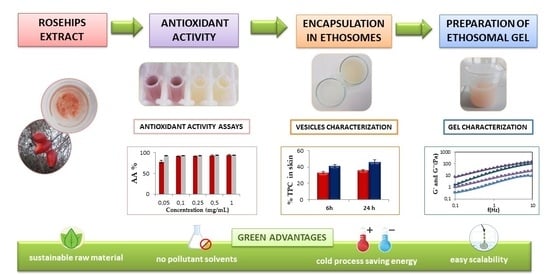
Design and Characterization of an Ethosomal Gel Encapsulating Rosehip Extract
Abstract
:1. Introduction
2. Results and Discussion
2.1. In Vitro Evaluation of Rosehip Extract Anti-Aging Properties
2.2. Preparation and Characterization of Ethosomes: Selection of Raw Materials, Influence of Ethanol, and Preparation Technique
2.3. Vesicles’ Physical Stability
2.4. In Vitro Release Studies
2.5. In Vitro Permeation Studies Using an Artificial Biomimetic Barrier
2.6. In Vitro Skin Permeation/Retention Studies Using Pig Ear Skin
2.7. In Vitro Cytotoxicity Assay
2.8. Development of Rosehip Ethosomal Gel
2.8.1. Physicochemical Characterization of Rosehip Ethosomal Gels
2.8.2. Rheological Properties of Ethosomal Gels
2.9. In Vitro Release from Gels
2.10. Stability Studies of Gels
3. Conclusions
4. Materials and Methods
4.1. Materials
4.2. In Vitro Evaluation of Rosehip Extract Anti-Aging Properties
4.2.1. Antioxidant Activity of Rosehip Extract according to DPPH Method
4.2.2. Antioxidant Activity of Rosehip Extract according to Reactive Oxygen Species (ROS) Production Measurement
4.3. Preparation of Ethosomes: Selection of Raw Materials, Influence of Ethanol, and Preparation Technique
4.4. Vesicle Characterization
4.4.1. Size and Zeta Potential Measurements
4.4.2. Entrapment Efficiency
4.4.3. pH Measurement
4.4.4. Physical Stability
4.5. In Vitro Release Studies
4.6. In Vitro Permeation Studies Using an Artificial Biomimetic Barrier
4.7. In Vitro Skin Permeation/Retention Studies Using Pig Ear Skin
4.8. Cell Viability Studies
4.9. Preparation of Ethosomal Gels
4.10. Physicochemical Characterization of Ethosomal Gels
4.10.1. Measurement of pH, Viscosity, and Spreadability
4.10.2. Rheological Measurements
4.11. In Vitro Release Studies from Ethosomal Gels
4.12. Stability Studies of Gels
4.13. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jaciow, M.; Rudawska, E.; Sagan, A.; Tkaczyk, J.; Wolny, R. The Influence of Environmental Awareness on Responsible Energy Consumption—The Case of Households in Poland. Energies 2022, 15, 5339. [Google Scholar] [CrossRef]
- Magano, J.; Au-Yong-Oliveira, M.; Ferreira, B.; Leite, Â. A Cross-Sectional Study on Ethical Buyer Behavior towards Cruelty-Free Cosmetics: What Consequences for Female Leadership Practices? Sustainability 2022, 14, 7786. [Google Scholar] [CrossRef]
- Maciejewski, G.; Lesznik, D. Consumers towards the Goals of Sustainable Development: Attitudes and Typology. Sustainability 2022, 14, 10558. [Google Scholar] [CrossRef]
- Kamalanon, P.; Chen, J.-S.; Le, T.-T.-Y. “Why Do We Buy Green Products?” An Extended Theory of the Planned Behavior Model for Green Product Purchase Behavior. Sustainability 2022, 14, 689. [Google Scholar] [CrossRef]
- Fortunati, S.; Martiniello, L.; Morea, D. The Strategic Role of the Corporate Social Responsibility and Circular Economy in the Cosmetic Industry. Sustainability 2020, 12, 5120. [Google Scholar] [CrossRef]
- Bom, S.; Ribeiro, H.M.; Marto, J. Sustainability Calculator: A Tool to Assess Sustainability in Cosmetic Products. Sustainability 2020, 12, 1437. [Google Scholar] [CrossRef]
- Ferreira, M.; Magalhães, M.; Oliveira, R.; Sousa-Lobo, J.; Almeida, I. Trends in the Use of Botanicals in Anti-Aging Cosmetics. Molecules 2021, 26, 3584. [Google Scholar] [CrossRef]
- Tengli, A.; Srinivasan, S.H. An Exploratory Study to Identify the Gender-Based Purchase Behavior of Consumers of Natural Cosmetics. Cosmetics 2022, 9, 101. [Google Scholar] [CrossRef]
- Mármol, I.; Sánchez-de-Diego, C.; Jiménez-Moreno, N.; Ancín-Azpilicueta, C.; Rodríguez-Yoldi, M. Therapeutic Applications of Rose Hips from Different Rosa Species. Int. J. Mol. Sci. 2017, 18, 1137. [Google Scholar] [CrossRef]
- Demir, N.; Yildiz, O.; Alpaslan, M.; Hayaloglu, A.A. Evaluation of Volatiles, Phenolic Compounds and Antioxidant Activities of Rose Hip (Rosa L.) Fruits in Turkey. LWT-Food Sci. Technol. 2014, 57, 126–133. [Google Scholar] [CrossRef]
- Elmastaş, M.; Demir, A.; Genç, N.; Dölek, Ü.; Güneş, M. Changes in Flavonoid and Phenolic Acid Contents in Some Rosa Species during Ripening. Food Chem. 2017, 235, 154–159. [Google Scholar] [CrossRef]
- Olsson, M.E.; Gustavsson, K.-E.; Andersson, S.; Nilsson, Å.; Duan, R.-D. Inhibition of Cancer Cell Proliferation in Vitro by Fruit and Berry Extracts and Correlations with Antioxidant Levels. J. Agric. Food Chem. 2004, 52, 7264–7271. [Google Scholar] [CrossRef]
- Nađpal, J.D.; Lesjak, M.M.; Šibul, F.S.; Anačkov, G.T.; Četojević-Simin, D.D.; Mimica-Dukić, N.M.; Beara, I.N. Comparative Study of Biological Activities and Phytochemical Composition of Two Rose Hips and Their Preserves: Rosa Canina L. and Rosa Arvensis Huds. Food Chem. 2016, 192, 907–914. [Google Scholar] [CrossRef]
- Winther, K.; Wongsuphasawat, K.; Phetcharat, L. The Effectiveness of a Standardized Rose Hip Powder, Containing Seeds and Shells of Rosa Canina, on Cell Longevity, Skin Wrinkles, Moisture, and Elasticity. CIA 2015, 10, 1849. [Google Scholar] [CrossRef] [PubMed]
- Michalak, M.; Pierzak, M.; Kręcisz, B.; Suliga, E. Bioactive Compounds for Skin Health: A Review. Nutrients 2021, 13, 203. [Google Scholar] [CrossRef] [PubMed]
- Duru, N.; Karadeniz, F.; Erge, H.S. Changes in Bioactive Compounds, Antioxidant Activity and HMF Formation in Rosehip Nectars During Storage. Food Bioprocess Technol. 2012, 5, 2899–2907. [Google Scholar] [CrossRef]
- Angelov, G.; Boyadzhieva, S.; Georgieva, S. Rosehip Extraction: Process Optimization and Antioxidant Capacity of Extracts. Open Chem. 2014, 12, 502–508. [Google Scholar] [CrossRef]
- Ruiz Canizales, J.; Velderrain Rodríguez, G.R.; Domínguez Avila, J.A.; Preciado Saldaña, A.M.; Alvarez Parrilla, E.; Villegas Ochoa, M.A.; González Aguilar, G.A. Encapsulation to Protect Different Bioactives to Be Used as Nutraceuticals and Food Ingredients. In Bioactive Molecules in Food; Mérillon, J.-M., Ramawat, K.G., Eds.; Reference Series in Phytochemistry; Springer International Publishing: Cham, Switzerland, 2019; pp. 2163–2182. ISBN 978-3-319-78029-0. [Google Scholar]
- Grgić, J.; Šelo, G.; Planinić, M.; Tišma, M.; Bucić-Kojić, A. Role of the Encapsulation in Bioavailability of Phenolic Compounds. Antioxidants 2020, 9, 923. [Google Scholar] [CrossRef]
- Andleeb, M.; Shoaib Khan, H.M.; Daniyal, M. Development, Characterization and Stability Evaluation of Topical Gel Loaded with Ethosomes Containing Achillea Millefolium L. Extract. Front. Pharmacol. 2021, 12, 603227. [Google Scholar] [CrossRef]
- Mota, A.H.; Prazeres, I.; Mestre, H.; Bento-Silva, A.; Rodrigues, M.J.; Duarte, N.; Serra, A.T.; Bronze, M.R.; Rijo, P.; Gaspar, M.M.; et al. A Newfangled Collagenase Inhibitor Topical Formulation Based on Ethosomes with Sambucus Nigra L. Extract. Pharmaceuticals 2021, 14, 467. [Google Scholar] [CrossRef]
- Touitou, E.; Dayan, N.; Bergelson, L.; Godin, B.; Eliaz, M. Ethosomes—Novel Vesicular Carriers for Enhanced Delivery: Characterization and Skin Penetration Properties. J. Control. Release 2000, 65, 403–418. [Google Scholar] [CrossRef] [PubMed]
- Arora, D.; Nanda, S. Quality by Design Driven Development of Resveratrol Loaded Ethosomal Hydrogel for Improved Dermatological Benefits via Enhanced Skin Permeation and Retention. Int. J. Pharm. 2019, 567, 118448. [Google Scholar] [CrossRef] [PubMed]
- Bayer, I.S. Hyaluronic Acid and Controlled Release: A Review. Molecules 2020, 25, 2649. [Google Scholar] [CrossRef] [PubMed]
- Bukhari, S.N.A.; Roswandi, N.L.; Waqas, M.; Habib, H.; Hussain, F.; Khan, S.; Sohail, M.; Ramli, N.A.; Thu, H.E.; Hussain, Z. Hyaluronic Acid, a Promising Skin Rejuvenating Biomedicine: A Review of Recent Updates and Pre-Clinical and Clinical Investigations on Cosmetic and Nutricosmetic Effects. Int. J. Biol. Macromol. 2018, 120, 1682–1695. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Liu, L.; Han, J.; Tang, Y. Encapsulating Plant Ingredients for Dermocosmetic Application: An Updated Review of Delivery Systems and Characterization Techniques. Int. J. Cosmet. Sci. 2020, 42, 16–28. [Google Scholar] [CrossRef]
- Bryła, A. Encapsulation of Elderberry Extract into Phospholipid Nanoparticles. J. Food Eng. 2015, 167, 189–195. [Google Scholar] [CrossRef]
- Shukla, R.; Tiwari, G.; Tiwari, R.; Rai, A.K. Formulation and Evaluation of the Topical Ethosomal Gel of Melatonin to Prevent UV Radiation. J. Cosmet. Dermatol. 2020, 19, 2093–2104. [Google Scholar] [CrossRef]
- Khan, P.; Akhtar, N. Phytochemical Investigations and Development of Ethosomal Gel with Brassica Oleraceae L. (Brassicaceae) Extract: An Innovative Nano Approach towards Cosmetic and Pharmaceutical Industry. Ind. Crop. Prod. 2022, 183, 114905. [Google Scholar] [CrossRef]
- Paiva-Santos, A.C.; Silva, A.L.; Guerra, C.; Peixoto, D.; Pereira-Silva, M.; Zeinali, M.; Mascarenhas-Melo, F.; Castro, R.; Veiga, F. Ethosomes as Nanocarriers for the Development of Skin Delivery Formulations. Pharm. Res. 2021, 38, 947–970. [Google Scholar] [CrossRef]
- Malekar, S.A.; Sarode, A.L.; Bach, A.C.; Worthen, D.R. The Localization of Phenolic Compounds in Liposomal Bilayers and Their Effects on Surface Characteristics and Colloidal Stability. AAPS PharmSciTech 2016, 17, 1468–1476. [Google Scholar] [CrossRef]
- Moulaoui, K.; Caddeo, C.; Manca, M.L.; Castangia, I.; Valenti, D.; Escribano, E.; Atmani, D.; Fadda, A.M.; Manconi, M. Identification and Nanoentrapment of Polyphenolic Phytocomplex from Fraxinus Angustifolia: In Vitro and in Vivo Wound Healing Potential. Eur. J. Med. Chem. 2015, 89, 179–188. [Google Scholar] [CrossRef] [PubMed]
- Khan, B.A.; Mahmood, T.; Menaa, F.; Shahzad, Y.; Yousaf, A.M.; Hussain, T.; Ray, S.D. New Perspectives on the Efficacy of Gallic Acid in Cosmetics & Nanocosmeceuticals. Curr. Pharm. Des. 2018, 24, 5181–5187. [Google Scholar] [CrossRef]
- Ramadon, D.; Wirarti, G.A.; Anwar, E. Novel Transdermal Ethosomal Gel Containing Green Tea (Camellia Sinensis L. Kuntze) Leaves Extract: Formulation and In Vitro Penetration Study. JYP 2017, 9, 336–340. [Google Scholar] [CrossRef]
- Lukić, M.; Pantelić, I.; Savić, S.D. Towards Optimal PH of the Skin and Topical Formulations: From the Current State of the Art to Tailored Products. Cosmetics 2021, 8, 69. [Google Scholar] [CrossRef]
- Fathalla, D.; Youssef, E.M.K.; Soliman, G.M. Liposomal and Ethosomal Gels for the Topical Delivery of Anthralin: Preparation, Comparative Evaluation and Clinical Assessment in Psoriatic Patients. Pharmaceutics 2020, 12, 446. [Google Scholar] [CrossRef] [PubMed]
- Iizhar, S.A.; Syed, I.A.; Satar, R.; Ansari, S.A. In Vitro Assessment of Pharmaceutical Potential of Ethosomes Entrapped with Terbinafine Hydrochloride. J. Adv. Res. 2016, 7, 453–461. [Google Scholar] [CrossRef]
- Magnano, G.C.; Sut, S.; Dall’Acqua, S.; Di Cagno, M.P.; Lee, L.; Lee, M.; Larese Filon, F.; Perissutti, B.; Hasa, D.; Voinovich, D. Validation and Testing of a New Artificial Biomimetic Barrier for Estimation of Transdermal Drug Absorption. Int. J. Pharm. 2022, 628, 122266. [Google Scholar] [CrossRef]
- Zou, L.; Liu, W.; Liu, W.; Liang, R.; Li, T.; Liu, C.; Cao, Y.; Niu, J.; Liu, Z. Characterization and Bioavailability of Tea Polyphenol Nanoliposome Prepared by Combining an Ethanol Injection Method with Dynamic High-Pressure Microfluidization. J. Agric. Food Chem. 2014, 62, 934–941. [Google Scholar] [CrossRef]
- Betz, G.; Aeppli, A.; Menshutina, N.; Leuenberger, H. In Vivo Comparison of Various Liposome Formulations for Cosmetic Application☆. Int. J. Pharm. 2005, 296, 44–54. [Google Scholar] [CrossRef]
- Souto, E.B.; Müller, R.H. Cosmetic Features and Applications of Lipid Nanoparticles (SLN®, NLC®). Int. J. Cosmet. Sci. 2008, 30, 157–165. [Google Scholar] [CrossRef]
- Salvioni, L.; Morelli, L.; Ochoa, E.; Labra, M.; Fiandra, L.; Palugan, L.; Prosperi, D.; Colombo, M. The Emerging Role of Nanotechnology in Skincare. Adv. Colloid Interface Sci. 2021, 293, 102437. [Google Scholar] [CrossRef] [PubMed]
- Juncan, A.M.; Moisă, D.G.; Santini, A.; Morgovan, C.; Rus, L.-L.; Vonica-Țincu, A.L.; Loghin, F. Advantages of Hyaluronic Acid and Its Combination with Other Bioactive Ingredients in Cosmeceuticals. Molecules 2021, 26, 4429. [Google Scholar] [CrossRef]
- Elena, O.B.; Maria, N.A.; Michael, S.Z.; Natalia, B.D.; Alexander, I.B.; Ivan, I.K. Dermatologic Gels Spreadability Measuring Methods Comparative Study. Int. J. App. Pharm. 2022, 14, 164–168. [Google Scholar] [CrossRef]
- Xie, J.; Ji, Y.; Xue, W.; Ma, D.; Hu, Y. Hyaluronic Acid-Containing Ethosomes as a Potential Carrier for Transdermal Drug Delivery. Colloids Surf. B Biointerfaces 2018, 172, 323–329. [Google Scholar] [CrossRef]
- Graça, A.; Gonçalves, L.; Raposo, S.; Ribeiro, H.; Marto, J. Useful In Vitro Techniques to Evaluate the Mucoadhesive Properties of Hyaluronic Acid-Based Ocular Delivery Systems. Pharmaceutics 2018, 10, 110. [Google Scholar] [CrossRef] [PubMed]
- Leite, F.D.G.; Oshiro Júnior, J.A.; Chiavacci, L.A.; Chiari-Andréo, B.G. Assessment of an Anti-Ageing Structured Cosmetic Formulation Containing Goji Berry. Braz. J. Pharm. Sci. 2019, 55, e17412. [Google Scholar] [CrossRef]
- Sallustio, V.; Chiocchio, I.; Mandrone, M.; Cirrincione, M.; Protti, M.; Farruggia, G.; Abruzzo, A.; Luppi, B.; Bigucci, F.; Mercolini, L.; et al. Extraction, Encapsulation into Lipid Vesicular Systems, and Biological Activity of Rosa Canina L. Bioactive Compounds for Dermocosmetic Use. Molecules 2022, 27, 3025. [Google Scholar] [CrossRef]
- Brand-Williams, W.; Cuvelier, M.E.; Berset, C. Use of a Free Radical Method to Evaluate Antioxidant Activity. LWT-Food Sci. Technol. 1995, 28, 25–30. [Google Scholar] [CrossRef]
- Marto, J.; Ascenso, A.; Gonçalves, L.M.; Gouveia, L.F.; Manteigas, P.; Pinto, P.; Oliveira, E.; Almeida, A.J.; Ribeiro, H.M. Melatonin-Based Pickering Emulsion for Skin’s Photoprotection. Drug Deliv. 2016, 23, 1594–1607. [Google Scholar] [CrossRef] [PubMed]
- Ma, H.; Guo, D.; Fan, Y.; Wang, J.; Cheng, J.; Zhang, X. Paeonol-Loaded Ethosomes as Transdermal Delivery Carriers: Design, Preparation and Evaluation. Molecules 2018, 23, 1756. [Google Scholar] [CrossRef]
- Tzanova, M.M.; Randelov, E.; Stein, P.C.; Hiorth, M.; di Cagno, M.P. Towards a Better Mechanistic Comprehension of Drug Permeation and Absorption: Introducing the Diffusion-Partitioning Interplay. Int. J. Pharm. 2021, 608, 121116. [Google Scholar] [CrossRef] [PubMed]
- Di Cagno, M.; Bibi, H.A.; Bauer-Brandl, A. New Biomimetic Barrier PermeapadTM for Efficient Investigation of Passive Permeability of Drugs. Eur. J. Pharm. Sci. 2015, 73, 29–34. [Google Scholar] [CrossRef] [PubMed]
- Makuch, E.; Nowak, A.; Günther, A.; Pełech, R.; Kucharski, Ł.; Duchnik, W.; Klimowicz, A. The Effect of Cream and Gel Vehicles on the Percutaneous Absorption and Skin Retention of a New Eugenol Derivative With Antioxidant Activity. Front. Pharmacol. 2021, 12, 658381. [Google Scholar] [CrossRef] [PubMed]
- Calonghi, N.; Farruggia, G.; Boga, C.; Micheletti, G.; Fini, E.; Romani, L.; Telese, D.; Faraci, E.; Bergamini, C.; Cerini, S.; et al. Root Extracts of Two Cultivars of Paeonia Species: Lipid Composition and Biological Effects on Different Cell Lines: Preliminary Results. Molecules 2021, 26, 655. [Google Scholar] [CrossRef]










| Samples * | Size (nm) | PDI | ζ (mV) | EE% | pH |
|---|---|---|---|---|---|
| ET1 | 312.4 ± 8.5 | 0.30 ± 0.02 | −52.12 ± 1.33 | - | 6.41 ± 0.10 |
| ET2 | 223.8 ± 5.4 | 0.25 ± 0.02 | −53.40 ± 1.70 | - | 6.30 ± 0.01 |
| ET3 | 178.8 ± 1.5 | 0.25 ± 0.01 | −53.12 ± 1.26 | - | 6.22 ± 0.04 |
| ET4 | 213.6 ±3.4 | 0.25 ± 0.01 | −54.13 ± 0.87 | - | 6.15 ± 0.05 |
| ET1R | 363.6 ± 7.3 | 0.35 ± 0.03 | −49.57 ± 1.48 | 68.78 ± 5.08 | 5.44 ± 0.08 |
| ET2R | 288.1 ± 8.6 | 0.30 ± 0.10 | −51.42 ± 0.95 | 89.42 ± 2.21 | 5.47 ± 0.09 |
| ET3R | 225.4 ± 7.0 | 0.26 ± 0.02 | −52.99 ± 1.40 | 93.41 ± 5.30 | 5.53 ± 0.05 |
| ET4R | 240.9 ± 1.9 | 0.29 ± 0.05 | −53.19 ± 1.08 | 87.10 ± 3.94 | 5.61 ± 0.06 |
| Sample | Viscosity (cP) * | pH * | Spreadability (mm2) * | Size (nm) * |
|---|---|---|---|---|
| HA1% | 305.0 ± 7.0 | 6.3 ± 0.1 | 4435.58 ± 90.28 | |
| R HA1% | 250.0 ± 1.0 | 5.6 ± 0.2 | 5025.57 ± 218.91 | - |
| ET3 HA1% | 403.3 ± 11.5 | 6.1 ± 0.1 | 3995.13 ± 128.71 | 281.5 ± 2.1 |
| ET3R HA1% | 397.5 ± 17.1 | 5.6 ± 0.2 | 3998.79 ± 319.52 | 363.5 ± 1.8 |
| HA 2% | 3233.3 ± 55.5 | 6.8 ± 0.2 | 2404.72 ± 133.28 | - |
| R HA2% | 3166.7 ± 57.7 | 5.6 ± 0.2 | 2178.11 ± 96.08 | - |
| ET3 HA2% | 3233.3 ± 57.7 | 7.0 ± 0.2 | 1556.20 ± 126.94 | 219.4 ± 10.4 |
| ET3R HA2% | 3233.3 ± 57.5 | 5.5 ± 0.2 | 1566.33 ± 40.34 | 289.7 ± 6.4 |
| Formulation | Peak Normal Force–Normal Force (N) * | Area Under Force–Time Curve (N·s) * |
|---|---|---|
| HA1% | −0.244 ± 0.020 | 0.514 ± 0.047 |
| R HA1% | −0.257 ± 0.012 | 0.502 ± 0.049 |
| ET3 HA1% | −0.399 ± 0.026 | 0.721 ± 0.056 |
| ET3R HA1% | −0.329 ± 0.015 | 0.743 ± 0.093 |
| HA 2% | −1.031 ± 0.039 | 1.294 ± 0.129 |
| R HA2% | −1.039 ± 0.021 | 1.161 ± 0.143 |
| ET HA2% | −1.436 ± 0.056 | 1.567 ± 0.192 |
| ET3R HA2% | −1.333 ± 0.036 | 1.385 ± 0.043 |
| Gel Formulation * | Temperature (°C) | Time (Day) | Viscosity (cP) | pH | Vesicle Size (nm) |
|---|---|---|---|---|---|
| ET3 HA1% | 4 ± 2 °C | 1 | 403.3 ± 11.5 | 6.1 ± 0.1 | 281.5 ± 2.1 |
| 7 | 405.5 ± 21.2 | 6.1 ± 0.1 | 259.5 ± 12.0 | ||
| 15 | 415.0 ± 7.1 | 6.0 ± 0.1 | 284.5 ± 1.1 | ||
| 30 | 426.7 ± 20.8 | 6.0 ± 0.1 | 304.0 ± 8.1 | ||
| 60 | 415.0 ± 21.2 | 5.9 ± 0.1 | 283.4 ± 5.8 | ||
| ET3 HA1% | 25 ± 2 °C | 1 | 403.3 ± 11.5 | 6.1 ± 0.1 | 281.5± 8.1 |
| 7 | 350.5 ± 10.2 | 6.1 ± 0.1 | 276.0 ± 18.4 | ||
| 15 | 375.1 ± 21.2 | 6.1 ± 0.1 | 282.2 ± 12.5 | ||
| 30 | 410.5 ± 14.4 | 5.9 ± 0.1 | 363.7 ± 18.6 | ||
| 60 | 420.0 ± 56.6 | 5.9 ± 0.1 | 355.2 ± 8.5 | ||
| ET3R HA1% | 4 ± 2 °C | 1 | 397.5 ± 17.1 | 5.6 ± 0.2 | 363.5 ± 1.8 |
| 7 | 440.3 ± 14.1 | 5.4 ± 0.2 | 352.5 ± 19.2 | ||
| 15 | 445.5 ± 7.1 | 5.4 ± 0.2 | 371.0 ± 19.8 | ||
| 30 | 435.0 ± 21.2 | 5.7 ± 0.2 | 405.9 ± 17.8 | ||
| 60 | 440.0 ± 28.3 | 5.5 ± 0.2 | 382.7 ± 9.8 | ||
| ET3R HA1% | 25 ± 2 °C | 1 | 397.5 ± 17.1 | 5.6 ± 0.2 | 363.5 ± 1.8 |
| 7 | 375.5 ± 7.1 | 5.4 ± 0.2 | 380.5 ± 10.6 | ||
| 15 | 410.0 ± 28.3 | 5.2 ± 0.2 | 391.0 ± 46.7 | ||
| 30 | 425.0 ± 21.2 | 5.4 ± 0.2 | 418.1 ± 7.7 | ||
| 60 | 400.0 ± 28.3 | 5.4 ± 0.2 | 457.4 ± 8.9 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sallustio, V.; Farruggia, G.; di Cagno, M.P.; Tzanova, M.M.; Marto, J.; Ribeiro, H.; Goncalves, L.M.; Mandrone, M.; Chiocchio, I.; Cerchiara, T.; et al. Design and Characterization of an Ethosomal Gel Encapsulating Rosehip Extract. Gels 2023, 9, 362. https://doi.org/10.3390/gels9050362
Sallustio V, Farruggia G, di Cagno MP, Tzanova MM, Marto J, Ribeiro H, Goncalves LM, Mandrone M, Chiocchio I, Cerchiara T, et al. Design and Characterization of an Ethosomal Gel Encapsulating Rosehip Extract. Gels. 2023; 9(5):362. https://doi.org/10.3390/gels9050362
Chicago/Turabian StyleSallustio, Valentina, Giovanna Farruggia, Massimiliano Pio di Cagno, Martina M. Tzanova, Joana Marto, Helena Ribeiro, Lidia Maria Goncalves, Manuela Mandrone, Ilaria Chiocchio, Teresa Cerchiara, and et al. 2023. "Design and Characterization of an Ethosomal Gel Encapsulating Rosehip Extract" Gels 9, no. 5: 362. https://doi.org/10.3390/gels9050362