Trusting the Dentist—Expecting a Leap of Faith vs. a Well-Defined Strategy for Anxious Patients
Abstract
:1. Introduction
2. Methods
2.1. Derivation of the Conceptual Components of Trust Re. Patient/Dentist/Anxiety
2.1.1. Antecedents of Trust
2.1.2. Attributes of Trust
2.1.3. Boundaries of Trust
2.1.4. Outcomes of Trust
“Trust emerges from the identification of a need that cannot be met without the assistance of another and some assessment of the risk involved in relying on the other to meet this need. Trust is a willing dependency on another’s actions, but it is limited to the area of need and is subject to overt and covert testing. The outcome of trust is an evaluation of the congruence between expectations of the trusted person and their actions.”
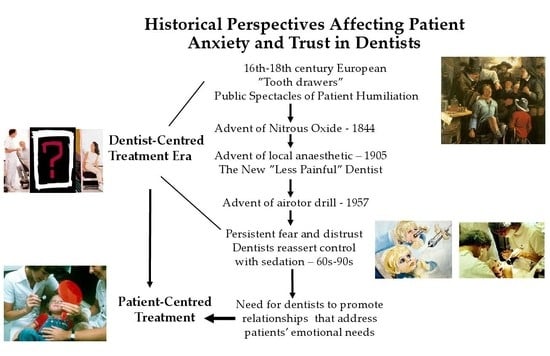
2.1.5. The Historical Background of Dentist-Patient Trust and Anxiety about Dental Treatment
Modern Society and the Image of the Dentist
3. Results
4. Discussion
4.1. Well-Defined Strategies to Improve Trust and Decrease Dental Anxiety
4.1.1. Increasing Patient Perceptions of Control in the Dental Chair
4.1.2. Practicing Active Listening, Empathy and Relationship Building
5. Conclusions
6. Future Directions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Moore, R. The Phenomenon of Dental Fear—Studies in Clinical Diagnosis, Measurement and Treatment. Ph.D. Thesis, University of Aarhus, Aarhus, Denmark, 1991. [Google Scholar]
- Moore, R. Psychosocial Aspects of Dental Anxiety and Clinical Pain Phenomena. Ph.D. Thesis, Aarhus University, Aarhus, Denmark, 2006. [Google Scholar]
- Armfield, J.; Ketting, M.; Chrisopoulos, S.; Baker, S.R. Do people trust dentists? Development of the Dentist Trust Scale. Austral. Dent. J. 2017, 62, 355–362. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Song, Y.; Luzzi, L.; Chrisopoulos, S.; Brennan, D.S. Are trust and satisfaction similar in dental care settings? Comm. Dent. Oral Epidemiol. 2020, 48, 480–486. [Google Scholar] [CrossRef] [PubMed]
- Hall, M.A.; Zheng, B.; Dugan, E.; Camacho, F.; Kidd, K.E.; Mishra, A.; Balkrishnan, R. Measuring Patients’ Trust in their Primary Care Providers. Med. Care Res. Rev. 2002, 59, 293–318. [Google Scholar] [CrossRef] [PubMed]
- Hupcey, J.E.; Penrod, J.; Morse, J.M.; Mitcham, C. An exploration and advancement of the concept of trust. J. Adv. Nurs. 2001, 36, 282–293. [Google Scholar] [CrossRef] [PubMed]
- Morse, J.M.; Havens, G.A.; Wilson, S. The comforting interaction: Developing a model of nurse-patient relationship. Schol. Inq. Nurs. Pract. 1997, 11, 321–343. [Google Scholar]
- Song, Y.; Luzzi, L.; Brennan, D.S. Trust in dentist-patient relationships: Mapping the relevant concepts. Eur. J. Oral Sci. 2020, 128, 110–119. [Google Scholar] [CrossRef]
- Wu, L.; Buchanan, H. Translation and validation of the Revised Dental Beliefs Survey (DBS-R) in China. Psychol. Health Med. 2020, 25, 812–823. [Google Scholar] [CrossRef]
- Wu, L.; Buchanan, H.; Topcu, G. Are dental-related psychological variables important for dental attendance in China? A cross-sectional study. J. Public Health Dent. 2021, 1–8. [Google Scholar] [CrossRef]
- Weiner, A. The Fearful Dental Patient: A Guide to Understanding and Managing; Wiley Blackwell: Ames, IO, USA, 2010. [Google Scholar]
- Milgrom, P.; Weinstein, P.; Heaton, L.J. Treating Fearful Dental Patients—A Patient Management Handbook, 3rd ed.; Dental Behavioral Resources: Seattle, WA, USA, 2009. [Google Scholar]
- Locker, D.; Liddell, A.; Shapiro, D. Diagnostic categories of dental anxiety: A population-based study. Behav. Res. Ther. 1999, 37, 25–37. [Google Scholar] [CrossRef]
- Yuan, S.; Freeman, R.; Hill, K.; Newton, T.; Humphris, G. Communication, Trust and Dental Anxiety: A Person-Centred Approach for Dental Attendance Behaviours. Dent. J. 2020, 8, 118. [Google Scholar] [CrossRef]
- Morse, J.M. Analyzing and Conceptualizing the Theoretical Foundations of Nursing; Springer: New York, NY, USA, 2017. [Google Scholar]
- Balkrishnan, R.P.; Dugan, E.P.; Camacho, F.T.M.S.; Hall, M.A.J.D. Trust and Satisfaction With Physicians, Insurers, and the Medical Profession. Med. Care 2003, 41, 1058–1064. [Google Scholar] [CrossRef]
- Dyer, T.; Owens, J.; Robinson, P.G. The acceptability of healthcare: From satisfaction to trust. Comm. Dent. Health 2016, 33, 1–10. [Google Scholar]
- Hoffman-Axthelm, W. History of Dentistry; Quintessence: Chicago, IL, USA, 1981. [Google Scholar]
- Mandel, I.D. Changing dental images—From stone tablets to comic strips. J. Am. Dent. Assoc. 1989, 118, 695–699. [Google Scholar] [CrossRef]
- Ring, M.E. Dentistry—An Illustrated History; Abrams: New York, NY, USA, 1985. [Google Scholar]
- DiMatteo, M.R.; McBride, C.A.; Shugars, D.A.; O’Neil, E.H. Public attitudes toward dentists: A U.S. household survey. J. Am. Dent. Assoc. 1995, 126, 1563–1570. [Google Scholar] [CrossRef]
- Reifel, N.M.; Rana, H.; Marcus, M. Consumer satisfaction. Adv. Dent. Res. 1997, 11, 281–290. [Google Scholar] [CrossRef]
- Skogedal, O.; Heloe, L.A. Public opinions on dentists in Norway. Comm. Dent. Oral Epidemiol. 1979, 7, 65–68. [Google Scholar] [CrossRef]
- Berry, J.H.; McCann, D. Dentistry’s public image: Does it need a boost? J. Am. Dent. Assoc. 1989, 118, 687–692. [Google Scholar] [CrossRef]
- Schuman, N.J.; Owens, B.M.; Johnson, W.W.; Moore, D.S. Dentistry as portrayed in motion pictures and television. Compendium 1993, 14, 102–106. [Google Scholar]
- Davis, P. The Social Context of Dentistry; Croom Helm: London, UK, 1980. [Google Scholar]
- Nettleton, S. Power and pain: The location of pain and fear in dentistry and the creation of a dental subject. Soc. Sci. Med. 1989, 29, 1183–1190. [Google Scholar] [CrossRef]
- Roper-Hall, H.T. Sedatives in dentistry. Br. Dent. J. 1935, 59, 177–186. [Google Scholar]
- Braceland, F.J. Psychologic and psychiatric aspects of pain control. In Control of Pain in Dental Practice: A Symposium Conducted by the Academy of Stomatology; Appleton, J.L.T., Ed.; Lippincott: Philadelphia, PA, USA, 1940; pp. 56–80. [Google Scholar]
- Best, E.S. The psychology of pain control. J. Am. Dent. Assoc. 1935, 22, 256–267. [Google Scholar]
- Epstein, S. Teaching psychology to dental students. J. Dent. Educ. 1964, 28, 203–206. [Google Scholar]
- Kent, G. Self-efficacious control over reported physiological, cognitive and behavioral symptoms of dental anxiety. Behav. Res. Ther. 1987, 25, 341–347. [Google Scholar] [CrossRef]
- Kent, G.; Gibbons, R. Self-efficacy and the control of anxious cognitions. J. Behav. Ther. Exp. Psychiatr. 1987, 18, 33–40. [Google Scholar] [CrossRef]
- Corah, N.L. Effect of perceived control on stress in pedodontic patients. J. Dent. Res. 1973, 52, 1261–1264. [Google Scholar] [CrossRef] [PubMed]
- Corah, N.L.; Bissell, G.D.; Illing, S.J. Effect of perceived control on stress reduction in adult dental patients. J. Dent. Res. 1978, 57, 74–76. [Google Scholar] [CrossRef] [PubMed]
- Gale, E.N. Fears of the dental situation. J. Dent. Res. 1972, 51, 964–966. [Google Scholar] [CrossRef] [PubMed]
- De Jongh, A.; Muris, P.; ter Horst, G.; Duyx, M.P. Acquisition and maintenance of dental anxiety: The role of conditioning experiences and cognitive factors. Behav. Res. Ther. 1995, 33, 205–210. [Google Scholar] [CrossRef]
- Moore, R.; Brødsgaard, I.; Rosenberg, N. The contribution of embarrassment to phobic dental anxiety: A qualitative research study. BMC Psychiatr. 2004, 4, 10. [Google Scholar] [CrossRef] [Green Version]
- Moore, R.; Jensen, C.G.; Andersen, L.B.; Brødsgaard, I. Reconsidering Co-Morbid Traits in Explanatory Models of High Dental Anxiety Using a Comparison of Psychiatric and Normal Patient Samples. Open J. Stomatol. 2016, 6, 211–227. [Google Scholar] [CrossRef] [Green Version]
- Coleman, H.; Burton, J. Aspects of control in the dentist-patient relationship. Int. J. Soc. Lang. 1985, 51, 75–104. [Google Scholar] [CrossRef]
- Walji, M.F.; Karimbux, N.Y.; Spielman, A.I. Person-Centered Care: Opportunities and Challenges for Academic Dental Institutions and Programs. J. Dent. Educ. 2017, 81, 1265–1272. [Google Scholar] [CrossRef] [Green Version]
- Jacquot, J. Trust in the Dentist-Patient Relationship: A Review. Available online: https://www.jyi.org/2005-june/2005/6/8/trust-in-the-dentist-patient-relationship-a-review (accessed on 1 June 2005).
- Kent, G.; Warren, P. A study of factors associated with changes in dental anxiety. J. Dent. Res. 1985, 64, 1316–1318. [Google Scholar] [CrossRef]
- Arntz, A.; Van Eck, M.; Heijmans, M. Predictions of dental pain: The fear of any expected evil, is worse than the evil itself. Behav. Res. Ther. 1990, 28, 29–41. [Google Scholar] [CrossRef]
- Corah, N.L.; O’Shea, R.M.; Bissell, G.D.; Thines, T.J.; Mendola, P. The dentist-patient relationship: Perceived dentist behaviors that reduce patient anxiety and increase satisfaction. J. Am. Dent. Assoc. 1988, 116, 73–76. [Google Scholar] [CrossRef]
- O’Shea, R.M.; Corah, N.L.; Thines, T.J. Dental patients’ advice on how to reduce anxiety. Gen. Dent. 1986, 34, 44–47. [Google Scholar]
- Corah, N.L.; O’Shea, R.M.; Bissell, G.D. The dentist-patient relationship: Perceptions by patients of dentist behavior in relation to satisfaction and anxiety. J. Am. Dent. Assoc. 1985, 111, 443–446. [Google Scholar] [CrossRef]
- Corah, N.L.; O’Shea, R.M.; Bissell, G.D. The dentist-patient relationship: Mutual perceptions and behaviors. J. Am. Dent. Assoc. 1986, 113, 253–255. [Google Scholar] [CrossRef]
- Apelian, N.; Vergnes, J.-N.; Bedos, C. Is the dental profession ready for person-centred care? Br. Dent. J. 2020, 229, 133–137. [Google Scholar] [CrossRef]
- Moore, R.; Brødsgaard, I.; Birn, H. Manifestations, acquisition and diagnostic categories of dental fear in a self-referred population. Behav. Res. Ther. 1991, 29, 51–60. [Google Scholar] [CrossRef]
- Berggren, U. Dental Fear and Avoidance—A Study of Etiology, Consequences and Treatment. Ph.D. Thesis, University of Göteborg, Göteborg, Sweden, 1984. [Google Scholar]
- Berggren, U. A Swedish Community Based Program for Treatment of Dental Fear and Avoidance; Institute of Odontology, University of Göteborg: Göteborg, Sweden, 1985; (Unpublished work). [Google Scholar]
- Collins, J.; Collins, M. Social Skills Training and the Professional Helper; John Wiley & Sons: Chichester, UK, 1992. [Google Scholar]
- Sadock, B.J. Group psychotherapy, combined individual and group psychotherapy, and psychodrama. In Comprehensive Textbook of Psychiatry; Kaplan, H., Sadock, B., Eds.; Williams & Wilkins: Baltimore, MD, USA, 1989; pp. 1517–1535. [Google Scholar]
- Moore, R.; Brødsgaard, I. Group therapy compared with individual desensitization for dental anxiety. Comm. Dent. Oral Epidemiol. 1994, 22, 258–262. [Google Scholar] [CrossRef]
- Berthelsen, H.; Petersen, P.E. [Stress at the workplace in view of changing demands to dentists] Stress i en tid med nye udfordringer til tandlægers faglighed. Tandlægebladet 2003, 107, 830–839. [Google Scholar]
- Dworkin, S.F.; Ference, T.P.; Giddon, D.B. Behavioral Science and Dental Practice; C.V. Mosby Company: St. Louis, MO, USA, 1978. [Google Scholar]
- Logan, H.L.; Muller, P.J.; Berst, M.R.; Yeaney, D.W. Contributors to dentists’ job satisfaction and quality of life. J. Am. Coll. Dent. 1997, 64, 39–43. [Google Scholar]
- Shugars, D.A.; DiMatteo, M.R.; Hays, R.D.; Cretin, S.; Johnson, J.D. Professional satisfaction among California general dentists. J. Dent. Educ. 1990, 54, 661–669. [Google Scholar] [CrossRef]
- Virshup, B.B.; Oppenberg, A.A.; Coleman, M.M. Strategic risk management: Reducing malpractice claims through more effective patient-doctor communication. Am. J. Med. Qual. 1999, 14, 153–159. [Google Scholar] [CrossRef]
- Freeman, R. The identification and behavioural management of the dentally anxious adult and child patient. In Essential Skills for Dentists; Mossey, P.A., Holsgrove, G.J., Davenport, E.S., Stirrups, D.R., Eds.; Oxford University Press: New York, NY, USA, 2006; pp. 132–149. [Google Scholar]
- Mills, I.; Frost, J.; Kay, E.; Moles, D.R. Person-centred care in dentistry—The patients’ perspective. Br. Dent. J. 2015, 218, 407–413. [Google Scholar] [CrossRef]
- Apelian, N.; Vergnes, J.-N.; Bedos, C. Humanizing clinical dentistry through a person-centred model. Int. J. Whole Person Care 2014, 1, 133–137. [Google Scholar] [CrossRef] [Green Version]
- Lee, H.; Chalmers, N.I.; Brow, A.; Boynes, S.; Monopoli, M.; Doherty, M.; Croom, O.; Engineer, L. Person-centered care model in dentistry. BMC Oral Health 2018, 18, 198. [Google Scholar] [CrossRef]
- Noushi, N.; Bedos, C. Developing Person-Centred Dental Care: The Perspectives of People Living in Poverty. Dent. J. 2020, 8, 82. [Google Scholar] [CrossRef]
- Feste, C.; Anderson, R.M. Empowerment: From philosophy to practice. Pat. Educ. Couns. 1995, 26, 139–144. [Google Scholar] [CrossRef]
- Persson, L.-O. Mood as a function of expectation and experience of success and failure in a test situations. Göteborg. Psychol. Rep. 1988, 18, 1–37. [Google Scholar]
- Arnold, M.S.; Butler, P.M.; Anderson, R.M.; Funnell, M.M.; Feste, C. Guidelines for facilitating a patient empowerment program. Diabetes Educ. 1995, 21, 308–312. [Google Scholar] [CrossRef] [PubMed]
- Anderson, R.M. Patient empowerment and the traditional medical model. A case of irreconcilable differences? Diabetes Care 1995, 18, 412–415. [Google Scholar] [CrossRef] [PubMed]
- Libassi, M.F.; Maluccio, A.N. Competence-centered social work: Prevention in action. J. Primary Prev. 1986, 6, 168–180. [Google Scholar] [CrossRef] [PubMed]
- Anderson, R.M.; Funnell, M.M.; Butler, P.M.; Arnold, M.S.; Fitzgerald, J.T.; Feste, C.C. Patient empowerment. Results of a randomized controlled trial. Diabetes Care 1995, 18, 943–949. [Google Scholar] [CrossRef]
- Brenders, D.A. Perceived control and the interpersonal dimension of health care. Health Commun. 1989, 1, 117–135. [Google Scholar] [CrossRef]
- Rogers, C.R. Client-Centered Therapy: Its Current Practice, Implications and Theory; Riverside: Cambridge, MA, USA, 1951. [Google Scholar]
- Rogers, C.R. On Becoming a Person—A Therapist’s View of Psychotherapy, 4th ed.; Constable: London, UK, 1972. [Google Scholar]
- Northouse, P.G. Effective helping relationships: The role of power and control. Health. Educ. Behav. 1997, 24, 703–706. [Google Scholar] [CrossRef]
- Stewart, M.; Brown, J.B.; Weston, W.W.; McWhinney, I.R.; McWilliam, C.L.; Freeman, T.R. Patient-Centered Medicine: Transforming the Clinical Method; Sage: Thousand Oaks, CA, USA, 1995. [Google Scholar]
- Dworkin, S.F. Behavioral sciences in dental education: Broad purposes and educational objectives. J. Dent. Educ. 1974, 38, 204–210. [Google Scholar] [CrossRef]
- Ewen, S.J. The dental interview: A guided psychological process. N. Y. J. Dent. 1951, 21, 392–397. [Google Scholar]
- Jepsen, C.H. Precision communication in dentistry. J. Dent. Pract. Adm. 1987, 4, 115–119. [Google Scholar]
- Jepsen, C.H. Are you harmful or helpful? J. Calif. Dent. Assoc. 1989, 17, 19–25. [Google Scholar]
- Rouse, R.A.; Hamilton, M.A. Dentists’ technical competance, communication, and personality as predictors of dental patient anxiety. J. Behav. Med. 1994, 13, 307–319. [Google Scholar] [CrossRef]
- Rouse, R.A. A paradigm of intervention: Emotional communication in dentistry. Health Commun. 1989, 1, 239–252. [Google Scholar] [CrossRef]
- Haase, R.F.; Tepper, D.T. Nonverbal components of empathic communication. J. Coun. Psychol. 1972, 19, 417–424. [Google Scholar] [CrossRef]
- Morse, J.M.; Bottorff, J.L.; Anderson, G.; O’Brien, B.; Solbjerg, S. Beyond empathy: Expanding expressions of caring. J. Adv. Nurs. 1992, 17, 809–821. [Google Scholar] [CrossRef]
- Morse, J.M.; Anderson, G.; Bottorff, J.L.; Yonge, O.; Brien, B.; Solberg, S.M.; McIlveen, K.H. Exploring empathy: A conceptual fit for nursing practice? Image J. Nurs. Scholarsh. 1992, 24, 273–280. [Google Scholar] [CrossRef]
- Borland, L.R. Odontophobia—Inordinate fear of dental tratment. Dent. Clin. N. Am. 1962, 6, 683–695. [Google Scholar]
- Kulich, K.R. Interpersonal Skills in the Dentist-Patient Relationship—The Art of Dentistry. Ph.D. Thesis, Department of Psychology, Göteborg University, Gothenburg, Sweden, 2000. [Google Scholar]
- Kulich, K.R.; Ryden, O.; Bengtsson, H. A descriptive study of how dentists view their profession and the doctor-patient relationship. Acta Odontol. Scand. 1998, 56, 206–209. [Google Scholar] [CrossRef]
- Kulich, K.R.; Berggren, U.; Hallberg, L.R. Model of the dentist-patient consultation in a clinic specializing in the treatment of dental phobic patients: A qualitative study. Acta Odontol. Scand. 2000, 58, 63–71. [Google Scholar] [CrossRef]
- Kulich, K.R.; Berggren, U.; Hallberg, L.R. A qualitative analysis of patient-centered dentistry in consultations with dental phobic patients. J. Health Commun. 2003, 8, 171–187. [Google Scholar] [CrossRef]
- Kulich, K.R.; Berggren, U.; Hakeberg, M.; Gustafsson, J.E. Factor structure of the Dental Beliefs Survey in a dental phobic population. Eur. J. Oral. Sci. 2001, 109, 235–240. [Google Scholar] [CrossRef]
- Balint, M. The Doctor, His Patient and the Illness, 2nd ed.; Pitman Medical Publishing: London, UK, 1964. [Google Scholar]
- Moerman, D.E. General medical effectiveness and human biology: Placebo effects in the treatment of ulcer disease. Med. Anthropol. Q. 1983, 14, 3–15. [Google Scholar] [CrossRef]
- Shapiro, A.P.; Morris, L.A. The placebo effect in medical and psychological therapies. In Handbook of Psychotherapy and Behavior Change: An Empirical Analysis; Garfield, S.L., Bergin, A.E., Eds.; John Wiley & Sons: New York, NY, USA, 1978; pp. 269–410. [Google Scholar]
- Roter, D.L.; Hall, J.A. Doctors Talking with Patients/Patients Talking with Doctors—Improving Communication in Medical Visits; Auburn House: Westport, CT, USA, 1993. [Google Scholar]
- Street, R.L., Jr. Patients’ satisfaction with dentists’ communicative style. Health Commun. 1989, 1, 137–154. [Google Scholar] [CrossRef]
- Street, R.L., Jr. Information-giving in medical consultations: The influence of patients’ communicative styles and personal characteristics. Soc. Sci. Med. 1991, 32, 541–548. [Google Scholar] [CrossRef]
- Street, R.L. Communicative styles and adaptations in physician-parent consultations. Soc. Sci. Med. 1992, 34, 1155–1163. [Google Scholar] [CrossRef]
- Street, R.L., Jr.; Millay, B. Analyzing patient participation in medical encounters. Health Commun. 2001, 13, 61–73. [Google Scholar] [CrossRef]
- Ong, L.M.; De Haes, J.C.; Hoos, A.M.; Lammes, F.B. Doctor-patient communication: A review of the literature. Soc. Sci. Med. 1995, 40, 903–918. [Google Scholar] [CrossRef]
- Carey, J.A.; Madill, A.; Manogue, M. Communications skills in dental education: A systematic research review. Eur. J. Dent. Educ. Off. J. Assoc. Dent. Educ. Eur. 2010, 14, 69–78. [Google Scholar] [CrossRef]
- Khalifah, A.M.; Celenza, A. Teaching and Assessment of Dentist-Patient Communication Skills: A Systematic Review to Identify Best-Evidence Methods. J. Dent. Educ. 2019, 83, 16–31. [Google Scholar] [CrossRef]
- Manning, P.; Ray, G.B. Setting the agenda: An analysis of negotiation strategies in clinical talk. Health Commun. 2002, 14, 451–473. [Google Scholar] [CrossRef]
- Segal, H.; Warner, R. Origins of paternalism. Med. Law 1985, 4, 269–273. [Google Scholar] [PubMed]
| Critical Inquiry: | Medicine | Sociology | Psychology | Nursing | Dentistry |
|---|---|---|---|---|---|
| 1. Trust develops: Instantaneously? Over time? | Over time | Over time | Both | Both | Over time |
| 2. Is ‘need’ a precondition of trust? | Yes | No | Yes | Yes | Yes |
| 3. Does trusting always place a person at risk? | Risk discussed | Calculated risk | Yes, commonly | Yes, commonly | Emotional risk often |
| 4. Does an individual choose to trust or not trust? | Yes, both | Yes, decision required | Yes | Yes, both | Yes, both |
| 5. Is trust inherent or does an individual learn to trust others? | No data | No data | Both | Both | Mostly learned |
| 6. Is person trusted by virtue of a role or by personal characteristics? | Both | Both | Personal traits | Both | Both, but role image is huge |
| 7. Is trust unilateral, bilateral, or reciprocal? | Reciprocal | Unilateral | All | All | Mostly unilateral |
| 8. Does establishment of trust involves testing behaviours? | No data | Yes | Yes | Yes | Yes |
| 9. Are there different kinds of trust? | Interpersonal vs. Global | Personal vs. System | Interpersonal | Intimate vs. Caring | Emotional, Technical, Economic |
| 10. What are the outcomes of loss of trust? | Lack rather than loss | Recontract | Lonliness/low self-image | Difficult recovery | Anxiety, pain, avoidance |
| 11. Expected outcome: Is trust a means to an end? | No data | Depends on expectation | Intrinsic vs. Extrinsic Outcomes | Means to achieve success | Yes: nice smile, no pain |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moore, R. Trusting the Dentist—Expecting a Leap of Faith vs. a Well-Defined Strategy for Anxious Patients. Dent. J. 2022, 10, 66. https://doi.org/10.3390/dj10040066
Moore R. Trusting the Dentist—Expecting a Leap of Faith vs. a Well-Defined Strategy for Anxious Patients. Dentistry Journal. 2022; 10(4):66. https://doi.org/10.3390/dj10040066
Chicago/Turabian StyleMoore, Rod. 2022. "Trusting the Dentist—Expecting a Leap of Faith vs. a Well-Defined Strategy for Anxious Patients" Dentistry Journal 10, no. 4: 66. https://doi.org/10.3390/dj10040066