in low-passage HSVSMCs from T2DM and non-T2DM patients, and in HSVSMCs treated for 48 h with hyperglycaemic (10 mM and 25 mM) glucose concentrations, by quantitative immunoblotting. Expression levels of OGT, OGA, and GFAT were not significantly different in HSVSMC lysates from T2DM patients versus non-T2DM controls. In addition, treatment with high glucose concentrations (10 mM and 25 mM) had no significant effect on the protein levels of these enzymes in HSVSMC lysates. From our findings, T2DM and hyperglycaemia do not significantly impact the expression levels of the O-GlcNAcylation-regulating enzymes OGT, OGA, and GFAT in HSVSMCs. This study provides a foundation for future studies to assess the role of O-GlcNAcylation on VGF in T2DM.
Full article
(This article belongs to the Special Issue Risk of Type 2 Diabetes Mellitus: Cardiorenometabolic Syndrome and Its Components)
Open AccessArticle
Epidemiology of Diabetes Mellitus in Adults and Seniors in Rio Branco, Acre, Western Brazilian Amazon
by
Yara de Moura Magalhães Lima, Fernanda Andrade Martins and Alanderson Alves Ramalho
Diabetology 2024, 5(2), 151-161; https://doi.org/10.3390/diabetology5020012 - 10 Apr 2024
Abstract
►▼
Show Figures
(1) Background: To analyze the prevalence and factors associated with diabetes mellitus in adults and the elderly in Rio Branco, Acre, Western Brazilian Amazon. (2) Methods: The R software version 4.0.5 was used for estimating the prevalence of diabetes mellitus, odds ratios, and
[...] Read more.
(1) Background: To analyze the prevalence and factors associated with diabetes mellitus in adults and the elderly in Rio Branco, Acre, Western Brazilian Amazon. (2) Methods: The R software version 4.0.5 was used for estimating the prevalence of diabetes mellitus, odds ratios, and 95% confidence intervals. Multiple analysis was conducted through hierarchical variable selection. (3) Results: 1.095 individuals aged 18 years and older participated in this study, with 6.4% of the respondents showing prevalence of diabetes mellitus. The prevalence of diabetes mellitus was positively associated with a prior medical diagnosis of obesity (OR: 3.2; 95% CI: 1.67–6.12), dyslipidemia (OR: 4.17; 95% CI: 2.08–8.36), and increasing age (OR: 1.07; 95% CI: 1.05–1.09). Conversely, an inverse association was observed with higher education (12 or more years of study; OR: 0.20; 95% CI: 0.07–0.61). (4) Conclusions: The prevalence of diabetes mellitus in the municipality of Rio Branco, Acre, Brazil, has significantly increased with advancing age. Education, obesity, and dyslipidemia were also identified as factors associated with diabetes mellitus in this population. Awareness campaigns regarding dietary patterns and lifestyle choices may serve as preventive and control measures.
Full article
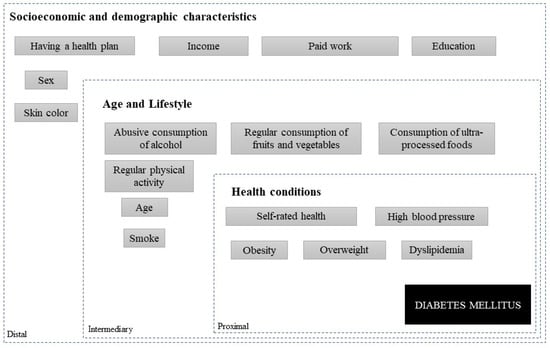
Figure 1
Open AccessArticle
Burden of Infected Diabetic Foot Ulcers on Hospital Admissions and Costs in a Third-Level Center
by
Roberto Da Ros, Roberta Assaloni, Andrea Michelli, Barbara Brunato, Enrica Barro, Marco Meloni and Cesare Miranda
Diabetology 2024, 5(2), 141-150; https://doi.org/10.3390/diabetology5020011 - 03 Apr 2024
Abstract
Diabetic foot is a common complication of diabetes that affects quality and prognosis of life for patients and often requires hospitalization. Infection, alone or in association with ischemia, is the main cause of hospital admission and impacts prognosis. The aim of this study
[...] Read more.
Diabetic foot is a common complication of diabetes that affects quality and prognosis of life for patients and often requires hospitalization. Infection, alone or in association with ischemia, is the main cause of hospital admission and impacts prognosis. The aim of this study is to analyze the costs of diabetic foot lesions and assess factors that influence the economic impact, focusing on infection. We included all people with diabetes with a first visit for diabetic foot during 2018 in our diabetic foot center. Database interrogation identified 422 patients. Diabetic foot treatment required hospitalization for 242 patients (58%), while 180 (42%) were treated in outpatient services. Healing time was different between the two groups: it was 136 ± 124 days (mean ± SD) for outpatients and 194 ± 190 days for patients that require hospitalization (p < 0.001). Costs: Treatment of 422 patients for diabetic foot globally costs 2063 million EUR and the mean cost for patients is 4888 EUR, with hospital stay having a high impact on this, accounting for 88% of the costs. Infection impacts hospitalization duration and ischemia impacts healing time. Ischemia and infection prolonged hospitalization duration and costs. Our work underlines that hospital treatment costs have a high impact on total costs.
Full article
(This article belongs to the Special Issue Feature Papers in Diabetology 2023)
Open AccessArticle
Utility of Flash Glucose Monitoring to Determine Glucose Variation Induced by Different Doughs in Persons with Type 2 Diabetes
by
Maria Antonietta Taras, Sara Cherchi, Ilaria Campesi, Valentina Margarita, Gavino Carboni, Paola Rappelli and Giancarlo Tonolo
Diabetology 2024, 5(1), 129-140; https://doi.org/10.3390/diabetology5010010 - 12 Mar 2024
Abstract
(1) Background: It has been previously shown that sourdough bread, compared to commercial yeast bread, elicits a lower postprandial glycemic and insulinemic response in patients with impaired glucose tolerance (IGT). Aims: Our aim was to evaluate the following aspects in persons with type
[...] Read more.
(1) Background: It has been previously shown that sourdough bread, compared to commercial yeast bread, elicits a lower postprandial glycemic and insulinemic response in patients with impaired glucose tolerance (IGT). Aims: Our aim was to evaluate the following aspects in persons with type 2 diabetes (T2DM): (1) glucose variations induced by three different doughs: X = bread prepared with functional alkaline biocrystal water, Y = sourdough-leavened bread, and W = bakery yeast bread; (2) the utility of flash glucose monitoring (FGM) to measure GL. (2) Methods: Twelve T2DM following diets (six males, diabetes duration 10.9 ± 1.3 years with no complications, Hba1c < 7.0%), after 12 h of fasting, consumed 180 g of the study breads leavened/matured for 48 (X), 8 (Y), and 4 h (W) at room temperature with 200 mL of water, in a random order, in single-blind conditions, on three different days. All patients had FGM running for the entire period of the experiments. Insulin was determined by capillary blood obtained for the basal and peak glucose concentrations. (3) Results: The peak glucose and peak insulin concentrations were significantly (p < 0.05) higher for W versus both X and Y, without significant differences between X and Y. The area under the curve of glucose variations for over 240 min was significantly higher in W than X (p < 0.01) and Y (p < 0.05), without significant differences between X and Y. (4) Conclusions: (1) Bread prepared with biocrystal water has the same lower GL of sourdough bread compared to bakery yeast bread, and it is easier to manage its leavening/maturation period; (2) FGM is a reliable method for determining rapid glucose changes in response to a carbohydrate meal in persons with type 2 diabetes.
Full article
(This article belongs to the Special Issue Feature Papers in Diabetology 2023)
►▼
Show Figures
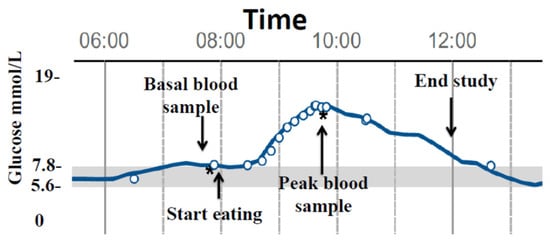
Figure 1
Open AccessArticle
Food as Medicine: FOODRx for Patients with Diabetes and Cardiovascular Disease in Central Minnesota—A PILOT STUDY
by
Mónica García-Pérez, Alexandra De Kesel Lofthus, David Tilstra, Kevin Switzer and Kristen Williamson
Diabetology 2024, 5(1), 110-128; https://doi.org/10.3390/diabetology5010009 - 08 Mar 2024
Abstract
►▼
Show Figures
The number of food-insecure individuals with diabetes is on the rise. FOODRx is a supplemental healthy food intervention program that gave disease-appropriate food boxes to food-insecure patients with diabetes at their care clinic and included nutrition and recipe materials in the patient’s preferred
[...] Read more.
The number of food-insecure individuals with diabetes is on the rise. FOODRx is a supplemental healthy food intervention program that gave disease-appropriate food boxes to food-insecure patients with diabetes at their care clinic and included nutrition and recipe materials in the patient’s preferred language (English, Spanish, or Somali). Implemented over a twelve-month period, we analyze FOODRx participants’ pre and post clinical measures, health care usage, and program/clinic satisfaction, and found that participation was linked to post improvements in fasting glucose and HgbA1c levels, reductions in ER visits and healthcare costs, and a decline in patients choosing between medication and food. Glucose levels decreased from 214 to 187 mg/dL and HgbA1c levels decreased from 9.6% to 9.1%. Average ER visits dropped from 1.21 to 1 visit and the reductions in healthcare costs were reflected in a decrease of an average of USD 250,000 in insurance claims. Patients were less likely to experience food insecurity, as measured in number of meals skipped and levels of hunger. Finally, the program improved patient satisfaction with the cultural responsiveness of the information shared with them.
Full article
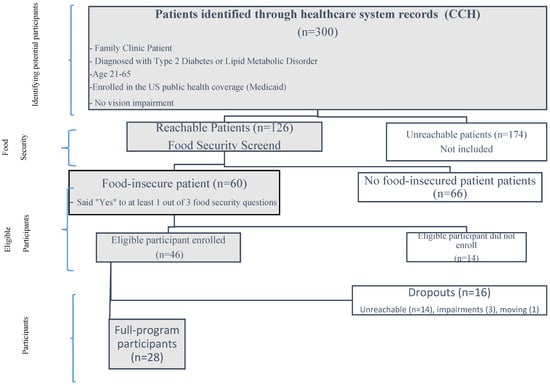
Figure 1
Open AccessArticle
Utilizing the Glucose and Insulin Response Shape of an Oral Glucose Tolerance Test to Predict Dysglycemia in Children with Overweight and Obesity, Ages 8–18 Years
by
Timothy J. Renier, Htun Ja Mai, Zheshi Zheng, Mary Ellen Vajravelu, Emily Hirschfeld, Diane Gilbert-Diamond, Joyce M. Lee and Jennifer L. Meijer
Diabetology 2024, 5(1), 96-109; https://doi.org/10.3390/diabetology5010008 - 01 Mar 2024
Abstract
Common dysglycemia measurements including fasting plasma glucose (FPG), oral glucose tolerance test (OGTT)-derived 2 h plasma glucose, and hemoglobin A1c (HbA1c) have limitations for children. Dynamic OGTT glucose and insulin responses may better reflect underlying physiology. This analysis assessed glucose and insulin curve
[...] Read more.
Common dysglycemia measurements including fasting plasma glucose (FPG), oral glucose tolerance test (OGTT)-derived 2 h plasma glucose, and hemoglobin A1c (HbA1c) have limitations for children. Dynamic OGTT glucose and insulin responses may better reflect underlying physiology. This analysis assessed glucose and insulin curve shapes utilizing classifications—biphasic, monophasic, or monotonically increasing—and functional principal components (FPCs) to predict future dysglycemia. The prospective cohort included 671 participants with no previous diabetes diagnosis (BMI percentile ≥ 85th, 8–18 years old); 193 returned for follow-up (median 14.5 months). Blood was collected every 30 min during the 2 h OGTT. Functional data analysis was performed on curves summarizing glucose and insulin responses. FPCs described variation in curve height (FPC1), time of peak (FPC2), and oscillation (FPC3). At baseline, both glucose and insulin FPC1 were significantly correlated with BMI percentile (Spearman correlation r = 0.22 and 0.48), triglycerides (r = 0.30 and 0.39), and HbA1c (r = 0.25 and 0.17). In longitudinal logistic regression analyses, glucose and insulin FPCs predicted future dysglycemia (AUC = 0.80) better than shape classifications (AUC = 0.69), HbA1c (AUC = 0.72), or FPG (AUC = 0.50). Further research should evaluate the utility of FPCs to predict metabolic diseases.
Full article
(This article belongs to the Special Issue Management of Type 2 Diabetes: Current Insights and Future Directions)
►▼
Show Figures
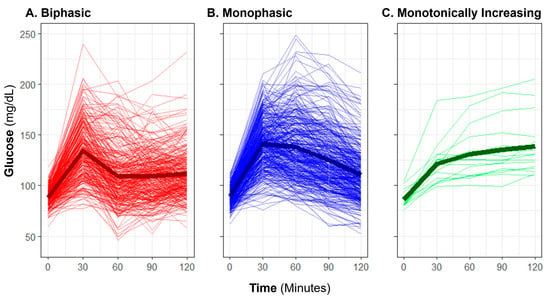
Figure 1
Open AccessArticle
Evaluating the Use of Web-Based Technologies for Self-Management among Arabic-Speaking Immigrants Living with Type 2 Diabetes Mellitus: A Cross-Sectional Study in Saudi Arabia
by
Anwar Althubyani, Clarice Tang, Jency Thomas and Sabrina Gupta
Diabetology 2024, 5(1), 85-95; https://doi.org/10.3390/diabetology5010007 - 28 Feb 2024
Abstract
This study aimed to investigate the use of and willingness to adopt web-based technology for self-management of type 2 diabetes among Arabic-speaking immigrants in Saudi Arabia. Conducted in Taif in 2022, it involved participants with type 2 diabetes mellitus, utilizing a study-specific questionnaire
[...] Read more.
This study aimed to investigate the use of and willingness to adopt web-based technology for self-management of type 2 diabetes among Arabic-speaking immigrants in Saudi Arabia. Conducted in Taif in 2022, it involved participants with type 2 diabetes mellitus, utilizing a study-specific questionnaire to gather data on demographics, disease specifics, and attitudes towards using this technology for diabetes management. Out of the 109 individuals who responded, 91 completed the survey and reported accessing web-based technology and an average usage of two hours per day. The primary use was for social media (90.1%) and information searching (73.6%). The study found a high willingness to use web-based technology for dietary planning (85.7%), physical activity monitoring (94.5%), and communication with healthcare providers (93.41%). Notably, younger participants, those with higher education, and married individuals showed more inclination towards using such technology, as indicated by significant correlations (p < 0.001, CI = 0.03–0.38; p < 0.039, CI = 1.06–10.26; p = 0.024, CI = 1.23–19.74). Over half of the participants (56%) considered web-based technology beneficial for diabetes management, with many finding it time-saving (61.5%). In conclusion, a significant proportion of participants demonstrated a strong preference for integrating web-based technology into their diabetes self-management routines. This preference was particularly evident in key areas such as diet, physical activity, and glucose monitoring. These findings underscore the potential of web-based technologies in supporting effective diabetes management among Arabic-speaking immigrants, highlighting the need for targeted interventions that leverage these digital tools.
Full article
(This article belongs to the Special Issue Management of Type 2 Diabetes: Current Insights and Future Directions)
►▼
Show Figures
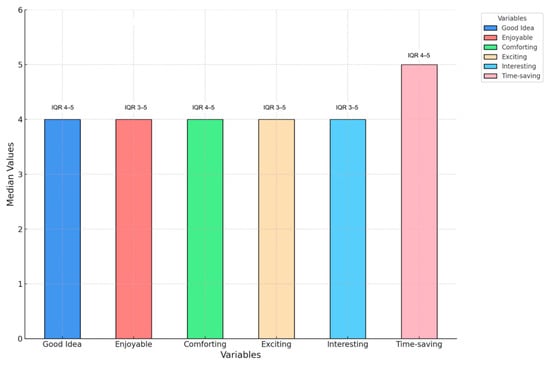
Figure 1
Open AccessReview
Melanocortins and Their Potential for the Treatment, Prevention and Amelioration of Complications of Diabetes
by
Gardner N. Robinson and Raelene J. Pickering
Diabetology 2024, 5(1), 69-84; https://doi.org/10.3390/diabetology5010006 - 04 Feb 2024
Abstract
Diabetes mellitus (type I and II) is an advancing global health problem, concerningly increasing in prevalence in most of the developed and developing world. Current therapies, such as the subcutaneous injection of insulin, are invasive and require a close monitoring of blood glucose
[...] Read more.
Diabetes mellitus (type I and II) is an advancing global health problem, concerningly increasing in prevalence in most of the developed and developing world. Current therapies, such as the subcutaneous injection of insulin, are invasive and require a close monitoring of blood glucose levels to prevent hypo- or hyperglycaemia from occurring. Despite an inexorable search for a cure since Banting and Best discovered and purified insulin in 1921, insulin remains a solitary insula, still the gold standard for treatment of type I and late-stage type II diabetes mellitus. Apropos of complications, diabetes causes a myriad of secondary maladies, ranging from diabetic kidney disease, diabetic retinopathy and diabetic neuropathy to erectile dysfunction and peripheral vascular disease. While scientists continue to interminably tinker with perfecting mechanical insulin pumps or dampening the immune response to pancreatic beta cells, an important aspect of the aetiology of diabetes should not be neglected, that of the metabolism. At its heart, diabetes can arguably be considered a metabolic disease, and this review suggests a return to focusing on preventing and treating diabetes by focussing on its metabolic causes. This narrative review summarises the potential of a recent class of synthetic peptides, the melanocortins, to help prevent and treat the complications of diabetes mellitus. The review summarises recent work showing the potential benefits of the melanocortins in treating diabetic complications through various pathways.
Full article
(This article belongs to the Special Issue Exclusive Papers Collection of Editorial Board Members in Diabetology)
►▼
Show Figures
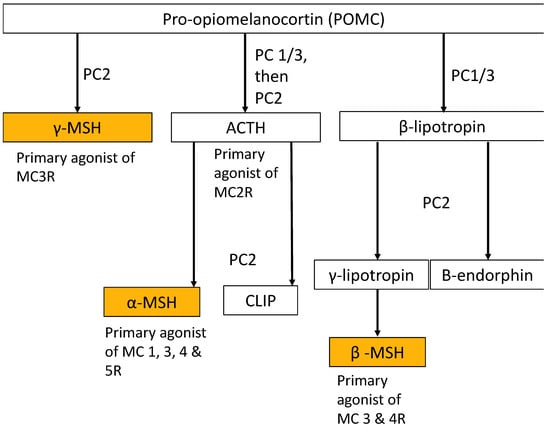
Figure 1
Open AccessCommunication
Effectiveness of Oral versus Injectable Semaglutide in Adults with Type 2 Diabetes: Results from a Retrospective Observational Study in Croatia
by
Sanja Klobučar, Andrej Belančić, Iva Bukša, Nikolina Morić and Dario Rahelić
Diabetology 2024, 5(1), 60-68; https://doi.org/10.3390/diabetology5010005 - 02 Feb 2024
Abstract
Background: The number of people with type 2 diabetes is increasing daily, and therefore, effective therapy is needed to successfully regulate glycemia and reduce the risk of associated complications. Recently, an oral formulation of the glucagon-like peptide-1 receptor agonist (GLP-1 RA) semaglutide has
[...] Read more.
Background: The number of people with type 2 diabetes is increasing daily, and therefore, effective therapy is needed to successfully regulate glycemia and reduce the risk of associated complications. Recently, an oral formulation of the glucagon-like peptide-1 receptor agonist (GLP-1 RA) semaglutide has become available. Therefore, the aim of our study was to compare the effectiveness of the new oral formulation and the existing injectable formulation of semaglutide in terms of glycemic and body weight control in a real-world setting. Patients and methods: This was a single-center retrospective observational study conducted at the Rijeka Clinical Hospital Centre. A total of 106 patients with inadequately controlled type 2 diabetes (HbA1c ≥ 7%) on different oral or basal insulin supported oral therapy were enrolled in the study, and data from electronic medical records were retrospectively collected and analyzed from May 2021 to November 2022. All subjects were GLP-1 RA-naive and consequently prescribed 0.5 or 1.0 mg of once weekly injectable semaglutide (IS) or 7 mg or 14 mg of once daily oral semaglutide (OS) for at least 6 months. Glycated hemoglobin (HbA1c), body weight, and body mass index (BMI) were assessed prior to semaglutide administration and after a 6-month follow-up period. The primary endpoint was the change from baseline in HbA1c, and secondary endpoints were the change in body weight and the proportion of participants with a reduction in body weight of ≥5% and ≥10%, respectively, 6 months after the initiation of semaglutide treatment. Results: At the 6-month follow-up, no significant difference was observed between the two formulations in terms of HbA1c reduction (IS −1.1% vs. OS −1.4%, p = 0.126) and weight loss (IS −6.50 kg vs. OS −5.90 kg, p = 0.714). Exactly the same proportion of participants in both groups achieved a weight loss of ≥5% (56.7%, n = 30). A weight loss ≥ 10% was observed in 20.7% (n = 11) of participants administered IS and 15.1% (n = 8) of participants administered OS, respectively (p = 0.454). Conclusion: In a real-world setting, oral semaglutide as an add-on therapy to ongoing antihyperglycemic treatment in patients with inadequately controlled type 2 diabetes who had not previously received GLP-1 RA demonstrated a similar effectiveness as injectable semaglutide in terms of glycemic control and weight loss after 6 months of treatment.
Full article
(This article belongs to the Special Issue Feature Papers in Diabetology 2023)
►▼
Show Figures
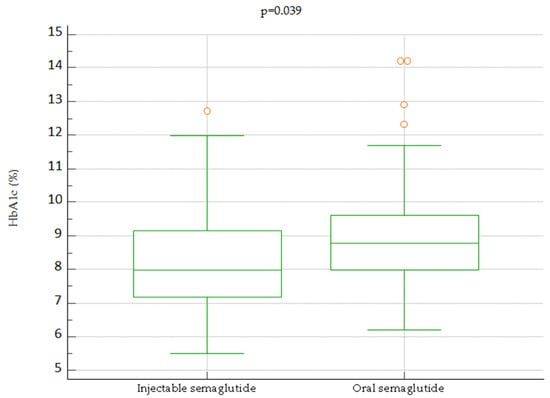
Figure 1
Open AccessSystematic Review
The Main Risk Factors in Type 2 Diabetes for Cognitive Dysfunction, Depression, and Psychosocial Problems: A Systematic Review
by
Maarja Randväli, Toomas Toomsoo and Jekaterina Šteinmiller
Diabetology 2024, 5(1), 40-59; https://doi.org/10.3390/diabetology5010004 - 11 Jan 2024
Abstract
►▼
Show Figures
The aim of this study is to analyze the risk factors that lead to cognitive impairment, depression, and psychosocial problems in type 2 diabetes and discern what aspects they have in common. Type 2 diabetes is associated with a higher risk of cognitive
[...] Read more.
The aim of this study is to analyze the risk factors that lead to cognitive impairment, depression, and psychosocial problems in type 2 diabetes and discern what aspects they have in common. Type 2 diabetes is associated with a higher risk of cognitive impairment, including dementia, which in turn increases the risk of hospitalization, falls, and premature mortality. In this study, we conducted a systematic review to achieve this goal, including searches on electronic databases such as PubMed, Medline, Web of Science, EBSCO Discovery, EBSCO host, Scopus, and ScienceDirect, from 2016 onwards. Additionally, we carried out manual searches in leading journals in the field. After evaluating and analyzing the articles, 60 remained, focusing on the following four main themes: disorders due to biological, psychological, social, and pharmacological causes that lead to neuropsychological complications. Based on the results, consistently analogous risk factors contributing to the onset of cognitive impairments, depression, and psychosocial predicaments encompass comorbid ailments, dysglycemia, gender, heightened levels of apprehension and anxiety, educational attainment, socio-economic standing, and pharmaceutical interventions. Furthermore, in the realm of type 2 diabetes, factors such as disease duration, adiposity, specifically overweight and obesity, and advancing age were also identified as significant contributors to cognitive impairments and depression. Concomitantly, the absence of a robust support system and social network emerged as a shared risk factor, predisposing individuals to psychosocial challenges and depressive states. These findings emphasize that the risk factors for cognitive impairments, depression, and psychosocial issues for type 2 diabetes are similar, highlighting the importance of psychosocial support, education, and patient-centered treatment to optimize outcomes and quality of life.
Full article
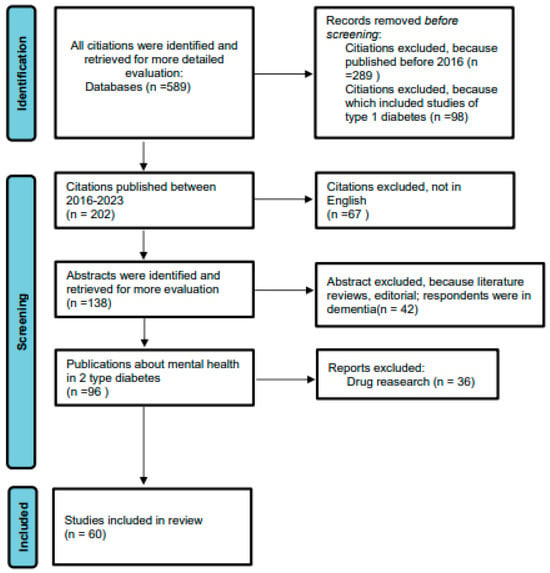
Figure 1
Open AccessArticle
Does the Efficacy of Semaglutide Treatment Differ between Low-Risk and High-Risk Subgroups of Patients with Type 2 Diabetes and Obesity Based on SCORE2, SCORE2-Diabetes, and ASCVD Calculations?
by
Martina Matovinović, Andrej Belančić, Juraj Jug, Filip Mustač, Maja Sirovica, Mihovil Santini, Anja Bošnjaković, Mario Lovrić and Martina Lovrić Benčić
Diabetology 2024, 5(1), 26-39; https://doi.org/10.3390/diabetology5010003 - 04 Jan 2024
Abstract
Background: Diabetes is the primary contributor to cardiovascular disease risk, and when combined with obesity, it further underscores the significance of cardiovascular risk assessment. Methods: A retrospective study of 64 patients with type 2 diabetes (T2D) and obesity on once-weekly subcutaneous semaglutide stratified
[...] Read more.
Background: Diabetes is the primary contributor to cardiovascular disease risk, and when combined with obesity, it further underscores the significance of cardiovascular risk assessment. Methods: A retrospective study of 64 patients with type 2 diabetes (T2D) and obesity on once-weekly subcutaneous semaglutide stratified by cardiovascular risk categories determined using the SCORE2/SCORE2-OP, SCORE2-Diabetes, and ASCVD score calculations. We compare the differences between groups (ASCVD: low + borderline + intermediate versus high-risk group; SCORE2/SCORE2-OP: low + moderate versus high + very high-risk group and SCORE2-Diabetes: low + moderate versus high + very high-risk group) in terms of change from baseline in body mass index (BMI) and HbA1c and weight loss outcomes. Results: Patients in the high-risk group, according to ASCVD risk score, had statistically better results in weight loss ≥ 3%, ≥5%, and ≥10% compared to ASCVD low + borderline + intermediate and without difference regarding HbA1c. According to SCORE2/SCORE2-OP, the high + very high-risk group had statistically better HbA1c and weight loss results but only for ≥5% versus the low + moderate risk group. Based on the score SCORE2-Diabetes, the high + very high-risk group had statistically significant better results in lowering HbA1c and weight loss but only for ≥5% versus the low + moderate risk group. Conclusions: To the best of our knowledge, this study represents the initial investigation linking glycemic control and weight reduction outcomes in individuals with T2D and obesity treated with once-weekly semaglutide stratified by cardiovascular risk categories determined using the SCORE2/SCORE2-OP, SCORE2-Diabetes and ASCVD score calculations.
Full article
(This article belongs to the Special Issue Feature Papers in Diabetology 2023)
►▼
Show Figures
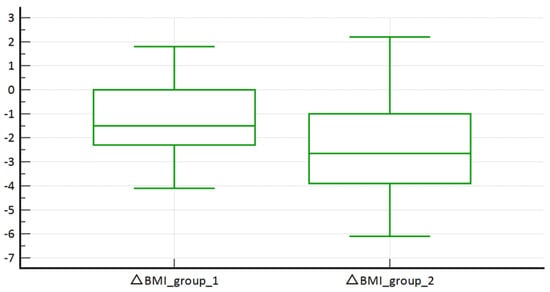
Figure 1
Open AccessArticle
Diet Supplementation with Rosemary (Rosmarinus officinalis L.) Leaf Powder Exhibits an Antidiabetic Property in Streptozotocin-Induced Diabetic Male Wistar Rats
by
Zelipha N. Kabubii, James M. Mbaria, Peter Mbaabu Mathiu, John M. Wanjohi and Evans N. Nyaboga
Diabetology 2024, 5(1), 12-25; https://doi.org/10.3390/diabetology5010002 - 04 Jan 2024
Abstract
Diabetes mellitus is a metabolic disorder that has a high global health burden and causes high mortality and morbidity in humans. Medicinal herbs and plants offer a promising alternative to conventional therapies for the management of diabetes. Rosemary (Rosmarinus officinalis L.) is
[...] Read more.
Diabetes mellitus is a metabolic disorder that has a high global health burden and causes high mortality and morbidity in humans. Medicinal herbs and plants offer a promising alternative to conventional therapies for the management of diabetes. Rosemary (Rosmarinus officinalis L.) is a traditional medicinal herb that has been used for the management of several diseases. Therefore, the present study investigates the antidiabetic properties of diets supplemented with R. officinalis leaf powder on streptozotocin-induced diabetic Wistar rats. First, the phytochemicals and 2,2-dephenyl-1-picrylhydrazyl (DPPH) free-radical scavenging activity of aqueous R. officinalis leaf extract were determined. Streptozotocin-induced diabetic male Wistar rats were fed a diet supplemented with R. officinalis leaf powder (ROP) at 3%, 6%, and 12%, respectively, for 6 weeks. Investigations of food intake, body weight, rat relative organ weights, blood glucose, lipid profiles, creatinine, bilirubin, alanine aminotransferase (ALT), and aspartate aminotransferase (AST) were estimated according to standard procedures. The results show that ROP aqueous extract contains significant amounts of phenolics, flavonoids, and tannins, which exhibit in vitro DPPH free-radical scavenging activity. Based on an in vivo study, ROP reduced blood glucose levels in streptozotocin-induced diabetic animals (p < 0.05). Dietary supplementation with ROP in diabetic rats significantly (p < 0.05) lowered ALT, AST, bilirubin, creatinine, total triglyceride (TG), total cholesterol (TC), and low-density lipoprotein (LDL) levels while increasing high-density lipoproteins (HDLs) when compared with the diabetic control group. Our findings demonstrate that a diet supplemented with R. officinalis leaf powder exhibits an antidiabetic potential with improved health outcomes, as demonstrated by the improved lipid and liver profile enzymes in our animal model.
Full article
Open AccessArticle
A Comparative Analysis of Machine Learning Models for the Detection of Undiagnosed Diabetes Patients
by
Simon Lebech Cichosz, Clara Bender and Ole Hejlesen
Diabetology 2024, 5(1), 1-11; https://doi.org/10.3390/diabetology5010001 - 03 Jan 2024
Abstract
Introduction: Early detection of type 2 diabetes is essential for preventing long-term complications. However, screening the entire population for diabetes is not cost-effective, so identifying individuals at high risk for this disease is crucial. The aim of this study was to compare the
[...] Read more.
Introduction: Early detection of type 2 diabetes is essential for preventing long-term complications. However, screening the entire population for diabetes is not cost-effective, so identifying individuals at high risk for this disease is crucial. The aim of this study was to compare the performance of five diverse machine learning (ML) models in classifying undiagnosed diabetes using large heterogeneous datasets. Methods: We used machine learning data from several years of the National Health and Nutrition Examination Survey (NHANES) from 2005 to 2018 to identify people with undiagnosed diabetes. The dataset included 45,431 participants, and biochemical confirmation of glucose control (HbA1c) were used to identify undiagnosed diabetes. The predictors were based on simple and clinically obtainable variables, which could be feasible for prescreening for diabetes. We included five ML models for comparison: random forest, AdaBoost, RUSBoost, LogitBoost, and a neural network. Results: The prevalence of undiagnosed diabetes was 4%. For the classification of undiagnosed diabetes, the area under the ROC curve (AUC) values were between 0.776 and 0.806. The positive predictive values (PPVs) were between 0.083 and 0.091, the negative predictive values (NPVs) were between 0.984 and 0.99, and the sensitivities were between 0.742 and 0.871. Conclusion: We have demonstrated that several types of classification models can accurately classify undiagnosed diabetes from simple and clinically obtainable variables. These results suggest that the use of machine learning for prescreening for undiagnosed diabetes could be a useful tool in clinical practice.
Full article
(This article belongs to the Special Issue Management of Type 2 Diabetes: Current Insights and Future Directions)
►▼
Show Figures
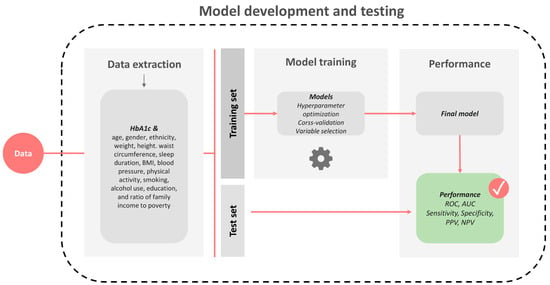
Figure 1
Open AccessArticle
Comorbidity of Type 2 Diabetes and Dementia among Hospitalized Patients in Los Angeles County: Hospitalization Outcomes and Costs, 2019–2021
by
D’Artagnan M. Robinson, Dalia Regos-Stewart, Mariana A. Reyes, Tony Kuo and Noel C. Barragan
Diabetology 2023, 4(4), 586-599; https://doi.org/10.3390/diabetology4040052 - 18 Dec 2023
Abstract
Hospitalizations for diabetes and dementia can impose a significant health and economic toll on older adults in the United States. This study sought to examine differences in hospitalization characteristics and outcomes associated with diabetes and dementia, separately and together, using 2019–2021 discharge record
[...] Read more.
Hospitalizations for diabetes and dementia can impose a significant health and economic toll on older adults in the United States. This study sought to examine differences in hospitalization characteristics and outcomes associated with diabetes and dementia, separately and together, using 2019–2021 discharge record data from the California Department of Health Care Access and Information. The sampled group were residents of Los Angeles County who were aged 50+ at the time of the study. The multivariable linear regression analysis showed that compared to those with no diabetes or dementia, patients with diabetes alone exhibited the highest total charges, while those with comorbid diabetes and dementia exhibited lower charges (p < 0.05). The multinomial logistic regression found that patients with comorbid diabetes and dementia had the highest odds of having a length of stay of 7+ days (Adjusted Odds Ratio = 1.49; 95% Confidence Interval (CI) = 1.44–1.53). A matched case–control analysis revealed that comorbid diabetes and dementia were associated with significantly lower odds of hypertensive disease than diabetes alone (Matched Odds Ratio = 0.81; 95% CI = 0.67–0.97). Collectively, these results highlight the complex factors that may influence the variable hospitalization outcomes that are common occurrences in these three distinct disease profiles. Study findings suggest a need to consider these complexities when developing policies or strategies to improve hospitalization outcomes for these conditions.
Full article
(This article belongs to the Special Issue Feature Papers in Diabetology 2023)
Open AccessArticle
Enrollment, Engagement, and Effectiveness of a Large-Scale Diabetes Prevention Program Using Synchronous Distance Technology
by
Casey Collins, Erin McCallum, Kelly Nordby, Surabhi Aggarwal, Emily Griffith, Cathy Thomas and Carolyn Dunn
Diabetology 2023, 4(4), 574-585; https://doi.org/10.3390/diabetology4040051 - 11 Dec 2023
Abstract
The Centers for Disease Control and Prevention (CDC) indicates that individuals with prediabetes are significantly less likely to develop type 2 diabetes if they participate in a lifestyle change program that results in at least 5% weight loss and 150 min of physical
[...] Read more.
The Centers for Disease Control and Prevention (CDC) indicates that individuals with prediabetes are significantly less likely to develop type 2 diabetes if they participate in a lifestyle change program that results in at least 5% weight loss and 150 min of physical activity per week. The CDC recognizes distance learning as an effective delivery mode for lifestyle change programs to prevent type 2 diabetes. The purpose of this study was to assess enrollment, engagement, and effectiveness of a type 2 diabetes prevention program (DPP) using synchronous distance technology. Eat Smart, Move More, Prevent Diabetes (ESMMPD) is an intensive 12-month DPP delivered using synchronous distance technology. Throughout 26 lessons, participants focused on healthy eating, physical activity, and mindfulness behaviors. Study findings showed a significant decrease in A1C (−0.24 p < 0.0001). Weight loss averaged 5.66% for those who completed the program. Based on the Wilcoxon signed-rank test, participants demonstrated statistically significant changes in self-reported confidence in their ability to perform all 18 health-promoting behaviors assessed (p < 0.0001). Participation in the program also resulted in the adoption of health promoting behaviors. A DPP using synchronous distance technology is an effective delivery mode to help participants adopt healthy behaviors, increase physical activity, and achieve the weight loss necessary to prevent or delay the onset of type 2 diabetes.
Full article
(This article belongs to the Special Issue Lifestyle Behavior Intervention for Diabetes Prevention and Management)
Open AccessArticle
Global Trends in Risk Factors and Therapeutic Interventions for People with Diabetes and Cardiovascular Disease: Results from the WHO International Clinical Trials Registry Platform
by
Musawenkosi Ndlovu, Phiwayinkosi V. Dludla, Ndivhuwo Muvhulawa, Yonela Ntamo, Asanda Mayeye, Nomahlubi Luphondo, Nokulunga Hlengwa, Albertus K. Basson, Sihle E. Mabhida, Sidney Hanser, Sithandiwe E. Mazibuko-Mbeje, Bongani B. Nkambule and Duduzile Ndwandwe
Diabetology 2023, 4(4), 560-573; https://doi.org/10.3390/diabetology4040050 - 08 Dec 2023
Abstract
This study presents a comprehensive analysis of 898 clinical trials conducted between 1999 and 2023, focusing on the interplay of metabolic syndrome, cardiovascular diseases (CVDs), and type 2 diabetes mellitus (T2D). This study draws upon data sourced from the International Clinical Trials Registry
[...] Read more.
This study presents a comprehensive analysis of 898 clinical trials conducted between 1999 and 2023, focusing on the interplay of metabolic syndrome, cardiovascular diseases (CVDs), and type 2 diabetes mellitus (T2D). This study draws upon data sourced from the International Clinical Trials Registry Platform (ICTRP) until August 2023. The trials were predominantly interventional (67%) or observational (33%). A geographical distribution reveals that while the United States registered approximately 18% of the trials, other regions like Australia, the United Kingdom, and multicounty trials made substantial contributions. Most studies (84%) included both male and female participants, with adults aged 18 to 65 years predominantly represented. The trials aimed at treatment (21%) and prevention (21%), emphasizing the dual focus on addressing existing CVD risk and preventing its development. Notably, CVDs (29%), T2D (8%), and the coexistence of both (21%) constituted the primary conditions of interest. Key interventions encompassed lifestyle and behavioral modifications, dietary supplementation, and drug therapies, with metformin and statins leading in pharmacological treatments. Interestingly, additional interventions such as glucagon-like peptide-1 agonists and dipeptidyl peptidase IV inhibitors are gaining recognition for their potential in managing metabolic syndrome-related conditions. Moreover, the report highlights a growing focus on inflammation, body mass index, blood pressure, body weight, and major adverse cardiovascular events as primary outcomes. Overall, the study highlights the importance of ICTRP as the source of data for clinical trials targeting metabolic syndrome, CVDs, and T2D and the growing recognition of diverse intervention strategies to address this critical global health concern.
Full article
(This article belongs to the Special Issue Management of Type 2 Diabetes: Current Insights and Future Directions)
►▼
Show Figures
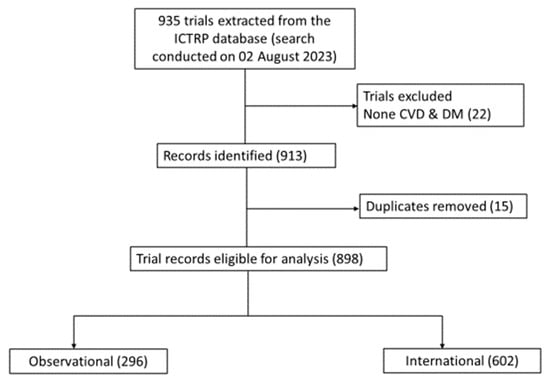
Figure 1
Open AccessCommentary
Could Microbiome Be the Common Co-Denominator between Type 2 Diabetes and Pancreatic Cancer?
by
Marin Golčić and Andrej Belančić
Diabetology 2023, 4(4), 553-559; https://doi.org/10.3390/diabetology4040049 - 07 Dec 2023
Abstract
Similar microorganisms, via similar mechanisms, play a role in the development of both pancreatic cancer (PC) and type 2 diabetes (T2D). Since the new onset of T2D is potentially one of the earliest signs of PC, it is highly plausible that a common
[...] Read more.
Similar microorganisms, via similar mechanisms, play a role in the development of both pancreatic cancer (PC) and type 2 diabetes (T2D). Since the new onset of T2D is potentially one of the earliest signs of PC, it is highly plausible that a common denominator might be responsible for both, as the growth of the cancer will take a longer time to manifest compared to the insulin resistance. Although a variety of host-dependent factors and susceptibility play a role, and the mechanisms connecting the two diseases remain poorly understood, future well-designed trials should hypothesize whether a microbial intervention (modification and/or transplantation) results in a lower incidence and the better treatment of both diseases since the T2D–PC–gut microbiome interconnection seems scientifically logical.
Full article
(This article belongs to the Special Issue Feature Papers in Diabetology 2023)
Open AccessReview
Importance of Dyslipidaemia Treatment in Individuals with Type 2 Diabetes Mellitus—A Narrative Review
by
Dominik Strikić, Andro Vujević, Dražen Perica, Dunja Leskovar, Kristina Paponja, Ivan Pećin and Iveta Merćep
Diabetology 2023, 4(4), 538-552; https://doi.org/10.3390/diabetology4040048 - 04 Dec 2023
Abstract
Type 2 diabetes mellitus (T2DM) is a common metabolic disease characterised by insulin resistance and elevated blood glucose levels, affecting millions of people worldwide. T2DM individuals with dyslipidaemia have an increased risk of cardiovascular disease (CVD). A complex interplay of risk factors such
[...] Read more.
Type 2 diabetes mellitus (T2DM) is a common metabolic disease characterised by insulin resistance and elevated blood glucose levels, affecting millions of people worldwide. T2DM individuals with dyslipidaemia have an increased risk of cardiovascular disease (CVD). A complex interplay of risk factors such as hyperglycaemia, dyslipidaemia, hypertension, obesity, inflammation, and oxidative stress favour the development of atherosclerosis, a central mechanism in the pathogenesis of cardiovascular disease. Dyslipidaemia, a hallmark of T2DM, is characterised by elevated triglycerides, decreased high-density lipoprotein (HDL) cholesterol and the presence of small, dense low-density lipoprotein (LDL) particles, all of which promote atherosclerosis. In this article, we have attempted to present various treatment strategies that include pharmacological interventions such as statins, ezetimibe, PCSK9 inhibitors, fibrates, and omega-3 fatty acids. We have also tried to highlight the pivotal role of lifestyle modifications, including physical activity and dietary changes, in improving lipid profiles and overall cardiovascular health in T2DM individuals. We have also tried to present the latest clinical guidelines for the management of dyslipidaemia in T2DM individuals. In conclusion, the treatment of dyslipidaemia in T2DM individuals is of great importance as it lowers lipid particle levels, slows the progression of atherosclerosis, and ultimately reduces susceptibility to cardiovascular disease.
Full article
(This article belongs to the Special Issue Management of Type 2 Diabetes: Current Insights and Future Directions)
►▼
Show Figures
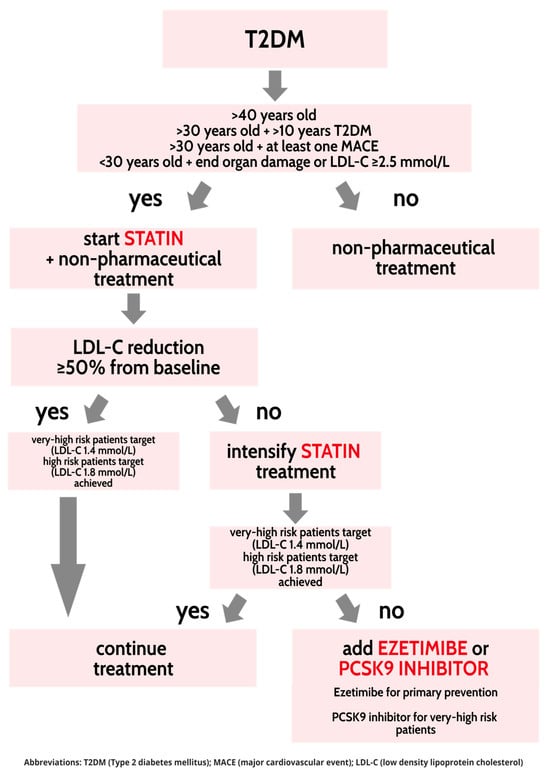
Figure 1
Open AccessCorrection
Correction: Brandão Palma et al. Biological Evidence of Improved Wound Healing Using Autologous Micrografts in a Diabetic Animal Model. Diabetology 2023, 4, 294–311
by
Diabetology Editorial Office
Diabetology 2023, 4(4), 537; https://doi.org/10.3390/diabetology4040047 - 24 Nov 2023
Abstract
The Diabetology Editorial Office would like to make the following correction to the published paper [...]
Full article
Open AccessReview
Sexual Dysfunction in Female Patients with Type 2 Diabetes Mellitus—Sneak Peek on an Important Quality of Life Determinant
by
Marija Rogoznica, Dražen Perica, Barbara Borovac, Andrej Belančić and Martina Matovinović
Diabetology 2023, 4(4), 527-536; https://doi.org/10.3390/diabetology4040046 - 13 Nov 2023
Abstract
Type 2 diabetes mellitus (T2DM) is a multisystemic disease with a high global burden and chronic complications. Sexual dysfunction (SD) in patients with T2DM is an often-overlooked complication, despite its high impact on quality of life (QoL). Female sexual disorders can affect women
[...] Read more.
Type 2 diabetes mellitus (T2DM) is a multisystemic disease with a high global burden and chronic complications. Sexual dysfunction (SD) in patients with T2DM is an often-overlooked complication, despite its high impact on quality of life (QoL). Female sexual disorders can affect women of reproductive age as well as menopausal women. Proposed mechanisms are intertwining a variety of physiological, neurological, vascular, hormonal, and psychological variables. The impairment of sexual function has been linked to hyperglycemia, insulin resistance, chronic low-grade inflammation, endothelial dysfunction, neuropathy, and hormonal abnormalities. There are many different manifestations of female sexual dysfunction, such as insufficient sexual desire, diminished arousal, difficulty in eliciting orgasm, and pain during sexual engagement. Numerous studies have shown that the QoL of patients living with diabetes mellitus (DM) is lower than that of those without DM. SD in women with T2DM leads to deteriorated QoL. Treatment must be individualized based on the diagnosis and the sexual dysfunction as well as underlying medical, psychological, and interpersonal issues. The goal of modern medical care for patients living with diabetes is not to delay death but to improve their health and QoL. The present review article aimed to raise awareness about female sexual dysfunction in patients with T2DM and to provide an overview of its impact on QoL.
Full article
(This article belongs to the Special Issue Feature Papers in Diabetology 2023)
►▼
Show Figures
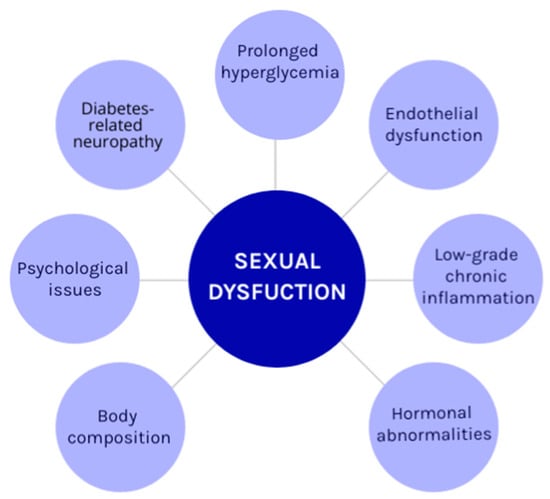
Figure 1
Highly Accessed Articles
Latest Books
E-Mail Alert
News
Topics

Conferences
Special Issues
Special Issue in
Diabetology
Gender Difference in Diabetes 2.0 Edition
Guest Editor: Giancarlo TonoloDeadline: 30 April 2024
Special Issue in
Diabetology
Women’s Special Issue Series: Diabetology
Guest Editors: Kirsten Suman, Medha PriyadarshiniDeadline: 31 May 2024
Special Issue in
Diabetology
Feature Papers in Diabetology 2024
Guest Editor: Peter CliftonDeadline: 30 September 2024
Special Issue in
Diabetology
Exclusive Papers Collection of Editorial Board Members in Diabetology
Guest Editor: Sathish ThirunavukkarasuDeadline: 31 December 2024







