Chronic Conditions and School Participation of First-Year University Students—HOUSE ULisbon Study
Abstract
:1. Introduction
- ▪
- Extend prior research and contribute to increasing the knowledge regarding this specific population (i.e., first-year university students with CC);
- ▪
- Deepen the impact that the time of diagnosis can have on the students’ psychosocial functioning;
- ▪
- Explore more in-depth the type of barriers that students with CC feel in terms of their school participation;
- ▪
- Contribute to health, school, and public policies regarding the importance of adequate health care for university students with CC since first-year students experience a decisive phase in the management of their health condition (they are often displaced from home and manage their health conditions alone, in many cases for the first time) and in the transition from pediatric care to adult care.
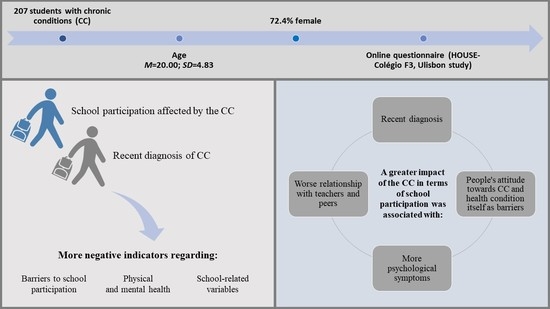
2. Method
2.1. Participants
2.2. Measures and Variables
2.3. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Noncommuicable Disease Education Manual. A Primer for Policy-Makers and Health-Care Professionals. 2018. Available online: https://apps.who.int/iris/handle/10665/260505 (accessed on 1 March 2022).
- World Health Organization. Noncommunicable Diseases in the Western Pacific. 2020. Available online: https://www.who.int/westernpacific/health-topics/noncommunicable-diseases (accessed on 1 March 2022).
- World Health Organization. Preventing Chronic Diseases: A Vital Investment. 2005. Available online: https://apps.who.int/iris/bitstream/handle/10665/43314/9241563001_eng.pdf?sequence=1&isAllowed=y (accessed on 1 March 2022).
- Forestier, B.; Anthoine, E.; Reguiai, Z.; Fohrer, C.; Blanchin, M. A systematic review of dimensions evaluating patient experience in chronic illness. Health Qual. Life Outcomes 2019, 17, 19. [Google Scholar] [CrossRef]
- Gledhill, J.; Rangel, L.; Garralda, E. Surviving chronic physical illness: Psychosocial outcome in adult life. Arch. Dis. Child. 2000, 83, 104–110. [Google Scholar] [CrossRef]
- Karekla, M.; Karademas, E.C.; Gloster, A.T. The Common Sense Model of Self-Regulation and Acceptance and Commitment Therapy: Integrating strategies to guide interventions for chronic illness. Health Psychol. Rev. 2018, 13, 490–503. [Google Scholar] [CrossRef]
- Mattsson, A. Long-Term Phsysical Illness in Childhood: A Challenge to Psychosocial adaptation. In Coping with Physical Illness; Moos, R.H., Tsu, V.D., Eds.; Springer: Berlin/Heidelberg, Germany, 2012; pp. 183–199. [Google Scholar]
- Butler, A.; Van Lieshout, R.J.; Lipman, E.L.; MacMillan, H.L.; Gonzalez, A.; Gorter, J.W.; Georgiades, K.; Speechley, K.N.; Boyle, M.H.; Ferro, M.A. Mental disorder in children with physical conditions: A pilot study. BMJ Open 2018, 8, e019011. [Google Scholar] [CrossRef]
- Ferro, M.A.; Gorter, J.W.; Boyle, M.H. Trajectories of depressive symptoms during the transition to young adulthood: The role of chronic illness. J. Affect. Disord. 2015, 174, 594–601. [Google Scholar] [CrossRef] [PubMed]
- Gold, S.M.; Köhler-Forsberg, O.; Moss-Morris, R.; Mehnert, A.; Miranda, J.J.; Bullinger, M.; Steptoe, A.; Whooley, M.A.; Otte, C. Comorbid depression in medical diseases. Nat. Rev. Dis. Prim. 2020, 6, 69. [Google Scholar] [CrossRef]
- Herts, K.L.; Wallis, E.; Maslow, G. College Freshmen with Chronic Illness: A Comparison with Healthy First-Year Students. J. Coll. Stud. Dev. 2014, 55, 475–480. [Google Scholar] [CrossRef]
- Revenson, T.A.; Hoyt, M.A. Chronic illness and mental health. In Encyclopedia of Mental Health, 2nd ed.; Friedman, H.S., Ed.; Academic Press: Cambridge, MA, USA; Elsevier: Amsterdam, The Netherlands, 2016; pp. 284–291. [Google Scholar]
- Runions, K.C.; Cross, D.S.; Vithiatharan, R.; Everard, M.; Hall, G. Bullying and psychosocial adjustment among children with and without asthma. J. Psychol. Couns. Sch. 2021, 31, 36–45. [Google Scholar] [CrossRef]
- Maslow, G.R.; Haydon, A.A.; Ford, C.A.; Halpern, C.T. Young Adult Outcomes of Children Growing Up with Chronic Illness. Arch. Pediatr. Adolesc. Med. 2011, 165, 256–261. [Google Scholar] [CrossRef]
- Mullins, A.J.; Gamwell, K.; Sharkey, C.M.; Bakula, D.M.; Tackett, A.P.; Suorsa, K.I.; Chaney, J.M.; Mullins, L.L. Illness uncertainty and illness intrusiveness as predictors of depressive and anxious symptomology in college students with chronic illnesses. J. Am. Coll. Health 2017, 65, 352–360. [Google Scholar] [CrossRef]
- Secinti, E.; Thompson, E.J.; Richards, M.; Gaysina, D. Research Review: Childhood chronic physical illness and adult emotional health—A systematic review and meta-analysis. J. Child Psychol. Psychiatry 2017, 9, 412–769. [Google Scholar] [CrossRef]
- Baker, A.M.; Johnston, J.; Davis, L.; Lockard, A. Medical Transition to a University Setting for Students with Chronic Illnesses. J. Coll. Stud. Dev. 2021, 62, 731–735. [Google Scholar] [CrossRef]
- Davis, E.S.; Paro, C. Preparing high school students with chronic illnesses for college transition: Lessons learned from college counselors. Prof. Sch. Couns. 2020, 23, 2156759X20907070. [Google Scholar] [CrossRef]
- Lemly, D.C.; Lawlor, K.; Scherer, E.A.; Kelemen, S.; Weitzman, E.R. College health service capacity to support youth with chronic medical conditions. Pediatrics 2014, 134, 885–891. [Google Scholar] [CrossRef]
- Ravert, R.D.; Russell, L.T. College students’ intentions to assist peers with chronic medical conditions. J. Am. Coll. Health 2020, 70, 355–362. [Google Scholar] [CrossRef]
- Saylor, J.; Hanna, K.M.; Calamaro, C.J. Experiences of College Students Who Are Newly Diagnosed with Type 1 Diabetes Mellitus. J. Pediatr. Nurs. 2019, 44, 74–80. [Google Scholar] [CrossRef] [PubMed]
- Kirkpatrick, K.M. Adolescents with Chronic Medical Conditions and High School Completion: The Importance of Perceived School Belonging. Contin. Educ. 2020, 1, 50–63. [Google Scholar] [CrossRef]
- Bethell, C.; Forrest, C.B.; Stumbo, S.; Gombojav, N.; Carle, A.; Irwin, C.E. Factors promoting or potentially impeding school success: Disparities and state variations for children with special health care needs. Matern. Child Health J. 2012, 16, 35–43. [Google Scholar] [CrossRef]
- Allen, C.W.; Diamond-Myrsten, S.; Rollins, L.K. School absenteeism in children and adolescents. Am. Fam. Physician 2018, 98, 738–744. [Google Scholar]
- Lum, A.; Wakefield, C.E.; Donnan, B.; Burns, M.A.; Fardell, J.E.; Jaffe, A.; Kasparian, N.A.; Kennedy, S.E.; Leach, S.T.; Lemberg, D.A.; et al. Facilitating engagement with school in students with chronic illness through positive education: A mixed-methods comparison study. Sch. Psychol. 2019, 34, 677. [Google Scholar] [CrossRef]
- Santos, T.; Matos, M.G.; Marques, A.; Simoes, C.; Leal, I.; Machado, M.C. Adolescent’s subjective perceptions of chronic disease and related psychosocial factors: Highlights from an outpatient context study. BMC Pediatr. 2016, 16, 211. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maslow, G.; Haydon, A.A.; McRee, A.-L.; Halpern, C.T. Protective Connections and Educational Attainment among Young Adults with Childhood-Onset Chronic Illness*. J. Sch. Health 2012, 82, 364–370. [Google Scholar] [CrossRef]
- Runions, K.C.; Vithiatharan, R.; Hancock, K.; Lin, A.; Brennan-Jones, C.G.; Gray, C.; Payne, D. Chronic health conditions, mental health and the school: A narrative review. Health Educ. J. 2019, 79, 471–483. [Google Scholar] [CrossRef]
- Lum, A.; Wakefield, C.E.; Donnan, B.; Burns, M.A.; Fardell, J.E.; Marshall, G.M. Understanding the school experiences of children and adolescents with serious chronic illness: A systematic meta-review. Child Care Health Dev. 2017, 43, 645–662. [Google Scholar] [CrossRef] [PubMed]
- Pittet, I.; Berchtold, A.; Akre, C.; Michaud, P.-A.; Suris, J.-C. Are adolescents with chronic conditions particularly at risk for bullying? Arch. Dis. Child. 2009, 95, 711–716. [Google Scholar] [CrossRef]
- Sentenac, M.; Gavin, A.; Nic Gabhainn, S.; Molcho, M.; Due, P.; Ravens-Sieberer, U.; de Matos, M.G.; Malkowska-Szkutnik, A.; Gobina, I.; Vollebergh, W.; et al. Peer victimization and subjective health among students reporting disability or chronic illness in 11 Western countries. Eur. J. Public Health 2012, 23, 421–426. [Google Scholar] [CrossRef]
- Sentenac, M.; Santos, T.; Augustine, L.; Michelsen, S.I.; Movsesyan, Y.; Ng, K.; Małkowska-Szkutnik, A.; Godeau, E. Chronic health conditions and school experience in school-aged children in 19 European countries. Eur. Child Adolesc. Psychiatry 2022, 1–11. [Google Scholar] [CrossRef]
- Taylor, R.M.; Gibson, F.; Franck, L.S. The experience of living with a chronic illness during adolescence: A critical review of the literature. J. Clin. Nurs. 2008, 17, 3083–3091. [Google Scholar] [CrossRef]
- Cerqueira, A.; Gaspar, T.; Botelho Guedes, F.; Godeau, E.; Gaspar de Matos, M. Chronic Conditions, School Participation and Quality of Life of Portuguese Adolescents: Highlights from the Health Behavior in School aged Children study-HBSC 2018. Child Indic. Res. 2022, 15, 297–313. [Google Scholar] [CrossRef]
- Kaushansky, D.; Cox, J.; Dodson, C.; McNeeley, M.; Kumar, S.; Iverson, E. Living a secret: Disclosure among adolescents and young adults with chronic illnesses. Chronic Illn. 2016, 13, 49–61. [Google Scholar] [CrossRef]
- Bradley, B.; Green, A.C. Do health and education agencies in the United States share responsibility for academic achievement and health? A review of 25 years of evidence about the relationship of adolescents’ academic achievement and health behaviors. J. Adolesc. Health 2013, 52, 523–532. [Google Scholar] [CrossRef] [Green Version]
- Georgiev, S.; Kamburova, M.S.; Un, M. A Healthy School Environment as a Precondition for the Welfare of Students and Staff. Int. J. Health Adm. Educ. Congr. 2015, 2, 31–43. [Google Scholar] [CrossRef]
- Pivik, J.; McComas, J.; Laflamme, M. Barriers and Facilitators to Inclusive Education. Counc. Rev. 2002, 69, 97–107. [Google Scholar] [CrossRef]
- Adama, E.A.; Arabiat, D.; Foster, M.J.; Afrifa-Yamoah, E.; Runions, K.; Vithiatharan, R.; Lin, A. The psychosocial impact of rare diseases among children and adolescents attending mainstream schools in Western Australia. Int. J. Incl. Educ. 2021, 1–14. [Google Scholar] [CrossRef]
- Márquez, C.; Melero-Aguilar, N. What are their thoughts about inclusion? Beliefs of faculty members about inclusive education. High. Educ. 2021, 83, 829–844. [Google Scholar] [CrossRef]
- Jackson, M. The special educational needs of adolescents living with chronic illness: A literature review. Int. J. Incl. Educ. 2013, 17, 543–554. [Google Scholar] [CrossRef]
- Emerson, N.D.; Distelberg, B.; Morrell, H.E.; Williams-Reade, J.; Tapanes, D.; Montgomery, S. Quality of life and school absenteeism in children with chronic illness. J. Sch. Nurs. 2016, 32, 258–266. [Google Scholar] [CrossRef]
- Brown, R.L. Perceived stigma among people with chronic health conditions: The influence of age, stressor exposure, and psychosocial resources. Res. Aging 2015, 37, 335–360. [Google Scholar] [CrossRef]
- Earnshaw, V.A.; Quinn, D.M.; Kalichman, S.C.; Park, C.L. Development and psychometric evaluation of the chronic illness anticipated stigma scale. J. Behav. Med. 2013, 36, 270–282. [Google Scholar] [CrossRef]
- Stuenkel, D.L.; Wong, V.K. Stigma. In Chronic Illness—Impact and Intervention; Lubkin, I.M., Larsen, P.D., Eds.; Jones & Bartlett Learning: Burlington, MA, USA, 2013. [Google Scholar]
- Matos, M.G. Equipa Aventura Social. In A Saúde dos Adolescentes Portugueses Após a Recessão, Relatório do Estudo 2018 do HBSC/OMS em Portugal; The Health of Portuguese Adolescents after the Recession, Report of the 2018 HBSC/WHO study in Portugal; HBSC: Geneva, Switzerland, 2018; Available online: https://aventurasocial.com/wp-content/uploads/2021/12/publicacao_1545534554.pdf (accessed on 9 March 2022).
- Inchley, J.; Currie, D.; Budisavljevic, S.; Torsheim, T.; Jåstad, A.; Cosma, A.; Kelly, C.; Arnasson, A.M. Spotlight on Adolescent Health and Well-Being; Findings from the 2017/2018 Health Behaviour in School-aged Children (HBSC) Survey in Europe and Canada. International Report; WHO: Geneva, Switzerland, 2020; Volume 1, Available online: https://apps.who.int/iris/bitstream/handle/10665/332091/9789289055000-eng.pdf (accessed on 9 March 2022).
- HOUSE-Colégio F3, ULisboa. Saúde e Estilos de vida dos Estudantes Universitários à Entrada da Universidade: Relatório do Estudo HOUSE-Colégio F3, Ulisboa; Health and Lifestyles of University Students at University Entrance: Report of the HOUSE-Colégio F3 Study, Ulisbon; University of Lisbon: Lisbon, Portugal, 2022. [Google Scholar]
- VandenBos, G.R. (Ed.) APA Dictionary of Psychology, 2nd ed.; American Psychological Association: Washington, DC, USA, 2015. [Google Scholar] [CrossRef]
- Cantril, H. The Pattern of Human Concerns; Rutgers University Press: New Brunswick, NJ, USA, 1965. [Google Scholar]
- Silva, J.A.D.; Souza, E.C.F.D.; Echazú Böschemeier, A.G.; Costa, C.C.M.D.; Bezerra, H.S.; Feitosa, E.E.L.C. Diagnosis of diabetes mellitus and living with a chronic condition: Participatory study. BMC Public Health 2018, 18, 699. [Google Scholar] [CrossRef] [Green Version]
- Helgeson, V.S.; Zajdel, M. Adjusting to Chronic Health Conditions. Annu. Rev. Psychol. 2017, 68, 545–571. [Google Scholar] [CrossRef] [PubMed]
- Gaspar, T.; Tomé, G.; Gaspar, S.; Guedes, F.B.; Cerqueira, A.; Matos, M.G. Como passam os adolescentes que vivem com doença crónica na escola, na família e com os amigos? [How do adolescents living with chronic illness are doing at school, with family and with friends?]. Rev. Psicol. Criança Adolesc. 2019, 10, 121–130. [Google Scholar]
- Anaby, D.; Hand, C.; Bradley, L.; DiRezze, B.; Forhan, M.; DiGiacomo, A.; Law, M. The effect of the environment on participation of children and youth with disabilities: A scoping review. Disabil. Rehabil. 2013, 35, 1589–1598. [Google Scholar] [CrossRef]
- Rai, S.S.; Syurina, E.V.; Peters, R.M.H.; Putri, A.I.; Zweekhorst, M.B.M. Non-Communicable Diseases-Related Stigma: A Mixed-Methods Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 6657. [Google Scholar] [CrossRef]
- Wakefield, E.O.; Zempsky, W.T.; Puhl, R.M.; Litt, M.D. Conceptualizing pain-related stigma in adolescent chronic pain: A literature review and preliminary focus group findings. PAIN Rep. 2018, 3, e679. [Google Scholar] [CrossRef]
- Berge, J.M.; Bauer, K.W.; Eisenberg, M.E.; Denny, K.; Neumark-Sztainer, D. Psychosocial and health behavior outcomes of young adults with asthma or diabetes. J. Community Med. Health Educ. 2012, 2, 144. [Google Scholar] [CrossRef] [PubMed]
- Compas, B.E.; Jaser, S.S.; Dunn, M.J.; Rodriguez, E.M. Coping with chronic illness in childhood and adolescence. Annu. Rev. Clin. Psychol. 2012, 8, 455–480. [Google Scholar] [CrossRef]
- Sav, A.; King, M.A.; Whitty, J.A.; Kendall, E.; McMillan, S.; Kelly, F.; Hunter, B.; Wheeler, A. Burden of treatment for chronic illness: A concept analysis and review of the literature. Health Expect. 2013, 18, 312–324. [Google Scholar] [CrossRef] [PubMed]
- Verhoof, E.J.; Maurice-Stam, H.; Heymans, H.S.; Evers, A.W.; Grootenhuis, M.A. Psychosocial well-being in young adults with chronic illness since childhood: The role of illness cognitions. Child Adolesc. Psychiatry Ment. Health 2014, 8, 12. [Google Scholar] [CrossRef]
- Champaloux, S.W.; Young, D.R. Childhood chronic health conditions and educational attainment: A social ecological approach. J. Adolesc. Health 2015, 56, 98–105. [Google Scholar] [CrossRef] [PubMed]
- Maslow, G.R.; Haydon, A.; McRee, A.-L.; Ford, C.A.; Halpern, C.T. Growing Up With a Chronic Illness: Social Success, Educational/Vocational Distress. J. Adolesc. Health 2011, 49, 206–212. [Google Scholar] [CrossRef] [Green Version]
- Campbell, F.; Biggs, K.; Aldiss, S.K.; O’Neill, P.M.; Clowes, M.; McDonagh, J.; While, A.; Gibson, F. Transition of care for adolescents from paediatric services to adult health services. Cochrane Database Syst. Rev. 2016, 4, CD009794. [Google Scholar] [CrossRef] [PubMed]
- Rutishauser, C.; Akré, C.; Surìs, J.-C. Transition from pediatric to adult health care: Expectations of adolescents with chronic disorders and their parents. Eur. J. Pediatr. 2010, 170, 865–871. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Variables | Measures |
|---|---|
| Recent diagnosis (in the last two years) | Recoded variable: 0—No; 1—Yes (original variable: 1—at birth; 2—before entering school; 3—1st cycle; 4—2nd cycle; 5—3rd cycle; 6—high school; 7—recently (last two years) |
| Concerns | Recoded variable: 0—No; 1—Yes (original variable: 1—Several times a day; 2—Practically every day; 3—Several times a week; 4—Several times a month; 5—Rarely or never worried) |
| School physical environment as a barrier to participation and academic success | 0—No; 1—Yes |
| People’s attitude towards CC as a barrier to participation and academic success | 0—No; 1—Yes |
| Health condition as a barrier to participation and academic success | 0—No; 1—Yes |
| Physical symptoms | Scale with five items (back pain, neck pain, headache, dizziness and stomach pain), on a five-point Likert scale (1—almost every day and 5—rarely or never). Minimum score of 5 and maximum of 25. The higher the value, the fewer physical symptoms. α = 0.76 |
| Psychological symptoms | Scale with five items (nervousness, irritation or bad mood, sadness and fear), on a five-point Likert scale (1—almost every day and 5—rarely or never). Minimum score of 4 and maximum of 20). The higher the value, the fewer psychological symptoms. α = 0.86 |
| Relationship with teachers | Scale adapted from Cantril [50], consisting of 11 steps, where the lowest step (0) corresponds to the worst quality of the relationship with teachers and the highest step (10) to the best quality of the relationship with teachers |
| Relationship with peers | Scale adapted from Cantril [50], consisting of 11 steps, where the lowest step (0) corresponds to the worst quality of the relationship with colleagues and the highest step (10) to the best quality of the relationship with peers |
| School participation affected by the CC | Scale with three items, which assess the impact that the chronic condition had on school participation (attendance, participation and academic success). α = 0.74 The variable was dichotomized with reference to affect or not to affect participation (No/Yes) |
| M ± SD or % (n) | p | |||
|---|---|---|---|---|
| Total (n = 207) | Recent Diagnosis No 71.3% (n = 127) | Recent Diagnosis Yes 28.7% (n = 50) | ||
| Concerns 2 | 0.633 | |||
| No | 10.7 (22) | 11.4 (14) | 14.0 (7) | |
| Yes | 89.3 (182) | 88.6 (109) | 86.0 (43) | |
| School physical environment as a barrier to participation and academic success 2 | 0.447 | |||
| No | 94.0 (172) | 92.2 (106) | 95.6 (43) | |
| Yes | 6.0 (11) | 7.8 (9) | 4.4 (2) | |
| People’s attitude towards CC as a barrier to participation and academic success 2 | 0.961 | |||
| No | 86.9 (159) | 87.0 (100) | 86.7 (39) | |
| Yes | 13.1 (24) | 13.0 (15) | 13.3 (6) | |
| Health condition as a barrier to participation and academic success 2 | ≤0.01 | |||
| No | 80.9 (148) | * 85.2 (98) | 66.7 (30) | |
| Yes | 19.1 (35) | 14.8 (17) | * 33.3 (15) | |
| Physical symptoms 1 | 18.13 ± 4.66 | 17.98 ± 4.70 | 17.59 ± 4.67 | 0.934 |
| Psychological symptoms 1 | 12.52 ± 4.46 | 12.59 ± 4.32 | 12.18 ± 4.53 | 0.634 |
| Relationship with teachers 1 | 6.86 ± 1.91 | 6.99 ± 1.85 | 6.26 ± 2.00 | 0.592 |
| Relationship with peers 1 | 7.38 ± 2.01 | 7.43 ± 1.89 | 6.98 ± 2.45 | ≤0.001 |
| School participation affected by the CC 1 | 3.45 ± 0.90 | 3.23 ± 0.66 | 4.00 ± 1.21 | ≤0.001 |
| No 2 | 76.3 (148) | * 87.0 (107) | 52.0 (26) | |
| Yes 2 | 23.7 (46) | 13.0 (16) | * 48.0 (24) | |
| M ± SD or % (n) | p | ||
|---|---|---|---|
| School Participation Affected by the CC No 76.3% (n = 148) | School Participation Affected by the CC Yes 23.7% (n = 46) | ||
| Recent diagnosis 2 | ≤0.001 | ||
| No | * 80.5 (107) | 40.0 (16) | |
| Yes | 19.5 (26) | * 60.0 (24) | |
| Concerns 2 | 0.277 | ||
| No | 12.2 (18) | 6.5 (3) | |
| Yes | 87.8 (129) | 93.5 (43) | |
| School physical environment as a barrier to participation and academic success 2 | 0.722 | ||
| No | 94.2 (130) | 92.7 (38) | |
| Yes | 5.8 (8) | 7.3 (3) | |
| People’s attitude towards CC as a barrier to participation and academic success 2 | ≤0.001 | ||
| No | * 94.2 (130) | 61.0 (25) | |
| Yes | 5.8 (8) | * 39.0 (16) | |
| Health condition as a barrier to participation and academic success 2 | ≤0.001 | ||
| No | * 94.2 (130) | 34.1 (14) | |
| Yes | 5.8 (8) | * 65.9 (27) | |
| Physical symptoms 1 | 18.74 ± 4.33 | 16.00 ± 5.34 | ≤0.01 |
| Psychological symptoms 1 | 13.14 ± 4.36 | 10.00 ± 4.25 | 0.941 |
| Relationship with teachers 1 | 7.19 ± 1.75 | 5.87 ± 2.21 | 0.138 |
| Relationship with peers 1 | 7.70 ± 1.82 | 6.35 ± 2.34 | ≤0.05 |
| Non-Standardized Coefficient | Standardized Coefficient | t | ||
|---|---|---|---|---|
| B | Standard Error | β | ||
| Recent diagnosis | 0.39 | 0.12 | 0.19 ** | 3.21 |
| Physical symptoms | 0.01 | 0.01 | 0.07 | 1.10 |
| Psychological symptoms | −0.03 | 0.01 | −0.15 * | −2.15 |
| Concerns | −0.28 | 0.16 | −0.11 | −1.73 |
| School physical environment as a barrier to participation and academic success | −0.19 | 0.20 | −0.06 | −0.96 |
| People’s attitude towards the chronic condition as a barrier to participation and academic success | 0.55 | 0.16 | 0.21 *** | 3.44 |
| Health condition as a barrier to participation and academic success | 1.05 | 0.14 | 0.45 *** | 7.34 |
| Relationship with teachers | −0.08 | 0.03 | −0.16 ** | −2.55 |
| Relationship with peers | −0.06 | 0.03 | −0.14 * | −2.20 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cerqueira, A.; Botelho Guedes, F.; Marques-Pinto, A.; Branco, A.; Galvão, C.; Sousa, J.; Goulao, L.F.; Bronze, M.R.; Viegas, W.; Gaspar, T.; et al. Chronic Conditions and School Participation of First-Year University Students—HOUSE ULisbon Study. Children 2022, 9, 1397. https://doi.org/10.3390/children9091397
Cerqueira A, Botelho Guedes F, Marques-Pinto A, Branco A, Galvão C, Sousa J, Goulao LF, Bronze MR, Viegas W, Gaspar T, et al. Chronic Conditions and School Participation of First-Year University Students—HOUSE ULisbon Study. Children. 2022; 9(9):1397. https://doi.org/10.3390/children9091397
Chicago/Turabian StyleCerqueira, Ana, Fábio Botelho Guedes, Alexandra Marques-Pinto, Amélia Branco, Cecília Galvão, Joana Sousa, Luis F. Goulao, Maria Rosário Bronze, Wanda Viegas, Tania Gaspar, and et al. 2022. "Chronic Conditions and School Participation of First-Year University Students—HOUSE ULisbon Study" Children 9, no. 9: 1397. https://doi.org/10.3390/children9091397