1. Introduction
The field of tissue engineering aims to repair and/or regenerate tissues damaged from age, disease, trauma, or congenital defects [
1]. Tissue engineering consists of three components: cells, scaffolds, and growth signals. The rapidly developing field holds the potential to help many individuals who have a poor quality of life due to these injuries and illnesses. While a loftier goal of tissue engineering may be to replace organs, the current literature focuses heavily on the use of polymeric materials for drug delivery and the ability of the materials to improve healing. As research into biomaterials continues to grow, it is important to understand the exact attributes of materials that allow them to meet the unique needs of clinical challenges.
Natural polymers are commonly used for scaffolds in tissue engineering. These polymers are found in nature and are typically extracted from plants and animals [
1]. Due to their origin, these polymers tend to exhibit desired interactions with cells when implanted in the body [
2] and thus tend to induce superior cell adhesion, migration, and proliferation when used as tissue engineering scaffolds. Across industries, natural polymers are implemented in different methods. In traditional textiles, natural polymers such as cellulose are made into viscose rayon or cellulose acetate fibers. In other material industries, natural rubber from tree latex is often vulcanized and used for conveyor belts [
3]. In biomedical research, there is ample evidence that incorporating natural polymers into biomaterials improves the bioactivity of the engineered material [
4]. Since the creation of the term of tissue engineering in the 1980s by Langer and Vacanti, researchers have been using natural polymers for tissue engineering scaffolds [
5]. However, many questions persist surrounding the exact mechanisms that allow for such bioactivity in a case-by-case manner.
The significance of understanding natural polymers’ interaction with biological systems comes from their tendency to elicit immune responses and the increased use of biodegradable synthetic polymers to counter this issue [
6]. The fourth generation of biomaterials has come to focus significantly on biomimetic materials while having an increased use of synthetic polymers [
7]. This polymer group comprises man-made polymers that are biocompatible and tend to be degradable by simple hydrolysis [
8]. This makes them very useful in tissue engineering because they can still be tailored for specific applications such as wound closure devices such as sutures or orthopedic fixation devices such as pins, rods, or screws [
9].
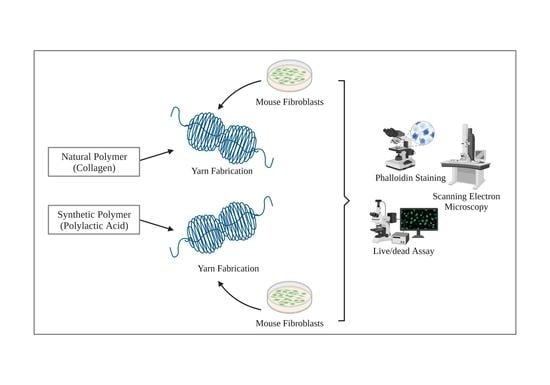
This study aims to compare how successfully cells adhere and proliferate on scaffolds produced by natural polymers compared to biodegradable synthetic ones. Specifically, we utilize fibrous scaffolds because these polymeric materials are widely popular for tissue engineering [
10]. Fibrous approaches have been shown to be better at mimicking the extracellular matrix (ECM) and providing more surface area for cellular attachment [
10]. We seek to gain any insight into the differences in natural polymers that may provide enhanced bioactivity in relation to the overall process of developing biomaterials. Understanding these mechanisms will help improve our understanding of what makes tissue engineering scaffolds biomimetic and will thus allow us to harness the “best of both worlds” from both synthetic and natural polymers to create more effective and functional fibrous scaffolds for drug delivery and clinical use.
To conduct this comparison, a model for each polymer class had to be selected. In the case of natural polymers, collagen will be used as a model because it is the most abundant protein in the human body [
11]. Additionally, collagen exhibits excellent biocompatibility, low antigenicity, and appropriate hemostatic properties for various tissue engineering applications [
12]. While these attributes make collagen attractive for scaffolds, the polymer is not without its disadvantages. These include mechanical weakness [
13] and variability in properties depending on the collagen source [
12]. Collagen also degrades quickly. Depending on the end-use of the scaffold, this rapid degradation can be considered an advantage or disadvantage. Typically, the degradation rate of a scaffold should match the de novo tissue formation at its site of use or implantation [
12,
14]. Because collagen exhibits advantages and disadvantages characteristic of most natural polymers, we will use it to represent these natural polymers in our comparative study. With the end goal of tissue engineering being a replica of tissue systems in human physiology, collagen offers an excellent model for comparison.
The model that will be used for biodegradable synthetic polymers is polylactic acid (PLA). This is highly biocompatible due to the material’s properties regarding degrading into lactic acid, carbon dioxide, and water [
15]. These compounds are common in the human body, allowing the material not to elicit an inflammatory response initially when implanted. We selected PLA to represent synthetic polymers in this study because, much like how collagen exhibits many key advantages and disadvantages of natural polymers, so does PLA for synthetic ones. These advantages include the aforementioned high biocompatibility, as well as the high biodegradability, excellent mechanical and barrier properties, relatively low cost, and high tunability, which can be controlled during production or post-processing [
16]. This allows for the more precise and controllable mimicry of the extracellular matrix. However, PLA and other synthetic polymers usually exhibit inferior cell adhesion, migration, and proliferation compared to collagen and other natural polymers. Additionally, PLA can induce inflammatory responses to its acidic byproducts during degradation [
17].
2. Materials and Methods
All chemicals and reagents were purchased from ThermoFisher (Waltham, MA, USA) unless otherwise noted.
2.1. Collagen and PLA Fibrous Scaffold Creation
Collagen Scaffold Fabrication: Bovine collagen fibers (donation of Kaneka Corporation) were processed through a card chute system (Reiter Card C4), followed by two rounds of drawing (Reiter RSB851) until the fibers were anisotropically aligned. They were then passed through the roving machine (Reiter Fly F4/1) and then a ring spinning machine (Reiter G5/2), where yarns of 265 denier (yarn thickness unit) were produced [
18,
19]. For this experiment, 12-inch pieces were cut and bundled up to make a tangled network of yarns. The samples were sterilized by soaking these yarns in a 70% ethanol solution and rinsing them with Dulbecco’s Phosphate-Buffered Saline (PBS) (DPBS, Cytiva). Each sample of yarn bundles was then placed into the wells of a 24-well plate. These yarn bundles are henceforth referred to as “collagen scaffolds”.
PLA Scaffold Fabrication: PLA fibers were provided by Xinxiang Sunshine Textiles Co., Ltd., Xinxiang, China, in yarn form (150 denier PLA yarn). The PLA yarn samples were spun into a yarn-like structure and processed with the same methods previously described for the collagen scaffold fabrication [
19]. Twelve-inch pieces were cut and tangled into weblike bundles before being sterilized with 70% ethanol and washed with PBS. These weblike bundles are henceforth referred to as “PLA scaffolds”.
2.2. Scanning Electron Microscopy
A scanning electron microscope (SEM) examines visual growth using secondary and backscattering scans. This provides an image of the topography and a deeper view of the surface to visually assess cellular attachment, proliferation, and migration into the scaffold while also characterizing the scaffold itself. Images were taken on days 1 and 7, following sample fixation, which was conducted by washing the seeded samples with PBS and then fixing them by submerging them in an SEM buffer comprising 4% paraformaldehyde for approximately 20 min. The samples were then washed with PBS two to three times and then a 0.1 M sodium cacodylate buffer, pH 7.2, supplemented with 5% sucrose for 15 min. They were then dehydrated with a progressively increasing amount of ethanol: 35%, 50%, 70%, 80%, 95%, and 100% diluted to the appropriate concentration in water; 35–95% are in intervals of 10 min, and the first 100% is in intervals of 3 by 10 min of washing, followed by a 40 min wash. After dehydration, the samples were soaked in a solution comprising a 1:1 ratio of 100% EtOH and hexamethyldisilane (HMDS) for 20 min and then in pure HDMS for 20 min. Once the samples were dried, they were mounted on imaging stubs with carbon tape.
2.3. NIH 3T3 Cells
The cells used for this study were NIH 3T3 fibroblasts. These embryonic murine fibroblasts are representative of a type of common cell found in connective tissues and an immortalized cell line which would allow for a generic comparison. The cells were cultured under static conditions and maintained in media consisting of Dulbecco’s modified eagle medium, 10% fetal bovine serum, and 1% penicillin-streptomycin. The media were changed every 72 h [
20]. The cells were passaged regularly using Trypsin—0.25% EDTA (Gibco, ThermoFisher, Waltham, MA, USA) upon reaching approximately 80% confluence. These cells were thawed at passage 12, plated onto plasticware coated with 0.1% gelatin, and then incubated at 37 °C and 5% CO
2. Once at the appropriate confluency for providing the correct seeding density was reached, the cells were counted and seeded onto scaffolds at a density of 100,000 cells/cm
2, with control wells (a well that contains only cells and no scaffold) seeded with 50,000 cells/cm
2 to prevent overgrowth. A higher number of cells were plated in the wells containing scaffolds to account for those cells that would adhere to the 3D volume of the scaffolds rather than the tissue culture plastic. To ensure maximum cell adhesion, the total number of cells were suspended in 20 μL of media, added to the collagen or PLA samples, and incubated for 20 min before a total volume of 1 mL of media was added to each well.
2.4. Cell Viability Testing
A LIVE/DEAD™ Cell Imaging Kit (488/570) (R37601, ThermoFisher, Waltham, MA, USA) analyzes the cell viability by measuring the cytotoxicity, intracellular esterase activity, and plasma membrane integrity. Calcein dye stains live cells bright green and ethidium-homodimer 2 stains dead cells red. The live cells turn green because of the enzymatic conversion of the non-fluorescent calcein to fluorescent calcein, which indicates intracellular esterase activity [
20]. The dead cells turn red because of binding to DNA when the dye gets through the damaged membrane. To test the cell viability, seeded samples were tested on days 1, 3, 5, and 7 post-seeding. After incubation, the samples were imaged with an EVOS FL Auto 2 (ThermoFisher) fluorescent microscope.
On the same days as the LIVE/DEAD™ assay, an alamarBlue™ assay was conducted to quantify cellular proliferation. The reagents were added to the complete media and incubated for 1–4 h. The alamarBlue™ Cell Viability Reagent is a non-toxic resazurin dye that enters the cell membranes. It is initially blue and non-fluorescent. However, once it enters a living cell, it is metabolized to resorufin, which is red and fluorescent. Therefore, cellular proliferation can be detected through the absorbance of 570 and 600 nm or the fluorescence excitation of 530–560 nm and the emission of 590 nm of the cells. The plates were incubated for 90 min and then read using a microplate reader (Synergy HT, BioTek, Santa Clara, CA, USA) set to 540/25 λ excitation and 590/35 λ emission and maintained at 37 °C.
2.5. Immunofluorescent Staining
Phalloidin immunofluorescence stain was used to elucidate the integrity and morphology of the cells’ cytoskeletons and to corroborate the cellular viability results from the LIVE/DEAD, alamarBlue, and SEM image results. Phalloidin dye has a high affinity for filamentous F-actin within the cytoskeleton. Thus, the dye stains the cytoskeleton and emits green fluorescence with excitation at 495 nm and emission at 518 nm. The samples were fixed on days 3 and 7 by a PBS wash, followed by submergence in 4% paraformaldehyde for approximately 20 min. Next, the samples were permeabilized with 0.20% TritonX-100 for 30 min and washed in PBS + 0.1% Tween-20 for 5 min. This step was repeated three times. The samples were then incubated in a blocking buffer comprising 2% Bovine Serum Albumin (BSA) and 2% goat serum in PBS + 0.1% Tween-20. Two drops per mL of Invitrogen™ ActinGreen™ 488 ReadyProbes™ Reagent containing the phalloidin stain were added to the blocking buffer. A total of 250 μL of the solution was added to each sample, and the samples were incubated for an hour. The samples were then washed with PBS and stained with Hoechst for 5 min at a concentration of 30 mL PBS and 30 μL Hoechst in order to allow for the imaging of the cell nuclei. Three washes of PBS were carried out, and two drops of Invitrogen ProLong Gold antifade solution (ThermoFisher) were added to each sample with 200 μL of PBS. The samples were then imaged using the FL Auto 2 fluorescent microscope (ThermoFisher).
4. Discussion
Consistent with previous studies and theory, the results indicate that the cells preferred natural collagen scaffolds to synthetic PLA scaffolds. The LIVE/DEAD™ assay indicated an increase in the cell viability of the collagen samples from day 1 to day 7 (
Figure 3). A visual assessment of the images suggests that the cells dispersed throughout the collagen scaffolds, migrating throughout the fibers. This suggests that the cells found the microenvironment provided by the collagen scaffolds more favorable. In addition, very few dead cells were present, indicating that the collagen scaffolds introduce little to no cytotoxicity. Notably, the dead cells are not attached to the scaffolds, indicating that those that did die likely failed to attach to the scaffold and thus died not due to a lack of scaffold biocompatibility but rather due to a lack of structural support. This is consistent with previous studies which indicate that collagen is biocompatible with the NIH3T3 cells and aids in cell adhesion and proliferation [
18] and the use of collagen scaffolds in a wide range of applications, from nanostructured mats electrospun alongside glycosaminoglycans for nerve tissue regeneration [
21] to promoting osteogenesis and differentiation for bone tissue engineering [
22].
The images for the PLA scaffolds and NIH 3T3 cells seeded onto them had a different trend. As the test progressed, the density of cells appeared to decrease over time. The cells adhered to the PLA scaffolds during the first day, but the cells detached and died as time progressed. PLA did not support the conditions necessary for maintaining long-term cell adhesion. Phalloidin staining images also supported the trends in adhesion. On day 7, the cells appeared to cover the collagen scaffolds and multiply over the testing period, while in contrast, the cell density decreased in the PLA samples. This suggests that while the synthetic scaffolds did not present cytotoxicity to the cells, they failed to promote the successful attachment and migration of the cells into the scaffolds and thus did not provide a suitable microenvironment for cellular proliferation.
The difference in cellular adhesion between the collagen and PLA samples suggests the existence of a structural difference between the polymer samples that cause different cellular interactions. Collagen is a protein that consists of amino acids, while PLA consists of lactic acid. A 2018 study by Kang and colleagues on modified peptides suggested that incorporating more Arginine–Glycine–Aspartate (RGD) amino acid motifs into films provided greater cellular adhesion [
23]. This was built upon previous work that indicated that the RGD sequence is essential to the cellular recognition of fibronectin and has been found to be the case in multiple natural polymers such as laminin, vitronectin, and fibrin [
24]. Collagen type I contains one or more of these sequences, so it is possible that the RGD sequence is responsible for its greater cellular adhesion [
24].
It is important to note that other factors are also important to the cellular adhesion to a fibrous biomaterial. Material properties such as the fiber diameter, fiber arrangement, cross-sectional shape, and surface hydrophobicity have all been shown to affect cellular adhesion to materials [
25]. Fiber diameters larger than those of cells allow cells to extend along fibers, while diameters smaller than those of cells allow them to wrap around fibers [
25]. Looking at
Figure 2, the fiber diameters between the collagen (12.562 ± 1.352 μm) and PLA (12.595 ± 0.753 μm) samples were relatively similar, with no significant difference. Based on that similarity, it is less likely that general material properties were responsible for the significant difference in adhesion between the samples. In addition, the SEM images in
Figure 2 also indicate that cells adhere along the length of the fiber, regardless of the yarn bundling. It is safer to assume that the most dominant reason for the adhesion differences is structural differences in the polymers used.
Beyond adhesion, the alamarBlue™ data indicated that cellular metabolic activity was also stronger with the collagen samples. This is evident with the much larger average fluorescence values seen in the collagen samples. This means that more cells were proliferating and content in their environment. On the other hand, the trend in the PLA alamarBlue™ data indicated that the cells proliferating on the scaffold decreased over time. In fact, the metabolic activity on the PLA sample was worse than that in the control well. This difference is likely due to the PLA samples having fewer live cells due to less adhesion.
The current understanding of molecular biology indicates that cellular metabolic activity is heavily influenced by cellular adhesion to a bigger extracellular matrix (ECM) [
26]. For cells such as epithelial, endothelial, and muscle cells, previous studies indicate that cells that fail to adhere to the ECM or lose contact with the matrix undergo apoptosis [
26]. With that reference, the difference in metabolic activity between the cells on the collagen and the PLA samples was likely rooted in their structural ability to encourage cellular adhesion and the formation of an ECM. This amplifies the importance of the ability of biomaterials to mimic cellular binding mechanisms for applications such as organ replacement or clinical challenges that are wound-healing in nature.
There are attempts in biomaterials that utilize the idea of tuning synthetic scaffolds to be more biomimetic through the use of natural polymers. For keratoprosthesis challenges, di-amino-PEG that contains the RGD peptide has been grafted onto PMMA surfaces and has restored cellular adhesion, with enhanced attachment compared to untreated PMMA [
27]. The same motif was utilized as a graft onto the surface of Poly(Carbonate-Urea)urethane and improved hepatocyte adhesion [
28]. Besides the most common RGD motif, the laminin motif IKVAV has been utilized in hydrogels to promote neurogenesis [
29]. An excellent review by Li and colleagues touches on incorporating bioactive ingredients in biomaterials for spinal regeneration [
30].
Despite the evidence for incorporating cellular binding mechanisms into tissue engineering, there are some limitations. Incorporating complete proteins increases the opportunity for immunogenic responses and infection. This is due to their susceptibility to proteolytic degradation and the presence of inflammation and infection in vivo, accelerating protein degradation [
31]. Most current attempts utilize presenting motifs that cells recognize in the form of immobilized peptides [
31]. Thus, it is imperative to probe the role of specific motifs in signaling cascades that result in increased cellular attachment and proliferation. This understanding will lead us to more efficient and biomimetic scaffolds for tissue engineering, which can ultimately be used for various applications, including wound healing, the repair and replacement of damaged tissues, and microfluidic models.
Outside of the binding considerations, some additional challenges need to be considered when designing more biomimetic scaffolds. While textile technology approaches tend to offer the advantages of mimicking the ECM and the anisotropic and strain-stiffening tendencies seen across human physiology, there are struggles among preparation techniques [
32]. Specifically, many reviews have indicated that electrospinning is currently the most dominant scaffold preparation in the modern tissue engineering literature but has major challenges with industrial replication due to Rayleigh, axisymmetric, and whipping instability [
32,
33]. Attempts at 3-D biomimetic scaffolds involve different woven, kitted, and braided patterns [
25]. An interesting future direction for biomimetic materials and tissue engineering is utilizing a commercially viable, nanofibrous fabrication technique with bioactive ingredients such as peptide motifs.