Radiation Therapy for Brain Tumors
A special issue of Cancers (ISSN 2072-6694). This special issue belongs to the section "Cancer Therapy".
Deadline for manuscript submissions: 31 October 2024 | Viewed by 4574
Special Issue Editor
Special Issue Information
Dear Colleagues,
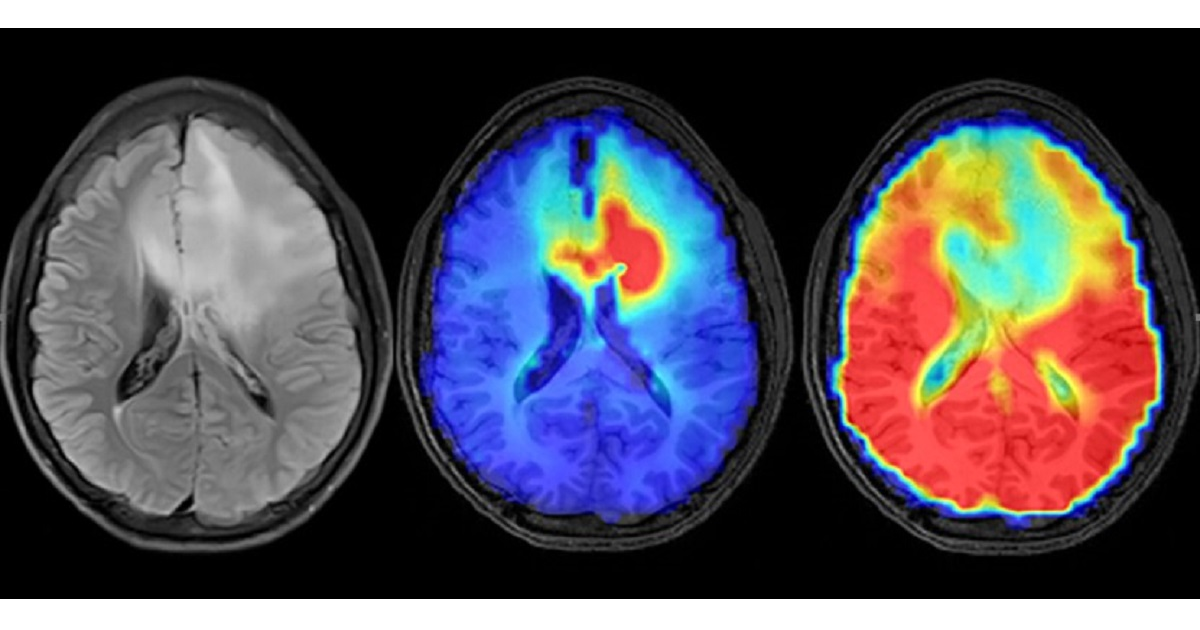
Radiation therapy plays a crucial role in managing both benign and malignant brain tumors. Recent advances in imaging and radiation delivery have expanded the use of radiation therapy and significantly improved patient outcomes. Advanced imaging techniques such as magnetic resonance imaging (MRI) utilizing three-dimensional spectroscopy and perfusion have enhanced the delineation of gliomas, allowing for more precise treatment planning and assessment of the treatment response. Furthermore, new radiation delivery techniques such as IMRT, stereotactic radiosurgery, and proton therapy have enabled more accurate targeting of tumors while minimizing damage to surrounding healthy tissue. These advancements have resulted in improved treatment outcomes and enhanced quality of life for patients with brain and spine tumors.
This series of articles will focus on recent breakthroughs in tumor imaging and radiation therapy for brain and spine tumors. The articles will cover various topics, including the role of functional imaging in treatment planning, the effectiveness of immunotherapy in combination with radiation therapy, and the potential of radiomics in predicting the treatment response. These articles will provide insights into the current state-of-the-art in radiation therapy for brain and spine tumors and offer valuable information for clinicians involved in managing these patients.
Dr. Jim Zhong
Guest Editor
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the special issue website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Cancers is an international peer-reviewed open access semimonthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2900 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- radiosurgery
- hypofractionated radiosurgery
- spectroscopic MRI
- proton radiation
- image-guided radiotherapy
- radiotherapy for benign tumors
- radiotherapy for gliomas
- gamma knife






