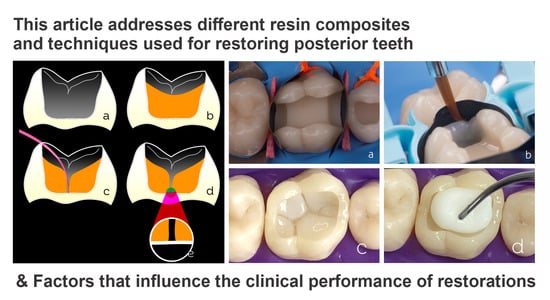
Resin Composites in Posterior Teeth: Clinical Performance and Direct Restorative Techniques
Abstract
:1. Introduction
2. Materials and Methods
3. Results and Discussion
3.1. Factors Influencing the Clinical Performance of Restorations
3.2. Resin Composites for Posterior Restorations
3.3. The Importance of Photoactivation
3.3.1. General Aspects Regarding LED Light-Curing Units
- Give preference to light-curing units with irradiance levels of ≥1000 mW/cm2, with large light guide tips that may avoid light concentration in small cavity areas, and units with a shape and/or design that makes them suitable for accessing the posterior dentition;
- The use of polywave units is not mandatory unless the resin composite manufacturer indicates otherwise;
- Routinely test the irradiance level of the unit to ensure that there has been no loss of power with clinical usage and aging;
- Cordless units should not be used when their battery is low (<25%);
- Tilting, inclination, or distancing of the light guide from the cavity may generate shadow areas or reduce the irradiance reaching the composite increment;
- Avoid several sequential photoactivations, e.g., irradiance times rounding off 2 min or more, and use intervals because the repetition of photoactivations may reduce the irradiance level;
- Do not purchase products of uncertain origin, brands without regulatory clearance in your country, or those for which the manufacturer does not provide auditable information about product specifications and tests.
3.3.2. Aspects to Improve the Efficiency of Photoactivation Procedures
- Learn how and train yourself to deliver maximum levels of light irradiance to the composite increment by correctly positioning the tip parallel and as close as possible to the irradiated surface.
- Keep the light guide’s tip clean, use barriers such as transparent polyvinyl chloride film without creating areas where the barrier becomes thick or poorly adapted.
- Learn the photoactivation time of each resin composite that you use; they normally require energy doses between 6 to 24 J/cm2, which are calculated by the product of the irradiance multiplied by the exposure time (e.g., 1000 mW/cm2 × 20 s = 20 J/cm2).
- When using darker composite shades, increase photoactivation times by at least 10 s.
- When the tip’s adaptation to the cavity is not optimal, or the photoactivation is performed at an inclination or at a greater distance from the composite, the exposure time should be extended.
- Do not reduce the photoactivation time recommended by the manufacturer, even when using light-curing units with irradiance above 1500 mW/cm2.
- Do not expect that a large cavity should be light-cured using only one central exposure because there is a chance that the light will not adequately reach and polymerize all cavity margins.
- When necessary, use overlapping photoactivation procedures to reach larger areas, especially if the cavity creates shadowy areas during light irradiance.
- In deep cavities with low dentin thickness, be careful not to overheat the structure, especially when photoactivating the adhesive and the first composite increments. If necessary, use an interval before a new photopolymerization procedure and/or use an air stream to cool down the dental structure.
- Cover soft tissues with gauze to avoid exposure to light, especially when the irradiance is high, and the procedure is performed near the dental cervical margin for long times.
- The dentist and assistant should use visual protection (orange goggles) so they can observe the correct positioning of the tip throughout the photopolymerization procedure and to avoid indirect exposure to the blue light. If possible, patients should also use orange goggles for protection.
3.4. Key Elements and Occlusion Levels in Posterior Restorations
3.5. Restorative Techniques
3.5.1. Restoration Considering the Shades and Opacities of Composites
- Monochromatic technique: This is used mainly in shallow cavities. A single increment of the composite can be used for chromatic enamel (composites that present a shade such as A1 and A2). Body composites or universal composites can also be used as they present an intermediate shade and degree of translucency, that is, neither low translucency as composites for dentin nor translucency as composites for enamel. Non-VITA shades of enamel composites are an additional option because they have interesting optical characteristics with which toemulate the dental enamel.
- Bichromatic technique: This technique is widespread and frequently used in posterior direct restorations. It can be applied in several cavity configurations that present a structural loss of dentin and enamel, thus employing two shades/opacities of a composite. For the reconstruction of the dentin portion, a composite with lower translucency and high saturation (such as dentin A3.5 or A4) is a good option. Remember the need to maintain a space of approximately 1.5 mm for the reconstruction of the next enamel portion. The measurement of the spaces can be performed with instruments with rounded tips, e.g., instruments with two balls with diameters of 1.5 mm and 2.5 mm. The professional experience acquired in the clinical routine also helps. A less saturated and higher value enamel or body/universal composite (enamel A1 or A2 or body/universal) should be used for the enamel portion.
- Polychromatic technique: This technique uses more than two shades/opacities of the composite, aiming at an excellent degree of mimicry of the dental structures, but requires the dentist to dedicate more attention and time to performing the layering process. The reconstruction is initiated from the dentin portion using the same principles of the bichromatic technique concerning shade (composites for dentin of high saturation and low translucency), with the difference being the need to maintain a slightly larger space (approximately 2.5 mm) for two layers of enamel to be accommodated above. Next, the reconstruction of the chromatic enamel layer is performed, usually using composite A1 or A2, and again paying attention to the maintenance of space for the final layer of approximately 1.5 mm. As a final covering layer, achromatic composites are the ideal materials. Achromatic enamel resin composites are those that have no shade themselves. They exhibit optical properties very similar to natural enamel and help form a semi-translucent milky layer. These composites are value modulators; color value is an optical property of great importance in restorative dentistry. Unlike chromatic resin composites, achromatic composites generally have no relation to the VITA shade scale, nor do they follow the same nomenclatures among manufacturers.
3.5.2. Bichromatic Technique for Class I Cavities
3.5.3. Technique for Class II Restorations
3.5.4. Restorations Using Bulk-Fill Composites
3.5.5. Restoration Using Shade-Matching Resin Composites
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Shenoy, A. Is it the end of the road for dental amalgam? A critical review. J. Conserv. Dent. 2008, 11, 99–107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moraes, R.R.; Cenci, M.S.; Moura, J.R.; Demarco, F.F.; Loomans, B.; Opdam, N. Clinical performance of resin composite restorations. Curr. Oral Health Rep. 2022, 9, 22–31. [Google Scholar] [CrossRef]
- Craig, R.G. Selected properties of dental composites. J. Dent. Res. 1979, 58, 1544–1550. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ilie, N.; Hickel, R. Resin composite restorative materials. Aust Dent. J. 2011, 56 (Suppl. 1), 59–66. [Google Scholar] [CrossRef] [PubMed]
- Aminoroaya, A.; Esmaeely Neisiany, R.; Nouri Khorasani, S.; Panahi, P.; Das, O.; Ramakrishna, S. A review of dental composites: Methods of characterizations. ACS Biomater. Sci. Eng. 2020, 6, 3713–3744. [Google Scholar] [CrossRef]
- Da Rosa Rodolpho, P.A.; Donassollo, T.A.; Cenci, M.S.; Loguércio, A.D.; Moraes, R.R.; Bronkhorst, E.M.; Opdam, N.J.M.; Demarco, F.F. 22-Year clinical evaluation of the performance of two posterior composites with different filler characteristics. Dent. Mater. 2011, 27, 955–963. [Google Scholar] [CrossRef]
- Da Rosa Rodolpho, P.A.; Rodolfo, B.; Collares, K.; Correa, M.B.; Demarco, F.F.; Opdam, N.J.M.; Cenci, M.S.; Moraes, R.R. Clinical performance of posterior resin composite restorations after up to 33 years. Dent. Mater. 2022, 38, 680–688. [Google Scholar] [CrossRef]
- Demarco, F.F.; Collares, K.; Coelho-de-Souza, F.H.; Correa, M.B.; Cenci, M.S.; Moraes, R.R.; Opdam, N.J. Anterior composite restorations: A systematic review on long-term survival and reasons for failure. Dent. Mater. 2015, 31, 1214–1224. [Google Scholar] [CrossRef]
- Demarco, F.F.; Collares, K.; Correa, M.B.; Cenci, M.S.; Moraes, R.R.; Opdam, N.J. Should my composite restorations last forever? Why are they failing? Braz. Oral Res. 2017, 31 (Suppl. 1), e56. [Google Scholar] [CrossRef] [Green Version]
- Demarco, F.F.; Corrêa, M.B.; Cenci, M.S.; Moraes, R.R.; Opdam, N.J. Longevity of posterior composite restorations: Not only a matter of materials. Dent. Mater. 2012, 28, 87–101. [Google Scholar] [CrossRef]
- Opdam, N.J.; Bronkhorst, E.M.; Loomans, B.A.; Huysmans, M.C. 12-year survival of composite vs. amalgam restorations. J. Dent. Res. 2010, 89, 1063–1067. [Google Scholar] [CrossRef] [PubMed]
- Pallesen, U.; van Dijken, J.W. A randomized controlled 30 years follow up of three conventional resin composites in Class II restorations. Dent. Mater. 2015, 31, 1232–1244. [Google Scholar] [CrossRef] [PubMed]
- Van de Sande, F.H.; Opdam, N.J.; Rodolpho, P.A.; Correa, M.B.; Demarco, F.F.; Cenci, M.S. Patient risk factors’ influence on survival of posterior composites. J. Dent. Res. 2013, 92 (Suppl. 7), 78S–83S. [Google Scholar] [CrossRef] [PubMed]
- Laske, M.; Opdam, N.J.; Bronkhorst, E.M.; Braspenning, J.C.; Huysmans, M.C. Risk factors for dental restoration survival: A practice-based study. J. Dent. Res. 2019, 98, 414–422. [Google Scholar] [CrossRef]
- Burke, F.J.; Lucarotti, P.S. The ultimate guide to restoration longevity in England and Wales. Part 10: Key findings from a ten million restoration dataset. Br. Dent. J. 2018, 225, 1011–1018. [Google Scholar] [CrossRef]
- Baldissera, R.A.; Corrêa, M.B.; Schuch, H.S.; Collares, K.; Nascimento, G.G.; Jardim, P.S.; Moraes, R.R.; Opdam, N.J.; Demarco, F.F. Are there universal restorative composites for anterior and posterior teeth? J. Dent. 2013, 41, 1027–1035. [Google Scholar] [CrossRef]
- Kuper, N.K.; Opdam, N.J.; Bronkhorst, E.M.; Huysmans, M.C. The infuence of approximal restoration extension on the development of secondary caries. J. Dent. 2012, 40, 241–247. [Google Scholar] [CrossRef]
- Van Meerbeek, B.; Yoshihara, K.; Van Landuyt, K.; Yoshida, Y.; Peumans, M. From Buonocore’s pioneering acid-etch technique to self-adhering restoratives. A status perspective of rapidly advancing dental adhesive technology. J. Adhes. Dent. 2020, 22, 7–34. [Google Scholar]
- Jardim, J.J.; Mestrinho, H.D.; Koppe, B.; de Paula, L.M.; Alves, L.S.; Yamaguti, P.M.; Almeida, J.C.F.; Maltz, M. Restorations after selective caries removal: 5-Year randomized trial. J. Dent. 2020, 99, 103416. [Google Scholar] [CrossRef]
- Laske, M.; Opdam, N.J.; Bronkhorst, E.M.; Braspenning, J.C.C.; Huysmans, M.C. Longevity of direct restorations in Dutch dental practices. Descriptive study out of a practice based research network. J. Dent. 2016, 46, 12–17. [Google Scholar] [CrossRef]
- Da Rosa, W.L.; Lima, V.P.; Moraes, R.R.; Piva, E.; da Silva, A.F. Is a calcium hydroxide liner necessary in the treatment of deep caries lesions? A systematic review and meta-analysis. Int. Endod. J. 2019, 52, 588–603. [Google Scholar] [CrossRef] [PubMed]
- Skupien, J.A.; Opdam, N.; Winnen, R.; Bronkhorst, E.; Kreulen, C.; Pereira-Cenci, T.; Huysmans, M.C. A practice-based study on the survival of restored endodontically treated teeth. J. Endod. 2013, 39, 1335–1340. [Google Scholar] [CrossRef] [PubMed]
- Jirathanyanatt, T.; Suksaphar, W.; Banomyong, D.; Ngoenwiwatkul, Y. Endodontically treated posterior teeth restored with or without crown restorations: A 5-year retrospective study of survival rates from fracture. J. Investig. Clin. Dent. 2019, 10, e12426. [Google Scholar] [CrossRef] [PubMed]
- Laske, M.; Opdam, N.J.; Bronkhorst, E.M.; Braspenning, J.C.; Huysmans, M.C. Ten-year survival of class II restorations placed by general practitioners. JDR Clin. Trans. Res. 2016, 1, 292–299. [Google Scholar] [CrossRef] [PubMed]
- Burke, F.J.; Lucarotti, P.S. The ultimate guide to restoration longevity in England and Wales. Part 4: Resin composite restorations: Time to next intervention and to extraction of the restored tooth. Br. Dent. J. 2018, 224, 945–956. [Google Scholar] [CrossRef] [Green Version]
- Mehta, S.B.; Bronkhorst, E.M.; Lima, V.P.; Crins, L.; Bronkhorst, H.; Opdam, N.J.; Huysmans, D.N.J.M.; Loomans, B.A. The effect of pre-treatment levels of tooth wear and the applied increase in the vertical dimension of occlusion (VDO) on the survival of direct resin composite restorations. J. Dent. 2021, 111, 103712. [Google Scholar] [CrossRef]
- Palmier, N.R.; Madrid Troconis, C.C.; Normando, A.G.C.; Guerra, E.N.S.; Araújo, A.L.D.; Arboleda, L.P.A.; Fonsêca, J.M.; de Pauli Paglioni, M.; Gomes-Silva, W.; Vechiato Filho, A.J.; et al. Impact of head and neck radiotherapy on the longevity of dental adhesive restorations: A systematic review and meta-analysis. J. Prosthet. Dent. 2021, in press. [Google Scholar] [CrossRef]
- Lucarotti, P.S.; Holder, R.L.; Burke, F.J. Outcome of direct restorations placed within the general dental services in England and Wales (Part 3): Variation by dentist factors. J. Dent. 2005, 33, 827–835. [Google Scholar] [CrossRef]
- Spreafico, R.C.; Krejci, I.; Dietschi, D. Clinical performance and marginal adaptation of class II direct and semidirect composite restorations over 3.5 years in vivo. J. Dent. 2005, 33, 499–507. [Google Scholar] [CrossRef]
- Van Dijken, J.W.; Pallesen, U. Clinical performance of a hybrid resin composite with and without an intermediate layer of flowable resin composite: A 7-year evaluation. Dent. Mater. 2011, 27, 150–156. [Google Scholar] [CrossRef]
- Yazici, A.R.; Kutuk, Z.B.; Ergin, E.; Karahan, S.; Antonson, S.A. Six-year clinical evaluation of bulk-fill and nanofill resin composite restorations. Clin. Oral Investig. 2022, 26, 417–426. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira, R.P.; Baia, J.; da Silva, T.; Magno, M.B.; Maia, L.C.; Loretto, S.C.; da Silva E Souza, M.H. Does addition of 10-MDP monomer in self-etch adhesive systems improve the clinical performance of noncarious cervical lesion restorations? A systematic review and meta-analysis. Oper. Dent. 2021, 46, E224–E239. [Google Scholar] [CrossRef] [PubMed]
- Dreweck, F.D.S.; Zarpellon, D.; Wambier, L.M.; Loguercio, A.D.; Reis, A.; Gomes, O.M. Is there evidence that three-step etch-and-rinse adhesives have better retention rates than one-step self-etch adhesives in noncarious cervical lesions? A systematic review and meta-analysis. J. Adhes. Dent. 2021, 23, 187–200. [Google Scholar] [PubMed]
- Dreweck, F.D.S.; Burey, A.; de Oliveira Dreweck, M.; Loguercio, A.D.; Reis, A. Adhesive strategies in cervical lesions: Systematic review and a network meta-analysis of randomized controlled trials. Clin. Oral Investig. 2021, 25, 2495–2510. [Google Scholar] [CrossRef] [PubMed]
- Miao, C.; Yang, X.; Wong, M.C.; Zou, J.; Zhou, X.; Li, C.; Wang, Y. Rubber dam isolation for restorative treatment in dental patients. Cochrane Database Syst. Rev. 2021, 5, CD009858. [Google Scholar]
- Schroeder, M.; Reis, A.; Luque-Martinez, I.; Loguercio, A.D.; Masterson, D.; Maia, L.C. Effect of enamel bevel on retention of cervical composite resin restorations: A systematic review and meta-analysis. J. Dent. 2015, 43, 777–788. [Google Scholar] [CrossRef] [PubMed]
- Opdam, N.J.; van de Sande, F.H.; Bronkhorst, E.; Cenci, M.S.; Bottenberg, P.; Pallesen, U.; Gaengler, P.; Lindberg, A.; Huysmans, M.C.; van Dijken, J.W. Longevity of posterior composite restorations: A systematic review and meta-analysis. J. Dent. Res. 2014, 93, 943–949. [Google Scholar] [CrossRef] [Green Version]
- Opdam, N.; Frankenberger, R.; Magne, P. From ‘direct versus indirect’ toward an integrated restorative concept in the posterior dentition. Oper. Dent. 2016, 41, S27–S34. [Google Scholar] [CrossRef] [Green Version]
- Pereira, F.A.; Zeola, L.F.; de Almeida Milito, G.; Reis, B.R.; Pereira, R.D.; Soares, P.V. Restorative material and loading type influence on the biomechanical behavior of wedge shaped cervical lesions. Clin. Oral Investig. 2016, 20, 433–441. [Google Scholar] [CrossRef]
- Blum, I.R.; Ozcan, M. Reparative dentistry: Possibilities and limitations. Curr. Oral Health Rep. 2018, 5, 264–269. [Google Scholar] [CrossRef] [Green Version]
- Estay, J.; Martín, J.; Viera, V.; Valdivieso, J.; Bersezio, C.; Vildosola, P.; Major, I.A.; Andrade, M.F.; Moraes, R.R.; Moncada, G.; et al. 12 Years of repair of amalgam and composite resins: A clinical study. Oper. Dent. 2018, 43, 12–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van de Sande, F.H.; Moraes, R.R.; Elias, R.V.; Montagner, A.F.; Rodolpho, P.A.; Demarco, F.F.; Cenci, M.S. Is composite repair suitable for anterior restorations? A long-term practice-based clinical study. Clin. Oral Investig. 2019, 23, 2795–2803. [Google Scholar] [CrossRef] [PubMed]
- Lima, V.P.; Crins, L.A.M.J.; Opdam, N.J.M.; Moraes, R.R.; Bronkhorst, E.M.; Huysmans, M.D.N.J.M.; Loomans, B.A.C. Deterioration of anterior resin composite restorations in moderate to severe tooth wear patients: 3-year results. Clin. Oral Investig. 2022, in press. [Google Scholar] [CrossRef]
- Loomans, B.; Opdam, N.; Attin, T.; Bartlett, D.; Edelhoff, D.; Frankenberger, R.; Benic, G.; Ramseyer, S.; Wetselaar, P.; Sterenborg, B.; et al. Severe tooth wear: European consensus statement on management guidelines. J. Adhes. Dent. 2017, 19, 111–119. [Google Scholar] [PubMed]
- Gurgan, S.; Koc Vural, U.; Kutuk, Z.B.; Cakir, F.Y. Does a new formula have an input in the clinical success of posterior composite restorations? A chat study. Clin. Oral Investig. 2021, 25, 1715–1727. [Google Scholar] [CrossRef] [PubMed]
- Van Dijken, J.W.V.; Pallesen, U. Bulk-filled posterior resin restorations based on stress-decreasing resin technology: A randomized, controlled 6-year evaluation. Eur. J. Oral Sci. 2017, 125, 303–309. [Google Scholar] [CrossRef]
- Heck, K.; Manhart, J.; Hickel, R.; Diegritz, C. Clinical evaluation of the bulk fill composite QuiXfil in molar class I and II cavities: 10-year results of a RCT. Dent. Mater. 2018, 34, e138–e147. [Google Scholar] [CrossRef]
- Pereira Sanchez, N.; Powers, J.M.; Paravina, R.D. Instrumental and visual evaluation of the color adjustment potential of resin composites. J. Esthet.Restor. Dent. 2019, 31, 465–470. [Google Scholar] [CrossRef]
- Schwendicke, F.; Göstemeyer, G.; Stolpe, M.; Krois, J. Amalgam alternatives: Cost-effectiveness and value of information analysis. J. Dent. Res. 2018, 97, 1317–1323. [Google Scholar] [CrossRef]
- Tobi, H.; Kreulen, C.M.; Vondeling, H.; van Amerongen, W.E. Cost-effectiveness of composite resins and amalgam in the replacement of amalgam Class II restorations. Community Dent. Oral Epidemiol. 1999, 27, 137–143. [Google Scholar] [CrossRef]
- Ferretti, M.A.; Pereira, R.; Lins, R.B.E.; Soares, M.G.C.; Pinto, L.J.H.; Martins, L.R.M.; Aguiar, F.H.B. Characterization of low-cost Brazilian resin composites submitted to tooth brushing. Braz. Oral Res. 2020, 35, e010. [Google Scholar] [CrossRef] [PubMed]
- Schneider, L.F.; Fonseca, A.S.; Natal, V.G.; Cavalcante, L.M.; Moraes, R.R. Is your opinion driven by the product price? Face 2019, 2, 274–276. [Google Scholar]
- Jandt, K.D.; Mills, R.W. A brief history of LED photopolymerization. Dent. Mater. 2013, 29, 605–617. [Google Scholar] [CrossRef] [PubMed]
- Lima, R.B.; Troconis, C.C.; Moreno, M.B.; Murillo-Gómez, F.; De Goes, M.F. Depth of cure of bulk fill resin composites: A systematic review. J. Esthet.Restor. Dent. 2018, 30, 492–501. [Google Scholar] [CrossRef] [PubMed]
- Kojic, D.D.; El-Mowafy, O.; Price, R.; El-Badrawy, W. Efficacy of light-emitting diode light polymerization units used in private practices in Toronto, Ontario, Canada. J. Am. Dent. Assoc. 2019, 150, 802–808. [Google Scholar] [CrossRef] [PubMed]
- Soares, C.J.; Rodrigues, M.P.; Oliveira, L.R.S.; Braga, S.S.L.; Barcelos, L.M.; Silva, G.R.D.; Giannini, M.; Price, R.B. An evaluation of the light output from 22 contemporary light curing units. Braz. Dent. J. 2017, 28, 362–371. [Google Scholar] [CrossRef] [Green Version]
- André, C.B.; Nima, G.; Sebold, M.; Giannini, M.; Price, R.B. Stability of the light output, oral cavity tip accessibility in posterior region and emission spectrum of light-curing units. Oper. Dent. 2018, 43, 398–407. [Google Scholar] [CrossRef]
- Price, R.B.; Shortall, A.C. Essentials of light curing. Dent. Update 2018, 45, 400–406. [Google Scholar] [CrossRef]
- Fluent, M.T.; Ferracane, J.L.; Mace, J.G.; Shah, A.R.; Price, R.B. Shedding light on a potential hazard: Dental light-curing units. J. Am. Dent. Assoc. 2019, 150, 1051–1058. [Google Scholar] [CrossRef]
- Rocha, M.G.; Maucoski, C.; Roulet, J.F.; Price, R.B. Depth of cure of 10 resin-based composites light-activated using a laser diode, multi-peak, and single-peak light-emitting diode curing lights. J. Dent. 2022, 122, 104141. [Google Scholar] [CrossRef]
- Alonso, A.A. Basics in Occlusion. In Desocclusion: Three-Dimensional Alignment and Occlusion, 1st ed.; Quintessence Publishing: Chicago, IL, USA, 2020; pp. 25–147. [Google Scholar]
- Muduroglu, R.; Ionescu, A.C.; Del Fabbro, M.; Scolavino, S.; Brambilla, E. Distribution of adhesive layer in class II composite resin restorations before/after interproximal matrix application. J. Dent. 2020, 103, 103494. [Google Scholar] [CrossRef] [PubMed]
- Chiodera, G.; Orsini, G.; Tosco, V.; Monterubbianesi, R.; Manauta, J.; Devoto, W.; Putignano, A. Essential Lines: A simplified filling and modeling technique for direct posterior composite restorations. Int. J. Esthet. Dent. 2021, 16, 168–184. [Google Scholar] [PubMed]









| Significant Influence on Longevity | |
| Cavity size and volume | Greater loss of dental structure and cavity walls increases the risk of failures [15] |
| Location of tooth in dental arch | Restorations in molars fail more often than in premolars, posterior restorations fail mainly due to fracture and secondary caries, and esthetic failures are prevalent in anterior restorations [16] |
| Cervical extension | Deep restorative margins increase the risk of failures [17] |
| Enamel etching | When enamel is present, etching with phosphoric acid is recommended [18] |
| Selective removal of carious tissue | Selective removal reduces the chances of pulp complications compared to more aggressive caries excavation methods [19] |
| Endodontic treatment | Restorations in endodontically treated teeth fail more often than in vital teeth [20] |
| Use of thick cavity liners | Glass-ionomer cement layers should be thin (<1 mm); the use of calcium hydroxide cement may not be necessary in deep cavities [21] |
| Presence of adjacent teeth | Restorations fail more often when no adjacent teeth are present or when the restored tooth is the last in the dental arch [22,23] |
| Patient’s age and sex | Studies generally report higher risk of restoration failures in men, children, and elderly patients [24,25] |
| Patient’s risks | Risks related to new caries lesions, occlusal stress, periodontal health, radiotherapy, smoking, dietary habits, and parafunctional habits (e.g., nail biting) increase the chances of failures [13,14,26,27] |
| Frequent change of dentists | Changing dentists increases the risk of unnecessary interventions and restoration failures [28] |
| Limited Influence on Longevity | |
| Restorative technique | It is important for the dentist to select a technique that will lead to fewer mistakes, to use few composite increments, to ensure low internal porosity, and provide optimal marginal adaptation and sealing [29,30,31] |
| Adhesive system | Simplified adhesives were usually regarded as having more failures than 3-step etch-and-rinse and 2-step self-etch adhesives, but current evidence points out that no significant differences may exist among different bonding systems [32,33,34] |
| Isolation method | When isolation of the operative field is carried out properly, no significant differences in the long term are observed between restorations carried out using a rubber dam or cotton rolls [35] |
| Beveling of enamel margins | It does not seem to affect the longevity of restorations and could be used at the dentist’s discretion [36] |
| Resin composite type and brand | The restorative technique and patient-related factors are more important to the longevity of restorations than material brands or types [7] |
| Polymerization shrinkage of composites | Contemporary composites have shrinkage levels compatible with long-lasting restorative procedures and techniques [37] |
| Finishing and polishing system | Although important for the quality of restorations, there is still insufficient evidence on the effect of different polishing systems for the longevity of restorations |
| Marginal staining | Marginal pigmentation does not entail marginal or secondary caries. Updated caries diagnosis methods and fewer unnecessary interventions will increase the longevity of restorations [7,38] |
| Technique * | Type of Resin Composite * | Characteristics |
|---|---|---|
| Conventional incremental technique (increments typically up to 2 mm in thickness) | Microhybrid/Nanohybrid | A resin matrix of dimethacrylate monomers filled with two types/sizes of inorganic particles: nanofillers (<100 nm) and microfillers (>1 μm) |
| Submicron/Supranano | Particle size is above the nano-scale (>100 nm) but below the micro-scale (<1 μm), typically 0.2–0.4 μm | |
| Nanofill | The filler system contains only discrete nanoparticles or nano-agglomerates | |
| Bulk-fill technique (increments may be larger than 2 mm in thickness) | Flowable | A fluid resin matrix of dimethacrylate monomers with low polymerization shrinkage, whose filler particles can be larger than those in conventional composites. The increased translucency allows for photopolymerization of thicker increments. Flowable bulk-fills should be used as a restorative base, which needs to be covered by a final, top layer of conventional composite |
| Regular | Similar in composition to the flowable composite but with higher viscosity. There is no need for a top layer of conventional composite. Typical increments are up to 4 mm in thickness | |
| Mixed | Composites with a regular viscosity that may be rendered more fluid through application of sonic vibration. Increments may be up to 5 mm in thickness | |
| Other nomenclatures for resin composites | Universal | Composites that can be used to restore both anterior and posterior teeth. More recently, the nomenclature has also been used for shade-matching composites |
| Single shade or shade-matching | Composites with chromatic technology for color matching different tooth shades (e.g., from A1 to D4) by using a single resin composite shade |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pizzolotto, L.; Moraes, R.R. Resin Composites in Posterior Teeth: Clinical Performance and Direct Restorative Techniques. Dent. J. 2022, 10, 222. https://doi.org/10.3390/dj10120222
Pizzolotto L, Moraes RR. Resin Composites in Posterior Teeth: Clinical Performance and Direct Restorative Techniques. Dentistry Journal. 2022; 10(12):222. https://doi.org/10.3390/dj10120222
Chicago/Turabian StylePizzolotto, Lucas, and Rafael R. Moraes. 2022. "Resin Composites in Posterior Teeth: Clinical Performance and Direct Restorative Techniques" Dentistry Journal 10, no. 12: 222. https://doi.org/10.3390/dj10120222