Emerging Applications of Nanotechnology in Dentistry
Abstract
:1. Introduction
2. Methodology
2.1. Search Criteria
2.2. Eligibility Criteria
3. Results
3.1. Classification of Nanoparticles in Dental Materials
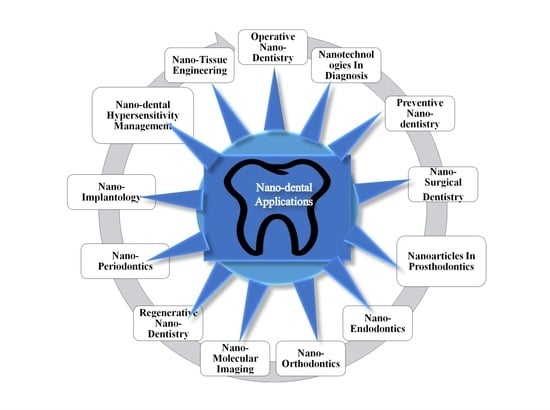
3.2. Application of Nanotechnology in Dentistry
3.2.1. Operative Nanodentistry
Nano-Glass Ionomer
Nanocomposites
3.2.2. Nanotechnology Applications in Prosthodontics
3.2.3. Nanotechnology Applications in Endodontics
3.2.4. Nanotechnology Applications in Orthodontics
3.2.5. Nanotechnology Applications in Periodontics and Implantology
3.2.6. Nanotechnology Applications for Hypersensitivity Management
3.2.7. Nanotechnology Applications for Nano-Tissue Engineering
3.2.8. Nanotechnology Applications in the Surgical Field
3.2.9. Preventive Nanodentistry
3.2.10. Nanotechnology Applications in Diagnosis
3.2.11. Nano-Molecular Imaging in Dental Science
3.2.12. Some Other Applications of Nanodentistry
3.3. Limitations in the Field
4. Future Perspectives and Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Jandt, K.D.; Watts, D.C. Nanotechnology in Dentistry: Present and Future Perspectives on Dental Nanomaterials. Dent. Mater. 2020, 36, 1365–1378. [Google Scholar] [CrossRef] [PubMed]
- Malik, S.; Muhammad, K.; Waheed, Y. Emerging Applications of Nanotechnology in Healthcare and Medicine. Molecules 2023, 28, 6624. [Google Scholar] [CrossRef] [PubMed]
- Barot, T.; Rawtani, D.; Kulkarni, P. Nanotechnology-Based Materials as Emerging Trends for Dental Applications. Rev. Adv. Mater. Sci. 2021, 60, 173–189. [Google Scholar] [CrossRef]
- Amissah, F.; Andey, T.; Ahlschwede, K.M. Nanotechnology-Based Therapies for the Prevention and Treatment of Streptococcus Mutans-Derived Dental Caries. J. Oral Biosci. 2021, 63, 327–336. [Google Scholar] [CrossRef]
- Gauba, K.; Gupta, A.; Sharda, S. Nanotechnology in Dentistry. Biomed. Transl. Res. Drug Des. Discov. 2022, 2022, 141–152. [Google Scholar]
- Subramani, K.; Elhissi, A.; Subbiah, U.; Ahmed, W. Introduction to nanotechnology. In Nanobiomaterials in Clinical Dentistry; Elsevier: Amsterdam, The Netherlands, 2019; pp. 3–18. [Google Scholar]
- Kennedy, S.; Srinivasan, S.; Jayavel, K.; Sundaram, R. Nanotechnology in Periodontal Management. Int. J. Orofac. Biol. 2019, 3, 8. [Google Scholar] [CrossRef]
- Contera, S.; Bernardino de la Serna, J.; Tetley, T.D. Biotechnology, Nanotechnology and Medicine. Emerg. Top. Life Sci. 2020, 4, 551–554. [Google Scholar] [CrossRef]
- Deepali, S.; Priyanka, A.; Shweta, B.; Kirti, P. Nanotechnology in periodontics. A review. Santosh Univ. J. Health Sci. 2021, 7, 6–10. [Google Scholar] [CrossRef]
- Patel, R.M.; Dahane, T.M.; Godbole, S.; Kambala, S.S.; Mangal, K. Applications of Nanotechnology in Prosthodontics. J. Evol. Med. Dent. Sci. 2020, 9, 3566–3571. [Google Scholar] [CrossRef]
- Soto, F.; Wang, J.; Ahmed, R.; Demirci, U. Medical Micro/Nanorobots in Precision Medicine. Adv. Sci. 2020, 7, 2002203. [Google Scholar] [CrossRef]
- Buniyamin, I.; Akhir, R.M.; Asli, N.A.; Khusaimi, Z.; Malek, M.F.; Mahmood, M.R. Nanotechnology Applications in Biomedical Systems. Curr. Nanomater. 2022, 7, 167–180. [Google Scholar] [CrossRef]
- Mirsasaani, S.S.; Hemati, M.; Dehkord, E.S.; Yazdi, G.T.; Poshtiri, D.A. Nanotechnology and nanobiomaterials in dentistry. In Nanobiomaterials in Clinical Dentistry; Elsevier: Amsterdam, The Netherlands, 2019; pp. 19–37. [Google Scholar]
- Joseph, B. Nanotechnology in Oral and Dental Diagnosis. In Nanomaterials in Dental Medicine; Springer: Berlin/Heidelberg, Germany, 2023; pp. 33–49. [Google Scholar]
- Haleem, A.; Javaid, M.; Singh, R.P.; Rab, S.; Suman, R. Applications of Nanotechnology in Medical Field: A Brief Review. Glob. Health J. 2023, 7, 70–77. [Google Scholar] [CrossRef]
- Foong, L.K.; Foroughi, M.M.; Mirhosseini, A.F.; Safaei, M.; Jahani, S.; Mostafavi, M.; Ebrahimpoor, N.; Sharifi, M.; Varma, R.S.; Khatami, M. Applications of Nano-Materials in Diverse Dentistry Regimes. RSC Adv. 2020, 10, 15430–15460. [Google Scholar] [CrossRef]
- Prabakar, J. Current applications of nanoparticles in preventive dentistry–A Literature review. J. Surv. Fish Sci. 2023, 10, 460–467. [Google Scholar]
- Kochan, O.; Boitsaniuk, S.; Levkiv, M.; Przystupa, K.; Manashchuk, N.; Pohoretska, K.; Chornij, N.; Tsvyntarna, I.; Patskan, L. Emergence of Nano-Dentistry as a Reality of Contemporary Dentistry. Appl. Sci. 2022, 12, 2008. [Google Scholar] [CrossRef]
- Agnihotri, R.; Gaur, S.; Albin, S. Nanometals in Dentistry: Applications and Toxicological Implications—A Systematic Review. Biol. Trace Elem. Res. 2019, 197, 70–88. [Google Scholar] [CrossRef]
- Uppal, M.K.; Sharma, M.L.; Sharma, S.; Thakar, S. The Magnanimity of Nanodentistry; OrangeBooks Publication: Bhilai, India, 2021. [Google Scholar]
- Sreenivasalu, P.K.P.; Dora, C.P.; Swami, R.; Jasthi, V.C.; Shiroorkar, P.N.; Nagaraja, S.; Asdaq, S.M.B.; Anwer, M.K. Nanomaterials in Dentistry: Current Applications and Future Scope. Nanomaterials 2022, 12, 1676. [Google Scholar] [CrossRef]
- Dissanayaka, W.L.; Sharpe, P. Editorial: Frontiers in Dental Medicine: Highlights in Regenerative Dentistry 2021/22. Front. Dent. Med. 2023, 4, 1212894. [Google Scholar] [CrossRef]
- Calisir, M. Nanotechnology in dentistry: Past, present, and future. In Nanomaterials for Regenerative Medicine; Springer: Berlin/Heidelberg, Germany, 2019; pp. 197–216. [Google Scholar]
- Guo, T.; Scimeca, J.-C.; Ivanovski, S.; Verron, E.; Gulati, K. Enhanced Corrosion Resistance and Local Therapy from Nano-Engineered Titanium Dental Implants. Pharmaceutics 2023, 15, 315. [Google Scholar] [CrossRef] [PubMed]
- Nandagopal, N.; Usha, M.; Sreejith, S.; Rajan, S. A Clinical Review of Nanotechnology in Maxillofacial Practice. J. Oral Res. Rev. 2021, 13, 149. [Google Scholar] [CrossRef]
- Umapathy, V.R.; Natarajan, P.M.; SumathiJones, C.; Swamikannu, B.; Johnson, W.M.S.; Alagarsamy, V.; Milon, A.R. Current Trends and Future Perspectives on Dental Nanomaterials—An Overview of Nanotechnology Strategies in Dentistry. J. King Saud Univ. Sci. 2022, 34, 102231. [Google Scholar] [CrossRef]
- Padmanabhan, S. Nanotechnology in Orthodontics. Semin. Orthod. 2023, 29, 79–84. [Google Scholar] [CrossRef]
- Ali Fathima, S.; Abiraj, K.R.; Pratheesha, A.P.; Mohan, S.M.; Krishna, A.S.; Dynamol, S. Knowing the unknown: A review on nanotechnology in Orthodontics. J. Pharm. Res. Int. 2023, 35, 30–40. [Google Scholar] [CrossRef]
- Zakrzewski, W.; Dobrzynski, M.; Dobrzynski, W.; Zawadzka-Knefel, A.; Janecki, M.; Kurek, K.; Lubojanski, A.; Szymonowicz, M.; Rybak, Z.; Wiglusz, R.J. Nanomaterials application in Othrodontics. Nanomaterials 2021, 11, 337. [Google Scholar] [CrossRef] [PubMed]
- Bhushan, J.; Maini, C. Nanoparticles: A Promising Novel Adjunct for Dentistry. Indian J. Dent. Sci. 2019, 11, 167. [Google Scholar] [CrossRef]
- Hossain, N.; Islam, M.A.; Chowdhury, M.A.; Alam, A. Advances of Nanoparticles Employment in Dental Implant Applications. Appl. Surf. Sci. Adv. 2022, 12, 100341. [Google Scholar] [CrossRef]
- Vasiliu, S.; Racovita, S.; Gugoasa, I.A.; Lungan, M.-A.; Popa, M.; Desbrieres, J. The Benefits of Smart Nanoparticles in Dental Applications. Int. J. Mol. Sci. 2021, 22, 2585. [Google Scholar] [CrossRef]
- Chandra, H.; Kumari, P.; Bontempi, E.; Yadav, S. Medicinal Plants: Treasure Trove for Green Synthesis of Metallic Nanoparticles and Their Biomedical Applications Biocatal. Agric. Biotechnol. 2020, 24, 101518. [Google Scholar] [CrossRef]
- Sakthi Devi, R.; Girigoswami, A.; Siddharth, M.; Girigoswami, K. Applications of Gold and Silver Nanoparticles in Theranostics. Appl. Biochem. Biotechnol. 2022, 194, 4187–4219. [Google Scholar] [CrossRef]
- Wang, Q.; Zhang, Y.; Li, Q.; Chen, L.; Liu, H.; Ding, M.; Dong, H.; Mou, Y. Therapeutic Applications of Antimicrobial Silver-Based Biomaterials in Dentistry. Int. J. Nanomed. 2022, 17, 443–462. [Google Scholar] [CrossRef]
- Fernandez, C.C.; Sokolonski, A.R.; Fonseca, M.S.; Stanisic, D.; Araújo, D.B.; Azevedo, V.; Portela, R.D.; Tasic, L. Applications of Silver Nanoparticles in Dentistry: Advances and Technological Innovation. Int. J. Mol. Sci. 2021, 22, 2485. [Google Scholar] [CrossRef]
- Butrón Téllez Girón, C.; Hernández Sierra, J.F.; DeAlba-Montero, I.; Urbano Peña, M.d.l.A.; Ruiz, F. Therapeutic Use of Silver Nanoparticles in the Prevention and Arrest of Dental Caries. Bioinorg. Chem. Appl. 2020, 2020, 8882930. [Google Scholar] [CrossRef] [PubMed]
- Castro-Rojas, M.A.; Vega-Cantu, Y.I.; Cordell, G.A.; Rodriguez-Garcia, A. Dental Applications of Carbon Nanotubes. Molecules 2021, 26, 4423. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, P.A.; Fahmy, A.E.; El Shabrawy, S.M. Three-Dimensionally Printed Denture Base Resins Modified by Nanoglass Particles and Carbon Nanotubes. J. Prosthet. Dent. 2023, 130, P797. [Google Scholar] [CrossRef] [PubMed]
- Mousavi, S.M.; Yousefi, K.; Hashemi, S.A.; Afsa, M.; BahranI, S.; Gholami, A.; Ghahramani, Y.; Alizadeh, A.; Chiang, W.-H. Renewable Carbon Nanomaterials: Novel Resources for Dental Tissue Engineering. Nanomaterials 2021, 11, 2800. [Google Scholar] [CrossRef]
- Radhi, A.; Mohamad, D.; Abdul Rahman, F.S.; Abdullah, A.M.; Hasan, H. Mechanism and Factors Influence of Graphene-Based Nanomaterials Antimicrobial Activities and Application in Dentistry. J. Mater. Res. Technol. 2021, 11, 1290–1307. [Google Scholar] [CrossRef]
- Nizami, M.Z.I.; Takashiba, S.; Nishina, Y. Graphene Oxide: A New Direction in Dentistry. Appl. Mater. Today. 2020, 19, 100576. [Google Scholar] [CrossRef]
- Xu, V.W.; Nizami, M.Z.I.; Yin, I.X.; Yu, O.Y.; Lung, C.Y.K.; Chu, C.H. Application of Copper Nanoparticles in Dentistry. Nanomaterials 2022, 12, 805. [Google Scholar] [CrossRef]
- He, L.; Dai, D.; Xie, L.; Chen, Y.; Zhang, C. Biological Effects, Applications and Strategies of Nanomodification of Dental Metal Surfaces. Mater. Des. 2021, 207, 109890. [Google Scholar] [CrossRef]
- Yazdanian, M.; Rostamzadeh, P.; Rahbar, M.; Alam, M.; Abbasi, K.; Tahmasebi, E.; Tebyaniyan, H.; Ranjbar, R.; Seifalian, A.; Yazdanian, A. The Potential Application of Green-Synthesized Metal Nanoparticles in Dentistry: A Comprehensive Review. Bioinorg. Chem. Appl. 2022, 2022, 2311910. [Google Scholar] [CrossRef]
- Thangavelu, L.; Veeraragavan, G.R.; Mallineni, S.K.; Devaraj, E.; Parameswari, R.P.; Syed, N.H.; Dua, K.; Chellappan, D.K.; Balusamy, S.R.; Bhawal, U.K. Role of Nanoparticles in Environmental Remediation: An Insight into Heavy Metal Pollution from Dentistry. Bioinorg. Chem. Appl. 2022, 2022, 1946724. [Google Scholar] [CrossRef] [PubMed]
- Pushpalatha, C.; Suresh, J.; Gayathri, V.; Sowmya, S.; Augustine, D.; Alamoudi, A.; Zidane, B.; Mohammad Albar, N.H.; Patil, S. Zinc Oxide Nanoparticles: A Review on Its Applications in Dentistry Front. Bioeng. Biotechnol. 2022, 10, 917990. [Google Scholar] [CrossRef]
- Moradpoor, H.; Safaei, M.; Mozaffari, H.R.; Sharifi, R.; Imani, M.M.; Golshah, A.; Bashardoust, N. An Overview of Recent Progress in Dental Applications of Zinc Oxide Nanoparticles. RSC Adv. 2021, 11, 21189–21206. [Google Scholar] [CrossRef]
- Raja, V.; Selvan, G.; Anbarasu, R.; Baskar, S. Synthesis of Zinc Oxide Nanoparticles and Setariaverticillata Assisted Activated Carbon Blended Zinc Oxide Nanoparticles. Indian J. Sci. Technol. 2019, 12, 37. [Google Scholar] [CrossRef]
- Karthikeyan, M.; Ahila, S.C.; Kumar, B.M. The antibacterial influence of nanotopographic titanium, zirconium, and aluminum nanoparticles against Staphylococcus aureus and porphyromonas gingivalis: An in vitro study. Indian J. Dent. Res. 2019, 30, 37. [Google Scholar]
- Gulati, K.; Ding, C.; Guo, T.; Guo, H.; Yu, H.; Liu, Y. Craniofacial Therapy: Advanced Local Therapies from Nano-Engineered Titanium Implants to Treat Craniofacial Conditions. Int. J. Oral Sci. 2023, 15, 15. [Google Scholar] [CrossRef]
- Gupta, S.; Noumbissi, S.; Kunrath, M.F. Nano Modified Zirconia Dental Implants: Advances and the Frontiers for Rapid Osseointegration. Med. Devices Sens. 2020, 3, e10076. [Google Scholar] [CrossRef]
- Nagarale, R.; Kadu, N.; Dhumavat, P.; Muluk, S.S.; Jamal, A. Nano Anesthesia and Nano Drug Delivery-A Review Article. Asian J. Dent. Sci. 2022, 5, 240–245. [Google Scholar]
- Ha, S.-W.; Weiss, D.; Weitzmann, M.N.; Beck, B.R., Jr. Applications of silica-based nanomaterials in dental and skeletal biology. In Nanobiomaterials in Clinical Dentistry; Elsevier: Amsterdam, The Netherlands, 2019; pp. 77–112. [Google Scholar]
- Bordea, I.R.; Candrea, S.; Alexescu, G.T.; Bran, S.; Băciuț, M.; Băciuț, G.; Lucaciu, O.; Dinu, C.M.; Todea, D.A. Nano-Hydroxyapatite Use in Dentistry: A Systematic Review. Drug Metab. Rev. 2020, 52, 319–332. [Google Scholar] [CrossRef] [PubMed]
- Sinjari, B.; Pizzicannella, J.; D’Aurora, M.; Zappacosta, R.; Gatta, V.; Fontana, A.; Trubiani, O.; Diomede, F. Curcumin/Liposome Nanotechnology as Delivery Platform for Anti-Inflammatory Activities via NFkB/ERK/pERK Pathway in Human Dental Pulp Treated With 2-HydroxyEthyl MethAcrylate (HEMA). Front. Physiol. 2019, 10, 633. [Google Scholar] [CrossRef]
- Altwaijri, Y.A.; Al-Habeeb, A.; Al-Subaie, A.S.; Bilal, L.; Al-Desouki, M.; Shahab, M.K.; Hyder, S.; Sampson, N.A.; King, A.J.; Kessler, R.C. Twelve-month Prevalence and Severity of Mental Disorders in the Saudi National Mental Health Survey. Int. J. Methods Psychiatr. Res. 2020, 29, e1831. [Google Scholar] [CrossRef] [PubMed]
- Vellaichamy, M.; Škarabot, M.; Muševič, I. Optical Gain and Photo-Bleaching of Organic Dyes, Quantum Dots, Perovskite Nanoplatelets and Nanodiamonds. Liq. Cryst. 2023, 50, 1–22. [Google Scholar] [CrossRef]
- Samanta, S. Periodontics: ORIGINAL REVIEW Nanoperiodontics-A Futuristic Trend in Periodontal Management. Clin. Dent. (0974-3979) 2022, 16, 12–20. [Google Scholar]
- Malik, S.; Muhammad, K.; Waheed, Y. Nanotechnology: A Revolution in Modern Industry. Molecules 2023, 28, 661. [Google Scholar] [CrossRef] [PubMed]
- Chokkattu, J.J.; Neeharika, S.; Rameshkrishnan, M. Applications of Nanomaterials in Dentistry: A review. J Int Soc Prev Community Dent. 2023, 13, 32–41. [Google Scholar] [CrossRef] [PubMed]
- Raura, N.; Garg, A.; Arora, A.; Roma, M. Nanoparticle Technology and Its Implications in Endodontics: A Review. Biomater. Res. 2020, 24, 21. [Google Scholar] [CrossRef]
- Gupta, R.; Sharma, S. Nanotechnology in Prosthetic Dentistry A Review. J. Prosthet. Implant Dent. 2022, 6, 42–47. [Google Scholar] [CrossRef]
- Choubisa, D. An Overview of Applications of Nanotechnology in Prosthodontics. J. Prosthodont. Dent. 2022, 17, 1–22. [Google Scholar]
- Sen, S.; Singh, G. Finding Hidden Gems: Nanoparticles in Oral Health-A Review. Int. J. Drug Res. Dent. Sci. 2020, 2, 24–28. [Google Scholar]
- Sen, D.; Patil, V.; Smriti, K.; Varchas, P.; Ratnakar, R.; Shetty, D.K.; Naik, N.; Kumar, S. Nanotechnology and Nanomaterials in Dentistry: Present and Future Perspectives in Clinical Applications. Eng. Sci. 2022, 20, 14–24. [Google Scholar] [CrossRef]
- Altankhishig, B.; Matsuda, Y.; Nagano-takebe, F.; Okuyama, K.; Yamamoto, H.; Sakurai, M.; Naito, K.; Hayashi, M.; Sano, H.; Sidhu, S.K.; et al. Potential of Fluoride containing Zinc Oxide and Copper Oxide nanocomposites on dental bonding ability. Nanomaterials 2022, 12, 1291. [Google Scholar] [CrossRef]
- Gupta, P.K. Applications of Nanotechnology in Dentistry. Nanotoxicol. Nanobiomed. 2023, 111–123. [Google Scholar]
- Asha, A.B.; Narain, R. Nanomaterials properties. Polymers Science and Nanotechnology. Fundam. Appl. 2020, 15, 343–359. [Google Scholar] [CrossRef]
- Hamouda, R.A.; Qarabai, F.A.K.; Shahabuddin, F.S.; Al-Shaikh, T.M.; Makharita, R.R. Antibacterial activity of Ulva/Nanocellulose and Ulva/Ag/Cellulose nanocomposites and both blended with Fluoride against bacteria causing dental decay. Polymers 2023, 15, 1047. [Google Scholar] [CrossRef] [PubMed]
- Bonilla-Represa, V.; Abalos-Labruzzi, C.; Herrera-Martinez, M.; Guerrero-Pérez, M.O. Nanomaterials in Dentistry: State of the Art and Future Challenges. Nanomaterials 2020, 10, 1770. [Google Scholar] [CrossRef] [PubMed]
- Orts-Gil, G.; Natte, K.; Österle, W. Multi-Parametric Reference Nanomaterials for Toxicology: State of the Art, Future Challenges and Potential Candidates. RSC Adv. 2013, 3, 18202. [Google Scholar] [CrossRef]
- Xenaki, V.; Marthinussen, M.C.; Costea, D.E.; Didilescu, A.C.; Susin, C.; Cimpan, M.R.; Åstrøm, A.N. Knowledge about Nanotechnology and Intention to Use Nanomaterials: A Comparative Study among Dental Students in Norway and Romania. Eur. J. Dent. Educ. 2019, 24, 79–87. [Google Scholar] [CrossRef]
- Tahmasbi, S.; Mohamadian, F.; Hosseini, S.; Eftekhar, L. A review on the applications of nanotechnology in orthodontics. Nanomed J. 2019, 6, 11–18. [Google Scholar]
- Zafar, M.S.; Amin, F.; Fareed, M.A.; Ghabbani, H.; Riaz, S.; Khurshid, Z.; Kumar, N. Biomimetic Aspects of Restorative Dentistry Biomaterials. Biomimetics 2020, 5, 34. [Google Scholar] [CrossRef]
- Modi, S.; Prajapati, R.; Inwati, G.K.; Deepa, N.; Tirth, V.; Yadav, V.K.; Yadav, K.K.; Islam, S.; Gupta, P.; Kim, D.-H.; et al. Recent Trends in Fascinating Applications of Nanotechnology in Allied Health Sciences. Crystals 2021, 12, 39. [Google Scholar] [CrossRef]
- Zafar, M.S.; Alnazzawi, A.A.; Alrahabi, M.; Fareed, M.A.; Najeeb, S.; Khurshid, Z. Nanotechnology and nanomaterials in dentistry. In Advanced Dental Biomaterials; Elsevier: Amsterdam, The Netherlands, 2019; pp. 477–505. [Google Scholar]
- Park, E.Y.; Kang, S. Current Aspects and Prospects of Glass Ionomer Cements for Clinical Dentistry. Yeungnam Univ. J. Med. 2020, 37, 169–178. [Google Scholar] [CrossRef]
- Zakrzewski, W.; Dobrzyński, M.; Zawadzka-Knefel, A.; Lubojański, A.; Dobrzyński, W.; Janecki, M.; Kurek, K.; Szymonowicz, M.; Wiglusz, R.J.; Rybak, Z. Nanomaterials Application in Endodontics. Materials 2021, 14, 5296. [Google Scholar] [CrossRef] [PubMed]
- Esteban Florez, F.L.; Trofimov, A.A.; Ievlev, A.; Qian, S.; Rondinone, A.J.; Khajotia, S.S. Advanced Characterization of Surface-Modified Nanoparticles and Nanofilled Antibacterial Dental Adhesive Resins. Sci. Rep. 2020, 10, 9811. [Google Scholar] [CrossRef] [PubMed]
- De Stefani, A.; Bruno, G.; Preo, G.; Gracco, A. Application of Nanotechnology in Orthodontic Materials: A State-of-the-Art Review. Dent. J. 2020, 8, 126. [Google Scholar] [CrossRef] [PubMed]
- Qi, M.; Li, X.; Sun, X.; Li, C.; Tay, F.R.; Weir, M.D.; Dong, B.; Zhou, Y.; Wang, L.; Xu, H.H.K. Novel Nanotechnology and Near-Infrared Photodynamic Therapy to Kill Periodontitis-Related Biofilm Pathogens and Protect the Periodontium. Dent. Mater. 2019, 35, 1665–1681. [Google Scholar] [CrossRef]
- Makvandi, P.; Josic, U.; Delfi, M.; Pinelli, F.; Jahed, V.; Kaya, E.; Ashrafizadeh, M.; Zarepour, A.; Rossi, F.; Zarrabi, A.; et al. Drug Delivery (Nano) Platforms for Oral and Dental Applications: Tissue Regeneration, Infection Control, and Cancer Management. Adv. Sci. 2021, 8, 2004014. [Google Scholar] [CrossRef]
- Panchbhai, A. Nanotechnology in dentistry. In Applications of Nanocomposite Materials in Dentistry; Elsevier: Amsterdam, The Netherlands, 2019; pp. 191–203. [Google Scholar]
- Moothedath, M.; Moothedath, M.; Jairaj, A.; Harshitha, B.; Baba, S.; Khateeb, S. Role of Nanotechnology in Dentistry: Systematic Review. J. Int. Soc. Prev. Community Dent. 2019, 9, 535. [Google Scholar] [CrossRef]
- Sachdeva, S.; Mani, A.; Mani, S.A.; Vora, H.R.; Gholap, S.S.; Sodhi, J.K. Nano-robotics: The future of health and dental care. IP Int. J Perio Implant. 2021, 6, 6–10. [Google Scholar] [CrossRef]
- Kumar, R.; Jha, K.; Barman, D. Nanotechnology in Oral Cancer Prevention and Therapeutics: A Literature Review. Indian J. Med. Paediatr. Oncol. 2021, 42, 146–152. [Google Scholar] [CrossRef]
- Tawfik, E.A.; Tawfik, A.F.; Alajmi, A.M.; Badr, M.Y.; Al-jedai, A.; Almozain, N.H.; Bukhary, H.A.; Halwani, A.A.; Al Awadh, S.A.; Alshamsan, A.; et al. Localizing Pharmaceuticals Manufacturing and Its Impact on Drug Security in Saudi Arabia. Saudi Pharm. J. 2022, 30, 28–38. [Google Scholar] [CrossRef]
- Mani, R.; Chellapandian, K.; Gayathri, K.; Kumar, S.K.; Kondas, V.V. Role of Nanotechnology in Regeneration of Pulpo-Dentinal Complex. Int. J. Health Sci. 2022, 6, 11450–11457. [Google Scholar] [CrossRef]
- Lubojanski, A.; Dobrzynski, M.; Nowak, N.; Rewak-Soroczynska, J.; Sztyler, K.; Zakrzewski, W.; Dobrzynski, W.; Szymonowicz, M.; Rybak, Z.; Wiglusz, K.; et al. Application of Selected Nanomaterials and Ozone in Modern Clinical Dentistry. Nanomaterials 2021, 11, 259. [Google Scholar] [CrossRef] [PubMed]
- Babu, N.A.; Anjuga, E.P.S.; Nagarajan, K.; Masthan, K.M.K. Nanotechnology in Detection of Oral Cancer. Indian J. Public Health Res. Dev. 2019, 10, 3205. [Google Scholar] [CrossRef]
- Tetè, G.; Capparè, P.; Gherlone, E. New Application of Osteogenic Differentiation from HiPS Stem Cells for Evaluating the Osteogenic Potential of Nanomaterials in Dentistry. Int. J. Environ. Res. Public Health 2020, 17, 1947. [Google Scholar] [CrossRef] [PubMed]
- Jandt, K.D.; Sigusch, B.W. Future Perspectives of Resin-Based Dental Materials. Dent. Mater. 2009, 25, 1001–1006. [Google Scholar] [CrossRef]
- Liu, F.; Hong, T.; Xie, J.; Zhan, X.; Wang, Y. Application of Reactive Oxygen Species-Based Nanomaterials in Dentistry: A Review. Crystals 2021, 11, 266. [Google Scholar] [CrossRef]
- Yazdanian, M.; Rahmani, A.; Tahmasebi, E.; Tebyanian, H.; Yazdanian, A.; Mosaddad, S.A. Current and Advanced Nanomaterials in Dentistry as Regeneration Agents: An Update. Mini-Rev. Med. Chem. 2021, 21, 899–918. [Google Scholar] [CrossRef]
- Mok, Z.H.; Proctor, G.; Thanou, M. Emerging Nanomaterials for Dental Treatments. Emerg. Top. Life Sci 2020, 4, 613–625. [Google Scholar] [CrossRef] [PubMed]
- Kumara Sundaram, R.; Varghese, B. All Ceramic Materials in Dentistry: Past, Present and Future: A Review. Int. J. Contemp. Med. Res. [IJCMR] 2020, 7, B9–B11. [Google Scholar] [CrossRef]
- Kalotra, J.; Gaurav, K.; Kaur, J.; Sethi, D.; Arora, G.; Khurana, D. Recent Advancements in Restorative Dentistry: An Overview. J. Curr. Med. Res. Opin. 2020, 3, 522–530. [Google Scholar] [CrossRef]
- Vijayalakshmi, R.; Ramakrishnan, T.; Srinivasan, S.; Kumari, B.N. Nanotechnology in Periodontics: An Overview. Medico-Legal Update 2020, 20, 2274–2279. [Google Scholar]
- Bastos, N.A.; Bitencourt, S.B.; Martins, E.A.; De Souza, G.M. Review of Nano-technology Applications in Resin-based Restorative Materials. J. Esthet. Restor. Dent. 2020, 33, 567–582. [Google Scholar] [CrossRef] [PubMed]
| Sr. No. | Search Items | Search Combinations |
|---|---|---|
| 1. | Nanotechnology |
Dentistry and nanotechnology Applications of nanotechnology in dentistry Update on nanodentistry |
| 2. | Nanodentistry | Nanodentistry benefits and application Latest update on nanoscience application in dental field |
| 3. | Nanomaterials | Nanomaterials used in dental sciences Nanomaterials and dentistry |
| 4. | Nanocomposites | Applications of nanocomposites in dentistry |
| 5. | Nanometals | Nanometals and dentistry |
| 6. | Nanoscineeces and healthcare | Healthcare and nanomaterials; latest applications Applications of nanomaterials in healthcare and dentistry |
| 7. | Nanorobots | Nanorobots applications in field of dentistry |
| Sr. No. | Nanomaterials | Properties | Benefits and Applications | References |
|---|---|---|---|---|
| 1. | Nanoparticles |
|
| [30,31,32] |
| 2. | Metallic nanoparticles |
|
| [33,34] |
| 3. | Silver nanoparticles (AgNPs) |
|
| [34,35,36,37] |
| 4. | Carbon nanotubes |
|
| [38,39,40] |
| 5. | Graphene-based NPs |
|
| [41,42] |
| 6. | Gold nanoparticles (AuNPs) |
|
| [33,34,36] |
| 7. | Copper nanoparticles (CuNPs) |
|
| [43] |
| 8. | Metal oxide nanoparticles |
|
| [33,44,45,46] |
| 9. | Zinc oxide nanoparticles (ZnO NPs) |
|
| [47,48,49] |
| 10. | Titanium dioxide nanoparticles (TiO2 NPs) |
|
| [24,50,51] |
| 11. | Titania-based NPs |
|
| [24,50,51] |
| 12. | Zirconium dioxide nanoparticles (ZrO2 NPs) |
|
| [50,52] |
| 13. | Aluminum oxide nanoparticles (Al2O3 NPs) |
|
| [1,50,53] |
| 14. | Silicon dioxide nanoparticles (SiO2 NPs) |
|
| [1,16,54] |
| 15. | Zirconia |
|
| [50,52] |
| 16. | Silica-based NPs |
|
| [35,54] |
| 17. | Hydroxyapatite (HAp)-based NP formulations. |
|
| [55,56,57] |
| Sr. No. | Unconventional Nanoparticles | Characteristics | Applications | References |
|---|---|---|---|---|
| 1. | Nanodiamonds |
|
| [20,58] |
| 2. | Quantum dots |
|
| [2,55,58,59] |
| 3. | Nanoshells |
|
| [13,55,60] |
| Quaternary ammonium methacrylate (QAM) nanoparticles |
|
| [17,18,61] | |
| Quaternary ammonium polyethyleneimine (QPEI) nanoparticles |
|
| [62,63] | |
| Amorphous calcium phosphate nanoparticles (ACP NPs) |
|
| [5,10,64] | |
| Nanoplatelet-based nanomaterials |
|
| [14,20,65,66] |
| Sr. No. | Nanotube-Based Nanomaterials | Properties | Applications | References |
|---|---|---|---|---|
| 1. | Carbon nanotubes (CNTs) |
|
| [38,40] |
| 2. | Halloysite nanotubes (HNTs) |
|
| [2,15,59] |
| 3. | Graphene oxide nanoplatelets |
|
| [41,42] |
| Biological Limitations | Chemical and Mechanical Limitations | Social Limitations | Ethical Limitations | Economic Limitations |
|---|---|---|---|---|
| Developing bio-friendly nanomaterials; Managing healthcare concerns; Extensive research needed. | Ensuring nanotechnological biocompatibility; Toxicity profiling and safety analyses. | Accessibility and acceptability; Overcoming social xenophobia. | Patients approval; Family consent; Dosage; Consideration and prior animal testing; Informed consent for human experimentation. | Marketing issues; Cost management; Financial constraints; Customer retention programs. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Malik, S.; Waheed, Y. Emerging Applications of Nanotechnology in Dentistry. Dent. J. 2023, 11, 266. https://doi.org/10.3390/dj11110266
Malik S, Waheed Y. Emerging Applications of Nanotechnology in Dentistry. Dentistry Journal. 2023; 11(11):266. https://doi.org/10.3390/dj11110266
Chicago/Turabian StyleMalik, Shiza, and Yasir Waheed. 2023. "Emerging Applications of Nanotechnology in Dentistry" Dentistry Journal 11, no. 11: 266. https://doi.org/10.3390/dj11110266