Colchicine in Cardiac Surgery: The COCS Randomized Clinical Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Inclusion Criteria
2.3. Exclusion Criteria
2.4. Randomization
2.5. Sample Size Calculation
2.6. Statistical Analyses
2.7. Endpoints: Primary Outcome Measure
2.8. Endpoints: Secondary Outcome Measure
2.9. Surgery
2.10. Monitoring
3. Results
4. Discussion
Limitations of the Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gudbjartsson, T.; Helgadottir, S.; Sigurdsson, M.I.; Taha, A.; Jeppsson, A.; Christensen, T.D.; Rieber, L.P.S. New-onset postoperative atrial fibrillation after heart surgery. Acta Anaesthesiol. Scand. 2020, 64, 145–155. [Google Scholar] [CrossRef] [PubMed]
- Ronzoni, R.M.; Souza, A.Z.M.; Leiria, T.L.L.; Lima, G.G. Update on management of postoperative atrial fibrillation after cardiac surgery. Braz. J. Cardiovasc. Surg. 2020, 35, 206–210. [Google Scholar]
- Eikelboom, R.; Sanjanwala, R.; Le, M.L.; Yamashita, M.H.; Arora, R.C. Postoperative atrial fibrillation after cardiac surgery: A systematic review and meta-analysis. Ann. Thorac. Surg. 2021, 111, 544–554. [Google Scholar] [CrossRef] [PubMed]
- Dobrev, D.; Aguilar, M.; Heijman, J.; Guichard, J.B.; Nattel, S. Postoperative atrial fibrillation: Mechanisms, manifestations and management. Nat. Rev. Cardiol. 2019, 16, 417–436. [Google Scholar] [CrossRef]
- Patel, P.; Dokainish, H.; Tsai, P.; Lakkis, N. Update on the association of inflammation and atrial fibrillation. J. Cardiovasc. Electrophysiol. 2010, 21, 1064–1070. [Google Scholar] [CrossRef]
- Hu, Y.F.; Chen, Y.J.; Lin, Y.J.; Chen, S.A. Inflammation and the pathogenesis of atrial fibrillation. Nat. Rev. Cardiol. 2015, 12, 230–243. [Google Scholar] [CrossRef]
- Sagris, M.; Vardas, E.P.; Theofilis, P.; Antonopoulos, A.S.; Oikonomou, E.; Tousoulis, D. Atrial fibrillation: Pathogenesis, predisposing factors, and genetics. Int. J. Mol. Sci. 2021, 23, 6. [Google Scholar] [CrossRef]
- Santangeli, P.; Marchlinski, F.E. Techniques for the provocation, localization, and ablation of non-pulmonary vein triggers for atrial fibrillation. Heart Rhythm 2017, 14, 1087–1096. [Google Scholar] [CrossRef] [Green Version]
- Yao, Y.; Yang, M.; Liu, D.; Zhao, Q. Immune remodeling and atrial fibrillation. Front. Physiol. 2022, 13, 927221. [Google Scholar] [CrossRef]
- Heijman, J.; Linz, D.; Schotten, U. Dynamics of atrial fibrillation mechanisms and comorbidities. Annu. Rev. Physiol. 2021, 83, 83–106. [Google Scholar] [CrossRef]
- Nattel, S. Molecular and cellular mechanisms of atrial fibrosis in atrial fibrillation. JACC Clin. Electrophysiol. 2017, 3, 425–435. [Google Scholar] [CrossRef] [PubMed]
- Kottkamp, H.; Schreiber, D.; Moser, F.; Rieger, A. Therapeutic approaches to atrial fibrillation ablation targeting atrial fibrosis. JACC Clin. Electrophysiol. 2017, 3, 643–653. [Google Scholar] [CrossRef] [PubMed]
- Schotten, U.; Verheule, S.; Kirchhof, P.; Goette, A. Pathophysiological mechanisms of atrial fibrillation: A translational appraisal. Physiol. Rev. 2011, 91, 265–325. [Google Scholar] [CrossRef]
- Sohns, C.; Marrouche, N.F. Atrial fibrillation and cardiac fibrosis. Eur. Heart J. 2020, 41, 1123–1131. [Google Scholar] [CrossRef] [PubMed]
- Yue, H.; Liang, W.; Zhan, Y.; Zhang, Z.; Qin, X.; Bian, L.; He, K.; Wu, Z. Colchicine: Emerging therapeutic effects on atrial fibrillation by alleviating myocardial fibrosis in a rat model. Biomed. Pharmacother. 2022, 154, 113573. [Google Scholar] [CrossRef]
- Shen, M.J.; Choi, E.K.; Tan, A.Y.; Han, S.; Shinohara, T.; Maruyama, M.; Chen, L.S.; Shen, C.; Hwang, C.; Lin, S.F.; et al. Patterns of baseline autonomic nerve activity and the development of pacing-induced sustained atrial fibrillation. Heart Rhythm 2011, 8, 583–589. [Google Scholar] [CrossRef] [Green Version]
- Wijesurendra, R.S.; Casadei, B. Mechanisms of atrial fibrillation. Heart 2019, 105, 1860–1867. [Google Scholar] [CrossRef]
- Kusayama, T.; Wan, J.; Yuan, Y.; Chen, P.S. Neural mechanisms and therapeutic opportunities for atrial fibrillation. Methodist DeBakey Cardiovasc. J. 2021, 17, 43–47. [Google Scholar] [CrossRef]
- Dvirnik, N.; Belley-Cote, E.P.; Hanif, H.; Devereaux, P.J.; Lamy, A.; Dieleman, J.M.; Vincent, J.; Whitlock, R.P. Steroids in cardiac surgery: A systematic review and meta-analysis. Br. J. Anaesth. 2018, 120, 657–667. [Google Scholar] [CrossRef] [Green Version]
- Rezaei, Y.; Gholami-Fesharaki, M.; Dehghani, M.R.; Arya, A.; Haghjoo, M.; Arjmand, N. Statin antiarrhythmic effect on atrial fibrillation in statin-naive patients undergoing cardiac surgery: A meta-analysis of randomized controlled trials. J. Cardiovasc. Pharmacol. Therapeut. 2016, 21, 167–176. [Google Scholar] [CrossRef]
- Imazio, M.; Brucato, A.; Ferrazzi, P.; Rovere, M.E.; Gandino, A.; Cemin, R.; Ferrua, S.; Belli, R.; Maestroni, S.; Simon, C.; et al. Colchicine reduces postoperative atrial fibrillation: Results of the Colchicine for the Prevention of the Postpericardiotomy Syndrome (COPPS) atrial fibrillation substudy. Circulation 2011, 124, 2290–2295. [Google Scholar] [CrossRef]
- Imazio, M.; Brucato, A.; Ferrazzi, P.; Pullara, A.; Adler, Y.; Barosi, A.; Caforio, A.L.; Cemin, R.; Chirillo, F.; Comoglio, C.; et al. Colchicine for prevention of postpericardiotomy syndrome and postoperative atrial fibrillation: The COPPS-2 randomized clinical trial. JAMA 2014, 312, 1016–1023. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sarzaeem, M.; Shayan, N.; Bagheri, J.; Jebelli, M.; Mandegar, M. Low dose Colchicine in prevention of atrial fibrillation after coronary artery bypass graft: A double-blind clinical trial. Tehran Univ. Med. J. 2014, 72, 147–154. [Google Scholar]
- Zarpelon, C.S.; Netto, M.C.; Jorge, J.C.; Fabris, C.C.; Desengrini, D.; Jardim, M.D.; Silva, D.G. Colchicine to reduce atrial fibrillation in the post-operative period of myocardial revascularization. Arq. Bras. Cardiol. 2016, 107, 4–9. [Google Scholar] [PubMed]
- Tabbalat, R.A.; Hamad, N.M.; Alhaddad, I.A.; Hammoudeh, A.; Akasheh, B.F.; Khader, Y. Effect of colchicine on the incidence of atrial fibrillation in open heart surgery patients: END-AF trial. Am. Heart J. 2016, 178, 102–107. [Google Scholar] [CrossRef] [PubMed]
- Mashayekhi, N.R.; Alisaeedi, A.; Rostami, A.; Soltani, P. The impact of colchicine in preventing postpericardiotomy syndrome; a double-blind clinical trial study. Immunopathol. Persa 2020, 6, e11. [Google Scholar] [CrossRef]
- Tabbalat, R.A.; Alhaddad, I.; Hammoudeh, A.; Khader, Y.S.; Khalaf, H.A.; Obaidat, M.; Barakat, J. Effect of low-dose colchicine on the incidence of atrial fibrillation in open heart surgery patients: END-AF low dose trial. J. Int. Med. Res. 2020, 48, 300060520939832. [Google Scholar] [CrossRef]
- Lennerz, C.; Barman, M.; Tantawy, M.; Sopher, M.; Whittaker, P. Colchicine for primary prevention of atrial fibrillation after open-heart surgery: Systematic review and meta-analysis. Int. J. Cardiol. 2017, 249, 127–137. [Google Scholar] [CrossRef]
- Rezaei, Y.; Peighambari, M.M.; Naghshbandi, S.; Samiei, N.; Ghavidel, A.A.; Dehghani, M.R.; Haghjoo, M.; Hosseini, S. Postoperative atrial fibrillation following cardiac surgery: From pathogenesis to potential therapies. Am. J. Cardiovasc. Drugs 2020, 20, 19–49. [Google Scholar] [CrossRef]
- January, C.T.; Wann, L.S.; Alpert, J.S.; Calkins, H.; Cigarroa, J.E.; Cleveland, J.C., Jr.; Conti, J.B.; Ellinor, P.T.; Ezekowitz, M.D.; Field, M.E.; et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: Executive summary: A report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation 2014, 130, 2071–2104. [Google Scholar] [CrossRef] [Green Version]
- Hindricks, G.; Potpara, T.; Dagres, N.; Arbelo, E.; Bax, J.J.; Blomström-Lundqvist, C.; Boriani, G.; Castella, M.; Dan, G.A.; Dilaveris, P.E.; et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur. Heart J. 2021, 42, 373–498. [Google Scholar] [PubMed]
- January, C.T.; Wann, L.S.; Calkins, H.; Chen, L.Y.; Cigarroa, J.E.; Cleveland, J.C., Jr.; Ellinor, P.T.; Ezekowitz, M.D.; Field, M.E.; Furie, K.L.; et al. 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society in Collaboration With the Society of Thoracic Surgeons. Circulation 2019, 140, e125–e151. [Google Scholar] [PubMed]
- Shvartz, V.; Le, T.; Kryukov, Y.; Sokolskaya, M.; Ispiryan, A.; Khugaeva, E.; Yurkulieva, G.; Shvartz, E.; Petrosyan, A.; Bockeria, L.; et al. Colchicine for Prevention of Atrial Fibrillation after Cardiac Surgery in the Early Postoperative Period. J. Clin. Med. 2022, 11, 1387. [Google Scholar] [CrossRef] [PubMed]
- Lehr, R. Sixteen S-squared over D-squared: A relation for crude sample size estimates. Stat. Med. 1992, 11, 1099–1102. [Google Scholar] [CrossRef]


| Parameters | Colchicine (n = 113) | Placebo (n = 127) | p |
|---|---|---|---|
| Clinical parameters of patients | |||
| Age, y | 62 (55; 67) | 61 (56; 67) | 0.851 |
| Male, n (%) | 83 (73.5) | 97 (76.4) | 0.601 |
| BSA, m2 | 2.01 (1.9; 2.18) | 2.02 (1.89; 2.13) | 0.806 |
| Weight, kg | 84 (74; 94) | 85 (76; 94) | 0.493 |
| BMI, kg/m2 | 29 (26; 31.9) | 29 (26; 32.3) | 0.638 |
| Angina pectoris, n (%) | 103 (91) | 112 (88) | 0.454 |
| Angina pectoris–classes III–IV, n (%) | 59 (52) | 67 (53) | 0.837 |
| Diabetes, n (%) | 28 (24.7) | 24 (19) | 0.270 |
| COPD, n (%) | 7 (6.2) | 7 (5.5) | 0.822 |
| Hypertension, n (%) | 100 (88.5) | 119 (93.7) | 0.155 |
| Previous AMI, n (%) | 46 (40.7) | 51 (40) | 0.931 |
| Stroke, n (%) | 2 (1.7) | 2 (1.6) | 0.906 |
| Smoking, n (%) | 25 (22.1) | 41 (32.3) | 0.079 |
| Echocardiographic parameters | |||
| LVEF, % | 60 (56; 64) | 60 (56; 64) | 0.507 |
| iESD | 16.5 (15.3; 18.1) | 16.5 (15; 18) | 0.644 |
| iEDD | 24.8 (22.8; 26.5) | 24 (22.7; 26.2) | 0.674 |
| iESV | 22.6 (18.7; 26.7) | 21.5 (18.4; 26.1) | 0.423 |
| iEDV | 56.3 (48.6; 66.7) | 55.8 (46.8; 64.4) | 0.562 |
| MR, degree | 1.5 (1; 1.5) | 1.5 (1; 1.5) | 0.492 |
| AR, degree | 1 (0; 1) | 0 (0; 1) | 0.577 |
| IVS, mm | 13 (12; 15) | 13 (12; 15) | 0.811 |
| LA size, cm | 4 (3.8; 4.4) | 4 (3.7; 4.4) | 0.964 |
| iLA size, cm | 2 (1.9; 2.17) | 2 (1.8; 2.22) | 0.782 |
| Laboratory test results | |||
| WBC, 10×9/L | 7.5 (6.4; 8.9) | 7.6 (6.6; 9.1) | 0.514 |
| Neutrophils, 10×9/L | 4.4 (3.4; 5.4) | 4.7 (3.7; 5.3) | 0.619 |
| Neutrophils, % | 58 (53; 65) | 58.9 (53.2; 63) | 0.677 |
| Platelets,10×9/L | 236 (197; 279) | 258 (213; 298) | 0.197 |
| Creatinine, mcmol/L | 83.8 (73; 93.6) | 84 (74; 95) | 0.840 |
| eGFR, mL/min | 93.5 (79.8; 107.3) | 89 (75.5; 110) | 0.940 |
| Glucose, mmol/L | 5.6 (5; 6.4) | 5.4 (4.9; 5.8) | 0.101 |
| AST, IU/L | 22 (17; 27) | 20 (17; 26) | 0.520 |
| ALT, IU/L | 23 (16; 33) | 24.5 (18; 34) | 0.439 |
| Potassium, mmol/L | 4.4 (4.1; 4.8) | 4.4 (4.1; 4.7) | 0.990 |
| Medicamentous therapy | |||
| Beta-blockers, % | 84 (74.3) | 95 (74.8) | 0.934 |
| ACE inhibitors, % | 69 (61) | 72 (56.7) | 0.493 |
| Calcium antagonists, % | 37 (32.7) | 46 (36.2) | 0.572 |
| Thiazide diuretics, % | 14 (12) | 7 (5.5) | 0.060 |
| Loop diuretics, % | 13 (11.5) | 10 (7.9) | 0.341 |
| Potassium-sparing diuretics, % | 24 (21) | 22 (17.3) | 0.442 |
| NSAIDs, n (%) | (0) | 0 (0) | |
| Acetylsalicylic acid, n (%) | 36 (31.8) | 44 (34.6) | 0.648 |
| Other antiaggregant, n (%) | 22 (19.5) | 22 (17.3) | 0.668 |
| Nitrates, % | 29 (25.7) | 25 (19.7) | 0.269 |
| Statins, % | 77 (68) | 101 (79.5) | 0.044 |
| LMWHs, n (%) | 27 (23.9) | 29 (22.8) | 0.846 |
| Parameters | Colchicine (n = 113) | Placebo (n = 127) | p |
|---|---|---|---|
| CPB, n (%) | 86 (76) | 100 (78.7) | 0.626 |
| CPB time, min | 105 (75; 130) | 108 (80; 130) | 0.533 |
| Cardioplegia, n (%) | 32 (28.3) | 33 (26) | 0.685 |
| ACC time, min | 62.5 (57; 66.5) | 63 (54; 70) | 0.928 |
| CABG, n (%) AC–1 AC–2 AC–3 VC–1 VC–2 VC–3 VC–4 | 92 (81.4) 63 (55.7) 4 (3.5) 0 (0) 39 (34.5) 35 (30.9) 9 (7.9) 3 (2.6) | 108 (85) 77 (60.6) 5 (3.9) 1 (0.8) 34 (26.7) 34 (26.7) 26 (20.5) 1 (0.8) | 0.453 |
| AV repair, n (%) | 32 (28.3) | 28 (22) | 0.263 |
| Cardiotonic support in ICU, n (%) | 48 (42.5) | 34 (26.7) | 0.010 |
| Lung ventilation time, h | 8.3 (5.8; 13.6) | 8.6 (5.8; 14.8) | 0.750 |
| Length of stay, days | 7 (7; 8) | 7 (6; 9) | 0.679 |
| Subgroup CABG | |||
| Parameters | Colchicine (n = 81) | Placebo (n = 99) | p |
| CPB, n (%) | 54 (66.7) | 72 (72.7) | 0.378 |
| CPB time, min | 83 (60; 106) | 97 (75; 128) | 0.030 |
| Cardiotonic support in ICU, n (%) | 27 (33.3) | 20 (20.2) | 0.046 |
| Lung ventilation time, h | 8 (5.9; 11.8) | 8.2 (5.4; 12.3) | 0.894 |
| Subgroup AV repair | |||
| Parameters | Colchicine (n = 32) | Placebo (n = 28) | p |
| CPB time, min | 131 (113; 149) | 123 (102; 135) | 0.177 |
| ACC time, min | 62.5 (57; 66.5) | 64.5 (54.5; 71.5) | 0.899 |
| AV repair + CABG, n (%) | 11 (34.4) | 9 (32) | 0.854 |
| Cardiotonic support in ICU, n (%) | 21 (65.6) | 14 (50) | 0.221 |
| Lung ventilation time, h | 9.8 (5.7; 17.4) | 12 (8; 17.3) | 0.528 |
| Parameters | Colchicine (n = 113) | Placebo (n = 127) | OR | 95% CI | p |
|---|---|---|---|---|---|
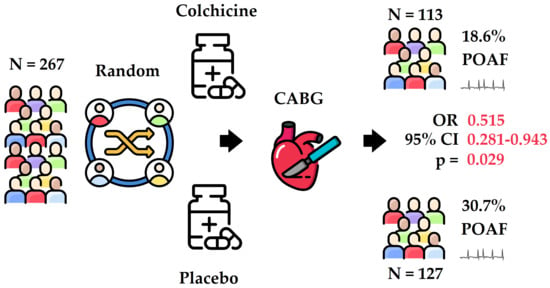
| POAF, n (%) | 21 (18.6) | 39 (30.7) | 0.515 | 0.281–0.943 | 0.029 |
| Hospital mortality, n (%) | 0 (0) | 0 (0) | |||
| Respiratory failure, n (%) | 0 (0) | 0 (0) | |||
| Stroke, n (%) | 0 (0) | 0 (0) | |||
| Bleeding, n (%) | 0 (0) | 0 (0) | |||
| Pericardial puncture, n (%) | (0) | 0 (0.8) | |||
| Infectious complications of postoperative wound, n (%) | 0 (0) | 0 (0) | |||
| Arrhythmias, except AF, n (%) | (3.5) | (3.2) | 1.128 | 0.275–4.621 | 0.866 |
| SVES, n (%) | (0.9) | (3.2) | 0.274 | 0.031–2.493 | 0.202 |
| Pacemaker implantation, n (%) | (2.6) | 0 (0) | |||
| Subgroup CABG | |||||
| POAF | 8 (12) | 25 (25.3) | 0.417 | 0.187–0.930 | 0.026 |
| Arrhythmias, except AF, n (%) | 1 (1.2) | 1 (1) | 1.225 | 0.075–19.89 | 0.887 |
| SVES, n (%) | 1 (1.2) | 3 (3) | 0.400 | 0.041–3.921 | 0.402 |
| Subgroup AV repair | |||||
| POAF | 11 (34.4) | 14 (50) | 0.524 | 0.185–1.481 | 0.220 |
| Arrhythmias, except AF, n (%) | 3 (9.4) | 3 (10.7) | 0.862 | 0.159–4.659 | 0.863 |
| SVES, n (%) | 0 (0) | 1 (3.6) | |||
| Parameters | Beta | Standard Error | t-Value | Exponent Beta | Wald Statistic | p |
|---|---|---|---|---|---|---|
| AV repair | 0.808 | 0.306 | 2.637 | 2.244 | 6.954 | 0.008 |
| Colchicine use | −0.567 | 0.274 | −2.068 | 0.567 | 4.278 | 0.038 |
| Cardiotonic support in ICU | −0.273 | 0.292 | −0.934 | 0.760 | 0.872 | 0.350 |
| Hypertension | 0.461 | 0.601 | 0.766 | 1.586 | 0.587 | 0.443 |
| Previous AMI | −0.231 | 0.325 | −0.711 | 0.793 | 0.508 | 0.476 |
| Male | −0.182 | 0.290 | −0.626 | 0.833 | 0.392 | 0.531 |
| Parameters | Colchicine (n = 113) | Placebo (n = 127) | p |
|---|---|---|---|
| Postoperative day 3 | |||
| LVEF, % | 55 (52; 56.8) | 55 (53; 57) | 0.182 |
| iESV | 19.8 (16.2; 25.2) | 20.1 (17.3; 23.8) | 0.954 |
| iEDV | 44.4 (40; 54.4) | 44.4 (39.4; 51.2) | 0.372 |
| Pericardial effusion, n (%) | 11 (9.5) | 20 (15.8) | 0.146 |
| Pericardial effusion, mm | 3.5 (2.5; 4) | 5 (5; 9) | 0.006 |
| Pleural effusion, n (%) | 48 (43) | 51 (40.5) | 0.698 |
| Pleural effusion, mm | 18 (12; 20) | 20 (15; 26) | 0.063 |
| Postoperative day 5 | |||
| LVEF, % | 55.6 (53; 58) | 55 (54; 58) | 0.511 |
| iESV | 19.7 (16.2; 23.4) | 19.6 (16.6; 23.8) | 0.867 |
| iEDV | 45.3 (38.3; 53.3) | 45 (38.5; 53.9) | 0.818 |
| Pericardial effusion, n (%) | 23 (20.4) | 28 (22.1) | 0.745 |
| Pericardial effusion, mm | 5 (3; 6) | 5 (5; 6) | 0.122 |
| Pleural effusion, n (%) | 49 (43.3) | 60 (47) | 0.491 |
| Pleural effusion, mm | 19.5 (10; 26) | 20 (15; 32) | 0.034 |
| Parameters | Colchicine (n = 113) | Placebo (n = 127) | p |
|---|---|---|---|
| Postoperative day 3 | |||
| WBC, 10×9/L | 11.4 (9.5; 14.2) | 12 (9.6; 14.6) | 0.284 |
| Neutrophils, 10×9/L | 8.8 (6.7; 12) | 8.9 (7.8; 12.7) | 0.536 |
| Neutrophils, % | 77 (71; 84) | 79 (72; 82) | 0.901 |
| Platelets,10×9/L | 189 (160; 237) | 199 (162; 254) | 0.442 |
| Creatinine, mcmol/L | 72 (65; 82) | 75 (66.7; 88.5) | 0.065 |
| eGFR | 107 (90; 119) | 100 (84; 124) | 0.216 |
| Glucose, mmol/L | 7 (5.7; 8.6) | 6.6 (5.7; 8.3) | 0.441 |
| AST, IU/L | 31 (24; 45) | 31 (21; 40) | 0.494 |
| ALT, IU/L | 20 (14; 30) | 21 (13; 29) | 0.995 |
| Potassium, mmol/L | 4.1 (3.8; 4.3) | 4.2 (3.9; 4.5) | 0.056 |
| Postoperative day 5 | |||
| WBC, 10×9/L | 9.3 (8; 11) | 10.9 (8.4; 13.2) | 0.003 |
| Neutrophils, 10×9/L | 5.9 (4.7; 7.5) | 6.8 (5; 9.4) | 0.014 |
| Neutrophils, % | 62 (58.6; 68.9) | 63 (57; 68) | 0.982 |
| Platelets, 10×9/L | 265 (211; 314) | 262 (217; 339) | 0.631 |
| Creatinine, mcmol/L | 75 (68; 83) | 77 (68; 86) | 0.566 |
| eGFR | 103 (85; 119) | 100 (82; 127) | 0.755 |
| Glucose, mmol/L | 6.4 (5.3; 7.4) | 5.9 (5.3; 7.3) | 0.905 |
| AST, IU/L | 28 (22; 34) | 29 (20; 38) | 0.885 |
| ALT, IU/L | 28 (20; 42) | 27 (17; 46) | 0.886 |
| Potassium, mmol/L | 4.1 (3.7; 4.4) | 4.3 (4; 4.6) | 0.011 |
| Parameters | Colchicine (n = 113) | Placebo (n = 127) | OR | 95% Cl | p |
|---|---|---|---|---|---|
| Nausea, n (%) | 14 (12.4) | 15 (11.8) | 1.055 | 0.486–2.296 | 0.891 |
| Vomiting, n (%) | 2 (1.8) | 6 (4.7) | 0.364 | 0.072–1.839 | 0.191 |
| Lack of appetite, n (%) | 19 (16.9) | 24 (18.9) | 0.867 | 0.447–1.676 | 0.674 |
| Diarrhea, n (%) | 29 (25.7) | 15 (11.8) | 2.578 | 1.300–5.111 | 0.005 |
| Abdominal pain, n (%) | 8 (7) | 2 (1.6) | 4.762 | 1.010–22.91 | 0.028 |
| Convulsions, n (%) | 2 (1.8) | 7 (5.5) | 0.309 | 0.063–1.518 | 0.115 |
| Tingling in hands and feet, n (%) | 9 (8) | 10 (7.8) | 1.012 | 0.396–2.588 | 0.979 |
| Skin rashes, n (%) | 0 (0) | 0 (0) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shvartz, V.; Le, T.; Enginoev, S.; Sokolskaya, M.; Ispiryan, A.; Shvartz, E.; Nudel, D.; Araslanova, N.; Petrosyan, A.; Donakanyan, S.; et al. Colchicine in Cardiac Surgery: The COCS Randomized Clinical Trial. J. Cardiovasc. Dev. Dis. 2022, 9, 363. https://doi.org/10.3390/jcdd9100363
Shvartz V, Le T, Enginoev S, Sokolskaya M, Ispiryan A, Shvartz E, Nudel D, Araslanova N, Petrosyan A, Donakanyan S, et al. Colchicine in Cardiac Surgery: The COCS Randomized Clinical Trial. Journal of Cardiovascular Development and Disease. 2022; 9(10):363. https://doi.org/10.3390/jcdd9100363
Chicago/Turabian StyleShvartz, Vladimir, Tatyana Le, Soslan Enginoev, Maria Sokolskaya, Artak Ispiryan, Elena Shvartz, Daria Nudel, Naylyana Araslanova, Andrey Petrosyan, Sergey Donakanyan, and et al. 2022. "Colchicine in Cardiac Surgery: The COCS Randomized Clinical Trial" Journal of Cardiovascular Development and Disease 9, no. 10: 363. https://doi.org/10.3390/jcdd9100363