Liquid Embolic Agents for Endovascular Embolization: A Review
Abstract
:1. Introduction
2. Clinical Applications of Liquid Embolic Agents
2.1. High-Flow Vascular Malformations
2.2. Hypervascular Tumors
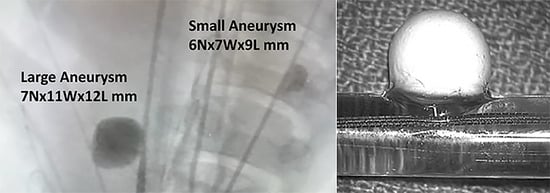
2.3. Aneurysms
3. Liquid Embolics
3.1. Polymerizing Liquid Embolics
3.1.1. Cyanoacrylate Glues
3.1.2. Fibrin Glue
3.1.3. In Situ Gelling Type
Poly(NIPAAm) Based
PPODA-QT/PEGDA-QT Based
3.1.4. Shear-Thinning Biomaterials
3.1.5. Silk Elastin Protein Liquid Embolic (SELP)
3.1.6. Instylla Embrace HES
3.1.7. Alginate
3.2. Precipitating Liquid Embolic Agents
3.2.1. Eudragit-E
3.2.2. Squid
3.2.3. Onyx
3.2.4. PHILTM
3.2.5. EASYXTM
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rautio, R.; Haapanen, A. Transcatheter Embolization of a Renal Artery Aneurysm Using Ethylene Vinyl Alcohol Copolymer. Cardiovasc. Intervent. Radiol. 2007, 30, 300–303. [Google Scholar] [CrossRef] [PubMed]
- Brassel, F.; Meila, D. Evolution of Embolic Agents in Interventional Neuroradiology. Clin. Neuroradiol. 2015, 25, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Jordan, O.; Doelker, E.; Rüfenacht, D.A. Biomaterials Used in Injectable Implants (Liquid Embolics) for Percutaneous Filling of Vascular Spaces. Cardiovasc. Intervent. Radiol. 2005, 28, 561–569. [Google Scholar] [CrossRef]
- Poursaid, A.; Jensen, M.M.; Huo, E.; Ghandehari, H. Polymeric Materials for Embolic and Chemoembolic Applications. J. Control. Release 2016, 240, 414–433. [Google Scholar] [CrossRef]
- Kulshrestha, A.S.; Mahapatro, A. Polymers for Biomedical Applications; American Chemical Society: Washington, DC, USA, 2008; pp. 1–7. [Google Scholar]
- Ray, C.E.; Lawson, M.C.; Bauer, J.R. Embolization Agents. In Image-Guided Interview, 2nd ed.; Mauro, M.A., Ed.; Elsevier Inc.: New York, NY, USA, 2014. [Google Scholar]
- Dunham, G.M.; Ingraham, C.R.; Maki, J.H.; Vaidya, S.S. Finding the Nidus: Detection and Workup of Non–Central Nervous System Arteriovenous Malformations. RadioGraphics 2016, 36, 891–903. [Google Scholar] [CrossRef]
- Legiehn, G.M.; Heran, M.K.S. Classification, Diagnosis, and Interventional Radiologic Management of Vascular Malformations. Orthop. Clin. N. Am. 2006, 37, 435–474. [Google Scholar] [CrossRef]
- Mulligan, P.R.; Prajapati, H.J.S.; Martin, L.G.; Patel, T.H. Vascular Anomalies: Classification, Imaging Characteristics and Implications for Interventional Radiology Treatment Approaches. Br. J. Radiol. 2014, 87, 20130392. [Google Scholar] [CrossRef]
- Vollherbst, D.F.; Sommer, C.M.; Ulfert, C.; Pfaff, J.; Bendszus, M.; Möhlenbruch, M.A. Liquid Embolic Agents for Endovascular Embolization: Evaluation of an Established (Onyx) and a Novel (PHIL) Embolic Agent in an In Vitro AVM Model. Am. J. Neuroradiol. 2017, 38, 1377–1382. [Google Scholar] [CrossRef]
- Wang, X.; Wang, Q.; Chen, G.; Leng, B.; Song, D. Endovascular Treatment of Congenital Brain Arteriovenous Fistulas with Combination of Detachable Coils and Onyx Liquid Embolic Agent. Neuroradiology 2010, 52, 1121–1126. [Google Scholar] [CrossRef] [PubMed]
- Dalyai, R.T.Z.; Schirmer, C.M.; Malek, A.M. Transvenous Balloon-Protected Embolization of a Scalp Arteriovenous Fistula Using Onyx Liquid Embolic. Acta Neurochir. 2011, 153, 1285–1290. [Google Scholar] [CrossRef]
- Kocer, N.; Hanimoglu, H.; Batur, S.; Kandemirli, S.G.; Kizilkilic, O.; Sanus, Z.; Oz, B.; Islak, C.; Kaynar, M.Y. Preliminary Experience with Precipitating Hydrophobic Injectable Liquid in Brain Arteriovenous Malformations. Diagnostic Interv. Radiol. 2016, 22, 184–189. [Google Scholar] [CrossRef]
- Blackburn, S.L.; Kadkhodayan, Y.; Ray, W.Z.; Zipfel, G.J.; Cross, D.T.; Moran, C.J.; Derdeyn, C.P. Onyx Is Associated with Poor Venous Penetration in the Treatment of Spinal Dural Arteriovenous Fistulas. J. Neurointerv. Surg. 2014, 6, 536–540. [Google Scholar] [CrossRef] [PubMed]
- Lamin, S.; Chew, H.S.; Chavda, S.; Thomas, A.; Piano, M.; Quilici, L.; Pero, G.; Holtmannspolter, M.; Cronqvist, M.E.; Casasco, A.; et al. Embolization of Intracranial Dural Arteriovenous Fistulas Using PHIL Liquid Embolic Agent in 26 Patients: A Multicenter Study. Am. J. Neuroradiol. 2017, 38, 127–131. [Google Scholar] [CrossRef] [PubMed]
- Taki, W.; Yonekawa, Y.; Iwata, H.; Uno, A.; Yamashita, K.; Amemiya, H. A New Liquid Material for Embolization of Arteriovenous Malformations. AJNR Am. J. Neuroradiol. 1990, 11, 163–168. [Google Scholar] [PubMed]
- Johnson, C.S.; Chiu, A.; Cheung, A.; Wenderoth, J. Embolization of Cranial Dural Arteriovenous Fistulas in the Liquid Embolic Era: A Sydney Experience. J. Clin. Neurosci. 2018, 49, 62–70. [Google Scholar] [CrossRef]
- Fusco, M.R.; Salem, M.M.; Gross, B.A.; Reddy, A.S.; Ogilvy, C.S.; Kasper, E.M.; Thomas, A.J. Preoperative Embolization of Extra-Axial Hypervascular Tumors with Onyx. J. Cerebrovasc. Endovasc. Neurosurg. 2016, 18, 12. [Google Scholar] [CrossRef]
- Clarençon, F.; Di Maria, F.; Cormier, E.; Sourour, N.-A.; Enkaoua, E.; Sailhan, F.; Iosif, C.; Le Jean, L.; Chiras, J. Onyx Injection by Direct Puncture for the Treatment of Hypervascular Spinal Metastases Close to the Anterior Spinal Artery: Initial Experience. J. Neurosurg. Spine 2013, 18, 606–610. [Google Scholar] [CrossRef]
- Trivelatto, F.; Nakiri, G.S.; Manisor, M.; Riva, R.; Al-Khawaldeh, M.; Kessler, I.; Mounayer, C. Preoperative Onyx Embolization of Meningiomas Fed by the Ophthalmic Artery: A Case Series. Am. J. Neuroradiol. 2011, 32, 1762–1766. [Google Scholar] [CrossRef]
- Brain Aneurysm Foundation: Statistics and Facts. Available online: https://bafound.org/about-brain-aneurysms/brain-aneurysm-basics/brain-aneurysm-statistics-and-facts/ (accessed on 1 May 2023).
- Weber, W.; Siekmann, R.; Kis, B.; Kuehne, D. Treatment and Follow-up of 22 Unruptured Wide-Necked Intracranial Aneurysms of the Internal Carotid Artery with Onyx HD 500. AJNR Am. J. Neuroradiol. 2005, 26, 1909–1915. [Google Scholar]
- Kim, J.-W.; Park, Y.-S. Endovascular Treatment of Wide-Necked Intracranial Aneurysms: Techniques and Outcomes in 15 Patients. J. Korean Neurosurg. Soc. 2011, 49, 97. [Google Scholar] [CrossRef]
- Eddleman, C.S.; Surdell, D.; DiPatri, A.; Tomita, T.; Shaibani, A. Infectious Intracranial Aneurysms in the Pediatric Population: Endovascular Treatment with Onyx. Child’s Nerv. Syst. 2008, 24, 909–915. [Google Scholar] [CrossRef] [PubMed]
- Ameli-Renani, S.; Vasileios Patsiogiannis, R.A.M. Type I Endoleak Embolization With Liquids: Does It Work? Indications, Limitations, and Outcomes of Liquid Embolization of Type I Endoleaks. Endovasc. Today 2018, 17, 77–80. [Google Scholar]
- Fanelli, F.; Falcone, G. Embolization for Type I and Type II Endoleaks An Overview of Embolization Techniques and Materials for These Indications. Endovasc. Today 2020, 19, 72–74. [Google Scholar]
- Kania, R.E.; Sauvaget, E.; Guichard, J.-P.; Chapot, R.; Huy, P.T.B.; Herman, P. Early Postoperative CT Scanning for Juvenile Nasopharyngeal Angiofibroma: Detection of Residual Disease. AJNR Am. J. Neuroradiol. 2005, 26, 82–88. [Google Scholar]
- Rosen, R.J.; Contractor, S. The Use of Cyanoacrylate Adhesives in the Management of Congenital Vascular Malformations. Semin. Intervent. Radiol. 2004, 21, 59–66. [Google Scholar] [CrossRef]
- Bruno, C.A.; Meyers, P.M. Endovascular Management of Arteriovenous Malformations of the Brain. Interv. Neurol. 2012, 1, 109–123. [Google Scholar] [CrossRef]
- Brothers, M.F.; Kaufmann, J.C.; Fox, A.J.; Deveikis, J.P. N-Butyl 2-Cyanoacrylate—Substitute for IBCA in Interventional Neuroradiology: Histopathologic and Polymerization Time Studies. AJNR Am. J. Neuroradiol. 1989, 10, 777–786. [Google Scholar]
- Yonemitsu, T.; Kawai, N.; Sato, M.; Sonomura, T.; Takasaka, I.; Nakai, M.; Minamiguchi, H.; Sahara, S.; Iwasaki, Y.; Naka, T.; et al. Comparison of Hemostatic Durability between N-Butyl Cyanoacrylate and Gelatin Sponge Particles in Transcatheter Arterial Embolization for Acute Arterial Hemorrhage in a Coagulopathic Condition in a Swine Model. Cardiovasc. Intervent. Radiol. 2010, 33, 1192–1197. [Google Scholar] [CrossRef]
- Yonemitsu, T.; Kawai, N.; Sato, M.; Tanihata, H.; Takasaka, I.; Nakai, M.; Minamiguchi, H.; Sahara, S.; Iwasaki, Y.; Shima, Y.; et al. Evaluation of Transcatheter Arterial Embolization with Gelatin Sponge Particles, Microcoils, and N-Butyl Cyanoacrylate for Acute Arterial Bleeding in a Coagulopathic Condition. J. Vasc. Interv. Radiol. 2009, 20, 1176–1187. [Google Scholar] [CrossRef]
- Levrier, O.; Mekkaoui, C.; Rolland, P.H.; Murphy, K.; Cabrol, P.; Moulin, G.; Bartoli, J.M.; Raybaud, C. Efficacy and Low Vascular Toxicity of Embolization with Radical versus Anionic Polymerization of N-Butyl-2-Cyanoacrylate (NBCA). An Experimental Study in the Swine. J. Neuroradiol. 2003, 30, 95–102. [Google Scholar]
- Gailloud, P. Endovascular Treatment of Cerebral Arteriovenous Malformations. Tech. Vasc. Interv. Radiol. 2005, 8, 118–128. [Google Scholar] [CrossRef]
- Senturk, C. Endovascular Treatment of Cerebral Arteriovenous Malformations. In Vascular Malformations of the Central Nervous System; IntechOpen: London, UK, 2020. [Google Scholar]
- Jafar, J.J.; Davis, A.J.; Berenstein, A.; Choi, I.S.; Kupersmith, M.J. The Effect of Embolization with N-Butyl Cyanoacrylate Prior to Surgical Resection of Cerebral Arteriovenous Malformations. J. Neurosurg. 1993, 78, 60–69. [Google Scholar] [CrossRef] [PubMed]
- Chiriac, A.; Baldof, J.; Dobrin, N.; Poeata, I. Embolic Materials for Cerebral Endovascular Theraphy. Rom. Neurosurg. 2010, XVII, 171–181. [Google Scholar]
- Szmigielski, W.; Klamut, M.; Wolski, T.; Studnicki, W.; Rubaj, B. Urogranoic Acid as a Radiopaque Additive to the Cyanoacrylic Adhesive in Transcatheter Obliteration of Renal Arteries. Investig. Radiol. 1981, 16, 65–70. [Google Scholar] [CrossRef]
- Günther, R.; Schubert, U.; Bohl, J.; Georgi, M.; Marberger, M. Transcatheter Embolization of the Kidney with Butyl-2-Cyanoacrylate: Experimental and Clinical Results. Cardiovasc. Radiol. 1978, 1, 101–108. [Google Scholar] [CrossRef] [PubMed]
- n-BCA Trail Investigators N-Butyl Cyanoacrylate Embolization of Cerebral Arteriovenous Malformations: Results of a Prospective, Randomized, Multi-Center Trial. AJNR Am. J. Neuroradiol. 2002, 23, 748–755.
- Jayaraman, M.V.; Marcellus, M.L.; Hamilton, S.; Do, H.M.; Campbell, D.; Chang, S.D.; Steinberg, G.K.; Marks, M.P. Neurologic Complications of Arteriovenous Malformation Embolization Using Liquid Embolic Agents. AJNR Am. J. Neuroradiol. 2008, 29, 242–246. [Google Scholar] [CrossRef]
- Cantasdemir, M.; Adaletli, İ.; Cebi, D.; Kantarci, F.; Selcuk, N.; Numan, F. Emergency Endovascular Embolization of Traumatic Intrarenal Arterial Pseudoaneurysms with N-Butyl Cyanoacrylate. Clin. Radiol. 2003, 58, 560–565. [Google Scholar] [CrossRef] [PubMed]
- Denys, A.; Lacombe, C.; Schneider, F.; Madoff, D.C.; Doenz, F.; Qanadli, S.D.; Halkic, N.; Sauvanet, A.; Vilgrain, V.; Schnyder, P. Portal Vein Embolization with N-Butyl Cyanoacrylate before Partial Hepatectomy in Patients with Hepatocellular Carcinoma and Underlying Cirrhosis or Advanced Fibrosis. J. Vasc. Interv. Radiol. 2005, 16, 1667–1674. [Google Scholar] [CrossRef]
- Miyachi, S.; Izumi, T.; Satow, T.; Srivatanakul, K.; Matsumoto, Y.; Terada, T.; Matsumaru, Y.; Kiyosue, H. Effectiveness of Preradiosurgical Embolization with NBCA for Arteriovenous Malformations—Retrospective Outcome Analysis in a Japanese Registry of 73 Patients (J-REAL Study). Neurointervention 2017, 12, 100–109. [Google Scholar] [CrossRef] [PubMed]
- Razavi, M.K.; Murphy, K. Embolization of Bronchial Arteries with N-Butyl Cyanoacrylate for Management of Massive Hemoptysis: A Technical Review. Tech. Vasc. Interv. Radiol. 2007, 10, 276–282. [Google Scholar] [CrossRef] [PubMed]
- Monsignore, L.M.; Scarpelini, S.; Santos, J.S.; Abud, D.G. Percutaneous Transcatheter Embolization with N-Butyl Cyanoacrylate of Hepatic Hemorrhagic Lesions in Urgent Situations. Diagnostic Interv. Radiol. 2012, 18, 403. [Google Scholar] [CrossRef] [PubMed]
- Pietura, R.; Toborek, M.; Dudek, A.; Boćkowska, A.; Janicka, J.; Piekarski, P. Endovascular Embolization of Varicoceles Using N-Butyl Cyanoacrylate (NBCA) Glue. Polish J. Radiol. 2013, 78, 26–30. [Google Scholar] [CrossRef]
- Yata, S.; Ihaya, T.; Kaminou, T.; Hashimoto, M.; Ohuchi, Y.; Umekita, Y.; Ogawa, T. Transcatheter Arterial Embolization of Acute Arterial Bleeding in the Upper and Lower Gastrointestinal Tract with N-Butyl-2-Cyanoacrylate. J. Vasc. Interv. Radiol. 2013, 24, 422–431. [Google Scholar] [CrossRef]
- Won, Y.; Lee, S.L.; Kim, Y.; Ku, Y.M. Clinical Efficacy of Transcatheter Embolization of Visceral Artery Pseudoaneurysms Using N-Butyl Cyanoacrylate (NBCA). Diagn. Interv. Imaging 2015, 96, 563–569. [Google Scholar] [CrossRef] [PubMed]
- Hassan, F.; Younes, A.; Rifai, M. Endovascular Embolization of Post-Tonsillectomy Pseudoaneurysm: A Single-Center Case Series. Cardiovasc. Intervent. Radiol. 2019, 42, 528–533. [Google Scholar] [CrossRef]
- Ugajin, A.; Fujii, H.; Nakamura, H.; Fujita, A.; Sasaki, T.; Mato, N.; Sugimoto, H. Transcatheter Proximal Coil Blocking with N-Butyl-2-Cyanoacrylate Injection via the Pulmonary Artery Alone for Rasmussen’s Aneurysm. Case Rep. Radiol. 2019, 2019, 1725238. [Google Scholar] [CrossRef]
- Bae, S.H. Transcatheter Embolization of the Esophagomediastinal Fistula with N-Butyl Cyanoacrylate Glue: A Case Report. Int. J. Surg. Case Rep. 2019, 65, 73–77. [Google Scholar] [CrossRef]
- Richling, B. Homologous Controlled-Viscosity Fibrin for Endovascular Embolization. Acta Neurochir. 1982, 64, 109–124. [Google Scholar] [CrossRef]
- Berguer, R.; Staerkel, R.L.; Moore, E.E.; Moore, F.A.; Galloway, W.B.; Mockus, M.B. Warning: Fatal Reaction to the Use of Fibrin Glue in Deep Hepatic Wounds. Case Reports. J. Trauma 1991, 31, 408–411. [Google Scholar] [CrossRef]
- Duarte, A.P.; Coelho, J.F.; Bordado, J.C.; Cidade, M.T.; Gil, M.H. Surgical Adhesives: Systematic Review of the Main Types and Development Forecast. Prog. Polym. Sci. 2012, 37, 1031–1050. [Google Scholar] [CrossRef]
- Nagino, M.; Kamiya, J.; Kanai, M.; Uesaka, K.; Sano, T.; Yamamoto, H.; Hayakawa, N.; Nimura, Y. Right Trisegment Portal Vein Embolization for Biliary Tract Carcinoma: Technique and Clinical Utility. Surgery 2000, 127, 155–160. [Google Scholar] [CrossRef] [PubMed]
- Olthof, P.B.; Huisman, F.; van Golen, R.F.; Cieslak, K.P.; van Lienden, K.P.; Plug, T.; Meijers, J.C.M.; Heger, M.; Verheij, J.; van Gulik, T.M. Use of an Absorbable Embolization Material for Reversible Portal Vein Embolization in an Experimental Model. Br. J. Surg. 2016, 103, 1306–1315. [Google Scholar] [CrossRef] [PubMed]
- Probst, E.N.; Grzyska, U.; Westphal, M.; Zeumer, H. Preoperative Embolization of Intracranial Meningiomas with a Fibrin Glue Preparation. AJNR Am. J. Neuroradiol. 1999, 20, 1695–1702. [Google Scholar] [PubMed]
- Beese, R.C.; Tomlinson, M.A.; Buckenham, T.M. Endoluminal Embolization of Bilateral Atherosclerotic Common Iliac Aneurysms with Fibrin Tissue Glue (Beriplast). Cardiovasc. Intervent. Radiol. 2000, 23, 239–241. [Google Scholar] [CrossRef]
- Kim, I.-M.; Yim, M.-B.; Lee, C.-Y.; Son, E.-I.; Kim, D.-W.; Kim, S.-P.; Sohn, C.-H. Merits of Intralesional Fibrin Glue Injection in Surgery for the Cavernous Sinus Cavernous Hemangiomas. J. Neurosurg. 2002, 97, 718–721. [Google Scholar] [CrossRef] [PubMed]
- Meyer, F.; Ricke, J.; Pech, M.; Lippert, H.; Halloul, Z. Impressive Closure of a Sustaining Periprosthetic Endoleak (Type II) Using Fibrin Glue Application after Former Endovascular Placement of an Infrarenal Aortic Prosthesis. Int. J. Surg. 2009, 7, 84–86. [Google Scholar] [CrossRef] [PubMed]
- Piazza, M.; Frigatti, P.; Scrivere, P.; Bonvini, S.; Noventa, F.; Ricotta, J.J.; Grego, F.; Antonello, M. Role of Aneurysm Sac Embolization during Endovascular Aneurysm Repair in the Prevention of Type II Endoleak-Related Complications. J. Vasc. Surg. 2013, 57, 934–941. [Google Scholar] [CrossRef]
- Piazza, M.; Squizzato, F.; Zavatta, M.; Menegolo, M.; Ricotta, J.J.; Lepidi, S.; Grego, F.; Antonello, M. Outcomes of Endovascular Aneurysm Repair with Contemporary Volume-Dependent Sac Embolization in Patients at Risk for Type II Endoleak. J. Vasc. Surg. 2016, 63, 32–38. [Google Scholar] [CrossRef]
- Choi, K.-M.; Kim, Y.-D.; Ahn, J.-H. Closure of Pancreatoduodenal Fistula Using Vascular Occluding Coil Embolization and Fibrin Glue Injection: A Case Study. Korean J. Hepato-Biliary-Pancreat. Surg. 2013, 17, 75. [Google Scholar] [CrossRef]
- Cui, Z.; Lee, B.H.; Pauken, C.; Vernon, B.L. Degradation, Cytotoxicity, and Biocompatibility of NIPAAm-Based Thermosensitive, Injectable, and Bioresorbable Polymer Hydrogels. J. Biomed. Mater. Res. Part A 2011, 98, 159–166. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.H.; Leon, C.; McLemore, R.; Macias, J.V.; Vernon, B.L. Synthesis and Characterization of Thermo-Sensitive Radio-Opaque Poly(N-Isopropylacrylamide-Co-PEG-2-Iodobenzoate). J. Biomater. Sci. Polym. Ed. 2011, 22, 2357–2367. [Google Scholar] [CrossRef] [PubMed]
- Bearat, H.H.; Lee, B.H.; Valdez, J.; Vernon, B.L. Synthesis, Characterization and Properties of a Physically and Chemically Gelling Polymer System Using Poly(NIPAAm-Co-HEMA-Acrylate) and Poly(NIPAAm-Co-Cysteamine). J. Biomater. Sci. Polym. Ed. 2010, 22, 1299–1318. [Google Scholar] [CrossRef] [PubMed]
- Bearat, H.H.; Preul, M.C.; Vernon, B.L. Cytotoxicity, in Vitro Models and Preliminary in Vivo Study of Dual Physical and Chemical Gels for Endovascular Embolization of Cerebral Aneurysms. J. Biomed. Mater. Res. Part A 2013, 101, 2515–2525. [Google Scholar] [CrossRef] [PubMed]
- Hu, J.; Albadawi, H.; Chong, B.W.; Deipolyi, A.R.; Sheth, R.A.; Khademhosseini, A.; Oklu, R. Advances in Biomaterials and Technologies for Vascular Embolization. Adv. Mater. 2019, 31, 1901071. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.H.; West, B.; McLemore, R.; Pauken, C.; Vernon, B.L. In-Situ Injectable Physically and Chemically Gelling NIPAAm-Based Copolymer System for Embolization. Biomacromolecules 2006, 7, 2059–2064. [Google Scholar] [CrossRef]
- Lee, B.H.; Beart, H.H.; Cheng, V.; McLemore, R.; Robb, S.A.; Cui, Z.; Dovigi, A.; Vernon, B.L. In Vitro and in Vivo Demonstration of Physically and Chemically in Situ Gelling NIPAAm-Based Copolymer System. J. Biomater. Sci. Polym. Ed. 2013, 24, 1575–1588. [Google Scholar] [CrossRef] [PubMed]
- Matsumaru, Y.; Hyodo, A.; Nose, T.; Ito, S.; Hirano, T.; Ohashi, S. Application of Thermosensitive Polymers as a New Embolic Material for Intravascular Neurosurgery. J. Biomater. Sci. Polym. Ed. 1996, 7, 795–804. [Google Scholar] [CrossRef]
- An, Y.H.; Basso, V.M.; Gutowska, A.; Mironov, V.A. 2000 Transactions of the Sixth World Biomaterials Congress, Kamuela, HI, USA, 15–20 May 2000; Society for Biomaterials: Minneapolis, MN, USA, 2000; p. 568. [Google Scholar]
- Vernon, B.; Martinez, A. Gel Strength and Solution Viscosity of Temperature-Sensitive, in-Situ-Gelling Polymers for Endovascular Embolization. J. Biomater. Sci. Polym. Ed. 2005, 16, 1153–1166. [Google Scholar] [CrossRef]
- Li, X.; Liu, W.; Ye, G.; Zhang, B.; Zhu, D.; Yao, K.; Liu, Z.; Sheng, X. Thermosensitive N-Isopropylacrylamide–N–Propylacrylamide-Vinyl Pyrrolidone Terpolymers: Synthesis, Characterization and Preliminary Application as Embolic Agents. Biomaterials 2005, 26, 7002–7011. [Google Scholar] [CrossRef]
- Robb, S.A.; Lee, B.H.; McLemore, R.; Vernon, B.L. Simultaneously Physically and Chemically Gelling Polymer System Utilizing a Poly(NIPAAm-Co-Cysteamine)-Based Copolymer. Biomacromolecules 2007, 8, 2294–2300. [Google Scholar] [CrossRef]
- Dai, F.; Tang, L.; Yang, J.; Zhao, X.; Liu, W.; Chen, G.; Xiao, F.; Feng, X. Fast Thermoresponsive BAB-Type HEMA/NIPAAm Triblock Copolymer Solutions for Embolization of Abnormal Blood Vessels. J. Mater. Sci. Mater. Med. 2009, 20, 967–974. [Google Scholar] [CrossRef]
- Zhao, Y.; Zheng, C.; Wang, Q.; Fang, J.; Zhou, G.; Zhao, H.; Yang, Y.; Xu, H.; Feng, G.; Yang, X. Permanent and Peripheral Embolization: Temperature-Sensitive p(N-Isopropylacrylamide-Co-Butyl Methylacrylate) Nanogel as a Novel Blood-Vessel-Embolic Material in the Interventional Therapy of Liver Tumors. Adv. Funct. Mater. 2011, 21, 2035–2042. [Google Scholar] [CrossRef]
- Zhao, H.; Zheng, C.; Feng, G.; Zhao, Y.; Liang, H.; Wu, H.; Zhou, G.; Liang, B.; Wang, Y.; Xia, X. Temperature-Sensitive Poly( N -Isopropylacrylamide-Co-Butyl Methylacrylate) Nanogel as an Embolic Agent: Distribution, Durability of Vascular Occlusion, and Inflammatory Reactions in the Renal Artery of Rabbits. Am. J. Neuroradiol. 2013, 34, 169–176. [Google Scholar] [CrossRef] [PubMed]
- Bearat, H.H.; Lee, B.H.; Vernon, B.L. Comparison of Properties between NIPAAm-Based Simultaneously Physically and Chemically Gelling Polymer Systems for Use in Vivo. Acta Biomater. 2012, 8, 3629–3642. [Google Scholar] [CrossRef]
- Vernon, B.; Birdno, M.; Preul, M.C. In Situ Gelling Self-Reactive Materials for Embolization. U.S. Patent US 8,048,407, 1 November 2011. [Google Scholar]
- Lord, J.; Britton, H.; Spain, S.G.; Lewis, A.L. Advancements in the Development on New Liquid Embolic Agents for Use in Therapeutic Embolisation. J. Mater. Chem. B 2020, 8, 8207–8218. [Google Scholar] [CrossRef] [PubMed]
- Riley, C.M.; McLemore, R.; Preul, M.C.; Vernon, B.L. Gelling Process Differences in Reverse Emulsion, in Situ Gelling Polymeric Materials for Intracranial Aneurysm Embolization, Formulated with Injectable Contrast Agents. J. Biomed. Mater. Res. Part B 2011, 96, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Brennecka, C.R.; Preul, M.C.; Vernon, B.L. In Vitro Delivery, Cytotoxicity, Swelling, and Degradation Behavior of a Liquid-to-Solid Gelling Polymer System for Cerebral Aneurysm Embolization. J. Biomed. Mater. Res. Part B Appl. Biomater. 2012, 100B, 1298–1309. [Google Scholar] [CrossRef]
- Brennecka, C.R.; Preul, M.C.; Bichard, W.D.; Vernon, B.L. In Vivo Experimental Aneurysm Embolization in a Swine Model with a Liquid-to-Solid Gelling Polymer System: Initial Biocompatibility and Delivery Strategy Analysis. World Neurosurg. 2012, 78, 469–480. [Google Scholar] [CrossRef] [PubMed]
- Brennecka, C.R.; Preul, M.C.; Becker, T.A.; Vernon, B.L. In Vivo Embolization of Lateral Wall Aneurysms in Canines Using the Liquid-to-Solid Gelling PPODA-QT Polymer System: 6-Month Pilot Study. J. Neurosurg. 2013, 119, 228–238. [Google Scholar] [CrossRef]
- Soodak, K.F.; Brennecka, C.R.; Vernon, B.L. In Vitro Characteristics of a Gelling PEGDA-QT Polymer System with Model Drug Release for Cerebral Aneurysm Embolization. J. Biomed. Mater. Res. Part B Appl. Biomater. 2013, 101, 1477–1488. [Google Scholar] [CrossRef] [PubMed]
- Avery, R.K.; Albadawi, H.; Akbari, M.; Zhang, Y.S.; Duggan, M.J.; Sahani, D.V.; Olsen, B.D.; Khademhosseini, A.; Oklu, R. An Injectable Shear-Thinning Biomaterial for Endovascular Embolization. Sci. Transl. Med. 2016, 8, 365ra156. [Google Scholar] [CrossRef] [PubMed]
- Xue, C.; Xie, H.; Eichenbaum, J.; Chen, Y.; Wang, Y.; van den Dolder, F.W.; Lee, J.; Lee, K.; Zhang, S.; Sun, W.; et al. Synthesis of Injectable Shear-Thinning Biomaterials of Various Compositions of Gelatin and Synthetic Silicate Nanoplatelet. Biotechnol. J. 2020, 15, e1900456. [Google Scholar] [CrossRef]
- Poursaid, A.; Price, R.; Tiede, A.; Olson, E.; Huo, E.; McGill, L.; Ghandehari, H.; Cappello, J. In Situ Gelling Silk-Elastinlike Protein Polymer for Transarterial Chemoembolization. Biomaterials 2015, 57, 142–152. [Google Scholar] [CrossRef] [PubMed]
- Griswold, E.; Cappello, J.; Ghandehari, H. Silk-Elastinlike Protein-Based Hydrogels for Drug Delivery and Embolization. Adv. Drug Deliv. Rev. 2022, 191, 114579. [Google Scholar] [CrossRef]
- Jensen, M.M.; Hatlevik, Ø.; Steinhauff, D.D.; Griswold, E.D.; Wei, X.; Isaacson, K.J.; Barber, Z.B.; Huo, E.; Taussky, P.; Jedrzkiewicz, J.; et al. Protein-Based Polymer Liquid Embolics for Cerebral Aneurysms. Acta Biomater. 2022, 151, 174–182. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.; Zhang, Y.; Lu, Z.; Wang, X.; Bai, S.; Chen, Y.; Mao, J.; Liu, G. Liquid Embolic Agents for Interventional Embolization. ChemPhysMater 2022, 1, 39–50. [Google Scholar] [CrossRef]
- Bendok, B.R.; Abi-Aad, K.R.; Ward, J.D.; Kniss, J.F.; Kwasny, M.J.; Rahme, R.J.; Aoun, S.G.; El Ahmadieh, T.Y.; El Tecle, N.E.; Zammar, S.G.; et al. The Hydrogel Endovascular Aneurysm Treatment Trial (HEAT). Neurosurgery 2020, 86, 615–624. [Google Scholar] [CrossRef]
- Ganguli, S.; Lareau, R.; Jarrett, T.; Soulen, M.C. A Water-Based Liquid Embolic: Evaluation of Its Safety and Efficacy in a Rabbit Kidney Model. J. Vasc. Interv. Radiol. 2021, 32, 813–818. [Google Scholar] [CrossRef]
- Goh, G.S.; Goodwin, M.D.; Huang, J.-F.; Kavnoudias, H.; Holden, A. A Pilot First-in-Human Study of Embrace, a Polyethylene Glycol-Based Liquid Embolic Agent, in the Embolization of Malignant and Benign Hypervascular Tumors. J. Vasc. Interv. Radiol. 2022, 33, 660–667. [Google Scholar] [CrossRef]
- Raymond, J.; Metcalfe, A.; Desfaits, A.C.; Ribourtout, E.; Salazkin, I.; Gilmartin, K.; Embry, G.; Boock, R.J. Alginate for endovascular treatment of aneurysms and local growth factor delivery. AJNR Am. J. Neuroradiol. 2003, 24, 1214–1221. [Google Scholar] [PubMed]
- Becker, T.A.; Preul, M.C.; Bichard, W.D.; Kipke, D.R.; McDougall, C.G. Calcium alginate gel as a biocompatible material for endovascular arteriovenous malformation embolization: Six-month results in an animal model. Neurosurgery 2005, 56, 793–801, discussion 793–801. [Google Scholar] [CrossRef]
- Becker, T.A.; Preul, M.C.; Bichard, W.D.; Kipke, D.R.; McDougall, C.G. Preliminary investigation of calcium alginate gel as a biocompatible material for endovascular aneurysm embolization in vivo. Neurosurgery 2007, 60, 1119–1128. [Google Scholar] [CrossRef]
- Fan, L.; Duan, M.; Xie, Z.; Pan, K.; Wang, X.; Sun, X.; Wang, Q.; Rao, W.; Liu, J. Injectable and Radiopaque liquid metal/calcium alginate hydrogels for endovascular embolization and tumor embolotherapy. Small 2020, 16, e1903421. [Google Scholar] [CrossRef]
- Evonik Eudragit Brochure. Available online: https://www.scribd.com/document/360752511/Evonik-Eudragit-Brochure (accessed on 1 May 2023).
- Tamura, G.; Kato, N.; Yamazaki, T.; Akutsu, Y.; Hosoo, H.; Kasuya, H.; Sonobe, M. Endovascular Embolization of Brain Arteriovenous Malformations with Eudragit-E. Neurol. Med. Chir. 2015, 55, 253–260. [Google Scholar] [CrossRef] [PubMed]
- Bogataj, M.; Mrhar, A.; Kristl, A.; Kozjek, F. Eudragit E Microspheres Containing Bacampicillin: Preparation by Solvent Removal Methods. J. Microencapsul. 1991, 8, 401–406. [Google Scholar] [CrossRef]
- Yamashita, K.; Taki, W.; Kikuchi, H.; Iwata, H.; Yamashita, K. A Cationic Polymer, Eudragit-E, as a New Liquid Embolic Material for Arteriovenous Malformations. Neuroradiology 1996, 38, S151–S156. [Google Scholar] [CrossRef]
- Sadato, A.; Numaguchi, Y.; Taki, W.; Iwata, H.; Yamshita, K. Nonadhesive Liquid Embolic Agent: Role of Its Components in Histologic Changes in Embolized Arteries. Acad. Radiol. 1998, 5, 198–206. [Google Scholar] [CrossRef] [PubMed]
- Arakawa, H.; Murayama, Y.; Davis, C.R.; Howard, D.L.; Baumgardner, W.L.; Marks, M.P.; Do, H.M. Endovascular Embolization of the Swine Rete Mirabile with Eudragit-E 100 Polymer. Am. J. Neuroradiol. 2007, 28, 1191–1196. [Google Scholar] [CrossRef]
- Squid: The New Liquid Embolic Device. Available online: https://biotech-ec.com/dist/pdfs/Squid_Brochure-black_oct2012.pdf#:~:text=The%20New%20Liquid%20Embolic%20device%20Non%20adhesive%20liquid,SQUID%20must%20be%20injected%20through%20a%20COMPATIBLE%20microcatheter (accessed on 1 May 2023).
- Pop, R.; Mertz, L.; Ilyes, A.; Mihoc, D.; Richter, J.S.; Manisor, M.; Kremer, S.; Beaujeux, R. Beam Hardening Artifacts of Liquid Embolic Agents: Comparison between Squid and Onyx. J. Neurointerv. Surg. 2019, 11, 706–709. [Google Scholar] [CrossRef]
- Ilkay, A.; Ergun, D.; Tunca, K.; Fatih, A.; Mert, S.; Ahmet, P.; Shehram, D.; Dogan, D.; Deniz, B.; Anil, A. Preliminary Experience with Squid: A New Liquid Embolizing Agent for Avm, Av Fistulas and Tumors. Turk. Neurosurg. 2014, 24, 565–570. [Google Scholar] [CrossRef]
- Kannath, S.; Rajan, J. Percutaneous Embolization of Scalp Arteriovenous Malformation Using New Liquid Embolic Agent, SQUID: A Technical Report. J. Clin. Interv. Radiol. ISVIR 2017, 1, 171–174. [Google Scholar] [CrossRef]
- Torcia, P.; Squarza, S.; Rossi, U.G.; Rigamonti, P.; Pescatori, L.C.; Damiani, G.; Cariati, M. Endovascular Embolization of Spontaneous Iliopsoas Hematoma: First Experience with Squidperi. Case Rep. Radiol. 2018, 2018, 4694931. [Google Scholar] [CrossRef]
- Venturini, M.; Lanza, C.; Marra, P.; Colarieti, A.; Panzeri, M.; Augello, L.; Gusmini, S.; Salvioni, M.; De Cobelli, F.; Del Maschio, A. Transcatheter Embolization with Squid, Combined with Other Embolic Agents or Alone, in Different Abdominal Diseases: A Single-Center Experience in 30 Patients. CVIR Endovasc. 2019, 2, 8. [Google Scholar] [CrossRef] [PubMed]
- Venturini, M.; Marra, P.; Augello, L.; Colarieti, A.; Guazzarotti, G.; Palumbo, D.; Lanza, C.; Melissano, G.; Chiesa, R.; De Cobelli, F. Elective Embolization of Splenic Artery Aneurysms with an Ethylene Vinyl Alcohol Copolymer Agent (Squid) and Detachable Coils. J. Vasc. Interv. Radiol. 2020, 31, 1110–1117. [Google Scholar] [CrossRef]
- Venturini, M.; Della Corte, A.; Lanza, C.; Fontana, F.; Chiesa, R.; De Cobelli, F. Embolization of 2 Coexisting Intraparenchymal Renal Artery Aneurysms with an Ethylene Vinyl Alcohol Copolymer Agent (Squid) and Coils. Cardiovasc. Intervent. Radiol. 2020, 43, 942–944. [Google Scholar] [CrossRef]
- Lozupone, E.; Bracco, S.; Trombatore, P.; Milonia, L.; D’Argento, F.; Alexandre, A.; Valente, I.; Semeraro, V.; Cioni, S.; Pedicelli, A. Endovascular Treatment of Cerebral Dural Arteriovenous Fistulas with SQUID 12. Interv. Neuroradiol. 2020, 26, 651–657. [Google Scholar] [CrossRef]
- Jabre, R.; Bernat, A.-L.; Peres, R.; Froelich, S. Brain Abscesses After Endovascular Embolization of a Brain Arteriovenous Malformation with Squid. World Neurosurg. 2019, 132, 29–32. [Google Scholar] [CrossRef]
- Moreno-Paredes, S.; Rodríguez-Alcalá, L.; Martín-Lagos Martínez, J.; Müller Locatelli, N.; Vázquez López, C.; Vargas Fernández, J.L.; Cabrera Peña, Á. Facial Palsy after Embolization with Squid® 12. BMC Neurol. 2021, 21, 45. [Google Scholar] [CrossRef]
- Chandra, R.V.; Leslie-Mazwi, T.M.; Mehta, B.P.; Yoo, A.J.; Rabinov, J.D.; Pryor, J.C.; Hirsch, J.A.; Nogueira, R.G. Transarterial Onyx Embolization of Cranial Dural Arteriovenous Fistulas: Long-Term Follow-Up. Am. J. Neuroradiol. 2014, 35, 1793–1797. [Google Scholar] [CrossRef] [PubMed]
- Ierardi, A.M.; Femia, M.; Petrillo, M.; Angileri, S.A.; Hörer, T.; Carrafiello, G. Onyx Liquid Embolic System (LES): An Underestimated Tool in the Management of Peripheral Bleedings. J. Endovasc. Resusc. Trauma Manag. 2018, 2, 49–56. [Google Scholar] [CrossRef]
- Siekmann, R. Basics and Principles in the Application of Onyx LD Liquid Embolic System in the Endovascular Treatment of Cerebral Arteriovenous Malformations. Interv. Neuroradiol. 2005, 11, 131–140. [Google Scholar] [CrossRef]
- Ashour, R.; Ali Aziz-Sultan, M. Onyx HD-500 for Embolization of Cerebral Aneurysms. Neurol. Res. 2014, 36, 363–367. [Google Scholar] [CrossRef]
- Loffroy, R.; Favelier, S.; Genson, P.-Y.; Guiu, B. Onyx for Embolization of Life-Threatening Hemoptysis: A Promising but Luxury Embolic Agent! Cardiovasc. Intervent. Radiol. 2012, 35, 221. [Google Scholar] [CrossRef] [PubMed]
- Chaloupka, J.C.; Viñuela, F.; Vinters, H.V.; Robert, J. Technical Feasibility and Histopathologic Studies of Ethylene Vinyl Copolymer (EVAL) Using a Swine Endovascular Embolization Model. AJNR Am. J. Neuroradiol. 1994, 15, 1107–1115. [Google Scholar] [PubMed]
- Chaloupka, J.C.; Huddle, D.C.; Alderman, J.; Fink, S.; Hammond, R.; Vinters, H. V A Reexamination of the Angiotoxicity of Superselective Injection of DMSO in the Swine Rete Embolization Model. Am. J. Neuroradiol. 1999, 20, 401–410. [Google Scholar]
- Xu, F.; Ni, W.; Liao, Y.; Gu, Y.; Xu, B.; Leng, B.; Song, D. Onyx Embolization for the Treatment of Brain Arteriovenous Malformations. Acta Neurochir. 2011, 153, 869–878. [Google Scholar] [CrossRef] [PubMed]
- Soltanolkotabi, M.; Schoeneman, S.E.; Alden, T.D.; Hurley, M.C.; Ansari, S.A.; DiPatri, A.J.; Tomita, T.; Shaibani, A. Onyx Embolization of Intracranial Arteriovenous Malformations in Pediatric Patients. J. Neurosurg. Pediatr. 2013, 11, 431–437. [Google Scholar] [CrossRef]
- Aoude, A.; Ghanaati, H.; Faghih Jouibari, M.; Shakiba, M.; Khaleghi, M.; Nowrouzi, A. Embolization of Intracranial Arteriovenous Malformations Using Onyx in 53 Patients. Iran. J. Radiol. 2016, in press. [Google Scholar] [CrossRef]
- Singfer, U.; Hemelsoet, D.; Vanlangenhove, P.; Martens, F.; Verbeke, L.; Van Roost, D.; Defreyne, L. Unruptured Brain Arteriovenous Malformations. Stroke 2017, 48, 3393–3396. [Google Scholar] [CrossRef]
- Numan, F.; Ömeroğlu, A.; Kara, B.; Cantaşdemir, M.; Adaletli, İ.; Kantarcı, F. Embolization of Peripheral Vascular Malformations with Ethylene Vinyl Alcohol Copolymer (Onyx). J. Vasc. Interv. Radiol. 2004, 15, 939–946. [Google Scholar] [CrossRef]
- Saeed Kilani, M.; Lepennec, V.; Petit, P.; Magalon, G.; Casanova, D.; Bartoli, J.-M.; Vidal, V. Embolization of Peripheral High-Flow Arteriovenous Malformations with Onyx. Diagn. Interv. Imaging 2017, 98, 217–226. [Google Scholar] [CrossRef]
- Né, R.; Chevallier, O.; Falvo, N.; Facy, O.; Berthod, P.-E.; Galland, C.; Gehin, S.; Midulla, M.; Loffroy, R. Embolization with Ethylene Vinyl Alcohol Copolymer (Onyx®) for Peripheral Hemostatic and Non-Hemostatic Applications: A Feasibility and Safety Study. Quant. Imaging Med. Surg. 2018, 8, 280–290. [Google Scholar] [CrossRef]
- Giurazza, F.; Corvino, F.; Cangiano, G.; Cavaglià, E.; Amodio, F.; Silvestre, M.; De Magistris, G.; Niola, R. Transarterial Embolization of Peripheral High-Flow Arteriovenous Malformation with Ethylene Vinyl Alcohol Copolymer (Onyx®): Single-Center 10-Year Experience. Radiol. Med. 2019, 124, 154–162. [Google Scholar] [CrossRef]
- Kim, S.T.; Jeong, H.W.; Seo, J. Onyx Embolization of Dural Arteriovenous Fistula, Using Scepter C Balloon Catheter: A Case Report. Neurointervention 2013, 8, 110. [Google Scholar] [CrossRef]
- Kawamura, Y.; Takigawa, T.; Hyodo, A.; Suzuki, K. Embolization of Dural Arteriovenous Fistula of the Sinus Confluence with Onyx Using Dual-Lumen Microballoon Catheter: A Case Report. Biomed. J. Sci. Tech. Res. 2018, 6, 5059–5060. [Google Scholar] [CrossRef]
- Patel, A.S.; Horton, T.G.; Kalapos, P.; Cockroft, K.M. Onyx-HD 500 Embolization of a Traumatic Internal Carotid Artery Pseudoaneurysm after Transsphenoidal Surgery. J. Neuroimaging 2015, 25, 656–659. [Google Scholar] [CrossRef]
- Lu, X.; Zhang, X. OnyxTM Embolization for an Angiographically Progressive Traumatic Pseudoaneurysm of the Middle Meningeal Artery: A Case Report and Literature Review. Exp. Ther. Med. 2019, 17, 4144–4148. [Google Scholar] [CrossRef]
- Lupattelli, T.; Abubacker, Z.; Morgan, R.; Belli, A.-M. Embolization of a Renal Artery Aneurysm Using Ethylene Vinyl Alcohol Copolymer (Onyx). J. Endovasc. Ther. 2003, 10, 366–370. [Google Scholar] [CrossRef]
- Jarauta Francisco Javier, M.; Clint, J.-L.; Insausti, I.; Belzunegui, T.; Urtasun, F. Embolization with Onyx Liquid Embolic Agent of a Ruptured Splenic Artery Aneurysm. Resuscitation 2010, 81, S85. [Google Scholar] [CrossRef]
- Larzon, T.; Mathisen, S.R. Internal Sealing of Acute Aortic Bleeding with a Catheter-Delivered Liquid to Solid Embolic Agent (Onyx). Vascular 2010, 18, 106–110. [Google Scholar] [CrossRef]
- Jamieson, R.W.; Bachoo, P.; Tambyraja, A.L. Evidence for Ethylene-Vinyl-Alcohol-Copolymer Liquid Embolic Agent as a Monotherapy in Treatment of Endoleaks. Eur. J. Vasc. Endovasc. Surg. 2016, 51, 810–814. [Google Scholar] [CrossRef] [PubMed]
- Martin, M.L.; Dolmatch, B.L.; Fry, P.D.; Machan, L.S. Treatment of Type II Endoleaks with Onyx. J. Vasc. Interv. Radiol. 2001, 12, 629–632. [Google Scholar] [CrossRef] [PubMed]
- Ling, A.J.; Pathak, R.; Garbowski, M.; Nadkarni, S. Treatment of a Large Type II Endoleak via Extraperitoneal Dissection and Embolization of a Collateral Vessel Using Ethylene Vinyl Alcohol Copolymer (Onyx). J. Vasc. Interv. Radiol. 2007, 18, 659–662. [Google Scholar] [CrossRef] [PubMed]
- Khaja, M.S.; Park, A.W.; Swee, W.; Evans, A.J.; Fritz Angle, J.; Turba, U.C.; Sabri, S.S.; Matsumoto, A.H. Treatment of Type II Endoleak Using Onyx With Long-Term Imaging Follow-Up. Cardiovasc. Intervent. Radiol. 2014, 37, 613–622. [Google Scholar] [CrossRef] [PubMed]
- Scallan, O.; Kribs, S.; Power, A.H.; DeRose, G.; Duncan, A.; Dubois, L. Onyx versus Coil Embolization for the Treatment of Type II Endoleaks. J. Vasc. Surg. 2021, 73, 1966–1972. [Google Scholar] [CrossRef] [PubMed]
- Alobaidi, H.; Kribs, S. Superiority of Intrasac Ethylene Vinyl Alcohol Copolymer Liquid Embolic (Onyx®) Embolization Compared with Other Embolization Agents and Techniques for the Treatment of Type II Endoleaks Following Endovascular Stent-Graft Treatment of Abdominal Aortic Ane. Proc. Arab. J. Interv. Radiol. 2018, 2, S27. [Google Scholar]
- Grisafi, J.L.; Boiteau, G.; Detschelt, E.; Potts, J.; Kiproff, P.; Muluk, S.C. Endoluminal Treatment of Type IA Endoleak with Onyx. J. Vasc. Surg. 2010, 52, 1346–1349. [Google Scholar] [CrossRef]
- Henrikson, O.; Roos, H.; Falkenberg, M. Ethylene Vinyl Alcohol Copolymer (Onyx) to Seal Type 1 Endoleak. A New Technique. Vascular 2011, 19, 77–81. [Google Scholar] [CrossRef]
- Cobb, R.J.; Patterson, B.; Karthikesalingam, A.; Morgan, R.; Thompson, M.; Loftus, I. Onyx: A Novel Solution for a Mycotic Aneurysm. Cardiovasc. Intervent. Radiol. 2014, 37, 541–543. [Google Scholar] [CrossRef]
- Eberhardt, K.M.; Sadeghi-Azandaryani, M.; Worlicek, S.; Koeppel, T.; Reiser, M.F.; Treitl, M. Treatment of Type I Endoleaks Using Transcatheter Embolization With Onyx. J. Endovasc. Ther. 2014, 21, 162–171. [Google Scholar] [CrossRef]
- Ameli-Renani, S.; Pavlidis, V.; Morgan, R.A. Early and Midterm Outcomes after Transcatheter Embolization of Type I Endoleaks in 25 Patients. J. Vasc. Surg. 2017, 65, 346–355. [Google Scholar] [CrossRef]
- Gore, P.; Theodore, N.; Brasiliense, L.; Kim, L.J.; Garrett, M.; Nakaji, P.; Gonzalez, L.F.; McDougall, C.G.; Albuquerque, F.C. The utility of onyx for preoperative embolization of cranial and spinal tumors. Neurosurgery 2008, 62, 1204–1212. [Google Scholar] [CrossRef] [PubMed]
- Rangel-Castilla, L.; Shah, A.H.; Klucznik, R.P.; Diaz, O.M. Preoperative Onyx Embolization of Hypervascular Head, Neck, and Spinal Tumors. Experience with 100 Consecutive Cases from a Single Tertiary Center. J. Neurointerv. Surg. 2014, 6, 51–56. [Google Scholar] [CrossRef] [PubMed]
- Luzzi, S.; Del Maestro, M.; Bongetta, D.; Zoia, C.; Giordano, A.V.; Trovarelli, D.; Raysi Dehcordi, S.; Galzio, R.J. Onyx Embolization Before the Surgical Treatment of Grade III Spetzler-Martin Brain Arteriovenous Malformations: Single-Center Experience and Technical Nuances. World Neurosurg. 2018, 116, e340–e353. [Google Scholar] [CrossRef]
- Chen, C.-J.; Ding, D.; Lee, C.-C.; Kearns, K.N.; Pomeraniec, I.J.; Cifarelli, C.P.; Arsanious, D.E.; Liscak, R.; Hanuska, J.; Williams, B.J.; et al. Embolization of Brain Arteriovenous Malformations With Versus Without Onyx Before Stereotactic Radiosurgery. Neurosurgery 2021, 88, 366–374. [Google Scholar] [CrossRef]
- Khalil, A.; Fartoukh, M.; Bazot, M.; Parrot, A.; Marsault, C.; Carette, M.-F. Systemic Arterial Embolization in Patients With Hemoptysis: Initial Experience With Ethylene Vinyl Alcohol Copolymer in 15 Cases. Am. J. Roentgenol. 2010, 194, W104–W110. [Google Scholar] [CrossRef] [PubMed]
- Mattay, R.R.; Shlansky-Goldberg, R.; Pukenas, B.A. Recurrent Massive Hemoptysis in a Patient with Cystic Fibrosis: Balloon Assisted Onyx Embolization after Bronchial Artery Coil Recanalization. CVIR Endovasc. 2021, 4, 4. [Google Scholar] [CrossRef]
- Loh, Y.; Duckwiler, G.R. A Prospective, Multicenter, Randomized Trial of the Onyx Liquid Embolic System and N-Butyl Cyanoacrylate Embolization of Cerebral Arteriovenous Malformations. J. Neurosurg. 2010, 113, 733–741. [Google Scholar] [CrossRef]
- Natarajan, S.K.; Born, D.; Ghodke, B.; Britz, G.W.; Sekhar, L.N. Histopathological Changes in Brain Arteriovenous Malformations after Embolization Using Onyx or N-Butyl Cyanoacrylate. J. Neurosurg. 2009, 111, 105–113. [Google Scholar] [CrossRef]
- Leyon, J.J.; Chavda, S.; Thomas, A.; Lamin, S. Preliminary Experience with the Liquid Embolic Material Agent PHIL (Precipitating Hydrophobic Injectable Liquid) in Treating Cranial and Spinal Dural Arteriovenous Fistulas: Technical Note. J. Neurointerv. Surg. 2016, 8, 596–602. [Google Scholar] [CrossRef]
- Prashar, A.; Butt, S.; Shaida, N. Introducing PHIL (Precipitating Hydrophobic Injectable Liquid)—A New Embolic Agent for the Body Interventional Radiologist. Diagn. Interv. Radiol. 2020, 26, 140–142. [Google Scholar] [CrossRef]
- Vollherbst, D.F.; Otto, R.; Do, T.; Kauczor, H.U.; Bendszus, M.; Sommer, C.M.; Möhlenbruch, M.A. Imaging Artifacts of Onyx and PHIL on Conventional CT, Cone-Beam CT and MRI in an Animal Model. Interv. Neuroradiol. 2018, 24, 693–701. [Google Scholar] [CrossRef]
- Helmy, A.; Shaida, N. Treatment of Type II Endoleaks with a Novel Agent: Precipitating Hydrophobic Injectable Liquid (PHIL). Cardiovasc. Intervent. Radiol. 2017, 40, 1094–1098. [Google Scholar] [CrossRef]
- Cheung, E.Y.H.; Ng, R.Y.T.; Yu, S.C.H.; Zhuang, J.T.F.; Wong, G.K.C. PHIL and Squid Embolization of Cerebral Arteriovenous Malformation: A Retrospective Case Series of 23 Patients. Neurointervention 2022, 17, 174–182. [Google Scholar] [CrossRef] [PubMed]
- Varadharajan, S.; Ramalingaiah, A.H.; Saini, J.; Gupta, A.K.; Devi, B.I.; Acharya, U.V. Precipitating Hydrophobic Injectable Liquid Embolization of Intracranial Vascular Shunts: Initial Experience and Technical Note. J. Neurosurg. 2018, 129, 1217–1222. [Google Scholar] [CrossRef] [PubMed]
- Kurda, D.; Guduguntla, G.; Maingard, J.; Kok, H.K.; Lalloo, S. Precipitating Hydrophobic Injectable Liquid (PHIL) Embolic for the Treatment of a Uterine Arteriovenous Malformation: A Technical Report. CVIR Endovasc. 2019, 2, 17. [Google Scholar] [CrossRef] [PubMed]
- Lacis, A.; Kupcs, K.; Savlovskis, J.; Kidikas, H. Parotid Gland Arteriovenous Malformation Embolisation: A Novel Approach to the Use of Precipitating Hydrophobic Injectable Liquid (PHIL). J. Phlebol. Lymphol. 2021, 14, 1–3. [Google Scholar] [CrossRef]
- Lucatelli, P.; Corona, M.; Teodoli, L.; Nardis, P.; Cannavale, A.; Rocco, B.; Trobiani, C.; Cipollari, S.; Zilahi de Gyurgyokai, S.; Bezzi, M.; et al. Use of Phil Embolic Agent for Bleeding in Non-Neurological Interventions. J. Clin. Med. 2021, 10, 701. [Google Scholar] [CrossRef]
- Dudeck, O.; Jordan, O.; Hoffmann, K.T.; Tesmer, K.; Kreuzer-Nagy, T.; Podrabsky, P.; Heise, M.; Meyer, R.; Okuducu, A.F.; Bruhn, H.; et al. Intrisically radiopaque iodine-containing polyvinyl alcohol as a liquid embolic agent: Evaluation in experimental wide-necked aneurysms. J. Neurosurg. 2006, 104, 290–297. [Google Scholar] [CrossRef]
- Dudeck, O.; Jordan, O.; Hoffman, K.T.; Okuducu, A.F.; Husmann, I.; Kreuzer-Nagy, T.; Tesmer, K.; Podrabsky, P.; Bruhn, H.; Hilborn, J.; et al. Embolization of experimental wide-necked aneurysms with iodine-containing polyvinyl alcohol solubilized in a low-angiotoxicity solvent. AJNR Am. J. Neuroradiol. 2006, 27, 1849–1855. [Google Scholar]
- Kulcsar, Z.; Karol, A.; Kronen, P.W.; Svende, P.; Klein, K.; Jordan, O.; Wanke, I. A novel, non-adhesive, precipitating liquid embolic implant with instrinsic radiopacity: Feasibility and safety animal study. Eur. Radiol. 2017, 27, 1248–1256. [Google Scholar] [CrossRef]
- Sapoval, M.; Vidal, V.; Dean, C.; Del Guidice, C.; Tradi, F.; Chevallier, O.; Charles-Nelson, A.; Pellerin, O.; Loffroy, R. Safety and efficacy of peripheral embolization with EASYX liquid embolic agent: A multicenter prospective study. J. Vasc. Interv. Radiol. 2021, 32, 1136–1143. [Google Scholar] [CrossRef] [PubMed]
- Becker, T.A.; Kipke, D.R.; Brandon, T. Calcium alginate gel: A biocompatible and mechanically stable polymer for endovascular embolization. J. Biomed. Mater. Res. 2001, 54, 76086. [Google Scholar] [CrossRef]
- Becker, T.A.; Kipke, D.R. Flow properties of liquid calcium alginate polymer injected through medical catheters for endovascular embolization. J. Biomed. Mater. Res. 2002, 61, 533–540. [Google Scholar] [CrossRef] [PubMed]
- Becker, T.A.; Kipke, D.R.; Preul, M.C.; Bichard, W.D.; McDougall, C.G. In vivo assessments of calcium alginate gel for endovascular embolization of a cerebral arteriovenous malformation model using the swine rete mirabile. Neurosurgery 2002, 51, 453–458, discussion 458–459. [Google Scholar] [CrossRef] [PubMed]


| Embolizing Agent | Trade Names | Ref(s). |
|---|---|---|
| N-butyl-2-cyanoacrylate (NBCA) | Histoacryl Avacryl Tru-Fill n-BCA | [2,3,4,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52] |
| Fibrin Glue | Tisseel Hemaseel | [3,4,53,54,55,56,57,58,59,60,61,62,63,64] |
| N-isopropylacrylamide (NIPAAm) Copolymers | [4,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80] | |
| Poly(ethylene glycol)/Poly(propylene glycol)/Penta erythritol tetrakis (3-mercaptopropionate) (PPODA/PEGDA/QT) | [81,82,83,84,85,86,87] | |
| Shear-Thinning Biomaterials | [88,89] | |
| Silk Elastin Protein (SELP) | [90,91,92] | |
| Poly(Ethylene Glycol) Hydrogel Embolization System (HES) | Instylla Embrace | [92,93,94,95,96] |
| Eudragit | [97,98,99,100] | |
| Calcium Alginate | [101,102,103,104,105,106] | |
| Ethylene vinyl alcohol copolymers | Squid and Squid Peri | [107,108,109,110,111,112,113,114,115,116,117] |
| Onyx | [118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146,147,148,149,150,151,152,153,154,155,156,157,158] | |
| Poly(lactide-co-glycolide) and poly(hydroxyethyl methacrylate) | PHIL | [159,160,161,162,163,164,165,166,167] |
| Iodinated polyvinyl alcohol | EASYX | [168,169,170,171] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pal, A.; Blanzy, J.; Gómez, K.J.R.; Preul, M.C.; Vernon, B.L. Liquid Embolic Agents for Endovascular Embolization: A Review. Gels 2023, 9, 378. https://doi.org/10.3390/gels9050378
Pal A, Blanzy J, Gómez KJR, Preul MC, Vernon BL. Liquid Embolic Agents for Endovascular Embolization: A Review. Gels. 2023; 9(5):378. https://doi.org/10.3390/gels9050378
Chicago/Turabian StylePal, Amrita, Jeffrey Blanzy, Karime Jocelyn Rosas Gómez, Mark C. Preul, and Brent L. Vernon. 2023. "Liquid Embolic Agents for Endovascular Embolization: A Review" Gels 9, no. 5: 378. https://doi.org/10.3390/gels9050378